Abstract
Microvascular rarefaction, defined by a loss of terminal arterioles, small venules and/or capillaries, is a common characteristic of the hypertension syndrome. While rarefaction has been associated with vessel specific free radical production, deficient leukocyte adhesion, and cellular apoptosis, the relationships of rarefaction with structural alterations at the network and cellular level remain largely unexplored. The objective of this study was to examine the architecture and perivascular cell phenotypes along microvascular networks in hypertensive versus normotensive controls in the context of imbalanced angiogenesis. Mesenteric tissues from age-matched adult male spontaneously hypertensive (SHR) and Wistar-Kyoto (WKY) rats were harvested and immnolabeled for PECAM and neuron-glia antigen 2 (NG2). Evaluation of intact rat mesenteric microvascular networks rats suggests that network alterations associated with hypertension are more complex than just a loss of vessels. Typical SHR versus WKY networks demonstrate a reduced branching architecture marked by more proximal arteriole/venous anastomoses and an absence of NG2 labeling along arterioles. Although less frequent, larger SHR microvascular networks display regions of dramatically increased vascular density. SHR and WKY lymphatic networks demonstrate increased vessel diameters and vascular density compared to networks in normotensive Wistar rats (the strain from which both the SHR and WKY originated). These observations provide a rationale for investigating the presence of local angiogenic factors and response of microvascular networks to therapies aimed at reversing rarefaction in genetic hypertension.
INTRODUCTION
Hypertension is associated with an increase of microvascular resistance due to two major mechanisms, arteriolar wall remodeling and microvessel rarefaction. Microvascular rarefaction can be classified as one of two types: functional and structural. Functional rarefaction in hypertension refers to non-perfusion of a vessel with blood cells and can be reversed by application of a vasodilator. Structural rarefaction is caused by the actual anatomical loss of microvessels, including small terminal arterioles, small venules and/or capillaries. Given that the development of elevated blood pressure is thought to be accompanied and in some cases preceded by a loss of microvessels (Hutchins and Darnell, 1974; Antonois et al., 2003; Antonois et al., 1999; Noon et al., 1997), therapies aimed at reversing microvascular rarefaction potentially represent candidate treatments of hypertension.
In the spontaneously hypertensive rat (SHR), which represents a model of hypertension with a genetic background, the microcirculation is characterized by smooth muscle medial hyperplasia, smooth muscle hypertrophy, enhanced smooth muscle longitudinal coverage, enhanced microvessel specific oxidative stress, elevated counts of activated circulating leukocytes, enhanced capillary flow resistance, impairment of selectin-mediated leukocyte adhesion, and extensive non-uniform endothelial cell apoptosis (Suematsu et al., 2002; Fukuda et al., 2004). These characteristics represent a complex remodeling scenario across multiple scales. In order to develop a new rational to therapeutically manipulate microvascular rarefaction, a full understanding of whether these vessel specific alterations in hypertension drive vessel loss or are resultants of impaired vessel angiogenesis is warranted. Angiogenesis, defined as the growth of new vessels from existing vessels, is itself dependent on the coordination of multiple mechanical, cellular, and molecular players (Peirce and Skalak, 2003). For the purpose of this chapter the term, angiogenesis, will be used in the general sense and will also encompass the remodeling of existing vessels described by capillary arterialization or arteriogenesis (Peirce and Skalak, 2003).
The objective of this chapter is to examine the architecture and perivascular cell phenotypes along microvascular networks in the SHR and its normotensive control, the Wistar Kyoto (WKY) rat. We present evidence for disturbed angiogenesis in rat mesenteric tissue in hypertension. Evaluation of microvascular architectural patterns and cell alterations in hypertensive animal models serve as the background for future investigation of microvascular dysfunction in this disease.
METHODS
Tissue Collection
All experimental protocols were reviewed and approved by the University of California-San Diego Animal Care and Use Committee. Age-matched adult (16–20 weeks) male spontaneous hypertensive rats (SHR; n=4) and Wistar-Kyoto (WKY; n=4) rats were given general anesthesia with pentobarbital (50 mg /kg b.w., i.m.). Approximately 30 minutes after the initial anesthetic injection, rats were euthanized by pentobarbital (120 mg/kg, intravenous injection via the femoral vein). The mesentery was exteriorized and vascularized sectors, defined as the thin translucent connective tissue in between the mesenteric arterial/venous vessels feeding the bowel, were harvested from each rat. Tissues were preferably harvested from the ileum. The mesenteric tissues were immediately placed in 10mM phosphate buffered saline (PBS), mounted on positively charged glass slides, and fixed for 1 hour in 4% paraformaldehyde at 4°C. The rat mesentery was selected for this study because it allows for 2-dimensional visualization of entire intact microvascular networks down to the single cell level.
