Abstract
The Glasgow Outcome Scale (GOS) and its most recent revision, the GOS–Extended (GOS-E), provide the gold standard for measuring traumatic brain injury (TBI) outcome. The GOS-E exhibits validity when used with adults and some adolescents, but validity with younger children is not established. Because the GOS-E lacks the developmental specificity necessary to evaluate children, toddlers, and infants, we modified the original version to create the GOS-E Pediatric Revision (GOS-E Peds), a developmentally appropriate structured interview, to classify younger patients. The criterion, predictive, and discriminant validity of the GOS-E Peds was measured in 159 subjects following TBI (mild: 36%; moderate: 12%; severe: 50%) at 3 and 6 months after injury. Participants were included from two studies completed at the Pediatric Neurotrauma Center at Children's Hospital of Pittsburgh. We assessed the relationship among GOS-E Peds, the GOS, and the Vineland Adaptive Behavior Scales as well as other standardized measures of functional, behavioral, intellectual, and neuropsychological outcome. Premorbid function was assessed 24–36 h after injury. The GOS-E Peds showed a strong correlation with the GOS at 3 and 6 month time points. Criterion-related validity was also indicated by GOS-E Peds' association with most measures at both time points and at injury severity levels. The 3 month GOS-E Peds was associated with the 6 month GOS-E Peds, everyday function, behavior, and most cognitive abilities. Discriminant validity is suggested by weak correlations between both 3 and 6 month GOS-E Peds and premorbid measures. The GOS-E Peds is sensitive to severity of injury and is associated with changes in TBI sequelae over time. This pediatric revision provides a valid outcome measure in infants, toddlers, children, and adolescents through age 16. Findings support using the GOS-E Peds as the primary outcome variable in pediatric clinical trials.
Key words: children, GOS-E, infants, pediatrics, TBI, toddlers, Vineland Adaptive Behavior Scales
Introduction
Although mortality rates from most critical illnesses have declined precipitously with advances in medical and surgical care, pediatric traumatic brain injury (TBI) remains the leading cause of death and disability for children in all age groups except for infants <1 year of age. Pediatric TBI affects 475,000 children yearly, and leads to 37,000 hospitalizations and >3000 deaths (Langlois and Sattin, 2005; Langlois et al., 2004) Because of medical advances, the focus of clinical care and experimental therapies has necessarily shifted to targeting improved neurological and neuropsychological outcome rather than mortality for benchmarking assessments of quality of care or measuring efficacy of specific treatments and interventions.
There are few pediatric outcome measures specifically developed for patients with TBI, and none to our knowledge that span infancy through adulthood. Perhaps the most widely used pediatric outcome measure in the hospital is the Pediatric Cerebral Performance Scale (PCPC), an instrument modeled after the Glasgow Outcome Scale (GOS) and constructed to measure short-term cognitive disability after life-threatening medical events (Fiser, 1992). This categorical scale was initially developed to assess outcome at discharge from critical care units. To date, studies have yet to establish the predictive validity of the PCPC beyond hospital discharge (Fiser et al., 2000). A clinically accessible, validated tool to determine functional outcome after TBI across the injury spectrum and across all age ranges would be valuable for both clinicians and researchers.
The GOS (Jennett and Bond, 1975) and its revision, the GOS-Extended (GOS-E) (Jennett et al., 1981), provide the gold standard for measuring TBI outcome of adults in clinical trials (Clifton et al., 1992). Although these measures have been shown to provide a valid measurement of outcome in adults with TBI, to our knowledge, there is no published validity information regarding their usage in children and adolescents <17 years of age. Acknowledging this limitation, we modified the original structured GOS-E interview to create the pediatric version (GOS-E Peds), a developmentally appropriate interview to classify TBI outcome in younger patients.
The goal of this study was to establish the validity of the GOS-E Peds as a measure of functional outcome after TBI by comparing it to the GOS in a population of children who varied in age and severity of acute TBI. We hypothesized that the GOS-E Peds would show a strong correlation with the GOS, the recognized gold standard. Additionally, the Vineland Adaptive Behavior Scales, a measure widely applied in pediatric studies outside the hospital, was used to provide a developmentally based reference for comparison. We explored the criterion-related validity of the GOS-E Peds by comparing it with highly standardized parent rating scales measuring daily function and behavior as well as to performance-based cognitive instruments collected at the same time point (concurrent validity). We also hypothesized that the GOS-E Peds assessed at 3 months would be strongly correlated with these same standardized outcome assessments at 6 months (predictive validity). In contrast, we hypothesized that the GOS-E Peds at 3 and 6 months post-TBI would be more weakly correlated with standardized measures of premorbid function (discriminant validity).
Methods
This study utilized an analysis of prospective data from two studies of TBI in children from the Pediatric Neurotrauma Center at Children's Hospital of Pittsburgh of the University of Pittsburgh Medical Center. The present study and the parent research projects were completed with appropriate Institutional Review Board oversight. Inclusion criteria were: 1) mild to severe non-penetrating TBI (intake or post-resuscitation Glasgow Coma Scale [GCS] score between 3 and 15) (Teasdale and Jennett, 1974); 2) birth to 16 years of age at injury; 3) GOS and GOS-E Peds scores for at least one study time point; and 4) English as the child's language of origin.
Premorbid functional abilities were assessed by caregiver interview using the Vineland Adaptive Behavior Scales–Interview Version [VABS] (Sparrow, 2006). Children ≥3 years of age underwent a behavioral survey (Conners' Parent Rating Scale [CPRS] (Conners, 2001)). This initial evaluation was generally completed within 24–36 h after injury. Demographic information was collected from the child's parent(s) or caregiver at the time of injury. Instruments administered at 3 and 6 months included the VABS and CPRS as well as an age- appropriate IQ measure and instruments assessing memory and learning and processing speed as described subsequently.
Measures of functional outcome and behavior
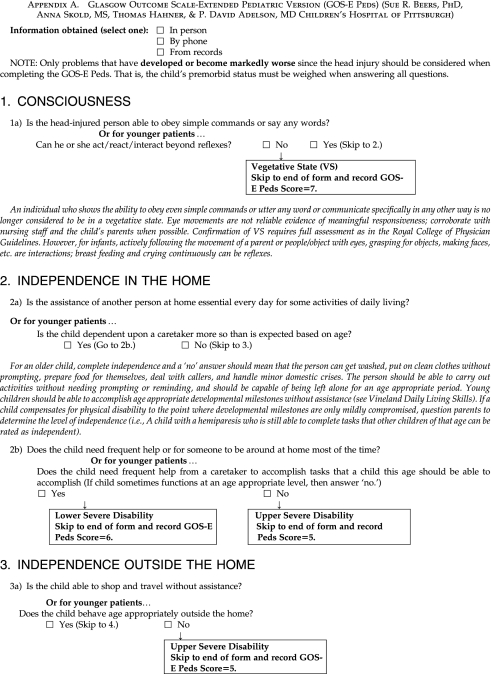
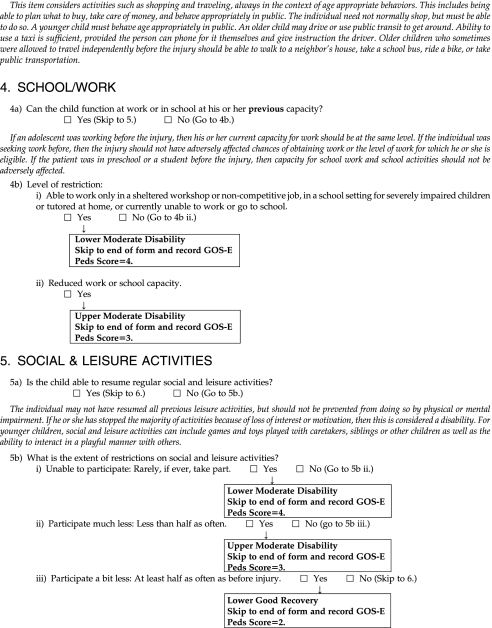
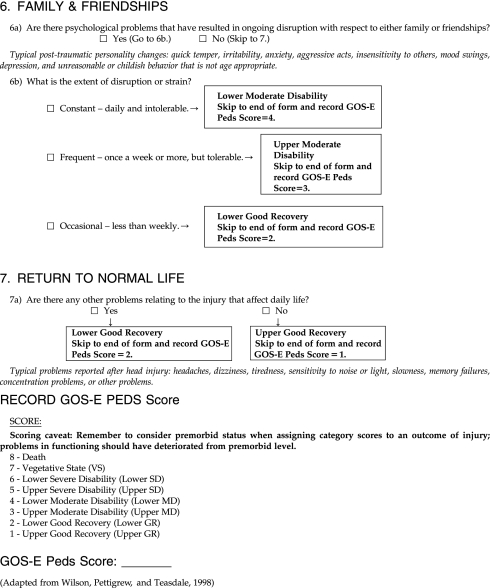
The original GOS was scored according to five categories: 1=good recovery, 2=moderate disability, 3=severe disability, 4=persistent vegetative state, and 5=death. The GOS-E Peds, including the developmentally appropriate interview and descriptors of category scores, is included in Appendix A. For more extensive information regarding standard GOS-E terms, the reader is referred to Wilson and associates (1998). For this study, both instruments were scored such that a higher score indicated increasing level of disability. A single trained technician, not blind to the severity of TBI, completed the GOS and GOS-E Peds with face-to-face interviews with caregivers, and children if age appropriate, at each study time point. The VABS, as a measure of parent-reported functional abilities at follow-up time points, was chosen as the primary reference measure to compare the GOS-E Peds. Behavior problems were assessed with the CPRS. Unlike the VABS and neuropsychological instruments discussed subsequently, higher scores on the CPRS reflect more problems.
