Abstract
Purpose
To evaluate and address the safety of vertebroplasty (VP) and kyphoplasty (KP) in terms of rate and type of cement leakage in the treatment of Multiple Myeloma (MM) vertebral fractures.
Methods
A total number of 37 treated vertebrae were evaluated post-operatively by using standard X-rays and CT scan looking for a cement leakage. VP was done using a monoportal approach in all cases (18 treated levels, group A), while KP was done using a monopedicular approach in 9 levels (group B1) and using a bipedicular approach in the remaining 10 levels (group B2). A computed tomography was used to establish the presence of any cement leakage and to determine its localization.
Results
Vertebral augmentation through VP and KP provides immediate pain relief and an improvement of the quality of life of patients affected by MM but it is gravated by high risk of cement leakage. Cement extravasation occurred in 27.7% of total VP procedures and in 21.05% of total KP procedures, but considering the whole number of treated levels, it was more common in multi-level VP and in bipedicular KP, in which a higher quantity of cement was employed.
Conclusions
KP procedure in these patients is slightly less risky but we suggest doing it with a monopedicular approach. It’s mandatory to use an high viscosity cement and we suggest not to use an amount of PMMA over 2 cc and a previous treatment with bone marrow transplant is related to a lower risk of cement leakage.
Keywords: Multiple myeloma, Spine fracture, Vertebroplasty, Kyphoplasty, Cement leakage
Introduction
Multiple myeloma (MM) is a neoplastic disease of B-cell origin, characterized by the accumulation of malignant plasma cells in the bone marrow. Its incidence varies from 2 to 3 per 100,000 among the general population. Bone destruction is the most frequent cause of morbidity and mortality in patients affected by this pathology [1]. Osteolytic lesions found in MM patients are in fact caused by an increased osteoclastic resorption that is not accompanied by a comparable increase in bone formation, leading to an unbalanced bone turnover that causes pathological fractures and severe pain.
Evidences of bone involvement at presentation vary from 70 to 100% of patients [2]. Vertebral involvement can be observed in 60% of cases at the time of diagnosis and is cause of chronic pain, reduction of mobility, spinal deformities, pulmonary and neurological complications [3].
Conservative treatment and radiotherapy alone are usually insufficient to control pain and to restore the integrity and stiffness of the collapsed vertebra [1].
Vertebral augmentation through vertebroplasty (VP) and kyphoplasty (KP) has been recently considered an established operative procedure for the treatment of osteoporotic or traumatic vertebral fractures in order to restore the vertebral body height and to reduce the kyphotic deformity caused by multiple-level vertebral compression fractures. Several authors have reported good results with relatively low complication rates also in multiple myeloma [1, 4, 5].
Cement leakage through the vertebral body boundaries is the most commonly described complication of VP and KP. Cement extravasation can occur through fracture fissures or through the vertebral vein fissures [7, 8]. It is rarely related to clinical manifestations [6], but it can cause neurological symptoms and paraplegia, pulmonary embolism, local or systemic reactions to cement and infections [9, 10]. There is currently little data on the safety of vertebral augmentation in terms of risk of cement leakage in patients affected by metastatic vertebral compression fractures.
The aim of this study is to assess the safety of VP and KP in the treatment of a cohort of 14 patients affected by MM vertebral fractures, through the evaluation of the rate and the type of cement leakage and of the related clinical manifestations.
Materials and methods
From November 2005 to May 2008, 14 patients underwent a surgical treatment for a MM vertebral fracture. The total number of vertebrae was 37, all treated with VP or KP.
The study includes 8 men and 6 women with a mean age of 63 years (range 48–81 years).
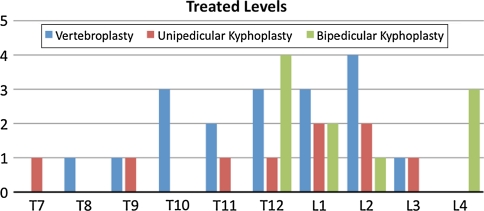
The treated levels were included between T7 and L4, most of the fractures were located at the thoraco-lumbar junction: 43.2% of fractures (16/37) involved the vertebral body of T12 or L1 (Fig. 1).