In-situ Immunohistochemistry
Similar to methods previously described (Murfee et al., 2007; Murfee et al., 2005), tissue specimens were labeled with one of the following immunolabeling protocols using primary antibodies against: A) platelet endothelial adhesion molecule (PECAM; CD31); or B) PECAM + neuron-glia antigen 2 (NG2). For the PECAM group 2 tissues were labeled per animal. For PECAM + NG2 group, 7 tissues from 3 SHR animals and 4 tissues from 3 WKY animals were labeled. All labeling steps were followed by at least three rinses with PBS + 0.1% Saponin (10 min each), except after the developing steps, which was followed by incubation in either distilled water (Vector Red) or PBS (Vector SG) for 5 minutes.
PECAM labeling
1) 1 hour incubation at room temperature with 1:200 mouse monoclonal biotinylated CD31 (BD PharMingen) antibody diluted in antibody buffer (0.1% Saponin in PBS + 2% BSA); 2) 1 hour incubation at room temperature with streptavidin-peroxidase secondary antibody solution (VECTASTAIN Elite ABC; Vector Laboratories); and 3) 15–20 minute incubation at room temperature with Vector Nova Red (Vector Laboratories) substrate.
PECAM + NG2 labeling
1) 20 minute incubation in 2.5% normal horse blocking serum (ImmPRESS Kit, Vector laboratories); 2) 1.5 hour incubation at room temperature with 1:100 or 1:200 rabbit polyclonal NG2 antibody (a gift from Dr. Bill Stallcup, Burnham Institute, La Jolla, CA) diluted in antibody buffer; 3) 1 hour incubation at room temperature with a peroxidase horse anti-rabbit secondary solution (Impress kit, Vector Laboratories); 4) incubation for 5–10 minutes at room temperature with Vector Nova Red (Vector Laboratories) substrate.; 5) Overnight incubation at 4°C with 1:200 mouse monoclonal biotinylated CD31 antibody (BD Pharmingen) diluted in antibody buffer; 6) 1 hour incubation at room temperature with streptavidin-peroxidase secondary antibody solution (VECTASTAIN Elite ABC; Vector Laboratories); 7) 10–20 minute incubation at room temperature with Vector SG (Vector Laboratories) substrate.
Microvascular Network Evaluation and Image Acquisition
Mesenteric microvascular networks were examined with an inverted microscope (Olympus IX71) with an Olympus 10×/numerical aperture (NA) = 0.3 and Olympus 20×/NA = 0.4. Images were captured using a similar microscope system (Olympus IX70), a Cooke 5x/numerical aperture (NA) = 0.15, CCD camera and a Scion frame grabber or an upright microscope (Olympus BX60), an Olympus 10×/NA = 0.3 or Olympus 40×/NA = 0.75, and a SPOT Insight camera. For the purpose of this study, microvascular networks were defined as having at least one arteriole/venule vessel pair originating from the periphery of the mesenteric connective tissue connecting to a branching vasculature and being isolated from another network. Small networks were classified as spanning an area less than 1 10× field of view. Larger networks were classified as spanning an area greater than 1 10× field of view and in some cases included multiple sub-networks interconnected at the capillary level. Mesenteric tissues were excluded from analysis if they were avascular or did not contain an isolated microvascular network. Arterial and venous vessel identity was determined based on position within the microvascular network, relative vessel diameter, and endothelial cell morphology. An arterial/venous (A/V) anastomosis was defined by direct connection between an arteriole and a venule. Capillaries were identified based on either vessel diameter (<10 μm) or blind-ended location. Pericyte specific NG2 positive cell labeling along capillaries was confirmed by identification of the typical elongated pericyte morphology (Murfee et al., 2005). Finally, for the evaluation of lymphatic vessels in the SHR and WKY tissues, additional mesenteric sectors were harvested from adult Wistar rats and immunolabeled for PECAM following the protocol as described above.
RESULTS
In comparison to tissues harvested from WKY rats, SHR mesenteric tissues contain smaller microvascular networks, consistent with previously documented microvascular rarefaction in other organs of the SHR (Chen et al., 1981; Greene et al., 1990; Hutchins and Darnell, 1974; Kobayashi et al., 2005; Prewitt et al., 1982). 15/15 SHR isolated networks from 6 tissues were classified as small defined by being contained to a 10× field of view. A 7th tissue contained 5 larger networks, atypical of the architectures associated with the other tissues and spanning vascular areas greater than a 10 × field of view. In contrast to the small SHR networks, 5/8 WKY networks spanned multiple fields of view. 5/6 WKY tissues contained these dramatically larger networks. Overall fewer WKY networks were observed because, based on our definition, an isolated network could consist of multiple interconnected sub-networks.
