Abstract
Objective
To test the Sociocultural Health Behavior Model in relation to the health behavior of prostate cancer (PCa) screening among Chinese American men.
Methods
Confirmatory factor analysis and structural equation model analyses were conducted among Chinese American men.
Results
The path analysis supported the components of the sociocultural model and indicated a positive and significant relationship between PCa screening and the enabling factors; between cultural factors and predisposing, enabling, and access/satisfaction with health care factors; and between enabling factors and access/satisfaction with health care.
Conclusions
The model highlights the significance that sociocultural factors play in relation to PCa screening.
Keywords: digital rectal exam, prostate specific antigen (PSA) blood test, prostate cancer screening, structural equation model
Prostate cancer (PCa) is the second leading cause of cancer deaths among men in the United States and the sixth leading cause of death overall.1 The American Cancer Society recommends that beginning at age 50, a prostate-specific antigen blood test (PSA) and digital rectal examination (DRE) should be offered to men annually.2 Although it remains controversial,3 due to insufficient evidence to recommend for or against screening,4,5 screening appears to be effective in reducing mortality from PCa, especially if screening and treatment are freely available to all patients.6
In Asian countries, the reported incidence rate and its subsequent mortality have been on the rise.7 For example, a 118% increase has been reported among Singaporean Chinese men.7 The PCa incidence and mortality rates are 104.2/100,000 and 11.8/100,000, respectively, among Asian men in the United States.8 Compared with Asian men in their native countries, Asian American men have increased PCa rates.9 With acculturation, many Asian Americans may be losing their cultural protective factors and acquiring high-risk ones. Although studies have examined the relationship between risk factors and PCa, there are few PCa screening studies among Asian American men or its subgroups to examine factors associated with PCa screening. The available data suggest that the uptake of PCa screening is very low in Asian American men, with more than three-quarters (78%) reporting never-screened.10 As found in other cancer prevention studies for Asian Americans, the major limitation in understanding the PCa prevention includes a lack of sufficient data from representative samples. Some studies adopted data from national surveys that did not include Asian American native speakers, leading to a biased estimate of cancer screening rates among this population.11
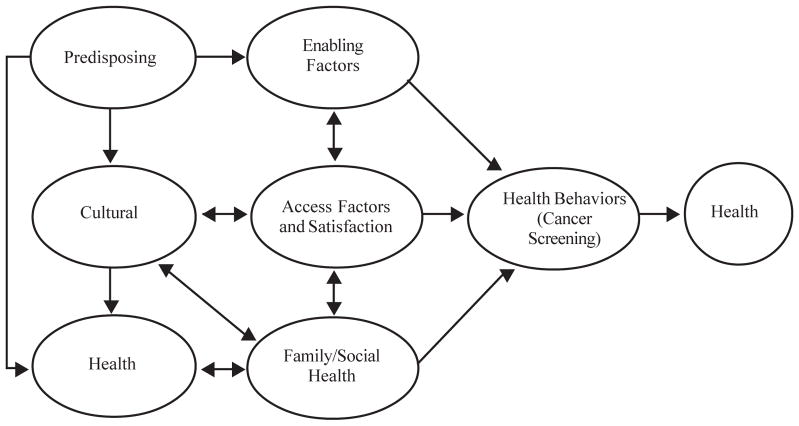
Ma et al developed a theoretical model, called the Sociocultural Health Behavior Model, to examine people’s health behavior for cancer screening practice (Figure 1)12 The model was developed by incorporating the major constructs of the Health Belief Model,13 social cognitive theory,14 the behavioral model, and access to medical care.15 The proposed theoretical model also acknowledges that the complexity and interaction of multiple factors play a major role in people’s health-seeking behaviors. The Sociocultural Health Behavior Model stresses the interrelationships among individual, interpersonal, and environmental factors. This model examines relationships between individual health behavior and interaction with the environment. The interactions and multiple levels of influence of individual, interpersonal, and environmental factors underlying the health behavior are emphasized in an ecological model. The model has been successfully used to explain hepatitis B screening behavior among Chinese Americans.12
Figure 1.
