Abstract
Introduction
Posterior dynamic stabilisation (PDS) aims at relieving lumbar discogenic pain and preserving adjacent levels from accelerated degeneration.
Purpose
To evaluate the results of a novel PDS system in 32 adult patients affected by chronic low back pain (CLBP) due to degenerative lumbar spine instability (DLSI).
Method
A progressive follow-up for 12 months of 32 patients, with collection of complete clinical (ODI and VAS back + leg) and radiological data (resting + functional radiographs and MRI).
Results
Mean ODI scores improved from 49 to 6%, VAS back from 5 to 1 and VAS leg from 7 to 2. Twenty-two patients underwent fusion of a lower lumbar segment and stabilisation of an upper segment (hybrid fusion) whereas ten underwent dynamic stabilisation. In 16/32 patients, decompression was added to treat radicular pain. Motion in non-fused instrumented levels was unrestricted on functional X-rays and MRIs did not show significant morphologic changes. Four patients (12.5%) had unchanged functional and pain scores while two (6.3%) suffered worsening low back pain necessitating implant removal and spinal fusion. No infection, no new neurologic deficit or implant failure was recorded.
Conclusions
The 1 year follow-up shows that the tested PDS system is able to provide a significant improvement in pain and disability scores when applied to patients affected by DLSI. The system does not provide better clinical results when compared to similar trials on posterior fusion. Further follow-up is ongoing to investigate the potential preservation of adjacent levels from accelerated degeneration.
Keywords: Lumbar spine, Instability, Degenerative discopathy, Dynamic stabilisation, Spinal fusion
Introduction
Disc degeneration is a natural process coupled with ageing of the human spine. The degenerative cascade progresses along many stages. It is thought to begin with dehydration of the intervertebral disc along with a decrease in the tensile modulus of the annulus fibrosus. This is followed by a corresponding loss of disc height that can lead to posterior facet joint subluxation (i.e., retrolisthesis) and to an abnormal pattern of motion causing segmental instability [11]. Subsequent to the instability phase, the spine in time undergoes major anatomical changes such as hypertrophy of the ligamenta flava and of the facet joints that tend to stiffen and re-stabilise it [6]. The standard of care for the surgical treatment of symptomatic degenerative lumbar spine instability (DLSI) has long been spinal fusion with or without instrumentation [1]. Nevertheless, the damaging effects of lumbar fusion are regularly commented, and are probably due to excessive mechanical stress on either side of the fusion area. Spinal fusion can have long-term effects on non-fused segments and impose considerable postural stress on levels above or below the fusion area [3]. Although fusion of one or two vertebrae does not significantly alter the global range of motion of the spine, it can have significant kinematic consequences at segments adjacent to the fusion itself [10, 12]. Five years following a lumbar fusion, adjacent level degeneration is most commonly seen cranial to a fusion and can reach a reported incidence of as high as 89% [2]. Complications related to spinal fusion are also not uncommon and include painful pseudarthrosis, adjacent stenosis, junction degeneration, donor site morbidity and fatigue failure of the implant [5, 8]. Recent advances in fusion techniques have elevated arthrodesis rates, without an equivalent improvement in relief of pain [1]. Some authors [9] reckon that the primary mechanism underlying the development of chronic low back pain (CLBP) is due to abnormal load distribution across the disc space following disc degeneration. Quantity of motion does not seem to be the cause of pain, but quality does. Abnormal direction or translation of the moving spinal unit may produce pain by causing abnormal distribution of load across the disc and the vertebral endplates [16]. Current research by spine specialists is focussed on a more physiological surgical approach in order to preserve movement, and non-fusion systems have been gaining popularity. The goal of dynamic stabilisation is to stabilise the motion segment with motion preservation [7, 15, 16, 19]. Posterior dynamic stabilisation (PDS) is based on the premise that the implant can restore functional stability while maintaining some or all of segmental motion [10]. In this way, PDS devices are thought to reduce or eliminate the incidence of adjacent level degeneration and to relieve discogenic pain by altering the transmission of abnormal loads through the degenerated disc [14]. The Flex-Plus Spinal System (FPSS, Spine Vision, Paris France) is a screw system conceived and designed to either perform a dynamic re-stabilisation while preserving the disc as well as the facet joints (dynamic neutralisation) or to join a fusion area to a dynamic one on top of it (hybrid fusion). FPSS has been tested on finite elements [19]; but as of date, to our knowledge it has not been the subject of a clinical investigation. The aim of the present study is to present and discuss the 1 year follow-up clinical results and complications correlated with the use of FPSS in a cohort of adult patients treated for CLBP due to DLSI and prospectively followed up at a single tertiary referral institution for spinal disorders.