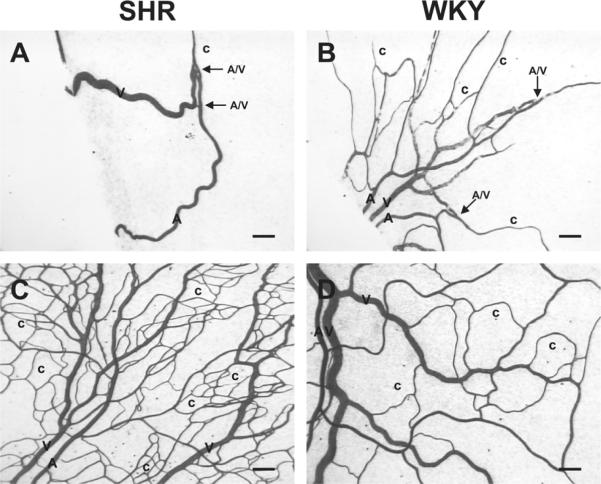
Inspection of microvascular architectures within SHR and WKY networks of comparable area served to identify alterations more complex than just a loss of microvessels (Figure 1). Typical small SHR networks had arterial/venous (A/V) anastomoses located proximal to the capillary level and prior to multiple arterial or venule branching (Figure 1A; Figure 2A). As a consequence, these networks had less of a tree-shape as compared to WKY networks (Figure 1A and 1B). Individual arterial and venous vessels were determined based on position within the microvascular network, relative vessel diameter, and endothelial cell morphology. The larger, but less frequent, SHR microvascular networks displayed an increased capillary density per vascular area (Figure 1C) compared to WKY networks (Figure 1D).
Figure 1.
Representative examples of SHR and WKY adult mesenteric microvascular networks identified by PECAM labeling. Panel A: Typical SHR microvascular networks display arterial/venous anastomoses and a non-branching or non-tree like architecture. Panel B: In comparison, similar size WKY networks display a more-tree like structure and increased vascular density per tissue area. Panel C: Atypical large SHR microvascular networks demonstrate increased vessel density and loop formation when compared to WKY networks (panel D) of comparable area. “A” = arteriole, “V” = venule, “c” = capillary, “A/V” = arterial/venous anastomoses, “L” = lymphatic vessel. Scale bars, 100 μm.
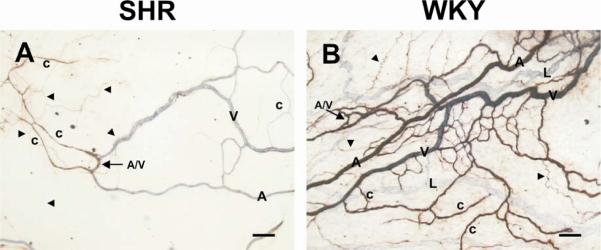
Figure 2.
Representative examples of SHR and WKY adult mesenteric microvascular networks labeled with PECAM (blue) and NG2 (dark red). Panel A) In typical SHR networks, perivascular cells along both arterioles and venules lack positive NG2 labeling. At the capillary level, vascular pericytes expression of NG2 is vessel specific. Panel B) In comparable WKY microvascular networks positive NG2 labeling is identifies arterioles versus venules and is present along most, if not all, capillaries. “A” = arteriole, “V” = venule, “c” = capillary, “A/V” = arterial/venous anastomoses, “L” = lymphatic vessel. Arrowheads identify NG2 positive nerve cells running along blood vessels or within the interstitial space. Scale bars, 100 μm.
SHR mesenteric microvascular networks also displayed an altered perivascular cell NG2 expression pattern. In typical small SHR networks, NG2 labeling did not identify smooth muscle cells, wrapping around arterioles or venules (Figure 2A). In comparably sized WKY networks, NG2 expression identified smooth muscle cells wrapping around arterioles and pericytes along most, if not all, capillaries (Figure 2B). In the SHR networks NG2-positive labeling is present only on a subset of capillaries (Figure 2A). Pericyte specific NG2-positive cell labeling along capillaries was confirmed by identification of the characteristic elongated, wrapping morphology (Figure 3; Murfee et al., 2005). These NG2 labeling patterns seemed to be associated with the SHR and WKY architectural differences. In one example of a typical SHR small network observed in a WKY tissue, NG2 expression patterns were similar to the SHR.
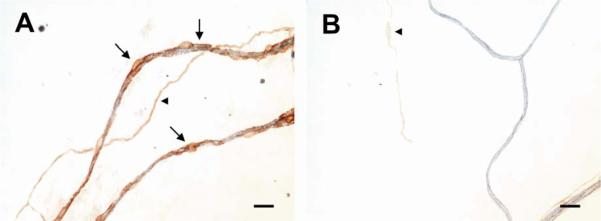
Figure 3.
