Abstract
Heterogeneous classes of comorbid trajectories of tobacco and marijuana use were examined in order to determine how they are related to subsequent antisocial behavior, poor self control and internalizing behavior. Data are from a four-wave longitudinal study of African American (n=243) and Puerto Rican (n=232) adolescents and adults in the community. Logistic regression analyses were employed to measure the association between the comorbid trajectories of tobacco and marijuana use and the psychological difficulty variables. We found six joint trajectory groups. We compared the non-or-experimental tobacco/marijuana use group with the other user groups in each of the psychological difficulty domains. The infrequent tobacco/late onset marijuana use and chronic tobacco/marijuana use groups differed most strongly from the non-or-experimental tobacco/marijuana use group across the antisocial behavior, poor self control, and internalizing problems domains. The chronic tobacco/maturing out marijuana use group also had significant associations in each of these domains. The infrequent tobacco/marijuana use and late onset tobacco/infrequent marijuana use groups had no or weak associations with the psychological outcomes. Tobacco and marijuana cessation programs should identify and address comorbid use of tobacco and marijuana, and antisocial behavior, poor self control, and internalizing problems, which are associated with histories of comorbid use of the two substances.
Keywords: Comorbidity, tobacco and marijuana use, psychological problems and drug use, logistic regression analysis
INTRODUCTION
Tobacco and marijuana are frequently used concurrently in the United States (1, 2). The number of American adolescents and young adults currently using both substances is estimated at 4.9 million (3). Research has indicated that the use of just one of these substances is associated with adverse health (4–6) and psychological outcomes (7, 8) later in life. Furthermore, researchers have determined that concurrent tobacco and marijuana use may have an additive, adverse effect on lung functioning (9). Additional research is needed on the outcomes associated with comorbid use of tobacco and marijuana in the psychological domain.
The current study incorporates theoretical concepts from Family Interactional Theory (FIT; 10) that can be applied to research on the outcomes of comorbid tobacco and marijuana use. According to FIT, histories of comorbidity of tobacco and marijuana use may be related to three aspects of psychological functioning; namely, antisocial behavior, poor self control, and internalizing problems. Antisocial behavior refers to aggressive or impulsive actions that violate conventional norms (11). Poor self control refers to a limited ability of the individual to regulate affect, control one’s impulses, and delay gratification (12). Internalizing problems refer to depression, anxiety, and interpersonal hypersensitivity (13).
Regarding antisocial behavior, McGue and Iacono (14) and Tucker, Martínez, Ellickson, and Edelen (15) have reported that tobacco use in adolescence predicts later antisocial disorders and criminality. Keyes, Iacono, and McGue (16) and Fergusson, Horwood, and Swain-Campbell (17) found support for a similar relationship between antisocial behaviors and marijuana use.
Both tobacco and marijuana use have similarly been shown to predict poor self control. Flory and Manuck (18), for example, reported that a history of tobacco use was associated with impulsivity, a component of poor self control. Piechatzek et al. (19) found similar results in their research on the association of a history of marijuana use with impulsivity. Another component of poor self control, a limited ability to delay gratification, has been predicted by age of first use of both tobacco and marijuana (20).
With respect to internalizing problems, Pederson and von Soest (21), Klungsøyr, Nygård, Sørensen, and Sandanger (22), and Cuijpers, Smit, ten Have, and de Graaf (23) found empirical support for a longitudinal association of smoking and nicotine dependence with later internalizing mood and anxiety disorders. Schuetze, Eiden, and Dombkowski (24) also found that a recent history of cigarette smoking was associated with interpersonal sensitivity, which we refer to here as hypersensitivity, among new mothers. With regard to marijuana use, Van Laar, van Dorsselaer, Monshouwer, and de Graaf (25), Patton, Coffey, Carlin, Degenhardt, Lynskey, and Hall (26), and Hayatbakhsh, Najman, Jamrozik, Mamun, Alati, and Bor (27) found support for a parallel association between marijuana use and depression and anxiety problems. Aragona and colleagues (28) additionally found support for the association between levels of THC, an active ingredient in cannabis, in the bloodstream and increased hypersensitivity.
In the present study, we will examine heterogeneous classes of comorbid trajectories of tobacco and marijuana use in order to determine how they are related to subsequent antisocial behavior, poor self control and internalizing behavior. Individual, as opposed to group, patterns of substance use over time are termed trajectories of use (29). A recent focus of substance use research, examination of the outcomes of trajectories of use allows for the identification of specific developmental periods during which substance use increases risk for later adverse outcomes. Research on trajectories of marijuana use alone has shown that heavy marijuana use during early adolescence, compared to abstention, is associated with a greater likelihood of problems in the antisocial behavior spectrum in adulthood such as antisocial personality symptoms and arrests (30). Research on trajectories of tobacco use alone have shown that heavy tobacco use during early adolescence, compared to abstention, has been associated with problems in the self-control spectrum such as limited ability to delay gratification (31), increased criminality (32) and “risky” personality characteristics such as low conscientiousness (33). Although research on marijuana use trajectories has not supported an association with internalizing problems thus far (30, 34), Chassin and colleagues (33) did find that their heavy tobacco use trajectory group was associated with negative affect.