Fig. 1.
Distribution of the treated levels with reference to the adopted procedure
All patients had an X-Ray, MRI, percutaneous biopsy and all relevant investigations preoperatively. Indication for vertebral augmentation was the presence of a symptomatic vertebral fracture without neurological deficit and a positive MRI signal. All Patients were strictly followed by the hematologists for the further management.
All augmentation procedures were performed in the operating room, under general anesthesia and under fluoroscopic guidance. All cases were treated through the use of acrylic cement, in particular low viscosity polymethylmetacrylate (PMMA) and using the same surgical technique and the same instrumentation. Among all patients six underwent both procedures, six were treated using only KP and two using only VP.
Vertebral augmentation was always performed through a transpedicular approach: vertebroplasty was done using a monoportal technique in all cases (18 treated levels, group A), while kyphoplasty was done using a monopedicular approach in 9 levels (group B1) and using a bipedicular approach in the remaining 10 levels (group B2).
Besides the conventional radiographs in two planes, a computed tomography (CT) of the level of interest was used to establish the presence of any cement leakage and to determine its localization.
Results
In a previous work [11], the results in terms of pain relief, vertebral body height restoration and correction of the kyphotic deformity concerning above described patients have already been published.
Aim of this study is to evaluate the risk of cement leakage in MM patients and to posteriorly analyze it in order to prevent this kind of complication.
Standard post-operative x-rays and a CT scan were employed in order to evaluate the rate of extravertebral cement leakage.
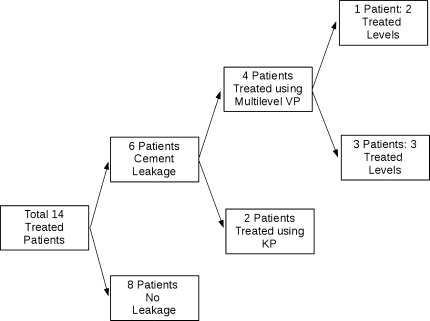
Cement leakage was observed in 6/14 patients (42.9%): 4 of these patients (66.6%) underwent a multilevel vertebroplasty and, in particular, 3 vertebrae were treated in 3 patients and 2 vertebrae in 1 patient (Fig. 2).
Fig. 2.
Flow-chart explaining the percentages of cement leakage considering the whole number of treated patients
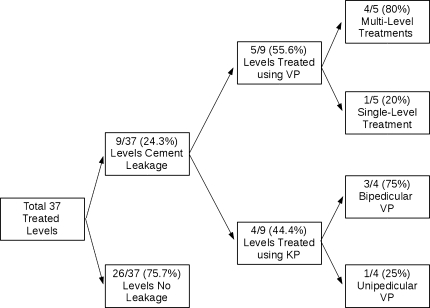
Considering all treated vertebrae, 9/37 levels (24.3%) showed a cement extravasation. Among this percentage, 5/9 levels (55.6%) were treated through VP and 4/5 were multilevel treatments: considering the full sample of VP, the total percentage of procedures that caused a leakage corresponds to 27.7%. 4/9 levels (44.4%) that showed a leakage were treated through KP: 1/4 and 3/4 were treated, respectively, using unipedicular and bipedicular KP (Fig. 3).
Fig. 3.
Flow-chart explaining the percentages of cement leakage considering the whole number of treated vertebrae. The highest risk of cement leakage was observed in monopedicular multilevels VP and in bipedicular KP
Considering the full sample of KP, the total percentage of procedures that caused a leakage corresponds to 21.05%.
Among all the leaking vertebrae, 5/9 were treated using unipedicular vertebroplasty (group A), 3/9 using bipedicular kyphoplasty (group B2) and 1/9 using unipedicular kyphoplasty (group B1).