Vascular pericyte identification along capillaries in SHR microvascular networks. Panel A) NG2 positive (dark red) labeling identifies pericytes (arrows), which wrap and elongate along the PECAM positive (blue) endothelial lined capillaries. Panel B) Along PECAM positive (blue) capillaries lacking pericytes, no observable NG2 labeling is observes. Note both images represent higher magnification, rotated views of vessels in Figure 2A. Arrowheads identify NG2 positive nerve cells. Scale bars, 20 μm.
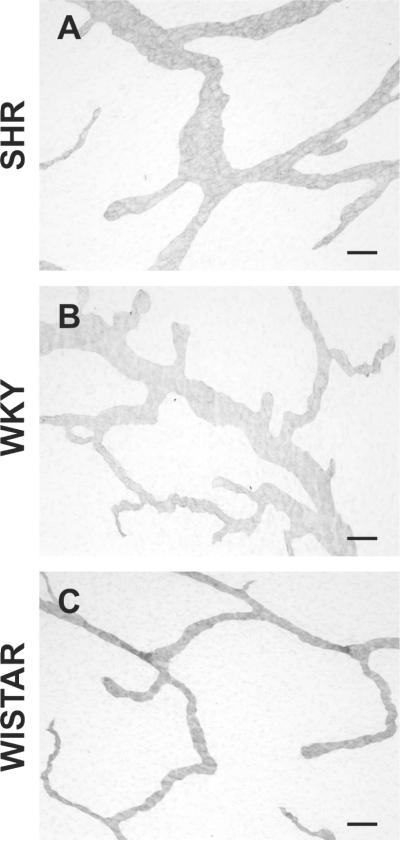
In addition to the blood vascular endothelial cells, PECAM labeling in rat mesenteric tissues also identified lymphatics endothelial cells. Lymphatic vessels were distinguishable from blood vessels by diameter, decreased PECAM labeling intensity, and endothelial cell morphology (Murfee et al., 2007). We observed significant structural differences in initial lymphatic vessels, including increased diameters and altered branching patterns, in SHR and WKY mesenteric tissues compared to tissues harvested from adult Wistar rats (Figure 4). The Wistar strain represents an alternative normotensive control given that it is the origin for both the SHR and the WKY and that the WKY, in spite of its lower blood pressure relative to the SHR, is still slightly hypertensive (DeLano et al., 2005).
Figure 4.
Representative examples of terminal lymphatic vessels labeled with PECAM in adult SHR, WKY, and WISTAR mesenteric tissues. In general, lymphatic vessels in SHR (Panel A) and WKY (Panel B) networks demonstrate increased diameters and increased branching patterns as compared to Wistar (Panel C) vessels. Scale bars, 100 μm.
DISCUSSION
Microvascular Rarefaction in Hypertension
Structural microvascular rarefaction, defined as an anatomical loss of microvessels, has been well documented in various tissues harvested from hypertensive animals (Seumatsu et al., 2002; Ferdinand et al., 1998; Sane et al., 2004) and is mechanistically supported by evidence for enhanced endothelial cell apoptosis along capillaries in hypertensive networks (Gobé et al., 1997; Tran and Schmid-Schönbein, 2007; Vogt and Schmid-Schönbein, 2001; Suematsu et al., 2002). However, recent evidence suggests that microvascular rarefaction might not be characteristic of all tissues. For example, no changes were found in the number of capillaries in human quadriceps muscle samples harvested from hypertensive patients (Hernandez et al., 1999). In left ventricular tissue, absent numbers of capillaries were found only in micro-areas in NO-deficient hypertensive Wistar rats (Okruhlicova et al., 2005). In SHR animals, rarefaction of arterioles was reported not to occur in either the pial vasculature (Werber et al., 1990) or the intestine (Bohlen, 1983). Finally, the length of arcade arterioles in spinotrapezius muscle harvested from SHR animals was higher compared to WKY animals (Engelson et al., 1986). Thus, though microvascular rarefaction and cellular apoptosis exist in hypertension, this phenomenon may be in part dependent on local tissue environments.
Signs for Disturbed Angiogenesis in Hypertension
The association of microvascular rarefaction with genetic forms of hypertension implicates angiogenesis as a potential treatment option. However, rarefaction is not characteristic of all tissues (see above). Based on recent evidence of elevated levels of angiogenic growth factors in certain models of hypertension (Sane et al., 2004), evaluation of angiogenesis aimed therapies for treating hypertension and, more broadly, a full understanding of the microcirculation's role in hypertension requires 1) a continued characterization of microvascular architectures in different tissues, 2) characterization of how microvascular network patterns change over the time course of the disease compared to the maturation of networks in tissues harvested normotensive animals and 3) evaluation of angiogenic responses in hypertensive animals at different ages.