In order to address the adverse outcomes experienced by individuals who have a history of use of both tobacco and marijuana, we will investigate the psychological outcomes associated with comorbid trajectories of tobacco and marijuana use. A comorbid trajectory is defined as a longitudinal profile of the use of multiple substances (35). Studies that have addressed these relationships between the trajectories use of one substance to trajectories of use of another have primarily focused on comorbidity with alcohol use (30, 36). Jackson, Sher, and Schulenberg (37) and Brook, Lee, Finch and Brown (38) are among the few research groups to have examined comorbid trajectories of tobacco and marijuana use. Jackson and colleagues identified seven comorbid trajectory pairs, while Brook and colleagues identified four. As both research teams focused on risk factors for membership in a comorbid trajectory pair, the need for research on the psychological outcomes of membership in comorbid trajectory pairs of tobacco and marijuana use has yet to be addressed. Such research will provide even more individualized information on developmental periods of risk for later adverse outcomes than studies of outcomes of membership in trajectory groups of use of a single substance, by taking into account the use of two substances simultaneously. This line of research has significant implications for substance use prevention and intervention programs.
We propose the following hypotheses: (1) There will be at most seven distinct comorbid trajectories, including a trajectory of chronic use of both tobacco and marijuana use, a trajectory of chronic use of tobacco and maturing out use of marijuana, a trajectory of infrequent use of tobacco and chronic use of marijuana, a trajectory of late onset of tobacco and marijuana use, and/or a trajectory of no or infrequent use of both substances. (2) The trajectory of no/infrequent use of tobacco and marijuana will be the most common. (3) Trajectories of chronic use of both tobacco and marijuana, of chronic use of tobacco and maturing out use of marijuana, of infrequent use of tobacco and chronic use of marijuana, and of late onset of tobacco and marijuana use will be more strongly associated compared to the non/infrequent use group on antisocial behavior, poor self control, and internalizing outcomes.
METHOD
Sample and Procedure
Data are from a four-wave longitudinal study of African American and Puerto Rican adolescents and adults. With regard to the race/ethnicity of our sample; when this study began, there were no studies designed to address substance use and problem behavior among minority youth. Furthermore, members of the community and the schools were eager to have data on African Americans and Puerto Ricans that could be used to make intervention programs culturally relevant and linguistically appropriate. We therefore decided to fill this gap by conducting a study of African Americans and Puerto Ricans.
The time 1 (T1) data were collected in 1990, time 2 (T2) in 1994, time 3 (T3) in 2000, and time 4 (T4) in 2002. Participants at T1 (N=1331) came from grades 7–10 in 11 schools serving the East Harlem area of New York City. The T1 data collection took place in classrooms, while the T2, T3, and T4 data were collected primarily via in-person home interviews. The T2 response rate was 89% of those who participated at T1. Because of budget limitations, the T3 data collection was a sub-sample of the T2 sample (T3 N=660). To insure sufficient N’s on our dependent variables, we oversampled respondents who reported using marijuana and/or having a child at T2. At T4, again due to budget restrictions, we took a sub-sample of the T3 participants (T4, N=475). As the T4 data collection emphasized tobacco use, smokers were oversampled. The 475 participants present at T4 were used in the trajectory analyses in this paper.
The Institutional Review Boards of the Mount Sinai School of Medicine and New York University School of Medicine approved the study’s procedures for data collections. Written informed assent was obtained from all minors and passive consent procedures were followed for parents of minors. For participants older than age 18, informed consent was obtained.
Participants who took part at T1 and T4, compared to those who participated at T1 only, reported greater tobacco and marijuana use (p ≤ .05). For a more complete sample description, we refer to our published paper using the same sample (38).
Of the 475 participants, 51% (n=243) were African American, and 49% (n=232) were Puerto Rican. With regard to gender, Females comprised 50.7% (n=241) of the sample. Mean ages were 13.9 (SD=1.3) at T1, 19.3 (SD=1.5) at T2, 24.4 (SD=1.3) at T3, and 26.1 (SD=1.4) at T4.
The median educational level at T4 was having completed at least one year of business or technical school. With regard to occupational level at T4, 33.4% were employed in clerical positions, 17.3% were employed in semi-skilled jobs (e.g., factory worker), 13.9% had professional level jobs, 11.0% had skilled jobs (e.g., mechanic), and 24.4% were unemployed. Of those who were unemployed, 17.2% were attending school. At T4, 60.6% of the sample were single, 20.6% of the participants were cohabiting, 16.0% of the sample were married and living together, and 2.8% of the sample were married but separated.
Measures
The respondents were asked about the number of cigarettes currently smoked at each wave (T1–T4). Response options included “none” (coded 1), “a few cigarettes or less a week” (2), “1 – 5 cigarettes a day” (3), “about half a pack a day” (4), “about one pack a day” (5), and “more than one pack a day” (6).
The respondents were asked about the frequency of their marijuana use. The response options included “never” (1), “a few times a year or less” (2), “about once a month” (3), “several times a month” (4), and “once a week or more” (5).
Table 1 presents the demographic variables and the psychological difficulty variables with their Cronbach’s alphas and sources (see Table 1). Racial and ethnic background were identified by the participants at T1 using pre-determined response options. Each psychological difficulty variable was assessed at T4. The Cronbach’s alphas were adequate. The psychological difficulty variables have been found in previous research to predict substance use and psychopathology (39, 40).