Cognitive outcome: Measures of intelligence and neuropsychological abilities
Standardized, performance-based outcome testing was completed 3 and 6 months post-injury. General intellectual functioning (i.e., IQ), assessed by either the Bayley Scales of Infant Development, 2nd Edition (BSID-2) (Bayley, 1993) or the Stanford Binet-IV (SB-IV) (Thorndike, 1986), was administered at <2.5 years and ≥2.5 years, respectively, as dictated by procedures in the parent research studies. For children ≥5 years, The California Verbal Learning Test–Child Version (CVLT-C) assessed rote memory ability in short- and long-delay free recall conditions. (Delis, 1994) and the Wechsler Intelligence Scale for Children-III (WISC-III) (Wechsler, 1991) Coding and Digit Symbol subtests were used to compute the Processing Speed Index according to manualized procedures. These instruments were selected because memory and processing speed problems are two of the most common sequelae of TBI in children (Beers and Levin, 2008).
Statistical analysis
Summary statistics were used to describe the clinical characteristics and outcome test scores for the overall sample and by severity group. Data analyses were performed to evaluate the GOS-E Peds as an improvement over the GOS. Comparisons were also made between the GOS-E Peds and GOS and the VABS as a developmentally based criterion measure. The neuropsychological tests were referenced to provide a broader representation of the developmental spectrum in children.
Premorbid status and 3 and 6 month outcomes were compared with the GOS and GOS-E Peds using the Spearman correlation coefficient. To assess the GOS-E Peds as an improvement, several analyses were performed. Assessment of primary criterion validity relied on a comparison of the GOS-E Peds with the GOS and the VABS. Predictive validity was assessed by comparing 3 month GOS-E Peds and GOS scores with VABS scores at 6 months. Finally, discriminant validity was assessed by comparing premorbid VABS and other test scores with the GOS and GOS-E Peds.
To measure sensitivity to change of the GOS and GOS-E Peds, we examined the association of change in the GOS/GOS-E Peds with the change in the VABS and other outcome measures at three intervals: 1) premorbid versus 3 months, 2) premorbid versus 6 months, and 3) 3 versus 6 months. Subjects were excluded from this analysis if they were deceased or did not have an assessment completed at both 3 and 6 month follow-up. Statistical significance level was defined as α=0.05 with two-sided alternative hypotheses.
Results
Description of the sample
The sample included 159 children and adolescents (62% males), with an age range of 1 to 204 months (80.9±56.9 months). Severity of injury was distributed as 50% severe (Glasgow Coma Scale [GCS] ≤8), 12% moderate (GCS 9–12), and 36% mild (GCS ≥13). Other characteristics of the study sample are presented in Table 1. Approximately 12% of the sample incurred abuse, raising an issue regarding assessment in this injury group. In this subgroup of patients, baseline and follow-up assessments were completed with the non-perpetrating parent. Assessments were completed for 148 subjects (93%) at 3 month follow-up and for 114 subjects (72%) at 6 month follow-up. The outcome test scores at follow-up time points are presented in Table 2.
Table 1.
Demographic Information and Injury Characteristics
| Characteristic | n | % |
|---|---|---|
| Gender | ||
| Male | 98 | 61.6 |
| Female | 61 | 38.4 |
| Primary race | ||
| White/Caucasian | 144 | 90.6 |
| Black/African-American | 13 | 8.2 |
| Asian | 1 | 0.6 |
| Multi-racial /No primary race | 1 | 0.6 |
| Hispanic or Latino | ||
| Yes | 1 | 0.6 |
| No | 157 | 98.7 |
| Injury mechanism | ||
| Fall | 39 | 24.5 |
| Motor vehicle collision | 35 | 22.0 |
| Car vs. pedestrian | 22 | 13.8 |
| Abuse | 20 | 12.6 |
| Recreational | 27 | 16.9 |
| Other | 16 | 10.1 |
| Severity of TBI (initial GCS Totala) | ||
| 3 | 5 | 3.1 |
| 4 | 4 | 2.5 |
| 5 | 7 | 4.4 |
| 6 | 25 | 15.7 |
| 7 | 28 | 17.6 |
| 8 | 10 | 6.2 |
| 9 | 3 | 1.8 |
| 10 | 10 | 6.3 |
| 11 | 5 | 3.1 |
| 12 | 1 | 0.6 |
| 13 | 4 | 2.5 |
| 14 | 16 | 10.1 |
| 15 | 38 | 23.9 |
Initial Glasgow Coma Scale (GCS) was unavailable for 3 subjects.
Table 2.
Mean and Standard Deviation Scores of Outcome Test Scores
| 3 month Mean±SD | 6 month Mean±SD | |
|---|---|---|
| Vineland Adaptive Behavior Scales | ||
| Communication SS | 97.8±15.2 | 97.6±17.4 |
| Daily Living SS | 97.3±18.2 | 94.7±21.1 |
| Socialization SS | 98.4±15.2 | 98.6±17.1 |
| Motor Skills SS | 33.1±50.8 | 36.0±52.8 |
| Adaptive Behavior Composite | 96.8±17.8 | 95.5±23.4 |
| Conners' Parent Rating Scale | ||
| Conduct Problem T | 51.5±13.0 | 51.3±14.3 |
| Learning Problem T | 56.6±15.8 | 56.6±17.1 |
| Psychosomatic T | 55.7±14.6 | 52.9±14.0 |
| Impulsive Hyperactive T | 53.8±12.1 | 52.2±12.9 |
| Anxiety T | 51.4±11.1 | 48.6±9.0 |
| Hyperactive Index | 54.6±14.4 | 54.0±15.6 |
| Bayley | ||
| MDI | 85.9±22.3 | 84.2±22.1 |
| PDI | 88.8±27.9 | 90.2±38.2 |
| Stanford-Binet | 96.0±14.8 | 96.5±16.1 |
| CVLT Short Delay Free Recall | 7.1±4.9 | 7.4±4.5 |
| CVLT Long Delay Free Recall | 7.1±4.9 | 7.3±4.5 |
| WISC-III Processing Speed Index | 100.0±24.8 | 96.6±25.0 |
CVLT, California Verbal Learning Test; WISC, Wechsler Intelligence Scale for Children; SS, Standard Score; T, T score.
Relationship of the GOS-E Peds to functional, behavioral, and cognitive outcome measures
Validity of the GOS-E Peds is evidenced by a strong positive correlation of the GOS-E Peds at both 3 and 6 months with the gold standard GOS (respectively, 0.865 and 0.824, p<0.001) and the VABS composite (respectively, −0.645 and −0.746; p<0.001). For the VABS composite score, the correlation of the GOS-E Peds was improved over the moderate correlation of the GOS with the VABS. Criterion-related validity that compared the same time point (i.e., concurrent validity) demonstrated a strong inverse correlation with 3 and 6 month outcome measures (Table 3). In all functional domains, the strength of the correlation was greater for the GOS-E Peds than for the GOS, indicating that the pediatric version explains more variance than the original GOS.