Cement extravasation involved, after vertebroplasty, the anterior space in two cases and the lateral space in two cases, while after kyphoplasty it involved the anterior space in three cases and the adjacent disk in two cases. No posterior leakage was observed at all. None of these patients had previously been treated with a bone marrow transplant. All cases of cement extravasation were asymptomatic.
Discussion
Skeletal involvement is one of the main causes of morbidity in Multiple Myeloma. Myelomatous osteolytic destruction often affects the spinal column, implying vertebral collapse and severe pain. Because of the increase of survival times due to modern oncologic treatments, a timely intervention to control pain in patients affected by MM vertebral fractures is necessary.
Vertebroplasty (VP) and Kyphoplasty (KP) are minimally invasive procedures used to reduce the intensity of pain and to improve the quality of life of patients affected by osteoporotic vertebral compression fractures. Few papers have reported the results of VP and KP in the treatment of metastatic spine lesions [2, 4, 5].
Leakage of cement after VP and KP may lead to serious complications as embolism and neurological problems as myelopathy and radiculopathy and, in rare cases, death [12, 13].
Few studies about the surgical treatment of osteopenic insufficiency fractures reported a lower risk of cement extravasation during KP: as the cement has to fill an empty cavity created by the inflation of a balloon tamp, its injection can occur at a lower pressure than in VP [14].
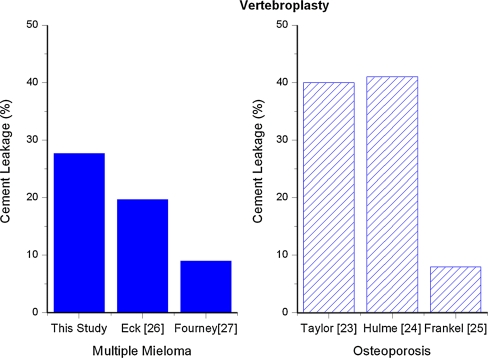
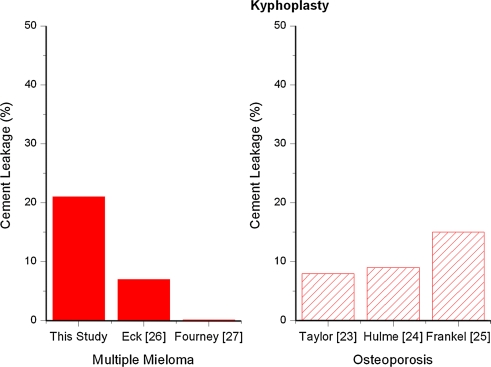
In the review by Taylor et al. [15], cement leakage was significantly higher with vertebroplasty (40%) than with kyphoplasty (8%), and 3% of vertebroplasty leaks were symptomatic whereas no kyphoplasty leaks were reported to be symptomatic. Hulme et al. [16] found similar rates of extravasation for vertebroplasty (41%) and kyphoplasty (9%), with subsequent clinical complications occurring in 3.9 and 2.2% of vertebroplasty and kyphoplasty cases, respectively.
Frankel’s comparative study [17] reported a percentage of cement extravasation that corresponded to 15% of KP cases and 8% of VP cases.
The lack of balance between osteoclastic resorption and bone addition that characterizes MM osteolytic lesions makes the bone structure particularly weak and the risk of cement leakage particularly dangerous. Eck’s work on minimally invasive treatment of spinal tumors showed that cement leakage occurred in 19.7% of VP cases and 7% of KP [18], and Fourney’s study reported a leakage rate corresponding to 9% of VP and 0% of KP procedures [19].
Nevertheless, Kose’s comparative study [20] recorded no cement leakages in patients treated with either KP or VP.
Figures 4 and 5 compare the percentages of cement leakage in MM and in osteoporosis respectively during VP and KP as reported in the literature.
Fig. 4.
Percentages of cement leakage in MM and in osteoporosis during VP as reported in the literature
Fig. 5.