TABLE 1.
Demographic and Psychological Difficulty Measures: Sources and Cronbach’s Alphas
| Domain/Scale and number of items | Cronhach’s Alpha | Source | Sample Item |
|---|---|---|---|
| Independent variables | |||
| Demographic | |||
| Gender | NA | 1: Female, 2: Male | |
| Age | NA | Age at Time 4 | |
| Ethnicity | NA | Are you Hispanic? (1: AA, 2: PR) | |
| Socioeconomic status – 5 items | NA | Combination of education level and job status of parents | |
| Psychological Difficulty: Antisocial behavior | |||
| Risk taking – 8 items | .75 | Jackson (41) | Do you like to live dangerously? |
| Rebellion – 3 items | .68 | Smith & Fogg (42) | Do you enjoy doing things you shouldn’t, just for the fun of it? |
| Psychological Difficulty: Poor self-control | |||
| Impulsivity – 4 items | .66 | Jackson (41); Brook, Brook, Gordon, Whiteman & Cohen (10) | Do you often act on the spur of the moment without stopping to think? |
| Psychological Difficulty: Internalizing problems | |||
| Depression – 8 items | .83 | Derogatis (43) | Do you sometimes feel unhappy, sad, or depressed? |
| Anxiety – 3 items | .76 | Derogatis (43) | Over the last few years, how much were you bothered by feeling fearful? |
| Interpersonal hypersensitivity* - 4 items | .72 | Derogatis (43) | Over the last few years, how much were you bothered by feeling easily annoyed or irritated? |
Interpersonal hypersensitivity was originally named interpersonal sensitivity in the source material.
Note 1. The alphas are estimated from our data.
2. AA=African American, PR=Puerto Rican
Analytic Plan
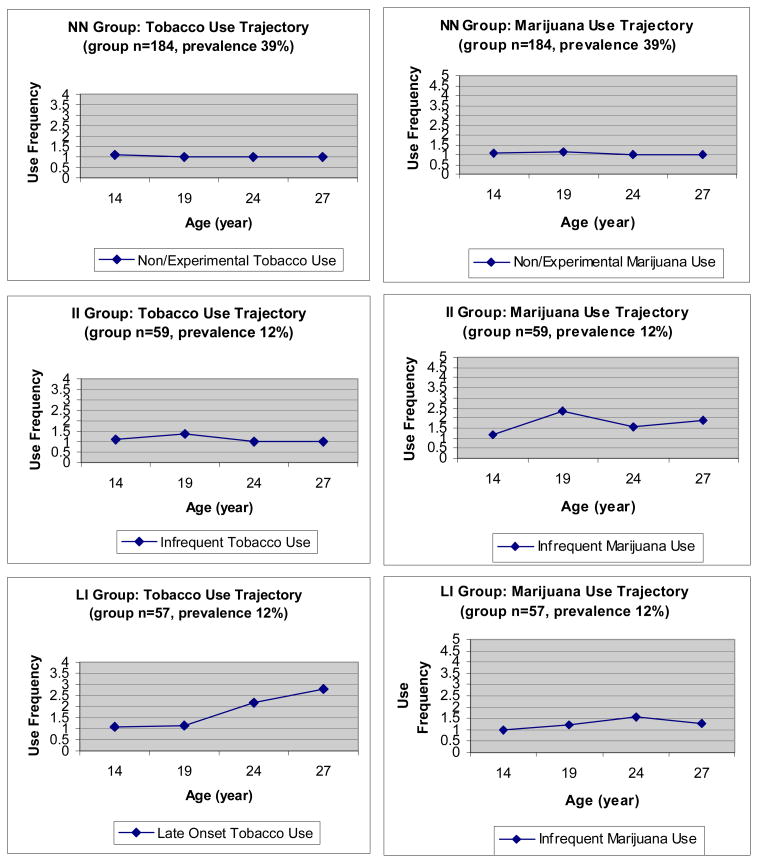
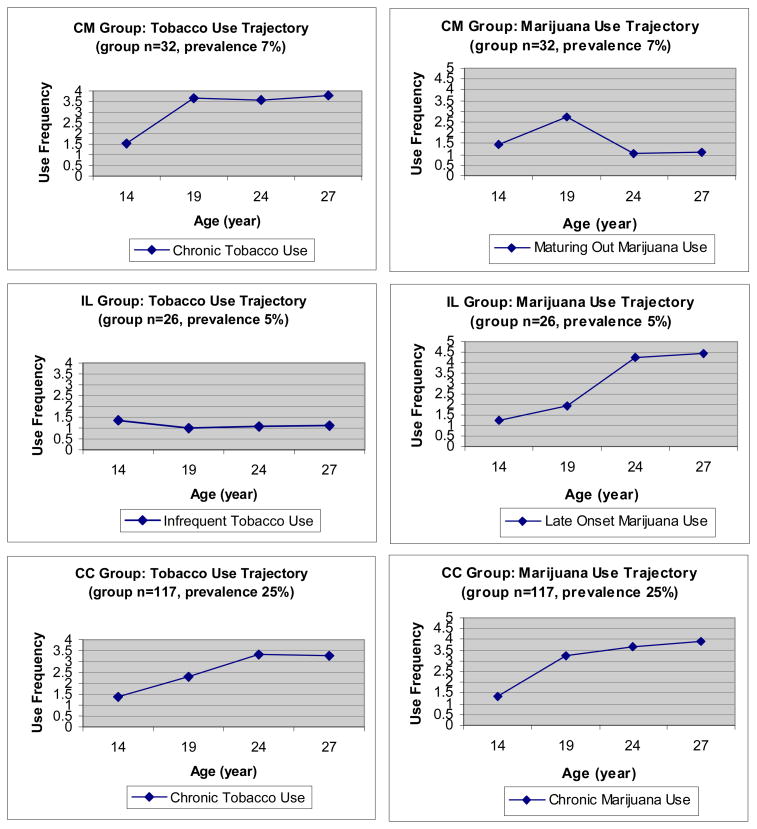
We used Mplus to obtain the comorbid trajectories of tobacco and marijuana use (44). The dependent variables, tobacco and marijuana use at each point in time, were treated as censored normal variables. We applied the full information maximum likelihood approach (45) (FIML) for missing data. We used the Bayesian Information Criterion (BIC) to determine the number of trajectory groups. Each participant was assigned to the trajectory group with the largest Bayesian posterior probability (BPP), and we created an indicator variable for each trajectory group that had a value of 1 if the participant was assigned to that group, and 0 otherwise. The observed trajectories for a group were the averages of tobacco and marijuana use at each point in time for the participants assigned to the group (see Figure 1).