Table 3.
Correlationa of GOS and GOS-E Peds with Outcome Measures at 3 and 6 Months
| |
GOS |
GOS-E Peds |
||||||
|---|---|---|---|---|---|---|---|---|
| |
3 Months |
6 Months |
3 Months |
6 Months |
||||
| Instruments | rs | 95% CI | rs | 95% CI | rs | 95% CI | rs | 95% CI |
| Vineland Adaptive Behavior Scales | ||||||||
| Communication SS | −0.436* | −0.56, −0.27 | −0.494* | −0.62, −0.30 | −0.549* | −0.64, −0.39 | −0.669* | −0.76, −0.54 |
| Daily Living Skills SS | −0.333* | −0.48, −0.16 | −0.485* | −0.62, −0.31 | −0.460* | −0.59, −0.31 | −0.613* | −0.73, −0.47 |
| Socialization SS | −0.410* | −0.57, −0.28 | −0.475* | −0.61, −0.29 | −0.558* | −0.63, −0.37 | −0.652* | −0.78, −0.56 |
| Motor Skills SS | −0.417† | −0.66, −0.19 | −0.742* | −0.84, −0.52 | −0.547* | −0.71, −0.28 | −0.842* | −0.90, −0.68 |
| Adaptive Behavior Composite SS | −0.478* | −0.60, −0.33 | −0.561* | −0.68, −0.40 | −0.645* | −0.71, −0.49 | −0.746* | −0.83, −0.66 |
| Bayley Scales of Infant Development-2 (ages <2.5 years) | ||||||||
| Mental Development Index | −0.652* | −0.78, −0.35 | −0.660* | −0.90, −0.60 | −0.734* | −0.84, −0.50 | −0.709* | −0.89, −0.58 |
| Psychomotor Development Index | −0.654* | −0.79, −0.39 | −0.747* | −0.91, −0.65 | −0.736* | −0.85, −0.53 | −0.817* | −0.93, −0.71 |
| Stanford-Binet Intelligence Scale-IV (ages ≥2.5 years) | ||||||||
| Composite Score | −0.415* | −0.56, −0.22 | −0.528* | −0.66, −0.32 | −0.564* | −0.69, −0.42 | −0.675* | −0.76, −0.48 |
| Conners' Parent Rating Scale | ||||||||
| Conduct Problem T | 0.192 | −0.12, 0.30 | 0.105 | −0.16 0.32 | 0.220 | −0.07, 0.34 | 0.152 | −0.05, 0.42 |
| Learning Problem T | 0.368* | 0.09, 0.48 | 0.376* | 0.20 0.61 | 0.421* | 0.18, 0.55 | 0.472* | 0.37, 0.71 |
| Psychosomatic T | 0.198 | −0.16, 0.27 | 0.084 | −0.19 0.30 | 0.218 | −0.10, 0.31 | 0.097 | −0.09, 0.38 |
| Impulsive Hyperactive T | 0.180 | −0.12, 0.30 | 0.191 | −0.03 0.44 | 0.246 | −0.02, 0.38 | 0.281† | 0.09, 0.53 |
| Anxiety T | 0.079 | −0.14, 0.28 | 0.063 | −0.15, 0.33 | 0.113 | −0.10, 0.31 | 0.034 | −0.21, 0.27 |
| Hyperactive Index T | 0.233 | −0.02, 0.38 | 0.312‡ | 0.06, 0.51 | 0.234‡ | 0.04, 0.44 | 0.472‡ | 0.25, 0.64 |
| CVLT-C Short Delay Free Recall T Score | −0.448* | −0.63, −0.25 | 0.524* | −0.70, −0.32 | −0.421* | −0.60, −0.21 | 0.368* | −0.61, −0.17 |
| CVLT-C Long Delay Free Recall T Score | −0.414* | −0.61, −0.24 | −0.491* | −0.67, −0.26 | −0.407* | −0.62, −0.25 | −0.448* | −0.59, −0.13 |
| WISC-III Processing Speed Index | −0.527* | −0.67, −0.31 | −0.592* | −0.75, −0.36 | −0.570* | −0.71, −0.37 | −0.593* | −0.75, −0.37 |
Correlation by Spearman's rho (rs).
p<0.001; †p<0.01; ‡p<0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; CVLT-C, California Verbal Learning Test-Child; WISC-III, Wechsler Intelligence Scale for Children, 3rd Edition; SS, Standard Score; T, T score.
For predictive validity, similar procedures were applied (Table 4) to examine the correlation between the 3 month GOS and GOS-E Peds scores and the 6 month test measures. With the 6 month VABS composite score, the GOS-E Peds correlation was −0.687 (p<0.001) and improved over the GOS (−0.549; p<0.001). The moderate-to-strong correlation for the GOS-E Peds was also higher than the GOS with 6 month IQ, processing speed, and CPRS rating scores.
Table 4.
Correlationa of GOS and GOS-E Peds at 3 Months with Outcome Measures at 6 Months
| |
GOS (3 Months) |
GOS-E Peds (3 Months) |
||
|---|---|---|---|---|
| Instruments (6 Months) | rs | 95% CI | rs | 95% CI |
| Vineland Scales of Adaptive Behavior | ||||
| Communication SS | −0.481* | −0.61, −0.28 | −0.616* | −0.71, −0.43 |
| Daily Living Skills SS | −0.451* | −0.59, −0.25 | −0.540* | −0.65, −0.34 |
| Socialization SS | −0.468* | −0.60, −0.27 | −0.598* | −0.70, −0.42 |
| Motor Skills SS | −0.660* | −0.79, −0.38 | −0.784* | −0.87, −0.58 |
| Adaptive Behavior Composite SS | −0.546* | −0.67, −0.37 | −0.687* | −0.77, −0.53 |
| Bayley Scales of Infant Development-2 (ages <2.5 years) | ||||
| Mental Development Index | −0.646* | −0.87, −0.51 | −0.701* | −0.86, −0.47 |
| Psychomotor Development Index | −0.727* | −0.85, −0.46 | −0.740* | −0.87, −0.51 |
| Stanford-Binet Intelligence Scale-IV (ages ≥2.5 years) | ||||
| Stanford-Binet Composite Score | −0.523* | −0.65, −0.27 | −0.635* | −0.74, −0.43 |
| Conners' Parent Rating Scale | ||||
| Conduct Problem T | 0.098 | −0.14, 0.35 | 0.137 | −0.09, 0.39 |
| Learning Problem T | 0.390* | 0.15, 0.59 | 0.459* | 0.26, 0.65 |
| Psychosomatic T | 0.047 | −0.16, 0.33 | 0.059 | −0.14, 0.35 |
| Impulsive Hyperactive T | 0.215 | −0.01, 0.47 | 0.320† | 0.11, 0.55 |
| Anxiety T | 0.007 | −0.26, 0.24 | −0.009 | −0.29, 0.20 |
| Hyperactive Index T | 0.274‡ | 0.05, 0.52 | 0.361† | 0.17, 0.59 |
| CVLT-C | ||||
| Short Delay Free Recall (SDFR) | −0.449* | −0.64, −0.19 | −0.421* | −0.62, −0.16 |
| Long Delay Free Recall (LDFR) | −0.414* | −0.57, −0.09 | −0.406* | −0.56, −0.07 |
| WISC-III Processing Speed Index | −0.537* | −0.74, −0.35 | −0.639* | −0.78, −0.42 |
Correlation by Spearman's rho (rs).
p<0.001; †p<0.01; ‡p<0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; CVLT-C, California Verbal Learning Test-Child; WISC-III, Wechsler Intelligence Scale for Children, 3rd Edition; SS, Standard Score; T, T score.
Discriminant validity of the 3 and 6 month GOS-E Peds, examined by comparison with the premorbid VABS Adaptive Behavior Composite and the CPRS scores, is demonstrated by the moderate-to-weak correlations (0.47 to 0.001) with only 3 of the14 coefficients falling >0.30.