Materials and methods
Study design
From February 2008 to March 2009 a consecutive series of patients affected by CLBP due to DLSI and lasting over at least 6 months of continuous conservative care were recruited to participate in a study of surgical treatment with FPSS. After approval of the institutional ethical committee and informed consent, one orthopaedic surgical team of a tertiary referral spinal centre treated the enrolled patients. All patients were operated on by the same surgeon. The study is ongoing and follow-up is scheduled until the 30th month after surgery. All patients were Italian residents. Inclusion criteria were: back pain and/or radicular pain resistant to conservative therapy for at least 6 months, age between 25 and 65 years, degenerative lumbar spine instability at 1 or 2 levels as suspected by clinical and measured by radiological analysis [17, 19]. Exclusion criteria were: previous lumbar surgery, rheumatic disease, infection, tumour, obesity (body mass index >30%) and osteoporosis (bone density scan values <2.5 SD compared to normal for the age). After selection of patients, two treatment groups resulted. Group 1 received a dynamic re-stabilisation procedure with elastic rods and four pedicle screws over one motion segment (Fig. 1a–g) because of a single level disease. Group 2 received a hybrid fusion procedure with hybrid (rigid at the bottom, elastic at the top) rods and six pedicle screws over two motion segments (Fig. 2a–l) because of a two-level disease. In both groups, a decompression procedure (laminotomy or discectomy) was added when indicated by the presence of radicular pain. Clinical results were evaluated with ODI 2.1 and VAS scales for back and leg pain [18] preoperatively, at 4 and at 12 months follow-up. Prior to surgery, all patients underwent standard X-ray, functional X-ray and MRI of the lumbar spine. Standard X-rays were also obtained 4 months after surgery and at 12 months follow-up. Functional X-rays plus MRI were obtained after 1 year from surgery. The evaluation of the fusion rate in Group 2 was made according to Christensen’s criteria [4] at 1-year follow-up on standard X-rays. The assessment of movement in the dynamic stabilisation areas (whether in Group 1 or 2) was evaluated on functional X-rays at 1-year follow-up [6, 10, 15–17]. The degenerative grade of each lumbar disc was assessed from conventional T2-weighted images according to the Pfirmann’s classification system before surgery and at 1-year follow-up [13].
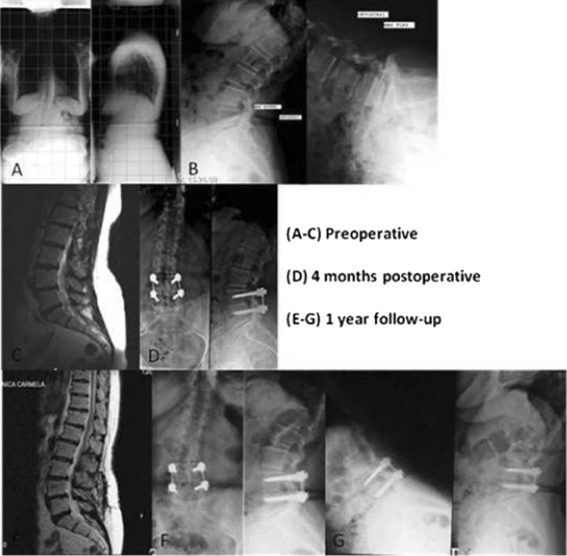
Fig. 1.
Radiographic set of a case treated with dynamic stabilisation for a single level disease
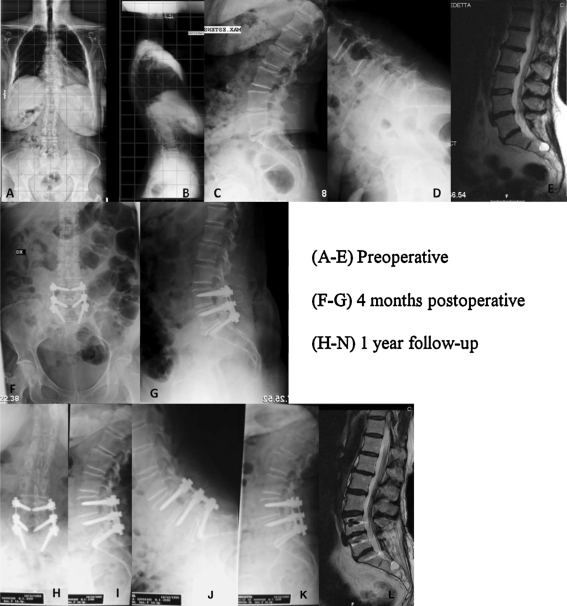
Fig. 2.