Figure 1.
Trajectories of Tobacco and Marijuana Use by Comorbid Trajectory Group.
We then conducted logistic regression analyses using SAS (46) to examine the association between the comorbid trajectories of tobacco and marijuana use and the psychological difficulty variables. In the logistic regression analyses, the indicator variables of the comorbid trajectories of tobacco and marijuana use were used as the independent variables. Each psychological difficulty variable at T4 was used as a dependent variable with a participant assigned a score of 1 if the participant’s scale value was in the top 16th percentile and 0 otherwise. The control variables were gender, ethnicity, age at T4, and education level at T4. T1 psychological difficulty variables for risk taking, rebellion, and depression were each used as additional control variables, respectively. Low ego integration at T1 was used as a control variable for the poor self control domain because we did not have an impulsivity measure from an earlier wave. Low ego integration at T4 is related to impulsivity at T4 (Pearson’s Correlation Coefficient = .50, p< .001).
RESULTS
The mean and standard deviation (SD) scores of tobacco use at each point in time were 1.2 (0.7), 1.6 (1.1), 1.9 (1.3), and 2.0 (1.3) for T1–T4, respectively. Similarly, the mean (SD) marijuana use scores at T1–T4, respectively, were 1.2 (0.7), 2.0 (1.5), 2.0 (1.5), and 2.1 (1.5).
Extracting the Joint Trajectories of Tobacco and Marijuana Use
A six-group model was selected, based on BIC. Figure 1 presents the observed trajectories and percentages for each of the six trajectory groups. For each group, the mean Bayesian posterior probability (BPP) of the participants who were assigned to the corresponding group ranged from 88% to 96%, which indicates a good classification.
The six joint trajectory groups were named: 1) non-or-experimental tobacco/non-or-experimental marijuana use (NN, 39%, mean BPP=93%), 2) infrequent tobacco/infrequent marijuana use (II, 12%, mean BPP=92%), 3) late onset tobacco/infrequent marijuana use (LI, 12%, mean BPP=91%), 4) chronic tobacco/maturing out marijuana use (CM, 7%, mean BPP=88%), 5) infrequent tobacco/late onset marijuana use (IL, 5%, mean BPP=91%), and 6) chronic tobacco/chronic marijuana use (CC, 25%, mean BPP=96%). As shown in Figure 1, the II user group started using both tobacco and marijuana in late adolescence, but did not increase thereafter. The LI user group started using both tobacco and marijuana in late adolescence and increased tobacco use over time, though they did not increase in the frequency of marijuana use. The CM user group started both using tobacco and marijuana in early adolescence and increased thereafter for tobacco while reducing marijuana use. The IL user group started using tobacco in early adolescence but did not increase over time and used marijuana in late adolescence and increased marijuana over time. The CC user group started using tobacco and marijuana in early adolescence and increased over time.
Correlates of Comorbidity
Table 2 shows odds ratios (OR) when gender, ethnicity, age at T4, education level at T4, and the corresponding T1 psychological difficulty measures were controlled in the logistic regression analyses.
TABLE 2.
