Abstract
Purpose
Untreated periocular discoid lupus erythematosus (DLE), though very rare, may lead to significant morbidity with lid deformities, trichiasis, and symblepharon formation. We present the largest reported cohort of patients with biopsy-proven DLE solely affecting the periorbital region.
Methods
Observational case series of patients managed over a 7-year period (2004–10).
Results
Seven patients (one male) presented to the Adnexal Service at Moorfields Eye Hospital at a median age of 47 years (range 23–71 years); median interval from symptom onset to biopsy-proven diagnosis was 38 months (range 6–86 months). Changes in peripheral skin were present in 1 patient (occurring after the initial eyelid presentation) and the presenting periocular features were dissimilar across the group, these included: chronic blepharo-conjunctivitis, madarosis, atypical chalazia, depigmentation of the eyelid margin, or marked, persistent periocular oedema with dacryoadenitis.
Two cases settled spontaneously, but five required systemic hydroxychloroquine or intralesional corticosteroid injections.
Conclusion
Periorbital DLE is rare and very varied in its presentation, the protean manifestations often resulting in significant diagnostic delay. All patients with unusual periocular skin disease and those with a refractory inflammatory dermopathy, should undergo biopsy of involved tissue(s), thus leading to earlier diagnosis and prevention of permanent cicatricial periocular changes.
Keywords: discoid lupus erythematosus, eyelid, periorbital oedema, madarosis
Introduction
Discoid lupus erythematosus (DLE) is a chronic autoimmune disease characterised by raised, erythematous, scaly lesions typically affecting sun-exposed areas. Isolated eyelid lesions are rarely the presenting feature of DLE.1 A series of seven patients with palpebral DLE is presented, emphasising the protean clinical signs that can lead to a delay in establishing the diagnosis.
Patients and methods
Seven patients (one male) presented to Moorfields Eye Hospital at a median age of 47 years (range 23–71 years); the median interval from symptom onset to biopsy-proven diagnosis was 38 months (range 6–86 months). The presenting periocular features were dissimilar across the group (Table 1).
Table 1. Summarises the case histories illustrating the protean of periorbital DLE presentations.
| Demographic (age is at onset of symptoms) | Interval to diagnosis (months) | Presentation | Examination findings | Investigations | Treatment and outcome | |
|---|---|---|---|---|---|---|
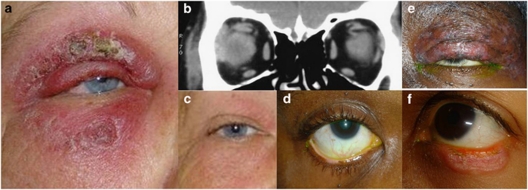
| Patient 1 | 50 F Caucasian | 6 | Painless, progressive periorbital swelling Treated as infective cellulites Concern regarding possible necrotising fasciitis | Significant oedema, violaceous erythema, and eczematous changes (Figure 1a) | CT orbits: enlarged lacrimal gland and extraocular muscles (Figure 1b) Lacrimal gland biopsy: lymphocytic infiltration Punch biopsy right upper lid: perivascular lymphocytic infiltration throughout dermis, lichenoid changes, vacuolar degeneration ANA: positive; dsDNA negative | No improvement with systemic antibiotics or corticosteroids. Spontaneous resolution after discontinuing all treatment |
| Patient 2 | 48 F Afro-Caribbean | 10 | Bilateral sore, itchy lower eyelids | Well-demarcated lid margin depigmentation (Figure 1d) Subtle tarsoconjunctival hypertrophy | Shave biopsy: histological abnormalities consistent with DLE ANA: negative | Significant improvement with hydroxychloroquine (200 mg OD) |
| Patient 3 | 47 F Afro-Caribbean | 38 | Intermittent left upper lid swelling | Atrophic anterior lamella (Figure 1e) Lid margin destruction, complete loss of lashes, patchy depigmentation Scarred meibomian orifices | Punch biopsy: direct immunofluorescence consistent with DLE ANA: negative | Significant improvement with hydroxychloroquine (200 mg OD) and oral corticosteroids Reduced sun exposure Mild residual hypopigmentation |
| Patient 4 | 43 F Asian | 57 | Left lower-lid lesion. Intermittent bleeding | Scaly erythematous plaque (Figure 1f) Shallow ulceration of lid margin, focal madarosis, tarsoconjunctival hyperaemia | Two biopsies: nonspecific inflammation Repeat full thickness biopsy: histological abnormalities consistent with DLE | No improvement with oral corticosteroids Intralesional corticosteroid—partially effective Significant improvement with hydroxychloroquine (200 mg OD) |
| Patient 5 | 23 M Afro-Caribbean | 86 | Recurrent right lower-lid swelling. Treated as atypical chalazion Previous surgical excision—recurrence after 6 months | Disorganised anterior lamella Areas of erosion, erythematous nodules and pigmentation | Full thickness biopsy: hyperkeratosis, perivascular and periadnexal chronic inflammatory cell infiltrate, in keeping with DLE ANA: negative | Improvement on hydroxychloroquine (200 mg OD) Poor compliance led to worsening of the lesion |
| Patient 6 | 46 F Caucasian | 48 | Itching, redness and thickening all four eyelids Previously diagnosed as blepharo-conjunctivitis treated with lid hygiene | Irregular, thickened, fissured lid margins Focal lash loss and conjunctival thickening | Biopsy: cutaneous lymphoid hyperplasia ANA: negative | Spontaneous resolution after discontinuing all treatment |
| Patient 7 | 71 F Caucasian | 18 | Right lower-lid itching and excoriation Treated as blepharitis and allergic dermatitis | Irregular, thickening and madarosis | Full thickness biopsy: lichenoid infiltrate consistent with DLE | Improvement on hydroxychloroquine (200 mg OD) |
Clinical case reports
Patient 1
A 50-year old Caucasian woman presented with 2 months painless, slowly progressive right periorbital swelling, previously treated unsuccessfully with systemic antibiotics for presumed infective cellulitis.