Radiographic set of a case treated with hybrid stabilisation for a two-level disease
Operative technique and postoperative care
All patients were operated on under general hypotensive anaesthesia in prone position on a spinal frame. In 16/32 (50%) patients a standard median approach was performed, because spinal canal decompression was necessary. In the remaining 16 patients, a Wiltse-type approach was performed [1, 10, 15]. After exposure of the posterior vertebral anatomy, pedicle screws were inserted with a free-hand technique with the aid of bi-planar fluoroscopy. FPSS features top loading mobile head 5.5, 6.5 and 7.5 mm diameter titanium pedicle screws and two types of 5.5 mm diameter rods: multiple titanium fibre woven elastic rods with a polycarbonate-urethane sheet and hybrid rods with a proximal rigid titanium part and a distal elastic part. In all patients, 6.5 mm diameter titanium screws were applied. Next, two parallel elastic rods of appropriate length were applied and secured to the screw heads in Group 1, while two hybrid rods were used in Group 2. The system was tightened with the set preload. No further distraction or lordosis was applied to the segment, and no attempt to reduce the spondylolisthesis was made. Decompression of the spinal canal was undertaken when needed with preservation of over 50% of each facet joint. Autologous bone graft harvested from the iliac crest was added at the bottom level postero-laterally in Group 2. Finally, the wound was closed in layers over a suction drainage that was left in place for 24 h. Antibiotic prophylaxis with a first generation intravenous cephalosporin (2 g) was started before surgery and discontinued after 36 h (1 g/12 h). Deep venous thrombosis prophylaxis was started with a fractioned heparin on the evening before surgery and discontinued after 4 weeks. Patients were mobilised and encouraged to walk with a soft brace after removal of the wound drain or as soon as general conditions allowed. Discharge home was allowed as soon as patients were independently caring for themselves and pain had become tolerable on oral analgesia. All patients wore a lumbar orthosis for 8 weeks.
Statistical methods
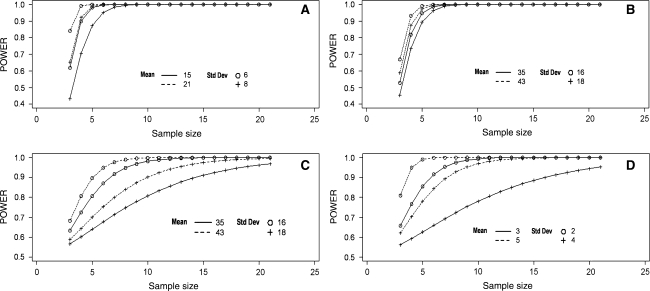
An orthopaedic spinal surgeon not involved in the care of patients (MT) independently reviewed the clinical and radiographic data. A professional statistician performed the statistical analysis. Descriptive statistics of position (mean and median) and dispersion (standard deviation and range) were used for all analysis variables. The evaluation of normal fitting was performed with the Kolmogorov–Smirnoff (KS) test. The use of a t test or a non-parametric approach was conditioned by the KS test results. Because of a strong dispersion in the data, non-parametric tests were chosen for all variables. The reduction of scores (ODI 2.1 and VAS for leg and back pain) was evaluated by a Wilcoxon signed rank for one sample test. The p values lower than 0.05 were considered significant. The non-parametric Mann–Whitney U test was applied to all variables for comparison between Groups 1 and 2. All analyses were performed by SAS software package version n 9.1.3 (SAS Institute Inc SAS 9.1.3 help and documentation, Cary, NC: SAS Institute Inc 2000–2004). Statistical power assessment was performed a posteriori using sampled parameters (sample mean and sample standard deviation) from our survey. The PROC POWER of SAS software package was used to evaluate the relation of the test power with sample size under the assumption of a normal distribution of the parameters using a range for means and standard deviations that included the sample estimates (Fig. 3).
Fig. 3.