Odds ratios (95% confidence intervals in parentheses) from logistic regression analyses of comorbid trajectories of tobacco and marijuana use to predict psychological difficulties.
| Comorbid Trajectories | Psychological Difficulties | |||||
|---|---|---|---|---|---|---|
| Antisocial behavior | Poor self-control | Internalizing problems | ||||
| Risk Taking | Rebellion | Impulsivity | Depression | Anxiety | Interpersonal Hypersensitivity | |
| II vs. NN | 1.8 (0.6, 5.0) | 2.5 (0.8, 7.8) | 2.0 (0.9, 4.3) | 2.4 * (1.0, 5.7) | 1.1 (0.5, 2.9) | 1.2 (0.5, 3.0) |
| LI vs. NN | 1.3 (0.4, 4.0) | 3.3 * (1.1, 10.3) | 0.8 (0.4, 2.0) | 1.4 (0.5, 3.7) | 1.0 (0.4, 2.7) | 1.0 (0.4, 2.6) |
| CM vs. NN | 3.1 (0.9, 10.3) | 7.9 *** (2.5, 25.2) | 2.9 * (1.2, 6.8) | 4.0 ** (1.5, 10.6) | 2.7 * (1.0, 7.2) | 2.8 * (1.1, 7.4) |
| IL vs. NN | 11.1 *** (3.9, 31.5) | 7.8 *** (2.4, 25.8) | 1.4 (0.5, 4.2) | 4.6 ** (1.6, 13.1) | 1.8 (0.5, 6.0) | 2.2 (0.8, 6.4) |
| CC vs. NN | 8.7 *** (4.0, 18.8) | 6.4 *** (2.6, 15.9) | 2.5 ** (1.4, 4.7) | 3.2 ** (1.6, 6.7) | 2.4 * (1.2, 4.7) | 2.2 * (1.1, 4.4) |
Note 1.
P<.05,
P<.01,
P<.001
2 Gender, ethnicity, age at T4, education level at T4, and/or T1 psychological difficulty variable were statistically controlled.
As noted in Table 2, we compared the IL, the CC, the CM, the II, and the LI the user groups to the NN group. For the IL user group, relative to the NN group, risk taking (OR=11.1, p<.001), rebellion (OR=7.8, p<.001), and depression (OR=4.6, p<.01) were associated with the IL trajectory. For the CC user group, compared to the NN group, all the variables were significantly associated with the CC comorbid trajectory group (risk taking, OR=8.7, p<.001; rebellion, OR=6.4, p<.001; impulsivity, OR=2.5, p<.01; depression, OR=3.2, p<.01; anxiety, OR=2.4, p<.05; interpersonal hypersensitivity, OR=2.2, p<.05). For the CM user group, relative to the NN group, rebellion (OR=7.9, p<.001), impulsivity (OR=2.9, p<.05), depression (OR=4.0, p<.01), anxiety (OR=2.7, p<.05), and interpersonal hypersensitivity (OR=2.8, p<.05) were associated with the CM comorbid trajectory group. Finally, in comparison with the NN group, depression (OR=2.4, p<.05) and rebellion (OR=3.3, p<.05) were related to the II and the LI groups, respectively.
DISCUSSION
We examined the developmental course of comorbid tobacco and marijuana use from adolescence to adulthood, and identified psychological outcomes associated with comorbid trajectories of tobacco and marijuana use. This is the first study to examine the psychological outcomes of antisocial behavior, poor self control, and internalizing behavior as related to comorbid trajectories of these substances.
We identified six comorbid trajectories of tobacco and marijuana use which were largely consistent with the hypothesized groups. In contrast to our previous study which extracted four comorbid trajectories by first extracting separate trajectories for tobacco and marijuana use (38), in the current study we extracted the comorbid trajectories by analyzing tobacco and marijuana use simultaneously. As anticipated, the chronic tobacco/chronic marijuana use was the most common group (25% prevalence) after the non-or-experimental tobacco/marijuana use group (39% prevalence).
One trajectory group, the infrequent tobacco/late onset marijuana users (prevalence 5%), is noteworthy for the presence of a substantial history of marijuana use in the absence of a significant history of tobacco use. This pattern does not lend support to the Gateway Theory, which maintains that legal drug use is a necessary prerequisite for illegal drug use (47).
With respect to psychological outcomes associated with membership in these trajectories, we found that the groups consisting of infrequent tobacco/late onset marijuana users and chronic tobacco/chronic marijuana users had the strongest associations with the adverse psychological outcomes (antisocial behavior, poor self control, and internalizing problems) in comparison to the non-or-experimental tobacco/marijuana users. The chronic tobacco/maturing out marijuana users also demonstrated associations with adverse psychological outcomes relative to the non-or-experimental tobacco/marijuana users. We found that the trajectory groups consisting of infrequent tobacco/infrequent marijuana users and late onset tobacco/infrequent marijuana users, shared few associations with the psychological outcomes compared to the non-or-experimental tobacco/marijuana users. The exceptions were weak associations between membership in the infrequent tobacco/infrequent marijuana use group and an increased likelihood of depression and between membership in the late onset tobacco/infrequent marijuana use group and an increased likelihood of rebellion.
The specific psychological outcomes of antisocial behavior, poor self control, and internalizing problems demonstrated unique associations with trajectory group membership which we will address in detail. With regard to antisocial behavior, membership in groups consisting of infrequent tobacco/late onset marijuana users and chronic tobacco/chronic marijuana users, compared to membership in the non-or-experimental tobacco/marijuana use group, predicted an increased likelihood of both risk taking and rebellion in adulthood. Membership in the chronic tobacco/maturing out marijuana use group also showed a strong association with rebellion in adulthood compared to the non-or-experimental tobacco/marijuana use group. Overall, the antisocial behavior dimension was the most prominent outcome of membership in the groups consisting of infrequent tobacco/late onset marijuana users and chronic tobacco/chronic marijuana users. The same was also true for the chronic tobacco/maturing out marijuana users. Substance use and antisocial behavior are both part of the problem behavior construct in Problem Behavior Theory (48). The theory proposes that involvement in one of these problem behaviors increases the likelihood of involvement in other problem behaviors over time by adversely affecting elements of the individual’s personality, social interactions, and environment. In this way, tobacco and marijuana use may facilitate antisocial behavior by exposing the individual to a range of risk factors for externalizing behavior. One specific mechanism for the relationship of substance use to antisocial behavior is the peer group. The peers who share in substance use behaviors with the substance using individual are also more likely to demonstrate antisocial behavior themselves, and these behaviors likely serve to normalize antisocial behaviors for the individual (49).