As evidence for an altered angiogenic activity during hypertension, hypertensive patients have been reported to have elevated circulating levels of VEGF, bFGF and TGF-β (Sane et al., 2004). In 18 week old SHR versus WKY animals, VEGF mRNA levels and capillary density were significantly higher (Gu et al., 2004). Patients with essential hypertension were found to have elevated plasma VEGF levels when compared to healthy controls (Belgore et al., 2001). In 4-week old SHR animals, implanted fibrin chambers contained more vessels than those implanted into WKY animals (Hudlett et al., 2005). Finally endothelial cell proliferation and increased angiogenesis are common characteristics of pulmonary hypertension (Tuder and Voelkel, 2002).
Disturbed angiogenesis in hypertensive tissues is supported by our observations of local increased vessel density in larger SHR microvascular networks compared to WKY networks of similar areas. From our observations we hypothesize that hypertensive networks in the rat mesentery are hypersensitive to angiogenic stimuli. Investigation of microvascular network structural remodeling during hypertension from an angiogenesis perspective will serve to provide valuable insight for assessing the potential for angiogenesis therapies aimed at reversing microvascular rarefaction.
Microvascular Pattern Alterations in Hypertension
Signs of microvascular network architectural alterations in tissues of hypertensive animals support the concept that microvascular rarefaction is more multivariate that just a loss of vessels. In typical SHR mesenteric networks, we observed non-tree like architectures marked by arterial/venous anastomoses. Whether these structural features are characteristic of younger normotensive networks and merely represent impaired microvascular network maturation remains to be determined, yet their presence do represent an altered network pattern that could influence, blood flow, capillary stasis, cellular apoptosis and the ability of the network to respond to angiogenic stimuli. More importantly, our observations of altered network patterns are supported by the characterization of microvascular structure in other tissues and harvested from adult SHR animals (Engelson et al., 1986). In spinotrapezius muscle, Engelson et al. reported almost twice as many transverse arterioles with shorter branches per unit tissue volume (Engelson et al., 1986). In adult SHR retinas, microvascular networks display abnormal patterning characterized by increased arteriovenous crossings and loop formation (Bhutto et al., 1997). Even in their hallmark paper identifying rarefaction in the cremaster muscle of the SHR, Hutchins and Darnell documented an increased arteriolar tortuosity (Hutchins and Darnell, 1974) and increase in the number of smallest venules.
Our observations in rat mesenteric networks also highlight a potential for increased lymphatic vessel diameter and density in hypertension. The mechanisms for these alterations remain currently unknown. Enhanced lymph flow in myocardial and intestinal tissue has been reported for the one-kidney, one-clip hypertension model (Laine, 1988; Laine and Granger, 1983) and in adult SHR animals mesenteric lymphatic vessels have been reported to exhibit extensive oxygen free radical formation (DeLano et al., 2005.). Though future investigation is required to compare lymphatic function in the SHR, WKY, and alternate normotensive strains, the potential association of altered lymphatic network patterns emphasizes a need to better understand the structural regulation of the microcirculation in various models of hypertension.
Role for Perivascular Cells in Hypertension
Perivascular cells include smooth muscle cells and vascular pericytes, which elongate along endothelial lined capillaries. Pericytes, which make direct membrane contact with endothelial cells (Gerhardt and Betsholtz, 2003) and regulate vessel permeability, vessel diameter, and endothelial cell proliferation (Gerhardt and Betsholtz, 2003; Hellstrom et al., 2001; Leveen et al., 1994), have been identified as critical players in angiogenesis (Gerhardt and Betsholtz, 2003).
Thus, not surprisingly, a role of pericytes has been implicated in hypertension. The number of SM α-actin positive pericytes is increased in SHR versus WKY brains (Herman and Jacobson, 1988). In the retina of SHR rats, Wallow et al. report a decreased number of vascular pericytes with increased coverage along capillaries and increased contractility (Wallow et al., 1993). To our knowledge a comprehensive description of perivascular cell presence, phenotype, and function across multiple tissues harvested from hypertensive animals has not been completed.
Common markers for pericytes include smooth muscle (SM) α-actin, desmin, and PDGFR-β, yet the expression of these markers is not pericyte specific (Gerhardt and Betsholtz, 2003). For example, SM α-actin can be expressed by pericytes, immature smooth muscle cells, which express SM α-actin and not SM myosin heavy chain, and mature smooth muscle cells, which express both contractile proteins (Nehls and Drenckhahn, 1991; Price et al., 1994; Van Gieson et al., 2003; Yoshida and Owens, 2005). Desmin and PDGF-β can also be expressed by smooth muscle cells and interstitial fibroblasts (Nehls et al., 1992). Further complicating the issue of pericyte identification, expression of the various markers differs depending on species, tissue, and even developmental stage. Thus, characterization of perivascular cells in hypertensive microvascular networks entails a multi-faceted approach involving morphological, phenotypic, and function descriptions.
