Abstract
Purpose
To assess if the evaluation of the spino-pelvic balance can be effective in the surgical decision making of the high-grade high dysplastic developmental spondylolisthesis (HDDS).
Methods
Sixteen patients affected with high-grade HDDS (6 treated with “in situ” fusion, and 10 with reduction and fusion) were retrospectively evaluated. A clinical and radiological assessment of the deformity correction was carried out, with a minimum follow-up of 2 years. The differences between the pre- and postoperative measures were statistically analyzed using a two-tailed, paired t test.
Results
The six patients treated with “in situ” fusion showed no statistically significant change at the last follow-up relative to pelvic tilt (PT), sacral slope (SS), and grade, while the 10 patients treated with reduction showed significant changes: PT significantly decreased following surgery, while SS and grade significantly increased.
Conclusions
The analysis of the spino-pelvic sagittal balance allows to identify two types of HDDS: the balanced deformities, which do not need reduction, and the unbalanced deformities, in which correction is needed.
Keywords: Spondylolisthesis, Sagittal balance, Reduction, “In situ” fusion
Introduction
The treatment of high-grade high dysplastic developmental spondylolisthesis (HDDS) is yet controversial. Many studies include a mixture of various types and grades of spondylolisthesis, making it difficult to determine the result of treatment of the specific entity of HDDS. Although the concept of reducing spinal deformity before fusion is attractive, the issue of surgical reduction versus “in situ” fusion remains controversial [4, 10, 24].
In situ posterolateral fusion is a well-known technique for which many surgeons have reported satisfactory clinical outcomes in low-grade spondylolisthesis [3, 19, 23]. In high-grade spondylolisthesis, the technique is prone to a significant rate of non-union or subsequent slip progression. For both low- and high-grade spondylolisthesis, in situ fusion runs contrary to the principle of restoring physiological alignment and balance and may have long-term implications on adjacent segment disease [1].
In L5-S1 spondylolisthesis, it has been clearly demonstrated over the past decade that sacro-pelvic morphology is abnormal and that combined with the presence of a local lumbo-sacral deformity and dysplasia, it can result in an abnormal sacro-pelvic orientation as well as to a disturbed global sagittal balance of the spine [6, 12, 18]. Reduction of the spondylolisthetic condition may lessen the incidence of non-union. Reduction of the slip angle (lumbosacral kyphosis) allows direct neural decompression and improves the sagittal lumbosacral orientation. The main argument against reduction is that it involves more extensive surgery, and an increase risk for neurologic injury [2, 25].
In the current controversy on whether high-grade deformities should or should not be reduced, Hresko et al. [7] divided HDDS in two different groups: the balanced deformities, which do not need reduction, and the unbalanced deformities, in which correction is mandatory, and Labelle et al. [13] provided a compelling rationale to reduce and realign the deformity, in order to restore global spino-pelvic balance and improve the biomechanical environment for fusion.
This paper reports the results of a retrospective study of 16 consecutive patients with lumbar high-grade HDDS managed according with the proposal by Labelle et al. [13] with the aim to assess the clinical usefulness of their classification.
Methods
Study design
A retrospective, single-cohort, observational study of 16 consecutive patients with lumbosacral high-grade HDDS (Meyerding grade IV, and spondyloptosis), operated between April 2003 and September 2008. A retrospective clinical and radiological review of the deformity correction was carried out on all the patients, with a minimum follow-up of 2 years.
Patient sample
The average age of patients was 19.6 years (range 15.8–27.9 years). There were seven males and nine females. Six patients underwent single-level postero-lateral “in situ” fusion, by a direct S1-L5 pediculo-body (trans-discal) fixation, while ten patients underwent L5 reduction, posterior lumbar interbody fusion with two cages, and L5-S1 posterior fixation and fusion.
Deformity measures
Spondylolisthesis was radiographically measured according to the Taillard technique and Meyerding grade. In addition, the following parameters were measured as proposed by Labelle et al. [11]:
Pelvic incidence (PI) defined as the angle between a line joining the center of the upper endplate of S1 to the axis of the femoral heads and a line perpendicular to the upper endplate of S1.
Sacral slope (SS) defined as the angle between the sacral plate and the horizontal line.
Pelvic tilt (PT) defined as the angle between the vertical line and the line joining the middle of the sacral plate and the axis of the femoral heads. It is positive when the hip axis lies in front of the middle of the sacral plate.
Severity Index as described by Lamartina et al. [15].
Unstable zone as described by Lamartina [14].
Surgical indications
The principal indication for surgery was relief of low-back and radicular pain. All patients had low back pain, which worsened under supraphysiologic stress. There were 13 patients who complained of sciatic pain, 12 patients with L5 sensory deficits, and 5 patients who had a L5 combined motor and sensory deficit.