Relationship of the GOS-E Peds to severity of injury
There was a strong correlation between the GOS and GOS-E Peds (Table 5) as well as between the GOS-E Peds with other outcome measures by severity of TBI at the 3 and 6 month time points. The correlation of the GOS-E Peds with outcome measures at 3 and 6 months by severity of TBI is presented in Tables 6 and 7. In the mild injury group, correlation of the GOS-E Peds with the VABS was higher than that for the GOS with the VABS in nearly all test domains. The correlations with VABS increased at 6 months' follow-up. In this case, moderate correlations were noted with overall everyday functional abilities measured by the VABS Adaptive Behavior Composite. In contrast, the GOS-E Peds' correlation with other behavioral outcome measures was more variable, ranging from a minimal correlation with CPRS measures of impulsivity and conduct problems to a moderate correlation with learning problems. These correlations reached statistical significance at 3 months but not at 6 months.
Table 5.
Correlation of the GOS and GOS-E Peds by Severity of Injury
| |
Mild (GCS ≥13) |
Moderate (GCS 9-12) |
Severe (GCS ≤8) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| r | p-value | 95% CI | r | p-value | 95% CI | r | p-value | 95% CI | |
| GOS & GOS-E (3-month) | 0.698 | <.0001 | 0.529, 0.810 | 0.769 | <0.001 | 0.420, 0.911 | 0.885 | <.0001 | 0.820, 0.925 |
| GOS & GOS-E (6-month) | 0.708 | <0.001 | 0.414, 0.861 | 0.698 | 0.002 | 0.307, 0.877 | 0.807 | <.0001 | 0.704, 0.874 |
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric.
Table 6.
Correlationa of 3-Month GOS and GOS-E Peds with Outcome Measures by Severity of TBI
| |
Mild (GCS ≥13) |
Moderate (GCS 9-12) |
Severe (GCS ≤8) |
|||
|---|---|---|---|---|---|---|
| Instruments | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI |
| VABS | ||||||
| Communication SS | −0.313‡ | −0.376† | 0.000 | −0.119 | −0.374† | −0.575* |
| −0.54, −0.03 | −0.59, −0.10 | −0.51, 0.51 | −0.59, 0.42 | −0.57, −0.12 | −0.72, −0.37 | |
| Daily Living Skills SS | 0.085 | −0.154 | 0.232 | 0.072 | −0.424* | −0.584* |
| −0.20, 0.35 | −0.41, 0.13 | −0.33, 0.66 | −0.46, 0.56 | −0.61, −0.18 | −0.73, −0.38 | |
| Socialization SS | −0.344‡ | −0.504* | −0.193 | −0.148 | −0.316‡ | −0.431* |
| −0.57, −0.07 | −0.68, −0.26 | −0.64, 0.36 | −0.61, 0.40 | −0.53, −0.06 | −0.62, −0.19 | |
| Motor Skills SS | −0.342 | −0.410 | −0.258 | −0.600 | −0.504‡ | −0.637† |
| −0.68, 0.13 | −0.72, 0.05 | −0.97, 0.94 | −0.99, 0.88 | −0.76, −0.09 | −0.83, −0.28 | |
| Adaptive Behavior Composite SS | −0.277‡ | −0.475* | 0.039 | −0.099 | −0.452* | −0.651* |
| −0.51, 0.00 | −0.66, −0.22 | −0.48, 0.54 | −0.58, 0.44 | −0.63, −0.22 | −0.78, −0.47 | |
| CPRS | ||||||
| Conduct Problem T | 0.033 | 0.287 | 0.634 | 0.647 | −0.067 | −0.156 |
| −0.30, 0.36 | −0.06, 0.56 | −0.17, 0.92 | −0.15, 0.92 | −0.38, 0.26 | −0.45, 0.17 | |
| Learning Problem T | 0.286 | 0.535* | 0.504 | 0.283 | −0.005 | 0.048 |
| −0.06, 0.56 | 0.24, 0.73 | −0.34, 0.88 | −0.54, 0.82 | −0.32, 0.32 | −0.28, 0.36 | |
| Psychosomatic T | 0.291 | 0.500 † | 0.063 | 0.298 | 0.051 | 0.004 |
| −0.05, 0.57 | 0.19, 0.71 | −0.67, 0.73 | −0.53, 0.82 | −0.27, 0.36 | −0.32, 0.32 | |
| Impulsive Hyperactive T | −0.004 | 0.256 | 0.507 | 0.401 | −0.230 | −0.215 |
| −0.34, 0.33 | −0.09, 0.54 | −0.34, 0.89 | −0.45, 0.85 | −0.51, 0.10 | −0.50, 0.12 | |
| Anxiety T | 0.079 | 0.330‡ | 0.319 | 0.560 | −0.008 | −0.052 |
| −0.26, 0.40 | −0.01, 0.59 | −0.51, 0.83 | −0.28, 0.90 | −0.33, 0.31 | −0.36, 0.27 | |
| Hyperactive Index T | 0.248 | 0.437† | 0.507 | 0.479 | −0.099 | −0.098 |
| −0.10, 0.53 | 0.12, 0.67 | −0.34, 0.89 | −0.37, 0.88 | −0.41, 0.23 | −0.40, 0.23 | |
| Bayley Scales | ||||||
| MDI | −0.433 | −0.613‡ | −0.775 | −0.800 | −0.650† | −0.711* |
| −0.77, 0.12 | −0.85, −0.12 | −0.99, 0.78 | −0.99, 0.76 | −0.85, −0.24 | −0.88, −0.35 | |
| PDI | −0.414 | −0.614† | −0.258 | −0.600 | −0.745* | −0.834* |
| −0.76, 0.14 | −0.85, −0.13 | −0.97, 0.94 | −0.99, 0.88 | −0.89, −0.41 | −0.93, −0.59 | |
| Stanford-Binet | ||||||
| −0.015 | −0.286 | −0.523 | −0.675‡ | −0.315‡ | −0.523* | |
| −0.34, 0.31 | −0.56, 0.05 | −0.85, 0.14 | −0.90, −0.09 | −0.56, −0.01 | −0.71, −0.26 | |
| CVLT SDFR | −0.305 | −0.071 | −0.211 | −0.346 | −0.542† | −0.606* |
| −0.61, 0.09 | −0.44, 0.32 | −0.76, 0.54 | −0.81, 0.43 | −0.75, −0.23 | −0.78, −0.32 | |
| CVLT LDFR | −0.359 | −0.260 | −0.156 | −0.318 | −0.547† | −0.637* |
| −0.65, 0.03 | −0.58, 0.14 | −0.74, 0.57 | −0.80, 0.46 | −0.75, −0.24 | −0.80, −0.36 | |
| WISC PSI | 0.137 | −0.122 | −0.520 | −0.509 | −0.715* | −0.771* |
| −0.26, 0.49 | −0.48, 0.27 | −0.87, 0.25 | −0.87, 0.26 | −0.86, −0.46 | −0.89, −0.55 | |
Correlation by Spearman's rho (rs).
p ≤0.001; † p ≤0.01; ‡p ≤0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; GCS, Glasgow Coma Scale; VABS, Vineland Adaptive Behavior Scales; SS, Scale Score; T, T-score; CPRS, Conners' Parent Rating Scale; CVLT-C, California Verbal Learning Test-Child; WISC-III, Wechsler Intelligence Scale for Children, 3rd Edition; SDFR, Short Delay Free Recall; LDFR, Long Delay Free Recall; PSI, Processing Special Index; MDI, Mental Development Index; PDI, Psychomotor Development Index.
Table 7.