Recently NG2 (neuron-glia antigen 2), the rat homologue of the Human Melanoma Proteoglycan (HMP), has been characterized as a pericyte maker (Ozerdem et al., 2001; Ozerdem et al., 2002). In quiescent rat mesenteric tissues NG2 labeling identifies smooth muscle cells along arterioles and vascular pericytes along all capillary vessels, yet not by smooth muscle cells along venules (Murfee et al., 2005). Our observations in typical SHR mesenteric networks indicate that a subset of capillaries are covered by NG2-positive pericytes and that pre- and post-capillary vessels positive for SM α-actin expression (data not shown) lack NG2 arterial/venous identification. Further investigation is needed to determine the functional implications of altered NG2 labeling patterns and arterial/venous identity on microvascular network development in the adult.
SUMMARY
In summary the results presented in this chapter indicate that mesenteric microvascular networks in spontaneously hypertensive rats are characterized by architectural and perivascular cell phenotype alterations in comparison to normotensive networks. These qualitative observations support an emerging paradigm that microvascular rarefaction is more complex than just a loss of vessels or apoptosis of endothelial cells and is associated with imbalanced angiogenesis. In the context of designing therapies to promote angiogenesis aimed at reversing vessel loss, this study highlights the importance for future quantitative description of the local tissue environments in microvascular networks over the time course of aging in hypertensive animals.
Acknowledgement
Supported by NHLBI Grant HL 10881
REFERENCES
- Antonios TF, Rattray FM, Singer DR, Markandu ND, Mortimer PS, MacGregor GA. Rarefaction of skin capillaries in normotensive offspring of individuals with essential hypertension. Heart. 2003;89(2):175–178. doi: 10.1136/heart.89.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonios TF, Singer DR, Markandu ND, Mortimer PS, MacGregor GA. Rarefaction of skin capillaries in borderline essential hypertension suggests an early structural abnormality. Hypertension. 1999;34(4 Pt 1):655–658. doi: 10.1161/01.hyp.34.4.655. [DOI] [PubMed] [Google Scholar]
- Belgore FM, Blann AD, Li-Saw-Hee FL, Beevers DG, Lip GY. Plasma levels of vascular endothelial growth factor and its soluble receptor (SFlt-1) in essential hypertension. Am. J. Cardiol. 2001;87(6):805–807. A9. doi: 10.1016/s0002-9149(00)01512-5. [DOI] [PubMed] [Google Scholar]
- Bhutto IA, Amemiya T. Vascular changes in retinas of spontaneously hypertensive rats demonstrated by corrosion casts. Ophthalmic Res. 1997;29(1):12–23. doi: 10.1159/000267986. [DOI] [PubMed] [Google Scholar]
- Bohlen HG. Intestinal microvascular adaptation during maturation of spontaneously hypertensive rats. Hypertension. 1983;5(5):739–745. doi: 10.1161/01.hyp.5.5.739. [DOI] [PubMed] [Google Scholar]
- Chen II, Prewitt RL, Dowell RF. Microvascular rarefaction in spontaneously hypertensive rat cremaster muscle. Am. J. Physiol. 1981;241(3):H306–H310. doi: 10.1152/ajpheart.1981.241.3.H306. [DOI] [PubMed] [Google Scholar]
- DeLano FA, Balete R, Schmid-Schönbein GW. Control of oxidative stress in the microcirculation of the spontaneously hypertensive rat. Am. J. Physiol. Heart Circ. Physiol. 2005;288:H805–H812. doi: 10.1152/ajpheart.00696.2004. [DOI] [PubMed] [Google Scholar]
- Engelson ET, Schmid-Schönbein GW, Zweifach BW. The microvasculature in skeletal muscle. II. Arteriolar network anatomy in normotensive and spontaneously hypertensive rats. Microvasc. Res. 1986;31(3):356–374. doi: 10.1016/0026-2862(86)90024-5. [DOI] [PubMed] [Google Scholar]
- Fukuda F, Yasu T, Kobayashi N, Ikeda N, Schmid-Schönbein GW. Contribution of fluid shear response in leukocyte to hemodynamic resistance in the spontaneously hypertensive rat. Circ. Res. 2004;95:100–108. doi: 10.1161/01.RES.0000133677.77465.38. [DOI] [PubMed] [Google Scholar]