Percentages of cement leakage in MM and in osteoporosis during KP as reported in the literature
According to this data, in our study cement extravasation occurred in 27.7% of total VP procedures and in 21.05% of total KP procedures.
Even if our results show a little advantage for KP, it should be stated that, considering all treated levels, the highest percentage of leakage (44.4%) was found in multi-level VP. This result could be mostly done by the pathology’s severity, that increases when MM involves more levels, but there should be also a technical problem done by the fact that the surgeon, trying to use a single dose of PMMA to treat multiple levels, injects the cement at higher pressure.
Among patients who underwent a multi-level VP that showed a leakage, none had previously been treated with a bone marrow transplant. Differently, patients that underwent a multi-level treatment who had previously been treated with bone marrow transplant did not show any leakage: an enhanced control of the pathology is therefore probably related to a lower risk of cement leakage.
Considering the rate of KP procedures that showed a cement extravasation, the highest percentage of leakage (33.3%) was found in bipedicular KP, while monopedicular KP showed a leakage in 11.1% of cases, that is the lowest percentage of leakage considering the whole number of treated levels. The high rate of PMMA extravasation in bipedicular KP could be caused by the higher quantity of inserted cement: in fact, in monoportal KP a total quantity of 2 cc of PMMA was used, while biportal KP implied the use of at least 3 cc of PMMA (Figs. 6, 7, 8, 9). This could prove a correlation between the quantity of used cement and the risk of its leakage.
Fig. 6.
Preoperative X-rays of a patient with multiple pathological fractures at the thoraco-lumbar junction (T12-L1-L2)
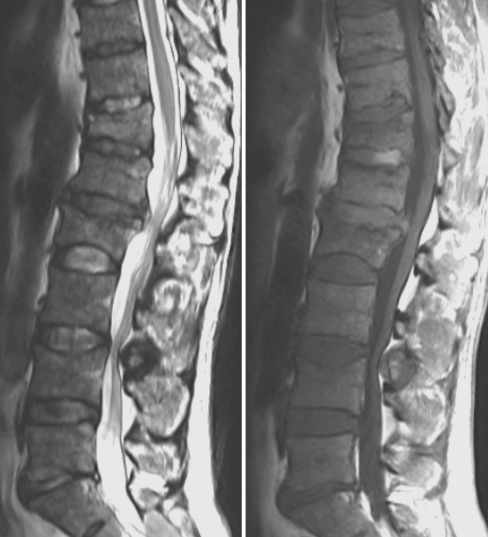
Fig. 7.
MRI scan with T1 and T2 weight images
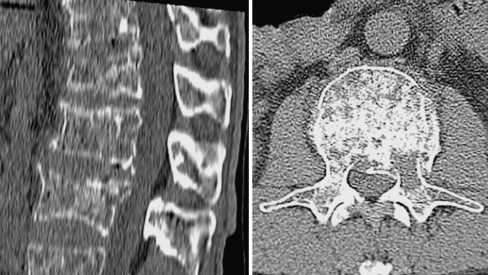
Fig. 8.
CT scan showing the severe bone destruction observed during multiple myeloma involvement
Fig. 9.
Postoperative X-rays after the KP procedure done with a bipedicular approach. There is a cement leakage within the disc above L2
The cement employed in this work was a first generation low viscosity PMMA, and this could be another reason for the high rate of cement leakage we observed: cement thickness is in fact a key feature in controlling the intravertebral cement filling. An experimental study [21] compared cement leakage and filling behavior of two existing delivery systems, respectively characterized by high viscosity and low viscosity: superior results were obtained with the high-viscosity system that showed an increase of filling uniformity and a reduction of cement leakage.