Sociocultural Health Behavior Model
Figure 1 illustrates how the Sociocultural Health Behavior Model explains health behavior. In addition to common theoretical components, this model includes cultural factors as a primary component. The model incorporates the interdependence of predisposing, enabling, need, family/social support, environmental health system, and cultural factors, all of which contribute to a particular health behavior or outcome. A number of variables can be included under cultural factors, including notions of fatalism, birth in the United States, years lived in the United States, English fluency, use of native language at home, frequency of eating native food, use of media sources in native language, and attendance at native social events.
Structural equation modeling has been used in studies related to health problems, including motivation and risk for prostate cancer screening.16–20 Structural equation modeling offers some advantages in examination of factors in the cultural and ecological approaches.21 The structure of relationships among a set of factors can be tested;22 there is increased statistical control over random measurement error and measurement biases21; and examination of interrelated constructs can occur without the disadvantages of a multivariate analysis of covariance approach.23 Because screening behavior is influenced by multiple factors, there is a need to identify these interrelationships and pathways among these factors. Often, the role of cultural factors is rarely included in health behavior analysis.
The purpose of this study was to validate the proposed Sociocultural Health Behavior Model by using a structural equation analysis to determine the direction and magnitude of the interdependence of the proposed components of the model in relation to the health behavior related to PCa screening among Chinese American men. Chinese is the largest ethnic group among Asian Americans, representing 24%,24 and yet there is lack of studies with regard to their behavior in PCa screening. It is hoped that the study will provide some explicit evidence in developing culturally and linguistically appropriate PCa intervention programs in Chinese American and other Asian American communities.
METHODS
Sample
This study was part of a larger study that included a sample of Chinese, Korean, Vietnamese, and Cambodian Asian Americans selected by obtaining a current list of 111 Asian American community organizations in the greater Philadelphia area, New Jersey, and New York City, which were identified by the Asian Community Cancer Coalition and Center for Asian Health.10 These organizations were located in geographic areas that maximized the coverage of Asian Americans across ethnic groups, ages, and socioeconomic status. Asian community organizations (N=52) were randomly selected as clusters from the list of 111 organizations. The selected community organizations were stratified based on the 4 racial/ethnic or language groups. A proportional allocation procedure of assigning the sample size proportionally to the subgroups’ size was used.25 Of the 2098 participants who agreed to participate in the study, 2011 completed the study, a response rate of 95.9%. The overall sample consisted of 2011 participants, with the distribution among the 4 racial/ethnic groups as follows: Chinese, 45.9% (N = 923); Korean, 19.1% (N = 384); Vietnamese, 18.1% (N = 364); and Cambodian, 16.9% (N=340).10 Based on the recommendations by the American Cancer Society, only men aged 50 years or older should talk to their doctors about prostate cancer screening. Therefore, only Chinese American men aged 50 years and older (N=163) were included in the study.
Design and Data Collection Procedures
The detailed design and data collection procedures were published elsewhere.10 Briefly, a cross-sectional research design was used in the study. Data collection was carried out in 2006. Data collection and administrative training were provided to all survey administrators as well as to on-site bilingual translators. The research team, in collaboration with community leaders, recruited eligible participants from community organizations’ facilities. Age 18 and above, self-identified Chinese, Korean, Vietnamese, and Cambodian participants provided written informed consent to participate in and to complete the study. The survey was administered using face-to-face instruction methods. The instructions on the questionnaire were read aloud by data collection administrators to enhance the understanding of procedures for completion of the survey. Participants had the choice of responding to the questions in English or in their native language (Chinese, Korean, Cambodian, or Vietnamese). Language assistance was provided during the survey administration. The questionnaire required approximately 25 minutes to complete. The responses to the questionnaire were back translated into English for analysis.
Measures
The survey questionnaire items used in the structural equation model (SEM) analysis are described below:
Satisfaction with health care
Seven items assessed a respondent’s perceptions of his health care and doctors’ services: arrangements for making appointments for medical care, length of time between making an appointment for care and visit, length of time waiting to see doctor at the office, overall rating of care at one’s medical group, convenience of location of the doctor’s office, access to medical care whenever needed, and quality of care from one’s physician. The response categories were on a 5-choice scale: “poor,” “fair,” “good,” “very good,” or “excellent.”