- Gerhardt H, Betsholtz C. Endothelial-pericyte interactions in angiogenesis. Cell Tissue Res. 2003;314:15–23. doi: 10.1007/s00441-003-0745-x. [DOI] [PubMed] [Google Scholar]
- Gobé G, Browning J, Howard T, Hogg N, Winterford C, Cross R. Apoptosis occurs in endothelial cells during hypertension-induced microvascular rarefaction. J. Struct. Biol. 1997;118:63–72. doi: 10.1006/jsbi.1996.3835. [DOI] [PubMed] [Google Scholar]
- Greene AS, Lombard JH, Cowleym AW, Jr., Hansen-Smith FM. Microvessel changes in hypertension measured by Griffonia simplicifolia I lectin. Hypertension. 1990;15(6 Pt 2):779–783. doi: 10.1161/01.hyp.15.6.779. [DOI] [PubMed] [Google Scholar]
- Gu JW, Fortepiani LA, Reckelhoff JF, Adair TH, Wang J, Hall JE. Increased expression of vascular endothelial growth factor and capillary density in hearts of spontaneously hypertensive rats. Microcirculation. 2004;11(8):689–697. doi: 10.1080/10739680490517749. [DOI] [PubMed] [Google Scholar]
- Hellstrom M, Kalen M, Lindahl P, Abramsson A, Betsholtz C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development. 1999;126:3047–3055. doi: 10.1242/dev.126.14.3047. [DOI] [PubMed] [Google Scholar]
- Herman IM, Jacobson S. In situ analysis of microvascular pericytes in hypertensive rat brains. Tissue Cell. 1988;20(1):1–12. doi: 10.1016/0040-8166(88)90002-x. [DOI] [PubMed] [Google Scholar]
- Hernández N, Torres SH, Finol HJ, Vera O. Capillary changes in skeletal muscle of patients with essential hypertension. Anat. Rec. 1999;256(4):425–432. doi: 10.1002/(SICI)1097-0185(19991201)256:4<425::AID-AR9>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Hudlett P, Neuville A, Miternique A, Griffon C, Weltin D, Stephan D. Angiogenesis and arteriogenesis are increased in fibrin gel chambers implanted in prehypertensive spontaneously hypertensive rats. J. Hypertens. 2005;23(8):1559–1564. doi: 10.1097/01.hjh.0000174607.18780.62. [DOI] [PubMed] [Google Scholar]
- Hutchins PM, Darnell AE. Observations of a decreased number of small arterioles in spontaneously hypertensive rats. Circ. Res. 1974;34–35(suppl 1):161–165. [Google Scholar]
- Kobayashi N, DeLano FA, Schmid-Schönbein GW. Oxidative stress promotes endothelial cell apoptosis and loss of microvessels in the spontaneously hypertensive rats. Arterioscler. Thromb. Vasc. Biol. 2005;25(10):2114–2121. doi: 10.1161/01.ATV.0000178993.13222.f2. [DOI] [PubMed] [Google Scholar]
- Laine GA. Microvascular changes in the heart during chronic arterial hypertension. Circ. Res. 1988;62(5):953–960. doi: 10.1161/01.res.62.5.953. [DOI] [PubMed] [Google Scholar]
- Laine GA, Granger HJ. Permeability of intestinal microvessels in chronic arterial hypertension. Hypertension. 1983;5(5):722–727. doi: 10.1161/01.hyp.5.5.722. [DOI] [PubMed] [Google Scholar]
- le Noble FA, Stassen FR, Hacking WJ, Struijker Boudier HA. Angiogenesis and hypertension. J. Hypertens. 1998;16(11):1563–1572. doi: 10.1097/00004872-199816110-00001. [DOI] [PubMed] [Google Scholar]
- Leveen P, Pekny M, Gebre-Medhin S, Swolin B, Larsson E, Betsholtz C. Mice deficient for PDGF B show renal, cardiovascular, and hematological abnormalities. Genes Dev. 1994;8:1875–1887. doi: 10.1101/gad.8.16.1875. [DOI] [PubMed] [Google Scholar]
- Murfee WL, Rappleye JW, Ceballos M, Schmid-Schönbein GW. Discontinuous expression of endothelial cell adhesion molecules along initial lymphatic vessels in mesentery: the primary valve structure. Lymphat. Res. Biol. 2007;5(2):81–89. doi: 10.1089/lrb.2007.1005. [DOI] [PubMed] [Google Scholar]
- Murfee WL, Skalak TC, Peirce SM. Differential arterial/venous expression of NG2 proteoglycan in perivascular cells along microvessels: identifying a venule-specific phenotype. Microcirculation. 2005;12(2):151–160. doi: 10.1080/10739680590904955. [DOI] [PubMed] [Google Scholar]
- Nehls V, Denzer K, Drenckhahn D. Pericyte involvement in capillary sprouting during angiogenesis in situ. Cell Tissue Res. 1992;270:469–474. doi: 10.1007/BF00645048. [DOI] [PubMed] [Google Scholar]