Surgical technique
After exposure of the transverse processes of L5 and S1, a Gill procedure with exposure of both the L5 and the S1 roots was accomplished. The L5 nerve roots were exposed far laterally.
Group with reduction Pedicle screws were placed bilaterally at L5 and the sacrum. The double-threaded Schanz screws (USS, Synthes) or the Uni-thread screws (Spinevision) were placed. Lumbosacral discectomy from both sides was performed, and interbody cages (titanium or PEEK cages filled with morselized iliac graft) were implanted bilaterally. The reduction of the slipped vertebral body was accomplished taking care to avoid any compression or over-distraction on the L5 roots. Finally, the pedicle screws were forced in compression to restore the normal lumbar lordosis, and lateral mass decortication and grafting was accomplished.
Group with “in situ” fusion
As described by Grob et al. [5], the screws were placed under fluoroscopic control. Laminectomy was performed as an additional procedure to decompress nerve roots, and postero-lateral fusion with autologous bone graft from iliac crest was accomplished.
Outcome measures
Patient demographics, surgical indications, operative details, and complications were recorded. Patients completed preoperative surveys recording Visual Analogue Pain Scores (VAS), and Short Form (SF)-12 Physical and Mental measures. Postoperative clinical outcome surveys recording VAS and SF-12 were administered along with patient satisfaction questionnaires at 6 weeks, 3, 6, 12, and 24 months or further follow-up.
Patient satisfaction surveys recorded five-point Patient Subjective Outcome scores (worse, unchanged, fair, good, excellent) and included two questions: “Do you consider the surgery was worthwhile?” “Under the same circumstances, would you have the surgery again?”
Retrospective measurements of the radiological parameters were accomplished on all the patients and were reviewed independently.
Statistical analysis
The differences between the pre- and postoperative measures of VAS, SF-12, sagittal displacement (olisthesis), and the other radiological parameters were analyzed using a two-tailed, paired t test.
Results
Clinical
Preoperative VAS improved from 6.8 ± 2.7 to 1.8 ± 3.2 at last follow-up (p < 0.01). The mean preoperative SF-12 measures, PCS and MCS, were 21.5 ± 11.8 and 34.7 ± 13.5, respectively. At the latest follow-up, they measured 43.4 ± 15.8 (p < 0.01) and 57.1 ± 11.7 (p < 0.01).
At final follow-up, 15 of 16 patients (93.8%) considered the surgery to have been worthwhile and indicated that they would have the surgery again under the same circumstances. Fourteen (87.5%) considered their outcome to be good or excellent, two felt they were unchanged.
Operative time and blood loss
For the reduction group, the mean surgical time was 216 min (range 180–310) and mean operative blood loss was 330 ml (range 120–800 ml).
For the group of in situ fusion the mean surgical time was 165 min (range 125–280) and mean operative blood loss was 210 ml (range 90–700 ml).
Operative complications
In this small series there were no serious intraoperative or interbody implant–related complications. There were no dural tears. Difficulty with pedicle screw placement was encountered in two patients.
Early and late postoperative complications
There was no pseudarthrosis. All patients had a solid bony fusion at latest follow-up. There was 1 superficial wound infection that responded to early reoperation. Two patients had signs of a L5 root lesion after surgery. In 1 of these patients, a revision was performed with further decompression of the L5 roots. Another patient who underwent reduction of a 84% L5-S1 slip back to 8% developed a delayed L5 radiculopathy with dysesthesia 3 days after surgery. This resolved completely over 6 weeks.
Deformity correction
Pre- and post-operative X-rays were available for analysis of deformity correction in all patients at the latest follow-up.
Table 1 provides the mean and standard deviations in the entire cohort for all radiological variables measured before and after surgery. With the exception of pelvic incidence, all other variables were significantly different after surgery (p < 0.01). The most important changes were noted for PT, which decreased significantly, SS which increased significantly, while grade was significantly improved from 87 to 40%.
Table 1.
Pre- and post-operative results for all measurements in the entire cohort, prior to sub grouping by type of surgery
| Variable | Pre-op | Post-op |
|---|---|---|
| Pelvic incidence (PI) | 77° ± 14 | 78° ± 13 |
| Pelvic tilt (PT)* | 35° ± 10 | 28° ± 11 |
| Sacral slope (SS)* | 41° ± 12 | 49° ± 13 |
| Grade* | 87% ± 21 | 40% ± 17 |
* indicates statistically significant difference (p < 0.01) between the pre-operative and the post-operative measure
At first glance, changes in SS and PT appeared relatively small when considering the entire cohort. However, changes became very significant when considering the two surgical sub-groups. The six patients treated with “in situ” fusion (Table 2), showed no statistically significant change at the last follow-up relative to PT, SS, and grade, while the 10 patients treated with correction of the deformity (Table 3) showed significant changes. Overall, pelvic tilt decreased significantly following surgery (from 41° to 30°, p < 0.01), while sacral slope increased significantly (from 36° to 47°, p < 0.01), and the same behavior can be observed for the grade (from 91 to 21%, p < 0.01).