Enabling factor
Enabling factor is the factor that makes it possible (or easier) for individuals or populations to change their behavior or their environment.26 The enabling factor was measured using 3 questions: Do you currently have health insurance? Do you have a primary health care provider to go to when you are sick? How many times did you visit your current primary physician in the last 12 months? The frequency of visiting a primary physician is an indicator of health care access. More visits will perhaps increase the likelihood of obtaining cancer screening, including PCa. The response categories were a binary choice (no/yes) for the first 2 questions. Potential answers for the third question were on an ordinal scale with 4 choices: “never,” “one or 2 times,” “3 or 4 times,” and “5 or more times.”
Predisposing factor
Predisposing factor is the factor that exerts its effects prior to a behavior’s occurring, by increasing or decreasing a person’s or population’s motivation to undertake that particular behavior.26 The predisposing factor measured the education level of the participants, including their highest grade of school completed and their years of education completed.
Cultural factor
The cultural factor included participants’ English proficiency and their level of information seeking (Internet use). The response categories were “not at all” to “very well” for English speaking and a binary choice (no/yes) for Internet use.
Cancer fear factor
The cancer fear factor reflected the fear of knowing a bad cancer test result and whether the participants felt embarrassment about cancer. The response categories were a binary choice (no/yes).
Statistical Methods
Model description
Latent model analyses were conducted using Mplus software. The models were covariance structural models with multiple indicators for all latent constructs. The analysis employed a 2-step procedure using maximum likelihood estimation. The first step was confirmatory factor analysis to test the measurement model. A measurement model describes the nature of the relationship between a number of latent variables and the observed variables corresponding to each of the constructs. The second step tested the structural model, depicted in Figure 2 in the Results section. This step represents the theoretically based model in which the relationships among exogenous variables (those variables with both emanating paths and receiving paths) and endogenous variables (those variables with mostly receiving paths) can be seen. The dependent factor was a binary variable: never screened vs screened. Using ordinal and dichotomous indicators is a very common practice in SEM literature. This practice is based on the assumption that the underlying construct represented by the dichotomous variables is continuous. A tetrachoric correlation was created instead of Pearson correlations for the SEM analysis.27
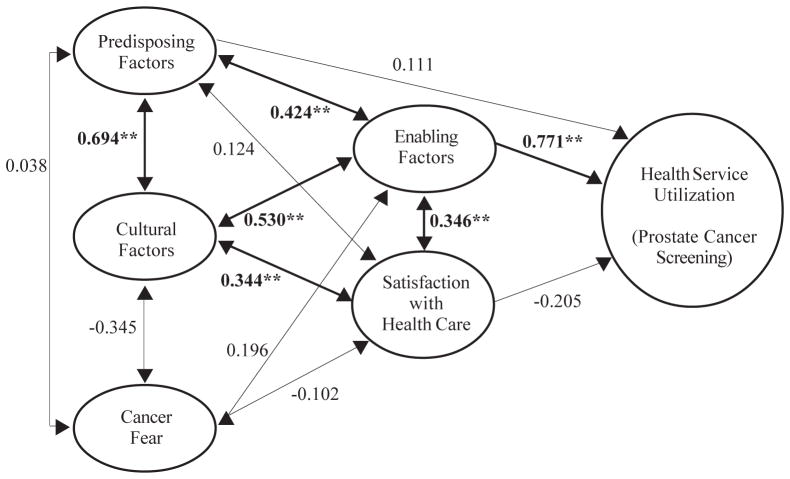
Figure 2.
Path Coefficients and Their Significance From the Structural Equation Modeling Analysis (N = 163)
Note.
CFI = 0.936; TLI = 0.948; RMSEA = 0.064
Understandardized estimates are shown. Prostate cancer screening is coded 1= no, 2 = yes.
Model fit tests
Multiple indices were used to test the model fit, and they included the following: comparative fit indices (CFI), where the value of 0.90 or higher is considered acceptable;22 Tucker-Lewis Index (TLI), where the value of 0.90 or higher is considered acceptable;22 and the root mean square error of approximation (RMSEA), with the value below 0.08 indicating a good fit.28
RESULTS
Sample Characteristics and PCa Screening
Of the 163 Chinese American men aged 50 years and older, the mean age was 60.2 years and ranged from 50 to 85 years old. Of the 163 men, 92 (56.7%) reported never-screened. Education level was significantly related to screening status, χ2 (1) = 13.28, P<.01. For Chinese with less than high school education, 81.6% reported never-screened, compared with 46.7% with high school or higher education who reported never-screened. Screening status was also associated with annual household income, χ2 (2) = 8.17, P<.05. Of respondents with less than $10,000 and $10,000–$30,000 annual household incomes, 63.2% and 62.8% reported never-screened, respectively, compared with 32.1% respondents with more than $30,000 annual household incomes reporting never-screened. Screening status was significantly related to health insurance, χ2 (1) =15.52, P<.01. Of those without current health insurance, 85.3% reported never-screened compared with 46.5% of those with health insurance reporting never-screened. Marital status and employment status were not significantly related to PCa screening status, P>.05.