With regard to self control, the group of infrequent tobacco/late onset marijuana users did not demonstrate a higher level of impulsivity beyond that of the non-or-experimental tobacco/marijuana use group. However, the chronic tobacco/chronic marijuana users did show a higher level of impulsivity in comparison to the non-or-experimental tobacco/marijuana use group. Likewise, the chronic tobacco/maturing out marijuana users also demonstrated a higher level of impulsivity relative to the non-or-experimental tobacco/marijuana users. The results for the chronic tobacco/chronic marijuana use group and the chronic tobacco/maturing out marijuana use group suggest that trajectories of substance use may serve to increase poor self control. Flory (18) and Piechatzek (19) have suggested a physiological mechanism for this relationship in which substance use disrupts the activity of the frontal lobes and frontostriatal circuits related to executive functioning. Another mechanism for the association of substance use in the chronic tobacco/chronic marijuana use group with poor self-control is the amotivational syndrome (50), in which marijuana use induces apathy and a reduced capacity to carry out long-term plans. The association of a history of substance use with poor self control is important to address as research suggests that this is likely a bi-directional relationship (12), in which an increased likelihood of poor self-control will serve to perpetuate substance use in the future.
Internalizing problems were associated with membership in groups consisting of infrequent tobacco/late onset marijuana users and chronic tobacco/chronic marijuana users, compared to the non-or-experimental tobacco/marijuana use group. Internalizing problems were also associated with membership in the group of chronic tobacco/maturing out marijuana users relative to the group of non-or-experimental tobacco/marijuana users. The internalizing problem most strongly predicted by membership in each of these groups was an increased likelihood of depression. Silberg, Rutter, D’Onofrio, and Eaves (51) have suggested that the relationship of substance use to later depression may be a result of the operations of both genetic and environmental mechanisms. Pedersen (21) and Hayatbakhsh (27) elaborated on possible mechanisms, such as impaired serotonin functioning and social stigmatism, which may account for this relationship. Another possible mechanism for the increased likelihood of depression is decreased family bonds resulting from persistent substance use. Problems with a spouse who disapproves of tobacco and marijuana use can serve to increase the likelihood of depression (52). Anxiety and interpersonal hypersensitivity were also predicted by membership in the chronic tobacco/chronic marijuana use group and in the chronic tobacco/maturing out marijuana use group, relative to membership in the non-or-experimental tobacco/marijuana use group.
This study has some limitations which are inherent to this type of research. Data are based on measures of self-report and are not verified by an additional source. However, studies have shown that self-report data can yield reliable results (53). Also, we did not control for several factors such as adult role stress which might mediate the relationship between tobacco and marijuana use and antisocial behavior, poor self control, and internalizing problems. Future studies should explore additional outcomes of comorbid trajectories of tobacco and marijuana use in domains such as these.
The results have implications for treatment interventions. As we have previously suggested (38), the data indicate a need for tobacco and marijuana cessation programs to identify and address the comorbid use of tobacco and marijuana. Furthermore, programs focused on treatment for the use of these substances should work to address likely psychological outcomes of a history of comorbid use of the substances such as antisocial behavior, poor self control and internalizing problems. Finally, future research should focus on understanding how trajectories of comorbid disorders are connected with functioning in a variety of other areas.
Acknowledgments
This work was supported by a Research Scientist Award [DA00244] and a research grant [DA005702] from the National Institutes of Drug Abuse, and by a research grant from the National Cancer Institute [CA084063]. The National Institutes of Drug Abuse and the National Cancer Institute were not involved in the design and conduct of the study; the collection, management, analysis, and interpretation of the data, or the preparation, review, and approval of the manuscript. The authors thank Dr. Martin Whiteman and David W. Brook, M.D. for critical review of the manuscript.