Correlation† of 6-Month GOS and GOS-E Peds with Outcome Measures by Severity of TBI
| |
Mild (GCS ≥13) |
Moderate (GCS 9-12) |
Severe (GCS ≤8) |
|||
|---|---|---|---|---|---|---|
| Instrument | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI |
| VABS | ||||||
| Communication SS | −0.450‡ | −0.579† | 0.337 | 0.061 | −0.449* | −0.690* |
| −0.74, 0.00 | −0.81, 0.17 | −0.20,0.71 | −0.45, 0.54 | −0.63, −0.21 | −0.80, −0.52 | |
| Daily Living Skills SS | −0.219 | −0.322 | 0.253 | −0.126 | −0.561* | −0.685* |
| −0.60, 0.25 | −0.66, 0.15 | −0.29, 0.66 | −0.58, 0.40 | −0.71, −0.35 | −0.80, −0.51 | |
| Socialization SS | −0.463‡ | −0.513‡ | 0.197 | −0.324 | −0.469* | −0.702* |
| −0.75, −0.01 | −0.77, −0.08 | −0.34, 0.62 | −0.70, 0.21 | −0.65, −0.23 | −0.81, −0.54 | |
| Motor Skills SS | −0.524 | −0.703‡ | −0.354 | −0.335 | −0.711* | −0.867* |
| −0.86, 0.19 | −0.92, −0.09 | −0.94, 0.79 | −0.93, 0.79 | −0.86, −0.41 | −0.94, −0.70 | |
| Adaptive Behavior Composite SS | −0.498‡ | −0.670† | 0.282 | −0.283 | −0.570* | −0.773* |
| −0.77, −0.06 | −0.85, −0.31 | −0.26, 0.68 | −0.68, 0.26 | −0.72, −0.36 | −0.86, −0.64 | |
| CPRS | ||||||
| Conduct Problem T | 0.230 | 0.251 | - | 0.268 | 0.066 | 0.187 |
| −0.38, 0.69 | −0.36, 0.70 | - | −0.41, 0.74 | −0.26, 0.38 | −0.15, 0.48 | |
| Learning Problem T | 0.460 | 0.425 | - | 0.374 | 0.469† | 0.592* |
| −0.14, 0.80 | −0.18, 0.78 | - | −0.31, 0.79 | 0.16, 0.68 | 0.32, 0.77 | |
| Psychosomatic T | 0.433 | 0.349 | - | 0.038 | −0.055 | 0.015 |
| −0.17, 0.79 | −0.26, 0.75 | - | −0.58, 0.62 | −0.37, 0.28 | −0.31, 0.34 | |
| Impulsive Hyperactive T | 0.143 | 0.214 | - | −0.112 | 0.175 | 0.334‡ |
| −0.45, 0.64 | −0.39, 0.68 | - | −0.66, 0.53 | −0.16, 0.47 | 0.01, 0.59 | |
| Anxiety T | 0.229 | −0.170 | - | 0.076 | 0.087 | |
| −0.38, 0.69 | −0.66, 0.43 | - | −0.55, 0.64 | −0.24, 0.40 | −0.31, 0.33 | |
| Hyperactive Index T | 0.342 | 0.287 | - | 0.224 | 0.285 | 0.487 † |
| −0.27, 0.75 | −0.32, 0.72 | - | −0.44, 0.72 | −0.05, 0.55 | 0.19, 0.70 | |
| Bayley Scales | ||||||
| MDI | −0.577 | −0.577 | −0.354 | −0.783 | −0.826* | −0.728† |
| −0.90, 0.25 | −0.90, 0.25 | −0.94, 0.79 | −0.98, 0.41 | −0.94, −0.52 | −0.90, −0.32 | |
| PDI | −0.577 | −0.866† | −0.707 | −0.894‡ | −0.892* | −0.812* |
| −0.90, 0.25 | −0.97, −0.36 | −0.97, 0.53 | −0.99, −0.05 | −0.96, −0.68 | −0.93, −0.49 | |
| Stanford-Binet | −0.610‡ | −0.560‡ | - | −0.374 | −0.508* | −0.676* |
| −0.86, −0.09 | −0.83, −0.02 | - | −0.79, 0.31 | −0.70, −0.24 | −0.81, −0.47 | |
| CVLT SDFR | 0.595 | 0.844† | - | 0.395 | −0.57866* | −0.513† |
| −0.23, 0.91 | 0.29, 0.97 | - | −0.33, 0.81 | −0.76, −0.30 | −0.72, −0.21 | |
| CVLT LDFR | 0.504 | 0.444 | - | 0.351 | −0.540* | −0.467† |
| −0.34, 0.88 | −0.41, 0.87 | - | −0.37, 0.30 | −0.74, −0.24 | −0.69, −0.15 | |
| WISC PSI | - | 0.258 | - | −0.577 | −0.573* | −0.584* |
| - | −0.94, 0.97 | - | −0.90, 0.25 | −0.76, −0.28 | −0.77, −0.29 | |
Correlation by Spearman's rho (rs).
p ≤0.001; †p ≤0.01; ‡p ≤0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; GCS, Glasgow Coma Scale; VABS, Vineland Adaptive Behavior Scales; SS, Scale Score; T, T-score; CPRS, Conners' Parent Rating Scale; CVLT-C, California Verbal Learning Test-Child; WISC-III, Wechsler Intelligence Scale for Children, 3rd Edition; SDFR, Short Delay Free Recall; LDFR, Long Delay Free Recall; PSI, Processing Special Index; MDI, Mental Development Index; PDI, Psychomotor Development Index.
The moderate TBI group demonstrated the weakest correlations, likely because of the small number of subjects in this group. Weak-to-moderate correlations were observed at 3 and 6 months' follow-up. Statistical significance was only reached for the Stanford-Binet at 3-months, and the Bayley Motor Index at 6-months.
In the severe injury group, correlation of the GOS-E Peds with the VABS and other measures were moderate to high, and greater than those for the GOS in nearly all domains at both follow-up time points. A high correlation (>0.7) was observed for overall adaptive behavior. More focused behavior-related scores (i.e., CPRS) correlated weakly with the GOS-E Peds in severely injury patients at 3 months, but increased at 6 months' follow-up. Specifically, the GOS-E Peds was highly correlated with overall behavior, reaching statistical significance for measures of learning, impulsivity, and overall hyperactivity.
Changes in GOS-E Peds categories among premorbid status, 3, and 6 months by severity
Assessments at 3 and 6 months were available for 103 subjects. Table 8 presents the correlations between the change in the GOS-E Peds and GOS versus the change in the premorbid VABS and the CPRS by severity of TBI. At 3 month follow-up (Table 8), the change in GOS-E Peds for the mild TBI group was weakly correlated with the VABS and CPRS change scores. In contrast, moderate correlations were noted for moderate and severe groups. At 6 months (Table 9), stronger associations were found when the GOS-E Peds versus VABS change scores were examined in the severe group, and mild group comparisons became moderately correlated.
Table 8.
Correlationa of Change in the Premorbid and 3-month Scores for the Vineland and Conners' versus the 3-month GOS and GOS-E Peds by Severity of TBI
| |
Mild (GCS ≥13) |
Moderate (GCS 9-12) |
Severe (GCS ≤8) |
|||
|---|---|---|---|---|---|---|
| Instrument | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI |
| VABS | ||||||
| Communication SS | −0.333 | −0.183 | −0.076 | 0.029 | −0.410‡ | −0.526* |
| −0.71, 0.28 | −0.54, 0.23 | −0.64,0.55 | −0.58, 0.62 | −0.64, −0.09 | −0.72, −0.24 | |
| Daily Living Skills SS | 0.042 | 0.044 | 0.375 | 0.81† | −0.389‡ | −0.523* |
| −0.36, 0.43 | −0.36, 0.43 | −0.31, 0.79 | −0.38, 0.95 | −0.63, −0.06 | −0.72, −0.23 | |
| Socialization SS | −0.181 | −0.259 | 0.000 | 0.138 | −0.239 | −0.322‡ |
| −0.53, 0.23 | −0.59, 0.16 | −0.60, 0.60 | −0.51, 0.68 | −0.52, −0.10 | −0.59, 0.01 | |
| Motor Skills SS | −0.448 | −0.558‡ | 0.258 | 0.400 | 0.005 | 0.018 |
| −0.78, 0.13 | −0.83, −0.02 | −0.94, 0.97 | −0.92, 0.98 | −0.53, 0.53 | −0.52, 0.54 | |
| Adaptive Behavior Composite SS | −0.285 | −0.235 | 0.112 | 0.437 | −0.363‡ | −0.474† |
| −0.61, 0.13 | −0.57, 0.18 | −0.53, 0.66 | −0.24, 0.81 | −0.61, −0.03 | −0.69, −0.17 | |
| CPRS | ||||||
| Conduct Problem T | −0.306 | −0.072 | - | - | 0.119 | −0.002 |
| −0.71, 0.28 | −0.58, 0.48 | - | - | −0.32, 0.51 | −0.42, 0.42 | |
| Learning Problem T | 0.456 | 0.247 | - | - | 0.138 | 0.065 |
| −0.12, 0.79 | −0.33, 0.68 | - | - | −0.30, 0.53 | −0.37, 0.47 | |
| Psychosomatic T | −0.044 | 0.000 | - | - | 0.109 | 0.008 |
| −0.56, 0.50 | −0.53, 0.53 | - | - | −0.33, 0.51 | −0.41, 0.43 | |
| Impulsive Hyperactive T | −0.262 | −0.327 | - | - | −0.423‡ | −0.432‡ |
| −0.69, 0.32 | −0.72, 0.26 | - | - | −0.71, 0.01 | −0.72, −0.00 | |
| Anxiety T | 0.229 | −0.170 | - | −0.045 | −0.231 | |
| −0.38, 0.69 | −0.66, 0.43 | - | - | −0.46, 0.38 | −0.59, 0.22 | |
| Hyperactive Index T | 0.390 | 0.209 | - | - | 0.110 | −0.01† |
| −0.19, 0.76 | −0.37, 0.66 | - | - | −0.33, 0.51 | −0.41, 0.43 | |
Correlation by Spearman's rho (rs).