Model Fit Index
The CFI for the SEM model was 0.936, which meets the acceptable model fit criterion. The TLI yielded a value of 0.948. The RMSEA compares the observed variances and covariances with those resulting from the model’s parameter estimates and is not sensitive to the sample size. The RMSEA of 0.064 indicated an acceptable fit of the measurement model.
Measurement Model
The factor loadings for the indicator variables associated with the constructs are presented in Table 2. The factor loadings are equivalent to standardized regression weights for predicting observed variables from latent constructs. The t-scores obtained for the coefficients in Table 2 were all significant except for one variable (Embarrassment/Shame). The magnitude of the factor loadings and their significance provided evidence to support the convergent validity of the indicators. Overall, the model fit indices and the factor loadings supported the reliability and validity of the constructs for their indicator variables. It was concluded that the theoretical constructs hypothesized to exist at the level of latent factors were assessed with an acceptable degree of precision and that the observed variables were adequate indicators of these factors.
Table 2.
Parameter Estimates for the Hypothesized Measurement Model
| Construct & Indicators | Factor Loading |
|---|---|
| Satisfaction with Health Care | |
| Arrangements for making appointments for medical care | 1.000 |
| Length of time waiting to see doctor at the office | 0.911 |
| Length of time between making an appointment for care and visit | 0.928 |
| Overall, how would you rate care at your medical group? | 0.848 |
| Convenience of location of the doctor’s office | 0.935 |
| Access to medical care whenever needed | 0.953 |
| Quality of care from your physician | 0.827 |
| Enabling Factor | |
| Currently have health insurance? | 1.000 |
| Have a primary health care provider to go to when you are sick? | 1.180 |
| Number of times visited current primary physician in the last 12 months | 0.609 |
| Predisposing Factor | |
| What is the highest grade of school you completed? | 1.000 |
| How many years of education have you completed? | 1.737 |
| Cultural Factor | |
| Do you often use the Internet for sources of information? | 1.000 |
| How well do you think you speak English? | 0.774 |
| Do you usually speak your native Asian language at home? | 0.158 |
| Cancer Fear Factor | |
| Fear of a getting a bad test result | 1.000 |
| Embarrassment/shame | 0.006 |
Structural Model
The hypothesized model and the standardized maximum likelihood estimates for the parameters of the model are presented in Figure 2. For all figures presented in this section, the constructs were coded in the same direction: a positive path coefficient indicates that it is more likely to be associated with PCa screening.
The path coefficients indicate the direction and magnitude of the associations. The enabling factor showed a positive and significant relationship with the screening factor (coefficient = 0.771, t = 5.392, P<.001). The significant path coefficient indicated that participants with health insurance, a primary health care provider, and frequent primary physician visits were more likely to have had prostate cancer screening. None of the other factors were significantly related to the screening factor. However, the cultural factor was significantly related to the enabling factor as well as to the satisfaction with health care factor whereas the predisposing factor was significantly associated with the enabling factor, but not with the satisfaction with health care factor. In addition, the cultural factor was associated with the predisposing factor. In contrast, the cancer fear factor was not related to any other factors in the model. The R2 value provides explained variance among construct variables. Overall, 48% of the PCa screening was explained by the model.
DISCUSSION
The present study focused on testing the Sociocultural Health Behavior Model by using a structural equation analysis to determine the direction and magnitude of the interdependence of the proposed components of the model in relation to the health behavior related to PCa screening among Chinese Americans. Specifically, this study adopted a structural equation model analysis to determine the structural relationship and multiple levels of influence of predisposing, enabling, cultural, environmental health system, and family/social support factors underlying PCa screening among Chinese American men. The study found some significant pathways of the original model proposed and some additional factors.