References
- 1.Richter KP, Kaur H, Resnicow K, Nazir N, Mosier MC, Ahluwalia JS. Cigarette smoking among marijuana users in the United States. Subst Abus. 2004;25:35–43. doi: 10.1300/j465v25n02_06. [DOI] [PubMed] [Google Scholar]
- 2.Lai S, Lai H, Page JB, McCoy CB. The association between cigarette smoking and drug abuse in the United States. J Addict Dis. 2000;19:11–24. doi: 10.1300/J069v19n04_02. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results from the 2007 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Office of Applied Studies; 2008. [Google Scholar]
- 4.Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374:1383–1391. doi: 10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- 5.Vianna EO, Gutierrez MRP, Barbieri MA, Caldeira RD, Bettiol H, Da Silva AAM. Respiratory effects of tobacco smoking among young adults. Am J Med Sci. 2008;336:44–49. doi: 10.1097/MAJ.0b013e31815c3b47. [DOI] [PubMed] [Google Scholar]
- 6.Sweis R, Berry JD, Ning H, Dyer AR, Lloyd-Jones DM. Lifetime risks for cardiovascular and non-cardiovascular disease endpoints by smoking status in men and women at selected ages: The cardiovascular lifetime risk pooling project. Circulation. 2009;120:S432. [Google Scholar]
- 7.Hall W, Degenhardt L, Lynskey M. The Health and Psychological Effects of Cannabis Use. (National Drug Strategy Monograph No. 25) Australia: University of New South Wales, National Drug and Alcohol Research Centre; 2001. [Google Scholar]
- 8.Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: A review of prospective behavioural studies. Addiction. 2006;101:948–958. doi: 10.1111/j.1360-0443.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- 9.Taylor DR, Fergusson DM, Milne BJ, Horwood LJ, Moffitt TE, Sears MR, Poulton R. A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction. 2002;97:1055–1061. doi: 10.1046/j.1360-0443.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- 10.Brook JS, Brook DW, Gordon AS, Whiteman M, Cohen P. The psychosocial etiology of adolescent drug use: A family interactional approach. Genet Soc Gen Psychol Monogr. 1990;116:111–267. [PubMed] [Google Scholar]
- 11.Frick PJ, Viding E. Antisocial behavior from a developmental psychopathology perspective. Dev Psychopathol. 2009;21:1111–1131. doi: 10.1017/S0954579409990071. [DOI] [PubMed] [Google Scholar]
- 12.Wills TA, Stoolmiller M. The role of self-control in early escalation of substance use: A time-varying analysis. J Consult Clin Psychol. 2002;70:986–997. doi: 10.1037//0022-006x.70.4.986. [DOI] [PubMed] [Google Scholar]
- 13.Achenbach TM. Manual for the Child Behavior Checklist 4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 14.McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. Am J Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- 15.Tucker JS, Martínez JF, Ellickson PL, Edelen MO. Temporal associations of cigarette smoking with social influences, academic performance, and delinquency: A four-wave longitudinal study from ages 13–23. Psychol Addict Behav. 2008;22:1–11. doi: 10.1037/0893-164X.22.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Keyes MA, Iacono WG, McGue M. Early onset problem behavior, young adult psychopathology, and contextual risk. Twin Res Hum Genet. 2006;10:45–53. doi: 10.1375/twin.10.1.45. [DOI] [PubMed] [Google Scholar]
- 17.Fergusson DM, Horwood LJ, Swain-Campbell N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97:1123–1135. doi: 10.1046/j.1360-0443.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- 18.Flory JD, Manuck SB. Impulsiveness and cigarette smoking. Psychosom Med. 2009;71:431–437. doi: 10.1097/PSY.0b013e3181988c2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piechatzek M, Indlekofer F, Daamen M, Glasmacher C, Lieb R, Pfister H, Tucha O, Lange KW, Wittchen H-U, Schütz CG. Is moderate substance use associated with altered executive functioning in a population-based sample of young adults? Hum Psychopharmacol. 2009;24:650–665. doi: 10.1002/hup.1069. [DOI] [PubMed] [Google Scholar]
- 20.Kollins SH. Delay discounting is associated with substance use in college students. Addict Behav. 2003;28:1167–1173. doi: 10.1016/s0306-4603(02)00220-4. [DOI] [PubMed] [Google Scholar]
- 21.Pedersen W, von Soest T. Smoking, nicotine dependence and mental health among young adults: A 13-year population-based longitudinal study. Addiction. 2009;104:129–137. doi: 10.1111/j.1360-0443.2008.02395.x. [DOI] [PubMed] [Google Scholar]
- 22.Klungsøyr O, Nygård JF, Sørensen T, Sandanger I. Cigarette smoking and incidence of first depressive episode: An 11-year, population-based follow-up study. Am J Epidemiol. 2006;163:421–432. doi: 10.1093/aje/kwj058. [DOI] [PubMed] [Google Scholar]
- 23.Cuijpers P, Smit F, ten Have M, de Graaf R. Smoking is associated with first-ever incidence of mental disorders: A prospective population-based study. Addiction. 2007;102:1303–1309. doi: 10.1111/j.1360-0443.2007.01885.x. [DOI] [PubMed] [Google Scholar]
- 24.Schuetze P, Eiden RD, Dombkowski L. The association between cigarette smoking during pregnancy and maternal behavior during the neonatal period. Infancy. 2006;10:267–288. [PMC free article] [PubMed] [Google Scholar]
- 25.van Laar M, van Dorsselaer S, Monshouwer K, de Graaf R. Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population? Addiction. 2007;102:1251–1260. doi: 10.1111/j.1360-0443.2007.01875.x. [DOI] [PubMed] [Google Scholar]