Different techniques can be used to prevent leakage; in addition to the use of high viscosity cement, radiopaque substances, as tungsten, tantalum powder, barium sulphate or zirconium dioxide can be added to PMMA in order to facilitate fluoroscopic visualization to monitor possible cement extravasation [22]. Another of these techniques is the eggshell procedure, during which, after the reduction with the KP balloon, a small amount of doughy cement is injected into the cavity, and then the balloon reinserted and reinflated: once the cement hardens, the cavity can be filled with cement, whose leak is prevented by the eggshell structure [23].
None of these techniques was employed in this study.
As regards the localization of cement extravasation, an interesting work [24] analyzed postoperative CT scans of patients that underwent VP for osteoporotic compression fractures and classified the patterns of leakage into three groups: those through the basivertebral vein (type B), via the segmental vein (Type S) and through a cortical defect (type C). Type B leaks proceed via the vascular foramen and in the spinal canal; they spread along the epidural venous plexus. Type S leaks usually proceed horizontally, along the segmental veins and they can reach the neural foramina. Type C leaks may invade any area through a cortical defect, including the disc space, the spinal canal, the neural foramen and outside the vertebra. In this study, all leakages were interpreted as type C leaks, occurred through a cortical defect, and none of them involved the spinal canal. This can be explained considering that the injection of cement into such a fragile and compromised vertebral body easily creates fissures through which cement leaks.
In our study, cement extravasation was always asymptomatic and involved the anterior space in two cases and the lateral space in two cases after VP, while it involved the anterior space in three cases and the adjacent disc in two cases after KP. Leaks into the adjacent disc space occurred only after KP, and never after VP suggesting a possible implication of the inflated balloon tamp in the genesis of this kind of extravasation.
Conclusions
Even if vertebroplasty shows a slightly higher rate of leakage, the poor quality of bone in MM, the necessity of a multi-level treatment and the use of a higher quantity of cement seem to influence the risk of cement leakage more than the choice of one or the other technique.
The higher risk of cement extravasation and complication is in patients treated with multilevel vertebroplasty and untreated with bone marrow transplant (44.4%), while the lower risk is in monoportal kyphoplasty (11.1%).
Kyphoplasty procedure in these patients is slightly less risky but we suggest to do it with a monopedicular approach and to place the balloon as much as possible in the center of the vertebral body in order to avoid an accidental injury of the upper vertebral body plate.
It is mandatory to use high viscosity cement and we suggest not using an amount of PMMA over 2 cc because in our hands it is associated with a higher risk of leakage.
In summary, VP and KP appear to be safe procedures in the treatment of MM vertebral lesions but, considering the remarkable fragility of the bone in MM, it is important to meticulously evaluate the surgical indication before the procedure, in order to avoid any possible posterior leakage.
A previous treatment with bone marrow transplant and, therefore, an enhanced control of MM, is related to a lower risk of cement leakage.
Conflict of interest
None.
References
- 1.Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12(20, Pt. 2):6243S–6249S. doi:10.1158/1078-0432.CCR-06-0931 [DOI] [PubMed]
- 2.Dudeney S, Lieberman IH, Reinhardt MK, et al. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol. 2002;20(9):2382–2387. doi: 10.1200/JCO.2002.09.097. [DOI] [PubMed] [Google Scholar]
- 3.Lecouvet FE, Vande Berg BC, Maldague BE, et al. Vertebral compression fractures in multiple myeloma. Distribution and appearance at MR imaging. Radiology. 1997;204:195–199. doi: 10.1148/radiology.204.1.9205246. [DOI] [PubMed] [Google Scholar]