Education, health insurance, and annual income status were significantly related to PCa screening. Those with less than a high school education, without health insurance, and with low annual income were more likely to be never screened for PCa than were those having more education, health insurance, and a higher income. Studies consistently show that lack of health insurance coverage leads to reduced cancer screening.29–31 A primary enabling factor is having health insurance to be able to pay for the services. Education may be directly and indirectly related to PCa screening. For example, more education has been shown to increase accuracy in self-reporting of PSA screening32 and may be associated with a better understanding of concepts related to PCa.33 Further, some educational interventions, even among low-literacy groups, have been influential in patients’ initiating conversations with their physicians about PCa screening.34 One study found that giving information about PCa screening increased knowledge about PCa; it also reduced positive attitudes toward PSA testing, with no changes in intention to get a PSA than that of a control group.35 This may be attributable to the concern that there is lack of proof that early detection and treatment of PCa reduce prostate cancer death and disability rates.5
Structural Equation Modeling
Overall, our results offered support for a multilevel sociocultural approach to understanding the relationship between access/satisfaction with health care, predisposing, enabling and cultural factors, and health beliefs and PCa screening. Factor loadings were significant for all factors except embarrassment/shame for screening and showed a positive and significant relationship with screening for PCa. Chinese American men with more than a high school education who had health insurance, higher annual income levels, a primary care provider whom they frequently see, and access to health care and who were satisfied with it were more likely to be screened for PCa than were those who did not have these factors.
The path analysis findings also lent support for components of the Sociocultural Health Behavioral Model and indicated that there was a positive and significant relationship between PCa screening and the enabling factors; between predisposing factors and enabling factors; between cultural factors and predisposing, enabling, and access/satisfaction with health care factors; and between enabling factors and access/satisfaction with health care. In general, if Chinese American men were able to access health care and had a primary care provider, they were more likely to get screened for PCa. There were a number of factors that were loaded heavily under access/satisfaction with health care. These factors included being able to make an appointment, not having to wait long, providers being in a convenient location, and the participants’ rating their provider highly. Physicians also need to initiate a dialogue with patients to educate them about the potential benefits and limitations of screening so that patients can make a personal and informed decision consistent with their own preferences and values. Physicians’ recommendation of screening is important for Chinese American men to go for screening.36 Some previous studies have shown that physicians often do not discuss PCa screening with patients, even those who were due for PSA testing. One study showed that such a discussion occurred only 36% of the time; barriers for discussing this included patient comorbidity, limited education/health literacy, prior refusal of care, physician forgetfulness, acute-care visits, and lack of time.37 Another study suggested that family physicians were more likely than general internists to recommend the PCa screening.38 Further study needs to be conducted among Chinese American patients and physicians who serve Chinese American patients to determine if physicians regularly discuss prostate cancer screening, how the decision of screening or not screening is made after such a discussion, and whether there is any difference of discussion among language concordant and discordant physician-patients.
The cultural factor was significantly related to the predisposing, enabling, and satisfaction with health care factors. Chinese American men who perceived they were fluent in English and used the Internet as a source of information were more likely to get screened than were those who were not fluent or did not use the Internet. The model accounted for 48% of the variance in PCa screening. The model highlights the significance that sociocultural factors play in relation to PCa screening and enabling factors. Those with low socioeconomic status were less likely to get screened for cancer.39–41 Acculturation was not found to be directly correlated with PCa screening, contrary to other cancer screening studies among Chinese Americans.40–42 We did, however, find that acculturation was significantly correlated with the predisposing, enabling, and health care satisfaction factors. These findings indicate that cultural alignment may be indirectly related to those factors that influence a Chinese American man’s decision to undergo PCa screening.
There were also racial/ethnic differences in PCa screening, though the reasons are not clear. Previous studies have cited that certain racial/ethnic groups, such as African Americans, are more likely to be diagnosed with advanced stages of cancer and have a higher mortality rate.43 This racial difference may be further compounded by English fluency deficiency. Chinese American men who have poor English language skills may need to be provided with language and clinical assistance, including having a better understanding of the importance of PCa testing.
Family/social support is an important factor in relation to health-seeking behavior,44 yet we did not find its significant contribution to the PCa screening. This may be due in part to the little variation among a relatively homogeneous sample of Chinese American men in our study, all of whom were involved in community organizations. Further study is warranted in this area from other ethnic groups and from other cancer screening practice.