- Nehls V, Drenckhahn D. Heterogeneity of microvascular pericytes for smooth muscle alpha-actin. J. Cell Biology. 1991;113:147–154. doi: 10.1083/jcb.113.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noon JP, Walker BR, Webb DJ, Shore AC, Holton DW, Edwards HV, Watt GC. Impaired microvascular dilatation and capillary rarefaction in young adults with a predisposition to high blood pressure. J. Clin. Invest. 1997;99(8):1873–1879. doi: 10.1172/JCI119354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okruhlicova L, Tribulova N, Weismann P, Sotnikova R. Ultrastructure and histochemistry of rat myocardial capillary endothelial cells in response to diabetes and hypertension. Cell Res. 2005;15(7):532–538. doi: 10.1038/sj.cr.7290322. [DOI] [PubMed] [Google Scholar]
- Ozerdem U, Grako KA, Dahlin-Huppe K, Monosov E, Stallcup WB. NG2 proteoglycan is expressed exclusively by mural cells during vascular morphogenesis. Develop. Dyn. 2001;222:218–227. doi: 10.1002/dvdy.1200. [DOI] [PubMed] [Google Scholar]
- Ozerdem U, Monosov E, Stallcup WB. NG2 proteoglycan expression by pericytes in pathological microvasculature. Microvasc. Res. 2002;63:129–134. doi: 10.1006/mvre.2001.2376. [DOI] [PubMed] [Google Scholar]
- Peirce SM, Skalak TC. Microvascular remodeling: a complex continuum spanning angiogenesis to arteriogenesis. Microcirculation. 2003;10(1):99–111. doi: 10.1038/sj.mn.7800172. [DOI] [PubMed] [Google Scholar]
- Prewitt RL, Chen II, Dowell R. Development of microvascular rarefaction in the spontaneously hypertensive rat. Am. J. Physiol. 1982;243(2):H243–H251. doi: 10.1152/ajpheart.1982.243.2.H243. [DOI] [PubMed] [Google Scholar]
- Price RJ, Owens GK, Skalak TC. Immunohistochemical identification of arteriolar development using markers of smooth muscle differentiation. Evidence that capillary arterialization proceeds from terminal arterioles. Circ. Res. 1994;75:520–527. doi: 10.1161/01.res.75.3.520. [DOI] [PubMed] [Google Scholar]
- Sane DC, Anton L, Brosnihan KB. Angiogenic growth factors and hypertension. Angiogenesis. 2004;7(3):193–201. doi: 10.1007/s10456-004-2699-3. [DOI] [PubMed] [Google Scholar]
- Suematsu M, Suzuki H, Delano FA, Schmid-Schönbein GW. The inflammatory aspect of the microcirculation in hypertension: oxidative stress, leukocytes/endothelial interaction, apoptosis. Microcirculation. 2002;9(4):259–276. doi: 10.1038/sj.mn.7800141. [DOI] [PubMed] [Google Scholar]
- Tran ED, Schmid-Schönbein GW. An In-Vivo Analysis of Capillary Stasis and Endothelial Apoptosis in a Model of Hypertension. Microcirculation. 2007;14(8):793–804. doi: 10.1080/10739680701419992. [DOI] [PubMed] [Google Scholar]
- Tuder RM, Voelkel NF. Angiogenesis and pulmonary hypertension: a unique process in a unique disease. Antioxid. Redox. Signal. 2002;4(5):833–843. doi: 10.1089/152308602760598990. [DOI] [PubMed] [Google Scholar]
- Van Gieson EJ, Murfee WL, Skalak TC, Price RJ. Enhanced smooth muscle cell coverage of microvessels exposed to increased hemodynamic stresses in vivo. Circ. Res. 2003;92:929–936. doi: 10.1161/01.RES.0000068377.01063.79. [DOI] [PubMed] [Google Scholar]
- Vogt CJ, Schmid-Schönbein GW. Microvascular endothelial cell death and rarefaction in the glucocorticoid-induced hypertensive rat. Microcirculation. 2001;8(2):129–139. [PubMed] [Google Scholar]
- Wallow IH, Bindley CD, Reboussin DM, Gange SJ, Fisher MR. Systemic hypertension produces pericyte changes in retinal capillaries. Invest. Ophthalmol. Vis. Sci. 1993;34(2):420–430. [PubMed] [Google Scholar]
- Werber AH, Fitch-Burke MC, Harrington DG, Shah J. No rarefaction of cerebral arterioles in hypertensive rats. Can. J. Physiol. Pharmacol. 1990;68(4):476–479. doi: 10.1139/y90-067. [DOI] [PubMed] [Google Scholar]
- Yoshida T, Owens GK. Molecular determinants of vascular smooth muscle cell diversity. Circ. Res. 2005;96:280–291. doi: 10.1161/01.RES.0000155951.62152.2e. [DOI] [PubMed] [Google Scholar]