Statistic evaluation
Results
Cohort and group results
32 patients were enrolled and 31 (96.9%) (6 males and 25 females, ratio = 1:4) with a mean age at surgery of 48 years (range 29–61) completed the first 12 months follow-up period. One patient (3.1%) was dropped-out because he refused to participate further. He had undergone a reoperation after 6 months from the index surgery because of increasing CLBP. His FPSS was removed and a spinal fusion was performed. Table 1 displays the demographics of the two treatment groups including levels and type of spinal disease. No variables were significantly different among groups that were as a consequence deemed comparable. In the study cohort (32 patients), back pain and sciatica were present in 16 cases (50%) and back pain only in 16 (50%) patients. The duration of symptoms averaged 12 months (range 6–23). On plain X-rays of the lumbosacral spine a spondylolisthesis of 15% was observed in 20 cases (62.5%), instability on functional X-rays of the lumbar spine in 30 (93.8%) and scoliosis in 10 (31.3%). After stratification per group, these figures were not statistically different and the groups were deemed comparable. Outcome variables are summarised in Table 2. VAS scales for back and leg did not show significant differences among groups throughout follow-up, nor did ODI scores. VAS and ODI scores improved significantly within groups and showed a higher than minimal clinically important difference (MCID, 30%) [18] between preoperative and 4 months postoperative scores that was maintained through follow-up. Post hoc power analysis showed that the sample size was adequate to perform a paired comparison of scores. With 32 subjects and under the assumption of a normal distribution of scores, statistical power exceeded the value of 0.8 (80% of power). Hospital stays averaged 4.2 days in Group 1 and 4.5 days in Group 2 (p = 0.03).
Table 1.
Patients’ demographics (mean ± SD)
| Group 1 | Group 2 | p | |
|---|---|---|---|
| Age (years) | 51 | 52.3 | 0.3 |
| F-up (months) | 12 | 12 | – |
| Sex (M:F) | 1:4 | 2:9 | 0.5 |
| Level of instability | L2–3 (2 cases); L4–5 (8 cases) | L4–S1 (22 cases) | – |
| Type of instability | Degenerative | Degenerative | – |
| Number of cases | 10 | 22 | 0.8 |
Table 2.
Outcome measures (mean ± SD)
| Cohort | Group 1 | Group 2 | p | |
|---|---|---|---|---|
| VAS, leg (preop/12 months) | 4.8/0.9 | 3.5/0.5 | 5.3/1.1 | 0.2 |
| VAS, back (preop/12 months) | 7.3/1.7 | 5.3/0.8 | 7.7/1.8 | 0.4 |
| ODI 2.1 (preop/12 months) % | 48.8/10 | 39/3 | 50.2/14.6 | 0.1 |
Adverse events
We did not record any case of death, cardiac or pulmonary adverse event, surgical infection or newly developing neurology in the study cohort. One female patient described above required removal of the implant and spinal fusion after 6 months, but her follow-up data does not surpass the 4 month postoperative control because she refused to participate further. A further female patient had persistent painful symptoms along with an outbreak of depressive symptoms after surgery. The objective clinical and radiographic evaluation data were within expected limits at 4 and 12 months follow-up. In this case, we chose not to treat the patient surgically and referred her for specialist advice.
Radiologic findings
In 8/32 (25%) cases, we observed a reversal of Pfirmann grading from 4 to 3, with evidence of rehydration from the posterior portion of the disc. In Group 1, at 4 and 12 months follow-up standing X-ray showed maintenance of the preoperative sagittal and coronal alignment. Functional X-rays showed reversed features of instability with translation of operated vertebrae reduced to up to 50% of the preoperative values (Fig. 1). Similarly, in Group 2, the elastic portion of the hybrid fusion did show reversal of the instability features. A postero-lateral spinal fusion mass that was judged a fusion was detected in all fused segments (Fig. 2). There were no signs of radiolucency of the implanted screws or signs of system fatigue. At 12 months follow-up, the intervertebral discs in the dynamic stabilisation at MRI showed in all cases a blocking of the degeneration process.
Discussion
Main findings
In the present prospective study, the first to test FPSS in the treatment of lumbar spine degenerative instability, patients had clinically and statistically significant improvements in VAS and ODI scores in both the dynamic and the hybrid group, as an objective measure of the success of treatment. Nevertheless, 4/32 (12.5%) patients did not show clinical improvements, thus making the results of this study comparable with those of similar ones reporting on outcomes of posterior spinal fusion for discogenic instability [1, 5, 6, 8] and of dynamic stabilisation for degenerative spondylolisthesis [10, 15]. BMI, age, gender, co-morbidities and duration of symptoms had no influence on patient outcome.