p<0.001; †p<0.01; ‡p<0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; GCS, Glasgow Coma Scale; VABS, Vineland Adaptive Behavior Scales; CPRS, Conners' Parent Rating Scale; SS, Standard Score; T, T score.
Table 9.
Correlationa of Change in the Premorbid and 6-Month Scores for the Vineland and Conners' with the 6-Month GOS and GOS-E Peds by Severity of TBI
| |
Mild (GCS ≥13) |
Moderate (GCS 9-12) |
Severe (GCS ≤8) |
|||
|---|---|---|---|---|---|---|
| Instrument | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI | GOS rs95% CI | GOS-E Peds rs95% CI |
| VABS | ||||||
| Communication SS | −0.155 | −0.357 | 0.050 | 0.305 | −0.673* | −0.665* |
| −0.69, 0.37 | −0.75, 0.26 | −0.57,0.63 | −0.37, 0.76 | −0.82, −0.42 | −0.82, −0.41 | |
| Daily Living Skills SS | −0.231 | −0.134 | 0.501 | 0.374 | −0.654* | −0.557* |
| −0.69, 0.37 | −0.63, 0.45 | −0.17, 0.84 | −0.31, 0.79 | −0.82, −0.42 | −0.75, −0.25 | |
| Socialization SS | −0.309 | −0.446 | 0.401 | 0.372 | −0.537† | −0.467† |
| −0.73, 0.30 | −0.79, 0.16 | −0.28, 0.80 | −0.38, 0.76 | −0.74, −0.22 | −0.70, −0.13 | |
| Motor Skills SS | - | - | 0.258 | 0.738 | −0.531 | −0.488 |
| - | - | −0.94, 0.97 | −0.81, 0.99 | −0.83, 0.05 | −0.81, 0.11 | |
| Adaptive Behavior Composite SS | −0.387 | −0.380 | 0.452 | 0.471 | −0.662* | −0.588* |
| −0.77, 0.22 | −0.76, 0.23 | −0.22, 0.82 | −0.20, 0.83 | −0.82, −0.39 | −0.78, −0.29 | |
| CPRS | ||||||
| Conduct Problem T | −0.283 | 0.125 | - | - | 0.411 | 0.469‡ |
| −0.82, 0.54 | −0.64, 0.76 | - | - | −0.04, 0.71 | 0.04, 0.74 | |
| Learning Problem T | 0.439 | 0.291 | - | - | 0.552† | 0.323 |
| −0.41, 0.87 | −0.54, 0.82 | - | - | 0.14, 0.79 | −0.13, 0.66 | |
| Psychosomatic T | 0.415 | 0.494 | - | - | 0.219 | 0.044 |
| −0.43, 0.86 | −0.35, 0.88 | - | - | −0.24, 0.59 | −0.39, 0.47 | |
| Impulsive Hyperactive T | −0.510 | 0.000 | - | - | 0.155 | 0.181 |
| −0.89, 0.34 | −0.70, 0.70 | - | - | −0.30, 0.55 | −0.28, 0.57 | |
| Anxiety T | 0.595 | −0.281 | - | −0.041 | −0.368 | |
| −0.23, 0.91 | −0.82, 0.54 | - | - | −0.40, 0.46 | −0.69, 0.08 | |
| Hyperactive Index T | 0.249 | 0.219 | - | - | 0.594† | 0.481‡ |
| −0.56, 0.81 | −0.58, 0.79 | - | - | 0.20, 0.81 | 0.05, 0.75 | |
Correlation by Spearman's rho (rs).
p<0.001; †p<0.01; ‡p<0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; GCS, Glasgow Coma Scale; VABS, Vineland Adaptive Behavior Scales; CPRS, Conners' Parent Rating Scale; SS, Standard Score; T, T score.
Table 10 shows the results of change scores calculated between 3 and 6 month outcome variables correlated with the GOS and the GOS-E Peds with respect to sensitivity to recovery from TBI. In this case, the GOS-E Peds showed an advantage over the GOS. Weak but significant associations on measures of functional ability, intelligence scales for younger children, and memory ability were demonstrated for the GOS-E Peds. As with most previous comparisons, the GOS-E Peds showed a stronger correlation with the VABS than did the GOS at both time points.
Table 10.
Correlation† of Change in the 3- and 6-month Scores for the Vineland and Conners' with the 6-month GOS and GOS-E Peds
| |
GOS |
GOSE-Peds |
||
|---|---|---|---|---|
| Instrument | rs | 95% CI | rs | 95%CI |
| Vineland Adaptive Behavior Scales | ||||
| Communication SS | −0.118 | −0.33, 0.11 | −0.216 | −0.41, 0.01 |
| Daily Living Skills SS | −0.013 | −0.23, 0.21 | −0.223c | −0.42, 0.00 |
| Socialization SS | −0.229c | −0.43, −0.01 | −0.181 | −0.38, 0.04 |
| Motor Skills SS | −0.077 | −0.41, 0.28 | −0.162 | −0.48, 0.20 |
| Adaptive Behavior Composite SS | −0.139 | −0.35 0.08 | −0.257c | −0.45, −0.04 |
| Conners' Parent Rating Scale | ||||
| Conduct Problem T | 0.229 | −0.07 0.48 | 0.121 | −0.18, 0.40 |
| Learning Problem T | 0.026 | −0.27, 0.31 | −0.104 | −0.38, 0.19 |
| Psychosomatic T | 0.064 | −0.232, 0.35 | 0.153 | −0.15, 0.42 |
| Impulsive Hyperactive T | 0.021 | −0.27, 0.31 | −0.056 | −0.34, 0.24 |
| Anxiety T | −0.218 | −0.48 0.08 | −0.097 | −0.38, 0.20 |
| Hyperactive Index T | −0.081 | −0.36, 0.22 | −0.093 | −0.37, 0.20 |
| Bayley Scales of Infant Development-2 (ages < 2.5 years) | ||||
| Mental Development Index | 0.213 | −0.194, 0.55 | −0.047 | −0.43, 0.35 |
| Psychomotor Development Index | −0.250 | −0.58, 0.16 | −0.424c | −0.69, −0.04 |
| Stanford-Binet (ages ≥ 2.5 years) | ||||
| Composite Score | −0.147 | −0.39, 0.11 | −0.234 | −0.46, 0.03 |
| CVLT Short Delay Free Recall T Score | −0.087 | −0.38, 0.22 | −0.201 | −0.47, 0.11 |
| CVLT Long Delay Free Recall T Score | −0.331c | −0.57, −0.03 | −0.300 | −0.55, 0.01 |
| WISC-III Processing Speed Index | −0.147 | −0.47,0.22 | −0.203 | −0.51, 0.16 |
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric; SS, Standard Score; T, T score.