- 26.Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: Cohort study. Br Med J. 2002;325:1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W. Cannabis and anxiety and depression in young adults: A large prospective study. J Am Acad Child Adolesc Psychiatry. 2007;46:408–417. doi: 10.1097/chi.0b013e31802dc54d. [DOI] [PubMed] [Google Scholar]
- 28.Aragona M, Onesti E, Tomassini V, Conte A, Gupta S, Gilio F, Pantano P, Pozzilli C, Inghilleri M. Psychopathological and cognitive effects of therapeutic cannabinoids in multiple sclerosis: A double-blind, placebo controlled, crossover study. Clin Neuropharmacol. 2009;32:41–47. doi: 10.1097/WNF.0B013E3181633497. [DOI] [PubMed] [Google Scholar]
- 29.Dumenci L, Windle M. Cluster analysis as a method of recovering types of intraindividual growth trajectories: A Monte Carlo study. Multivariate Behav Res. 2001;36:501–522. doi: 10.1207/S15327906MBR3604_02. [DOI] [PubMed] [Google Scholar]
- 30.Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Dev Psychopathol. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- 31.Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug Alcohol Depend. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J Consult Clin Psychol. 2004;72:400–410. doi: 10.1037/0022-006X.72.3.400. [DOI] [PubMed] [Google Scholar]
- 33.Chassin L, Presson CC, Sherman SJ, Pitts SC. The natural history of cigarette smoking from adolescence to adulthood in a Midwestern community sample: Multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19:223–231. [PubMed] [Google Scholar]
- 34.Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: Predictors and outcomes. Dev Psychopathol. 2004;16:1007–1027. doi: 10.1017/s0954579404040118. [DOI] [PubMed] [Google Scholar]
- 35.Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult alcohol and tobacco use. J Abnorm Psychol. 2005;114:612–626. doi: 10.1037/0021-843X.114.4.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orlando M, Tucker JS, Ellickson PL, Klein DJ. Concurrent use of alcohol and cigarettes from adolescence to young adulthood: An examination of developmental trajectories and outcomes. Subst Use Misuse. 2005;40:1051–1069. doi: 10.1081/JA-200030789. [DOI] [PubMed] [Google Scholar]
- 37.Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult substance use. Alcohol Clin Exp Res. 2008;32:723–737. doi: 10.1111/j.1530-0277.2008.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brook JS, Lee JY, Finch SJ, Brown EN. Course of comorbidity of tobacco and marijuana use: Psychosocial risk factors. Nicotine Tob Res. 2010;12:474–482. doi: 10.1093/ntr/ntq027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brook JS, Whiteman M, Czeisler LJ, Shapiro J, Cohen P. Cigarette smoking in young adults: Childhood and adolescent personality, familial, and peer antecedents. J Genet Psychol. 1997;158:172–188. doi: 10.1080/00221329709596660. [DOI] [PubMed] [Google Scholar]
- 40.Crawford TN, Cohen P, Brook JS. Dramatic-erratic personality disorder symptoms: II. Developmental pathways from early adolescence to adulthood. J Pers Disord. 2001;15:336–350. doi: 10.1521/pedi.15.4.336.19185. [DOI] [PubMed] [Google Scholar]
- 41.Jackson DN. Jackson Personality Inventory-Revised Manual. Port Heron, MI: Sigma Assessment Systems, Inc; 1997. [Google Scholar]
- 42.Smith GM, Fogg CP. Psychological antecedents of teenage drug use. In: Simmons R, editor. Research in Community and Mental Health: An Annual Compilation of Research. Vol. 1. Greenwich, CT: JAI; 1979. pp. 87–102. [Google Scholar]
- 43.Derogatis LR. Symptoms Checklist 90-R Administration, Scoring Procedures Manual. 3. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- 44.Muthén LK, Muthén BO. Mplus User’s Guide. 4. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 45.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 46.Cody RP, Smith JK. Applied Statistics and the SAS Programming Language. 5. Upper Saddle River, NJ: Prentice-Hall, Inc; 2005. [Google Scholar]
- 47.Bretteville-Jensen AL, Melberg HO, Jones AM. Sequential patterns of drug use initiation: Can we believe in the gateway theory? B E J Econom Anal Policy. 2008;8:1–29. [Google Scholar]
- 48.Jessor R, Donovan JE, Costa FM. Beyond Adolescence: Problem Behavior and Young Adult Development. Cambridge, UK: Cambridge University Press; 1991. [Google Scholar]
- 49.Kaufmann DR, Wyman PA, Forbes-Jones EL, Barry J. Prosocial involvement and antisocial peer affiliations as predictors of behavior problems in urban adolescents: Main effects and moderating effects. J Commun Psychol. 2007;35:417–434. [Google Scholar]
- 50.McGlothin WH, West LJ. The marihuana problem: An overview. Am J Psychiatry. 1968;125:126–134. [PubMed] [Google Scholar]
- 51.Silberg J, Rutter M, D’Onofrio B, Eaves L. Genetic and environmental risk factors in adolescent substance use. J Child Psychol Psychiatry. 2003;44:664–676. doi: 10.1111/1469-7610.00153. [DOI] [PubMed] [Google Scholar]
- 52.Choi H, Marks NF. Marital conflict, depressive symptoms, and functional impairment. J Marriage Fam. 2008;70:377–390. doi: 10.1111/j.1741-3737.2008.00488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mennes CE, Abdallah AB, Cottler LB. The reliability of self-reported cannabis abuse, dependence and withdrawal symptoms: Multisite study of differences between general population and treatment groups. Addict Behav. 2009;34:223–226. doi: 10.1016/j.addbeh.2008.10.003. [DOI] [PubMed] [Google Scholar]