Table 2.
Pre- and post-operative results for all measurements in the “in situ” fusion group
| Variable | Pre-op | Post-op |
|---|---|---|
| Pelvic incidence (PI) | 79° ± 17 | 78° ± 15 |
| Pelvic tilt (PT) | 25° ± 13 | 24° ± 12 |
| Sacral slope (SS) | 54° ± 18 | 55° ± 16 |
| Grade | 79% ± 12 | 75% ± 17 |
Table 3.
Pre- and post-operative results for all measurements in the reduction group
| Variable | Pre-op | Post-op |
|---|---|---|
| Pelvic incidence (PI) | 76° ± 13 | 77° ± 19 |
| Pelvic tilt (PT)* | 41° ± 15 | 30° ± 14 |
| Sacral slope (SS)* | 36° ± 11 | 47° ± 13 |
| Grade* | 91% ± 24 | 21% ± 10 |
* indicates statistically significant difference (p < 0.01) between the pre-operative and the post-operative measure
Discussion
The optimal surgical management of lumbar spondylitic spondylolisthesis remains controversial. Although the primary goal of surgery is the relief of neurological compression, the correction of associated deformity or spinal imbalance is attracting increasing attention in the literature [4, 9, 22].
With regard to early clinical outcomes, Kawakami et al. [9] in 2002 noted improved clinical recovery rates in patients undergoing fusion for degenerative spondylolisthesis when increased lordosis of the fused segments was achieved and the position of the plumb line in front of the sacrum was <35 mm.
Duval-Beaupère et al. [17, 20] have demonstrated that PI is an important anatomic parameter that describes the shape of the pelvis and greatly influences the configuration of the spine and pelvis, and thus of sagittal spino-pelvic alignment. PI is the algebraic sum of SS and PT, two position-dependent variables, which determine pelvic orientation in the sagittal plane. Because of this mathematical association between PI, SS, and PT, the morphology of the pelvis is a strong determinant of the spatial position of the pelvis and the spine in the standing position.
Recently, Hresko et al. [7] analyzed sagittal alignment in high grade spondylolisthesis patients and reported two distinct groups termed “balanced” and “unbalanced” pelvis. PT and SS were similar in balanced pelvis patients and control population with high PI. Unbalanced pelvis patients were characterized by a high PT and a low SS and, consequently, had a sagittal spinal alignment that differed from the balanced pelvis and control groups, suggesting that reduction techniques might be considered in this group. Moreover, excessive PT has been associated with an increased prevalence of pain [16].
Ideally, surgery should restore normal anatomy with minimal functional restriction. This process entails complete correction of the local deformity with the shortest possible fusion. Complete reduction of the L5/S1 slippage with restoration of segmental lordosis and correction of the sacral position (that is the reduction of the PT towards normal values) allows for normalization of the overall sagittal profile. The load distribution in the adjacent segments is normalized, and, thus, potential adjacent disc degeneration is avoided.
Our findings support the hypothesis that the reduction of the deformity is indicated only in that patients who show an unbalanced pelvis, while the patients with a balanced pelvis (Fig. 1a–c) need fusion, and correction is not necessary.
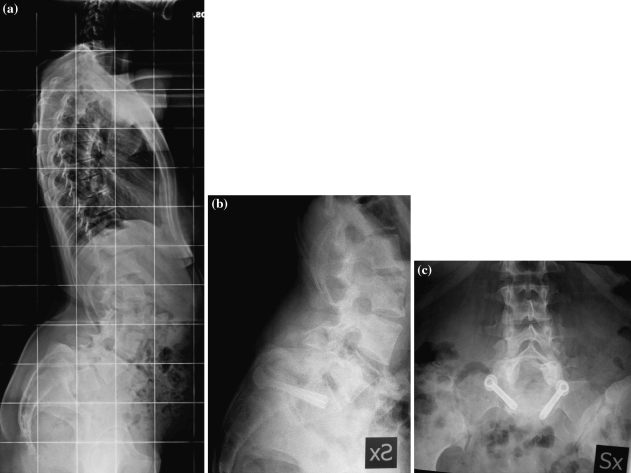
Fig. 1.