This study analyzed and illustrated a model of the pathways among constructs leading to PCa screening among Chinese American men. By using structural equation modeling, the most likely linkages among constructs and the mediating factors can be examined. This model investigated how cultural, predisposing, enabling, access/satisfaction with health care, and health belief factors are related to PCa screening. To our knowledge, our present study is one of the first studies to perform a path analysis with regard to factors that may lead to PCa screening among Chinese American men.
However, our study is not exempt from limitations. First, because the study was cross-sectional, the causality of relationships among the constructs cannot be determined. Second, these findings are based on self-reporting questionnaires and, as a result, may include participant response bias. Third, our small sample size may lack the power to detect some factors that were directly contributable to the screening. Fourth, because the sample was drawn from Chinese American men who participate in community organizations, the findings may not be generalizable to all Chinese American males, especially those who do not participate in community-based organizations.
Despite these limitations, our study can provide information for the development of future interventions based on the social/cultural model. The model may be applied and validated in other health behavior and other ethnic groups and in other geographic areas of the country. The model suggests that a culturally appropriate, community-based service with a combined educational service approach could facilitate the PCa screening in Chinese American men. PCa screening programs may be more effective if they include the cultural, predisposing, enabling, access/satisfaction with health care, and health belief factors associated with PCa screening. Sensitivity to ethnic and cultural factors, especially English language and other family or community contexts and dynamics, should be present throughout all secondary prevention activities, especially with the provision of translation services and education materials in one’s native language to enhance interventions that target improved PCa screening rates among Chinese Americans. Furthermore, the significant relationship that cultural factors had to more proximal constructs suggests that the use of culturally appropriate materials should be explored. The use of community organizations, which served as the basis for the study, can play a role in assisting Chinese American men in identifying, planning, and adopting effective evidence-based screening programs. The community organizations may work in collaboration with representatives from the local health department, university research centers, and other related partners who can work together more successfully than the work of a single agency in implementing prevention programs.
Table 1.
Socio-demographic Characteristics and Prostate Cancer Screening Status
| Sociodemographic Characteristics | Never-Screened (%) | Screened (%) |
|---|---|---|
| Current Marital Status | ||
| Unmarried | 52.9 | 47.1 |
| Married | 57.3 | 42.7 |
| Highest Degree** | ||
| <HighSchool | 81.6 | 18.4 |
| >HighSchool | 46.7 | 53.3 |
| Employment Status | ||
| Employed | 59.3 | 40.7 |
| Unemployed | 52.0 | 48.0 |
| Annual Income** | ||
| <$10,000 | 63.2 | 36.8 |
| $10,000–$30,000 | 62.7 | 37.3 |
| >$30,000 | 32.1 | 67.9 |
| Current Health Insurance** | ||
| No | 85.3 | 14.7 |
| Yes | 46.5 | 53.5 |
P<.05 from chi-square test
P<.01 from chi-square test
Acknowledgments
This research was supported by NIH grants U01 CA114582 ATECAR-Asian Community Cancer Network and by U54CA153513.
Contributor Information
Grace X. Ma, Department of Public Health, Director of Center for Asian Health, College of Health Professions, Temple University, Philadelphia, PA.
Steven E. Shive, Center for Asian Health, Temple University; and Department of Health, East Stroudsburg University, East Stroudsburg University, East Stroudsburg, PA.
Wanzhen Gao, Center for Asian Health, Department of Public Health, College of Health Professions, Temple University, Philadelphia, PA.
Yin Tan, Center for Asian Health, Department of Public Health, College of Health Professions, Temple University, Philadelphia, PA.
Min Qi Wang, Department of Behavioral and Community Health, University of Maryland School of Public Health, College Park, MD.