- 4.Astolfi S, Scaramuzzo L, Logroscino CA. A minimally invasive surgical treatment possibility of osteolytic vertebral collapse in multiple myeloma. Eur Spine J. 2009;18(Suppl 1):S115–S121. doi: 10.1007/s00586-009-0977-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald RJ, Trout AT, Gray LA, et al. Vertebroplasty in Multiple Myeloma: outcomes in a large patient series. Am J Neuroradiol. 2008;29:642–648. doi: 10.3174/ajnr.A0918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kayanja MM, Schlenk R, Togawa D, et al. The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments. Spine. 2006;31:769–774. doi: 10.1097/01.brs.0000207466.40955.31. [DOI] [PubMed] [Google Scholar]
- 7.Choe DH, Marom EM, Ahrar K, et al. Pulmonary embolism of polymethylmethacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004;183:1097–1102. doi: 10.2214/ajr.183.4.1831097. [DOI] [PubMed] [Google Scholar]
- 8.Stoffel M, Wolf I, Ringel F, et al. Treatment of painful osteoporotic compression and burst fractures using kyphoplasty: a prospective observational design. J Neurosurg Spine. 2007;6:313–319. doi: 10.3171/spi.2007.6.4.5. [DOI] [PubMed] [Google Scholar]
- 9.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 10.Kalteis T, Luring C, Gugler G, et al. Acute tissue toxicity of PMMA bone cements. Z Orthop Ihre Grenzgeb. 2004;142:666–672. doi: 10.1055/s-2004-832317. [DOI] [PubMed] [Google Scholar]
- 11.Maida GA, Sala F, Callea G, et al. Efficacy of unipedicular balloon kyphoplasty for treatment of multiple myeloma vertebral lesions. Asian Spine J. 2011;5(3):162–168. doi: 10.4184/asj.2011.5.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hiwatashi A, Ohgiya Y, Kakimoto N, et al. Cement leakage during vertebroplasty can be predicted on preoperative MRI. Am J Roentgenol. 2007;188:1089–1093. doi: 10.2214/AJR.06.0903. [DOI] [PubMed] [Google Scholar]
- 13.Bouza C, Lopez T, Magro A, Navalpotro L, Amate JM. Efficacy and safety of balloon kyphoplasty in the treatment of vertebral compression fractures: a systematic review. Eur Spine J. 2006;15:1050–1067. doi: 10.1007/s00586-005-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCall T, Cole C, Dailey A. Vertebroplasty and kyphoplasty: a comparative review of efficacy and adverse events. Curr Rev Musculoskelet Med. 2008;1:17–23. doi: 10.1007/s12178-007-9013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine. 2006;31:2747–2755. doi: 10.1097/01.brs.0000244639.71656.7d. [DOI] [PubMed] [Google Scholar]
- 16.Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 17.Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007;7(5):575–582. doi: 10.1016/j.spinee.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Eck JC, Nachtigall D, Humphreys SC, et al. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008;8:488–497. doi: 10.1016/j.spinee.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Fourney DR, Schomer DF, Nader R. Percutaneous vertebroplasty and kyphoplasty for painful vertebral fractures in cancer patients. J Neurosurg. 2003;98:21E2–30E2. doi: 10.3171/spi.2003.98.1.0021. [DOI] [PubMed] [Google Scholar]
- 20.Kose KC, Cebesoy O, Akan B, Altinel I, Dincer D, Yazar T. Functional results of vertebral augmentation techniques in pathological vertebral fractures of myelomatous patients. J Natl Med Assoc. 2006;98:1654–1658. [PMC free article] [PubMed] [Google Scholar]
- 21.Habib M, Serhan H, et al. Cement leakage and filling pattern study of low viscous vertebroplastic versus high viscous confidence cement. SAS J. 2010;4:26–33. doi: 10.1016/j.esas.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lieberman IH, Togawa D, et al. Vertebroplasty and kyphoplasty: filler materials. Spine J. 2005;5:305S–316S. doi: 10.1016/j.spinee.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 23.Greene DL, Isaac R, Neuwirth M, et al. The eggshell technique for prevention of cement leakage during kyphoplasty. J Spinal Disord Tech. 2007;20:229–232. doi: 10.1097/01.bsd.0000211276.76024.30. [DOI] [PubMed] [Google Scholar]
- 24.Yeom JS, Kim WJ, Choy WS, et al. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg (Br) 2003;85-B:83–89. doi: 10.1302/0301-620X.85B1.13026. [DOI] [PubMed] [Google Scholar]