L5 HDDS (spondyloptosis) with balanced pelvis (PT = 29°, SS = 53°) (a). After in situ fusion (b–c), the L5 slippage, PT, and SS are almost unchanged
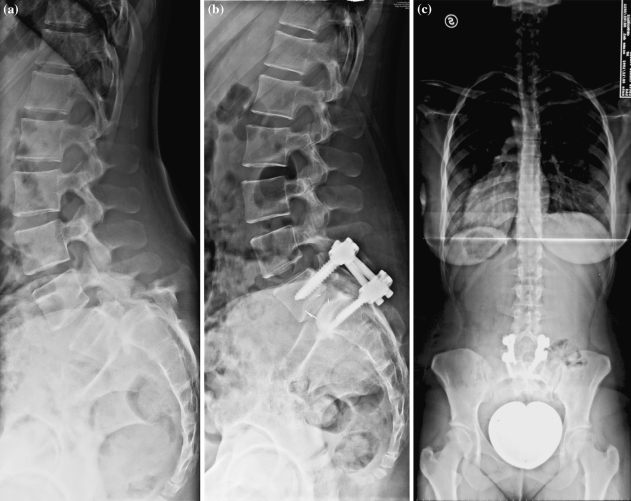
Figure 2a is an example of a patient affected with L5 HDDS (spondyloptosis) and an unbalanced pelvis (high PT and low SS). After surgical reduction (Fig. 2b, c), the most common pattern of changes in spino-pelvic alignment can be observed: the position of L5 over S1 is almost normal with an almost complete reduction of slip, PT is decreased from 42° to 22°, SS is increased from 36° to 55°, while PI is unchanged. The changes at the lumbo-sacral area produce a secondary adaptation of pelvic orientation in the standing position, presumably to maintain a stable posture, with a significant decrease of PT and increase of SS. This change from a retroverted unbalanced to a more balanced pelvic position induces a change in shape of the lumbar spine, which adapts to the new position of the sacrum and of the sacral plate.
Fig. 2.
L5 HDDS (spondyloptosis) with unbalanced pelvis (PT = 42°, SS = 36°) (a). After surgical reduction (b–c), the L5 slippage is almost completely reduced PT is decreased to 22°, and SS is increased to 55°, PI is unchanged
In our series, the PT showed to be the most sensitive parameter of pelvic morphology able to define the effect of surgery in HDDS. In the unbalanced patients, PT is significantly decreased at the follow-up (from 41° to 30°) indicating the reduction of the pelvic retroversion and the improvement in spino-pelvic sagittal balance. Recently, Min et al. [21], performed a retrospective review of 15 consecutive patients who were treated by posterior sacral dome resection and single-stage reduction with pedicle screw fixation for high-grade HDDS. They reported that, after surgery, PI remained unchanged, SS decreased from 51° to 46° and PT increased from 25° to 30°. These results, which are conflicting with our findings, can be related to two main in differences in the two studies. The first difference is that the study of Min et al. has been performed on patients with balanced pelvis, while our series is exclusively composed of unbalanced pelvis. The second difference is that Min et al. performed the surgical resection of the sacral dome to help the reduction of the slipped L5, but, as proposed by Hresko et al. [8], the sacral plate resection should alter the postoperative measurements. Anyway, if a more physiological spino-pelvic balance in HDDS is related to the reduction of pelvis retroversion, necessarily the post-operative PT must be lower and not higher than the pre-operative PT. Moreover, in our opinion, this is also the reason because the first aim of the preoperative planning should be the reduction of the PT and not the reduction of the slippage.
The technique of reduction described in a previous paper [15] meets this requirement. The hyperextension of the hips forces the anterior rotation of the pelvis, pushes the sacrum to be less vertical, reduces the lumbosacral kyphosis, and thus the PT.
Conclusions
Although the long-term role of deformity correction and restoration of spino-pelvic balance in HDDS is yet to be completely defined, the current results allow to clarify two principal aspects of the problem: when the correction of the deformity is necessary, and what should be the surgical strategy to achieve correction. In agreement with Hresko et al. [8], our results show that correction has to be reserved for unbalanced HDDS, while in situ fusion without correction has to be preferred in balanced HDDS. The strategy of correction must be aimed to restore a physiologic spino-pelvic balance, this last is defined not only by the reduction of the L5 slippage, but, above all, by the reduction of the PT, which is the best indicator of pelvic retroversion/anteversion.
Conflict of interest
None.