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2007 Incidence and Mortality Web-based Report. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; [Accessed June 4, 2011]. Available at: http://www.cdc.gov/uscs. [Google Scholar]
- 2.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer. CA: A Cancer Journal for Clinicians. 2004;54(1):41–52. doi: 10.3322/canjclin.54.1.41. [DOI] [PubMed] [Google Scholar]
- 3.Barry MJ. Clinical practice. Prostate-specific-antigen testing for early diagnosis of prostate cancer. N Engl J Med. 2001;344(18):1373–1377. doi: 10.1056/NEJM200105033441806. [DOI] [PubMed] [Google Scholar]
- 4.Burack RC, Wood DP. Screening for prostate cancer. The challenge of promoting informed decision making in the absence of definitive evidence of effectiveness. Med Clin North Am. 1999;83(6):1423–1442. doi: 10.1016/s0025-7125(05)70173-5. [DOI] [PubMed] [Google Scholar]
- 5.U S. Preventive Services Task Force. Screening for prostate cancer: recommendation and rationale. Ann Intern Med. 2002;137(11):915–916. doi: 10.7326/0003-4819-137-11-200212030-00013. [DOI] [PubMed] [Google Scholar]
- 6.Bartsch G, Horninger W, Klocker H, et al. Tyrol Prostate Cancer Demonstration Project: early detection, treatment, outcome, incidence and mortality. Br J Urol. 2008;101(7):809–816. doi: 10.1111/j.1464-410X.2008.07502.x. [DOI] [PubMed] [Google Scholar]
- 7.Sim HG, Cheng WS. Changing demography of prostate cancer in Asia. Eur J Cancer. 2005;41(6):834–845. doi: 10.1016/j.ejca.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer Facts and Figures. Atlanta (GA): American Cancer Society; 2007. [Accessed May 5, 2007]. Available at: http://www.cancer.org/Research/CancerFactsFigures/CancerFactsFigures/index. [Google Scholar]
- 9.Lee J, Demissie K, Lu SE, et al. Cancer incidence among Korean-American immigrants in the United States and native Koreans in South Korea. Cancer Control. 2007;14(1):78–85. doi: 10.1177/107327480701400111. [DOI] [PubMed] [Google Scholar]
- 10.Ma GX, Shive SE, Wang MQ, et al. Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav. 2009;33(6):650–660. doi: 10.5993/ajhb.33.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goel MS, Wee CC, McCarthy EP, et al. Racial and ethnic disparities in cancer screening. Journal of General Internal Medicine. 2003;18(12):1028–35. doi: 10.1111/j.1525-1497.2003.20807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma GX, Lee S, Wang MQ, et al. The role of sociocultural factors in Hepatitis B screening among Asian Americans. Southern Medical Journal. 2011;104(7):466–472. doi: 10.1097/SMJ.0b013e31821f8ab0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janz NK, Becker MH. The health belief model: a decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Pearson; 1986. [Google Scholar]
- 15.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 16.Copenhaver MM, Lee IC. Optimizing a community-friendly HIV risk reduction intervention for injection drug users in treatment: a structural equation modeling approach. J Urban Health. 2006;83(6):1132–1142. doi: 10.1007/s11524-006-9090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ebrahim SH, Anderson JE, Weidle P, Purcell DW. Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS. 2004;18(1):27–33. doi: 10.1089/108729104322740893. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Doukas DJ. Health motivation and emotional vigilance in genetic testing for prostate cancer risk. Clin Genet. 2004;66(6):512–516. doi: 10.1111/j.1399-0004.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- 19.Gelderen B, Heuven E, Veldhoven M, et al. Psychological strain and emotional labor among police-officers: a diary study. Journal of Vocational Behavior. 2007;71(3):446–459. [Google Scholar]
- 20.Wang MQ, Matthew RF, Bellamy N, et al. A structural model of the substance use pathways among minority youth. Am J Health Behav. 2005;29(6):531–541. doi: 10.5555/ajhb.2005.29.6.531. [DOI] [PubMed] [Google Scholar]
- 21.Bentler PM, Wu EJ. EQS for Windows User’s Guide. Encino, CA: Multivariate Software, Inc; 1995. [Google Scholar]
- 22.Joreskog KG. Testing Structural Equation Models. Newbury Park: Sage; 1993. [Google Scholar]
- 23.Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: extending a public health-oriented research base. J Consult Clin Psychol. 1998;66(2):385–399. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- 24.Barnes JS, Bennett CE. The Asian Population: 2000. Census 2000 Brief, #C2KBR/01-16. 2002 [Google Scholar]; Nguyen EV. Cancer in Asian American Males: Epidemiology, Causes, Prevention, and Early Detection. Asian Am Pac Isl J Health. 2003;10(2):86–99. [PubMed] [Google Scholar]
- 25.Sudman S, Bradburn NM. Asking Questions. San Francisco, CA: Jossey-Bass; 1983. [Google Scholar]
- 26.Green LW, Kreuter MW. Health Promotion Planning: An Educational and Ecological Approach. 3. Mountain View, CA: Mayfield; 1999. [Google Scholar]
- 27.Muthén B, Muthén L. [Accessed August 12, 2000];Mplus User’s Guide (online) Available at: http://www.statmodel.com/ugexcerpts.shtml.