Correlation by Spearman's rho (rs). Statistical significance: a p < 0.001; b p < 0.01; c p < 0.05.
Sensitivity of the GOS-E Peds to outcome in younger versus older children grouped by TBI severity
To assess the ability of the GOS-E Peds to characterize children across childhood, we examined the correlation coefficients between younger (<2.5 years) and older (≥2.5 years) children in each severity group. As noted earlier and represented in Tables 3 and 4, assessment for younger versus older children required different instruments. At the 3 month time point the GOS-E Peds was moderately to highly correlated with the IQ scores for both younger (i.e., BSID-2 Mental and Psychomotor Development Index) and older children (i.e., SB-IV Composite Score) within the mild injury severity group, and highly correlated with both age groups of children who experienced moderate and severe injury. At 6 months, the relationship between instruments was stronger for all injury groups across the age range.
In Table 11, VABS results are compared because the instrument is appropriate for the entire age range. The GOS-E Peds was moderately to highly correlated in the older age group. In contrast, among the younger children, the GOS-E Peds demonstrated a stronger correlation at 6 months than at 3 months post-injury.
Table 11.
Comparisona of GOS and GOS-E Peds with Outcome Measures at 3- and 6-Month Follow-up by Age Group
| |
Age<2.5 years |
Age≥2.5 years |
||||||
|---|---|---|---|---|---|---|---|---|
| |
GOS |
GOS-E Peds |
GOS |
GOS-E Peds |
||||
| Instruments | 3 mo rs95% CI | 6 mo rs95% CI | 3 mo rs95% CI | 6 mo rs95% CI | 3 mo rs95% CI | 6 mo rs95% CI | 3 mo rs95% CI | 6 mo rs95% CI |
| Vineland Scales | ||||||||
| Communication SS | −0.254 | −0.687* | −0.260 | −0.731* | −0.490* | −0.420* | −0.650* | −0.652* |
| −0.53, 0.09 | −0.84, −0.40 | −0.54, 0.08 | −0.86, −0.47 | −0.63, −0.31 | −0.59, −0.19 | −0.75, −0.50 | −0.76, −0.48 | |
| Daily Living Skills SS | 0.015 | −0.417c | 0.012 | −0.465‡ | −0.464* | −0.571* | −0.667* | −0.719* |
| −0.31, 0.34 | −0.68, −0.03 | −0.32, 0.34 | −0.71, −0.09 | −0.61, −0.28 | −0.71, −0.38 | −0.76, −0.53 | −0.81, −0.57 | |
| Socialization SS | −0.502† | −0.707* | −0.384‡ | −0.780* | −0.404* | −0.388* | −0.571* | −0.652* |
| −0.71, −0.19 | −0.85, −0.43 | −0.63, −0.05 | −0.89, −0.55 | −0.56, −0.21 | −0.57, −0.16 | −0.69, −0.41 | −0.76, −0.48 | |
| Motor Skills SS | −0.360‡ | −0.769* | −0.381‡ | −0.834* | −0.687‡ | −0.639‡ | −0.866* | −0.806‡ |
| −0.61, −0.02 | −0.88, −0.53 | −0.63, −0.04 | −0.91, −0.65 | −0.90, −0.11 | −0.88, −0.03 | −0.96, −0.52 | −0.94, −0.36 | |
| Adaptive Behavior Composite SS | −0.363‡ | −0.728* | −0.339‡ | −0.813* | −0.535* | −0.533* | −0.740* | −0.750* |
| −0.61, −0.02 | −0.86, −0.46 | −0.60, −0.01 | −0.91, −0.61 | −0.66, −0.36 | −0.68, −0.33 | −0.82, −0.62 | −0.83, −0.62 | |
Correlation by Spearman's rho (rs).
p<0.001; †p<0.01; ‡p<0.05.
GOS, Glasgow Outcome Scale; GOS-E Peds, Glasgow Outcome Scale-Extended Pediatric: SS, Standard Score.
Discussion
Jennett and Bond (1975) developed the GOS to encompass areas of major life functions, with a categorical scale of 1 to 5 used to characterize overall disability after TBI. The lack of sensitivity to specific deficits and variability within the category scores led to the subsequent development of the GOS-E. (Wilson et al., 1998) These investigators established the inter-rater reliability of the GOS-E structured interview among three raters (κ=0.85) in a group of subjects having varied injury severity. The validity of the GOS-E has been investigated within the context of the World Health Organization classifications of impairment, disability, and handicap (Teasdale et al., 1998). Levin and associates (2001) assessed the validity of the interview-based GOS-E in adults by comparing it to standardized performance-based measures (i.e., neuropsychological tests) at 3 and 6 months. Their results indicated that the GOS-E provided a valid measure of outcome at 3 months and was also more sensitive to change than the GOS, establishing the GOS-E as the gold standard for assessing outcome after TBI in adults (Levin et al., 2001). Although the structured interview format minimized the subjectivity of the GOS-E, the instrument still lacked the developmental specificity needed to evaluate individuals <16 years of age (Pettigrew et al., 1998). Acknowledging this limitation and need for a global outcomes measures for clinical trials in pediatric TBI, we modified the original structured interview to create the GOS-E Peds and assessed the validity of this revision.
The current study demonstrates that the GOS-E is an improvement over the GOS as a valid measure of overall outcome of infants, toddlers, and children after TBI across the injury spectrum. As expected, the GOS-E Peds is highly correlated with its parent instrument, the GOS. Importantly, in this sample of infants, toddlers, and young children, the concurrent and predictive validity analyses indicate that the GOS-E Peds is an improvement over the GOS in relation to the VABS, a commonly used and developmentally appropriate parent rating of daily living skills, and other measures of functional outcome and behavioral surveys at both 3 and 6 months post-injury. Our findings for measures of cognitive status, including intellectual ability, memory and learning, and processing speed were mixed. Although the GOS-E Peds showed a stronger relationship than the GOS with IQ and processing speed, the instrument did not improve upon the GOS with respect to evaluating either current memory ability or predicting future memory performance. This is an important finding, because it suggests how the current structured GOS-E Peds interview can be improved to increase validity.
All pediatric instruments face the challenge of evaluating children at differing stages of development. Stratification of our sample on age revealed that the GOS-E Peds has some advantage for assessing outcome in children >2.5 years, both 3 and 6 months after injury. For infants and toddlers, the pediatric revision was highly correlated with abilities at 6 months post-injury; however, variability was noted at 3 months for some functional abilities assessed by parent report. Although the GOS-E Peds showed improvement over the GOS in assessing overall adaptive and motor skills, an important exception was noted for communication and daily living skills at 3 months post-injury. Perhaps parents found characteristics such as vocalizations, eating behaviors, understanding environmental demands (e.g., a soiled diaper), and appropriate self-care difficult to evaluate in very young children who had experienced TBI. This may be because the range of “normal” behavior in the youngest children is broad (e.g., toilet training accomplished between the ages of 2 and 3½ years is within normal limits). Alternatively, it may be especially difficult for parent to assess changes in the speed of development of new skills that sometimes occurs after pediatric TBI as opposed to the improvement of already established skills, as with older children and adults.
Because the GOS-E Peds characterizes behaviors that can be found in some children without brain injury (e.g., typical school problems; subclinical attention difficulties) it is important to determine that the instrument can actually distinguish between behaviors frequently found in typically developing children and those who have experienced overt brain injury. In this case, our study found the discriminant validity of the GOS-E Peds to be acceptable. In all functional domains, the relationship between premorbid behavior and post-injury functional outcome was weak, especially at 6 months post-injury. This finding is consistent with the report by Yeates and associates (1997) that retrospective parent ratings of premorbid school performance were associated with outcome after both TBI and orthopedic injury in children aged 6–12 years. Therefore, a strength of this study is that it provides information regarding discriminant as well as concurrent and predictive validity of the GOS-E Peds when compared not only with the most widely used categorical measures of outcome in TBI, the GOS, but also with the VABS and other standardized, performance-based cognitive instruments. Murphy and Davidshofer (1991) deem all three types of validity necessary to establish the overall clinical utility of any instrument.