Features of the study
For this trial, sample size calculations were carried out in order to ensure that clinically relevant changes would be detected (Table 1). The results of this prospective study are limited by the sample size—with a 3.1% dropout rate thus far—and by the length of follow-up. This necessarily hides future effects on adjacent segment degeneration and potential disc rehydration and will need further reports as the study is ongoing. Mean hospital stay in our series was comparable to similar series on both posterior fusion [1, 5, 6, 8] and stabilisation surgery [10, 15].
Technical considerations
From a subjective point of view, surgeons did not judge handling and ease of use of the FPSS system differently from those of most pedicle screw spinal stabilisation and fusion systems available on the market, in that the size of the implant negatively affects the ability to perform a spinal canal decompression.
Complications: types and rates
UK’s National Institute for Health and Clinical Excellence (Interventional Procedure Guidance 183) suggested in 2006 that current evidence on the safety of non-rigid stabilisation procedures is unclear and involves a variety of different devices and outcome measures. Therefore, these procedures should only be used with special arrangements for consent and for audit or research. This study investigated one of the systems that were recently introduced to the European market in a standardised protocol. In this setting, FPSS gave a 12.5% failure rate, i.e., was not able to provide clinical improvements as measured by VAS and ODI scores. FPSS did not show mechanical failures at 12 months but again this needs a longer audit to be validated. This data compares well with similar literature [5, 6, 10, 15].
In summary, FPSS proved safe enough to be used in surgical patients affected by lumbar spine instability. At an average follow-up of 12 months, FPSS was able to provide significant improvements in disability and pain scores with a reasonable percentage of complication, without showing any significant difference from similar series on stabilisation or fusion surgery for similar diseases. UK’s National Institute for Health and Clinical Excellence (Interventional Procedure Guidance 183) concluded in 2006 that “limited evidence suggests that non-rigid stabilisation procedures for the treatment of low back pain provide clinical benefit for a proportion of patients with intractable back pain”. This study adds 12 months’ prospective data on the issue and is designed to add further data as follow-up is ongoing.
Conflict of interest
None.
References
- 1.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6:2–18. doi: 10.1007/BF01676569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chou WY, Hsu CJ, Chang WN, et al. Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg. 2002;122:39–43. doi: 10.1007/s004020100314. [DOI] [PubMed] [Google Scholar]
- 3.Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine. 2007;32:2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 4.Christensen FB, Laursen M, Gelineck J, et al. Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detalied classification system in posterolateral spinal fusion. Spine. 2001;1:538–543. doi: 10.1097/00007632-200103010-00018. [DOI] [PubMed] [Google Scholar]
- 5.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18:2231–2239. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Friberg O. Lumbar instability: a dynamic approach by traction-compression radiography. Spine. 1987;12(2):119–129. doi: 10.1097/00007632-198703000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Lazennec JY, Ramare S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McAfee PC, Weiland DJ, Carlow JJ. Survivorship analysis of pedicle spinal instrumentation. Spine. 1991;16(suppl 8):S422–S427. [PubMed] [Google Scholar]
- 9.Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002;11:S198–S205. doi: 10.1007/s00586-002-0422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nockels RP. Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine. 2005;30:S68–S72. doi: 10.1097/01.brs.0000174531.19982.99. [DOI] [PubMed] [Google Scholar]
- 11.Panjabi M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5:390–398. doi: 10.1097/00002517-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Panjabi MM. Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech. 2007;22:257–265. doi: 10.1016/j.clinbiomech.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Pfirmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26(17):1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Schmoelz W, Huber JF, Nydegger T, et al. Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech. 2003;16:418–423. doi: 10.1097/00024720-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 16.Sengupta DK, Mulholland RC. Fulcrum assisted soft stabilization system: a new concept in the surgical treatment of degenerative low back pain. Spine. 2005;30(9):1019–1029. doi: 10.1097/01.brs.0000160986.39171.4d. [DOI] [PubMed] [Google Scholar]
- 17.Stokes I, Frymoyer J. Segmental motion and instability. Spine. 1987;12:68–91. doi: 10.1097/00007632-198709000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Zanoli G. Outcome assessment in lumbar spine surgery. Acta Orthop Suppl. 2005;76(318):5–47. [PubMed] [Google Scholar]
- 19.Zhang QH, Zhou YL, Petit D, et al. Evaluation of load transfer characteristics of a dynamic stabilization device on disc loading under compression. Med Eng Phys. 2009;31(5):533–538. doi: 10.1016/j.medengphy.2008.09.011. [DOI] [PubMed] [Google Scholar]