References
- 1.Akamaru T, Kawahara N, Yoon ST, et al. Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments. Spine. 2003;28:1560–1566. [PubMed] [Google Scholar]
- 2.Boos N, Marchesi D, Zuber K, Aebi M. Treatment of severe spondylolisthesis by reduction and pedicular fixation. A 4–6 year follow-up study. Spine. 1993;18:1655–1661. doi: 10.1097/00007632-199309000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:461–472. doi: 10.1097/00002517-199306060-00001. [DOI] [PubMed] [Google Scholar]
- 4.DeWald RL, Faut MM, Taddonio RF, Neuwrith MG. Severe lumbosacral spondylolisthesis in adolescents and children: reduction and staged circumferential fusion. J Bone Joint Surg (Am) 1981;63:619–626. [PubMed] [Google Scholar]
- 5.Grob D, Humke T, Dvorak J. Direct pediculo-body fixation in cases of spondylolisthesis with advanced intervertebral disc degeneration. Eur Spine J. 1996;5:281–285. doi: 10.1007/BF00301335. [DOI] [PubMed] [Google Scholar]
- 6.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine. 2002;27:2026–2029. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high grade spondylolistheses based on pelvic version and spinal balance: possible rationale for reduction. Spine. 2007;32(20):2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 8.Hresko MT, Hirschfeld R, Buerk A, Zurakowski D. The effect of reduction and instrumentation of spondylolisthesis on spinopelvic sagittal alignment. J Pediatr Orthop. 2009;29:157–162. doi: 10.1097/BPO.0b013e3181977de8. [DOI] [PubMed] [Google Scholar]
- 9.Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after spondylolisthesis. Spine. 2002;27:59–64. doi: 10.1097/00007632-200201010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Johnson JR, Kirwan EO. The long-term results of fusion in situ for severe spondylolisthesis. J Bone Joint Surg (Br) 1983;65:43–46. doi: 10.1302/0301-620X.65B1.6822600. [DOI] [PubMed] [Google Scholar]
- 11.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Hresko T, Chopin D, Dimnet J. Spondylolisthesis, pelvic incidence and sagittal spino-pelvic balance: a correlation study. Spine. 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 12.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5-S1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005;30(6 Suppl):S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 13.Labelle H, Mac-Thiong J, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. 2011;20(Suppl 5):641–646. doi: 10.1007/s00586-011-1932-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamartina C. A square to indicate the unstable zone in severe spondylolisthesis. Eur Spine J. 2001;10(5):444–448. doi: 10.1007/s005860100284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamartina C, Zavatsky JM, Petruzzi M, Specchia N. Novel concepts in the evaluation and treatment of high-dysplastic spondylolisthesis. Eur Spine J. 2009;18(Suppl 1):133–142. doi: 10.1007/s00586-009-0984-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazennec JY, Ramare S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for the 3D regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marchetti PG, Bartolozzi P. Classification of spondylolisthesis as a guideline for treatment. In: Bridwell KH, DeWald RL, editors. The textbook of spinal surgery. 2. Philadelphia: Lippincott-Raven; 1997. pp. 1211–1254. [Google Scholar]
- 19.Mardjetko S, Connolly P, Shott S. Degenerative spondylolisthesis: a meta-analysis of the literature 1970–1993. Spine. 1994;10:2256S–2265S. doi: 10.1097/00007632-199410151-00002. [DOI] [PubMed] [Google Scholar]
- 20.Marty C, Boisaubert B, Descamps H, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Min K, Liebscher Th, Rothenfluh D (2011) Sacral dome resection and single-stage posterior reduction in the treatment of high-grade high dysplastic spondylolisthesis in adolescents and young adults. Eur Spine J 20. doi:10.1007/s00586-011-1949-5 [DOI] [PMC free article] [PubMed]
- 22.Molinari RW, Bridwell KH, Lenke LG, Baldus C. Anterior column support in surgery for high-grade, isthmic spondylolisthesis. Clin Orthop. 2002;394:109–120. doi: 10.1097/00003086-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Moller H, Hedlund R. Surgery versus conservative management in adult isthmic spondylolisthesis: a prospective randomized study: part 1. Spine. 2000;25:1711–1715. doi: 10.1097/00007632-200007010-00016. [DOI] [PubMed] [Google Scholar]
- 24.Poussa M, Schlenzka D, Seitsalo S, Ylikoski M, Hurri H, Osterman K. Surgical treatment of severe isthmic spondylolisthesis in adolescents: reduction or fusion in situ. Spine. 1993;18:894–901. doi: 10.1097/00007632-199306000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation after decompression in spondylolytic spondylolisthesis. Spine. 1997;22:210–219. doi: 10.1097/00007632-199701150-00016. [DOI] [PubMed] [Google Scholar]