Based on this study, the GOS-E Peds offers advantages over the PCPC. Although the concurrent and discriminant validity of the PCPC have been described, this work included only severely ill children and lacked the degree of rigor deemed essential in establishing validity (Fiser, 1992). Fiser assessed the relationship between the PCPC and measures “commonly employed terms for describing morbidity and severity of … injury” (p. 69) rather than with the parent GOS and with standardized, performance-based instruments that provide objective measures of cognitive status. In a second study again completed with children discharged from intensive care units, the PCPC's predictive validity at 1 and 6 month follow-up, most important if an instrument is to be useful in clinical trials, was assessed only in the context of the Pediatric Overall Performance Category score (Fiser et al., 2000). Although the PCPC category scores were shown to reflect meaningful change in measures of intellectual ability at hospital discharge, this conclusion was based on comparisons of group means rather than comparison of individual scores.
The results of this study demonstrate that the GOS-E Peds is sensitive to both severity of injury and to recovery over time, at least for the first 6 months after TBI. Because the GOS was originally established to assess the effects of severe TBI, the relationship between both the GOS and the GOS-E Peds and the spectrum of injury severity is important in establishing the clinical utility of the instruments. Our analyses examined the validity of the GOS-E Peds overall and within injury severity groups. For those with mild TBI, results indicate no marked advantage of either instrument at the 3 month time point. At 6 months, however, the GOS-E Peds showed a distinct advantage, having stronger associations with everyday function as measured by the VABS and with measures of intelligence. This finding suggests that the expanded categories probably are better able account for the subtle differences in everyday function associated with milder forms of TBI. Although sample size was limited, the GOS-E Peds showed a strong association with intelligence, especially in younger children. For infants and children with severe TBI, the pediatric revision of the GOS-E showed a distinct advantage in comparison to the GOS. In this case, the child-centered interview format, in addition to expanded categories, probably accounted for the stronger association with everyday outcome and cognitive abilities.
The increased sensitivity of the GOS-E Peds to change across the injury spectrum compared with the GOS endorses the value of using the GOS-E Peds in clinical trials research of pediatric TBI. Although the two instruments were somewhat comparable when assessing change between premorbid function and both post-injury timepoints, the GOS-E Peds provided optimal information regarding recovery. The GOS-E Peds was more strongly associated with changes in functional abilities than was the GOS. Moreover, change in neuropsychological outcome scores was more commonly correlated with the GOS-E Peds at 6 months. Similar to the research findings by Levin and associates (2001), the GOS-E Peds bears enhanced sensitivity to change within the GOS disability levels (i.e., severely disabled, moderately disabled, and good recovery). As researchers increasingly focus on novel therapeutic interventions to improve outcomes associated with TBI in pediatric patients, there is a need for an outcomes measure that can detect changes, even if subtle, in functional status. Whereas GOS-E Peds allowed for a greater detection of change within the instrument's expanded disability categories than the GOS, research directly comparing sensitivity to change between the GOS-E Peds and the VABS is yet to be completed.
Although this study offered the advantage of prospective evaluation, we note several limitations. We did not investigate the validity of the GOS-E Peds when administered outside the clinical setting or by using a variety of administration techniques. For example, with the advent of Skype and technologies used in telemedicine, the GOS-E Peds might be completed via computer. Inclusion of the subgroup of subjects with mild TBI, who evidence few TBI symptoms, may have inflated some of the correlations. However, the persistent correlations observed after stratifying on severity groups reduces the likelihood of significant overestimation. Lastly, this study did not assess the validity of the GOS-E Peds for use with other injury groups or the reliability of the instrument when used by multiple examiners.
Conclusion
Overall, the results of this study demonstrate the advantages of GOS-E Peds. This instrument showed strong association with parent report of functional outcome, including the VABS, and most performance-based cognitive tests for both younger and older children, suggesting it can be used to guide treatment in the early phases of recovery. Because the GOS-E Peds is a downward extension of the GOS-E, an adult instrument with known validity, these two measures of functional outcome can be combined seamlessly in studies of brain injury across the full developmental spectrum. Today, as clinical trials are beginning to explore the effects of treatments past the period of spontaneous recovery, this finding is of importance.
Acknowledgments
This work was supported by National Institute of Neurological Disorders and Stroke (NINDS) grant RO1 NS 38448-01.
Author Disclosure Statement
Salary support for Sue R. Beers, Stephen R. Wisniewski, Rachel Berger, and P. David Adelson, and partial salary support for Michael Bell was provided by the National Institutes of Health. The other authors have no competing financial interests.
References
- Bayley N. Manual for the Bayley Scales of Infant Development. 2nd. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Beers S.R. Levin H.S. Principles and Practice of Pediatric Neurosurgery. Thieme; New York: 2008. Rehabilitation and outcome of head injuries; pp. 848–863. [Google Scholar]
- Clifton G.L. Hayes R.L. Levin H.S. Michel M.E. Choi S.C. Outcome measures for clinical trials involving traumatically brain-injured patients: report of a conference. Neurosurgery. 1992;31:975–978. doi: 10.1227/00006123-199211000-00028. [DOI] [PubMed] [Google Scholar]
- Conners C.K. Conners' Rating Scales –Revised. Multi-Health Systems; Tonawanda, NY: 2001. [Google Scholar]
- Delis D.D. KIH Kaplan E. Ober B.A. California Verbal Learning Test – Child Version, Manual. Psychological Corporation; San Antonio, TX: 1994. [Google Scholar]
- Fiser D.H. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74. doi: 10.1016/s0022-3476(05)82544-2. [DOI] [PubMed] [Google Scholar]
- Fiser D.H. Long N. Roberson P.K. Hefley G. Zolten K. Brodie-Fowler M. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit. Care Med. 2000;28:2616–2620. doi: 10.1097/00003246-200007000-00072. [DOI] [PubMed] [Google Scholar]
- Jennett B. Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- Jennett B. Snoek J. Bond M.R. Brooks N. Disability after severe head injury: observations on the use of the Glasgow Outcome Scale. J. Neurol. Neurosurg. Psychiatry. 1981;44:285–293. doi: 10.1136/jnnp.44.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langlois J. Rutland-Brown W. Thomas K. Traumatic Brain Injury in the United States: Emergency Department Visits, Hosptializations, and Deaths. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, GA: 2004. [Google Scholar]
- Langlois J.A. Sattin R.W. Traumatic brain injury in the United States: research and programs of the Centers for Disease Control and Prevention (CDC) J. Head Trauma Rehabil. 2005;20:187–188. doi: 10.1097/00001199-200505000-00001. [DOI] [PubMed] [Google Scholar]
- Levin H.S. Boake C. Song J. McCauley S. Contant C. Diaz-Marchan P. Brundage S. Goodman H. Kotrla K.J. Validity and sensitivity to change of the extended Glasgow Outcome Scale in mild to moderate traumatic brain injury. J Neurotrauma. 2001;18:575–584. doi: 10.1089/089771501750291819. [DOI] [PubMed] [Google Scholar]
- Murphy K.R. Davidshofer C.O. Psychological Testing: Principles and Applications. 2nd. Prentice Hall; Englewood Cliffs, NJ: 1991. [Google Scholar]
- Sparrow S.S. Bulla D.A. Cicchetti D.V. Vineland Adaptive Behavior Scales –II. Pearson Educational Inc.; Circle Pines, MN: 2006. [Google Scholar]
- Teasdale G. Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;13:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Teasdale G.M. Pettigrew L.E. Wilson J.T. Murray G. Jennett B. Analyzing outcome of treatment of severe head injury: a review and update on advancing the use of the Glasgow Outcome Scale. J. Neurotrauma. 1998;15:587–597. doi: 10.1089/neu.1998.15.587. [DOI] [PubMed] [Google Scholar]
- Thorndike R.L. Hagen E.P. Sattler J. Stanford–Binet Intelligence Scale. 4th. Riverside; Chicago: 1986. [Google Scholar]
- Wechsler D. Weschler Intelligence Scale for Children. 3rd. Psychological Corporation; New York: 1991. [Google Scholar]
- Yeates K.O. Taylor H.G. Predicting premorbid neuropsychological functioning following pediatric traumatic brain injury. J. Clin. Exp. Neuropsychol. 1997;19:825–837. doi: 10.1080/01688639708403763. [DOI] [PubMed] [Google Scholar]