- 28.Bollen KA, Long JS. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 29.New York City Department of Health and Mental Hygiene. Cervical cancer screening in New York City. NYC Vital Signs. 2006;5(3):1–4. [Google Scholar]
- 30.Secginli S, Nahcivan NO. Factors associated with breast cancer screening behaviors in a sample of Turkish women: a questionnaire survey. Int J Nurs Stud. 2006;43(2):161–171. doi: 10.1016/j.ijnurstu.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 31.Ward E, Jemal A, Cokkinides V, et al. Cancer Disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 32.Chan EC, Vernon SW, Ahn C, et al. Do men know that they have had a prostate-specific antigen test? Accuracy of self-reports of testing at 2 sites. Am J Public Health. 2004;94(8):1336–1338. doi: 10.2105/ajph.94.8.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hughes GD, Sellers DB, Fraser L, Jr, et al. Prostate cancer community collaboration and partnership: education, awareness, recruitment, and outreach to southern African-American males. J Cult Divers. 2007;14(2):68–73. [PubMed] [Google Scholar]
- 34.Kripalani S, Sharma J, Justice E, et al. Low-literacy interventions to promote discussion of prostate cancer: a randomized controlled trial. Am J Prev Med. 2007;33(2):83–90. doi: 10.1016/j.amepre.2007.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Watson E, Hewitson P, Brett J, et al. Informed decision making and prostate specific antigen (PSA) testing for prostate cancer: a randomized controlled trial exploring the impact of a brief patient decision aid on men’s knowledge, attitudes and intention to be tested. Patient Educ Couns. 2006;63(3):367–379. doi: 10.1016/j.pec.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Teng EJ, Friedman LC, Green CE. Determinants of colorectal cancer screening behavior among Chinese Americans. Psychooncology. 2006;15(5):374–381. doi: 10.1002/pon.958. [DOI] [PubMed] [Google Scholar]
- 37.Guerra CE, Jacobs SE, Holmes JH, et al. Are physicians discussing prostate cancer screening with their patients and why or why not? A pilot study. J Gen Intern Med. 2007;22(7):901–907. doi: 10.1007/s11606-007-0142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim HL, Benson DA, Stern SD, et al. Practice trends in the management of prostate disease by family practice physicians and general internists: an internet-based survey. Urology. 2002;59(2):266–271. doi: 10.1016/s0090-4295(01)01504-7. [DOI] [PubMed] [Google Scholar]
- 39.Sun WY, Basch CE, Wolf RL, et al. Factors associated with colorectal cancer screening among Chinese-Americans. Prev Med. 2004;39(2):323–329. doi: 10.1016/j.ypmed.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 40.Taylor VM, Choe JH, Yasui Y, et al. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J Community Health. 2005;30(6):477–490. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thompson MJ, Taylor VM, Yasui Y, et al. HBV knowledge and practices among Chinese Canadian women in Vancouver, British Columbia. Can J Public Health. 2003;94(4):281–286. doi: 10.1007/BF03403606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones RA, Underwood SM, Rivers BM. Reducing prostate cancer morbidity and mortality in African American Men: issues and Challenges. Clin J Oncol Nurs. 2007;11(6):865–872. doi: 10.1188/07.CJON.865-872. [DOI] [PubMed] [Google Scholar]
- 43.Choe JH, Tu SP, Lim JM, et al. Heat in their intestine: colorectal cancer prevention beliefs among older Chinese Americans. Ethn Dis. 2006;16(1):248–254. [PubMed] [Google Scholar]
- 44.Broadhead WE, Gehlbach SH, deGruy FV, et al. Functional versus structural social support and health care utilization in a family medicine outpatient practice. Med Care. 1989;27(3):221–233. doi: 10.1097/00005650-198903000-00001. [DOI] [PubMed] [Google Scholar]