At presentation, prominent oedema and violaceous erythema of the eyelids and forehead was present, with eczematous changes (Figure 1a), but no skin necrosis. Peripherally, there was a maculo-papular knee rash that had been present for 3 weeks. In view of diagnostic uncertainty and chronicity, orbital CT imaging was performed revealing enlargement of the ipsilateral lacrimal gland, superior rectus, and lateral rectus (Figure 1b).
Figure 1.
(Patient1) (a) Violaceous swelling with eczematous changes at presentation; (b) Coronal orbital CT images demonstrate right lacrimal gland, superior and lateral recti enlargement. (c) Facial swelling almost completely resolved without scarring; (Patient 2) (d) Localised lower lid margin depigmentation, preserved lashes, no erythema; (Patient 3) (e) Diffusely bulky left upper eyelid with areas of depigmentation and atrophy; lateral lid margin destruction and madarosis. (Patient 4) (f) Lower lid at presentation shows erythematous, scaly, discoid lesion with madarosis.
Over the next 2 weeks, the periorbital oedema progressed to involve her malar region, despite topical steroid and oral anti-inflammatory medication, prompting a lacrimal gland biopsy. This identified a lymphocytic infiltration but no clues as to a possible aetiology. Oral corticosteroids were discontinued after 1 week due to systemic side effects and no clinical response. A punch biopsy from the right upper lid showed a marked perivascular lymphocytic infiltrate throughout the dermis and basal epidermal layer, with florid lichenoid changes and vacuolar degeneration—these findings being consistent with DLE.
All treatment was discontinued and her condition improved dramatically at 12 months, with no recurrence after 2 years follow up (Figure 1c).
Patient 2
Presenting with a 6-month history of sore and itchy eyes, a 48-year-old Afro-Caribbean female had been managed locally for blepharitis without improvement. The patient had well-demarcated areas of depigmentation on both lower lid margins, but no associated madarosis or erythematous plaques (Figure 1d). Shave biopsy showed chronic inflammation, initially interpreted as chalazia, but subsequently identified by a dermatopathologist as being consistent with DLE. Her cutaneous symptoms and signs resolved significantly on oral hydroxychloroquine.
Patient 3
A 23-year-old Afro-Caribbean male was referred with persistent right lower lid swelling that had been previously treated as atypical chalazion. The patient underwent surgical excision; however, the swelling recurred after 6 months. On examination, the anterior lamellar of the lower eyelid was disorganised, associated with areas of erosion, pigmentation, and erythematous nodules. A full-thickness lid biopsy confirmed features consistent with DLE. Clinical signs improved with oral hydroxychloroquine; however, poor compliance led to subsequent worsening of the lesion.
Discussion
DLE is part of the spectrum of systemic lupus erythematosus. Lesions are typically circumscribed, raised, erythematous and scaly, and are encountered on the face, scalp and ears in 70% of patients.1 Eyelid involvement occurs in only 6% of patients, often associated with other cutaneous abnormalities.2 DLE solely affecting the eyelids is exceptionally rare and is reflected in the diagnostic delay that frequently occurs.3
The wide variation of clinical features among patients with periocular DLE is evident in this series and, indeed, DLE can masquerade convincingly as blepharo-conjunctivitis, allergic dermatitis, psoriasis, lichen planus and basal or sebaceous cell carcinoma. Therefore, DLE should be considered whenever any of these conditions is present and persists despite appropriate medical management.1, 3 Untreated eyelid DLE can lead to significant morbidity from permanent scarring, disorganisation of the muco-cutaneous junction and symblepharon formation.4
In our case series, six out of seven patients were women, with a median diagnostic delay of 38 months. This diagnostic delay is mirrored in a review of 38 patients with eyelid DLE, of whom 58% also had peripheral disease, where a mean diagnostic delay of 2 years was reported.1 In contrast to this cohort, none of the patients described in our series had peripheral skin lesions at the time of presentation.
Our series demonstrates a wide clinical spectrum with only 1 patient presenting with a ‘classical' discoid lesion (Patient 4; Table 1). Although DLE has been reported to present with periorbital oedema,5 the first patient described (Patient 1, Table 1) is unusual both in terms of the extent of disease and, more unexpectedly, the inflammatory involvement of both lacrimal gland and extraocular muscles; the latter phenomenon considered to represent ‘inflammatory spillover' from chronic sub-cutaneous inflammation.
In marked contrast, patient 2 presented with localised depigmentation and no preceding inflammatory changes or plaque formation—a previously unreported, isolated, clinical finding. A female patient has been described, in whom the only presenting feature was madarosis, with subsequent development of a local plaque.6 With such variation in periocular symptoms and signs, the cases reported in this study are a reminder of the high index of suspicion necessary in reaching the correct diagnosis—even in the context of a non-specific previous eyelid biopsy.
Treatment is aimed at preventing progression of existing lesions and avoiding new occurrences. DLE lesions can be photo-sensitive, and patients are therefore advised to protect against sun exposure. Medical treatment includes hydroxychloroquine, which was successful in five of our patients. The marked inflammation in our first patient was ultimately self-limiting and it is of interest (and previously unreported) that this settled without cicatricial sequelae—despite secondary orbital involvement.
Thus, isolated eyelid DLE is rare, can be highly variable in its presentation, posing significant diagnostic challenge. The persistence of inflammatory dermopathy refractory to conventional treatments should prompt the clinician to exclude current or past peripheral skin disease, and consider further biopsies where doubt remains.
The authors declare no conflict of interest.
References
- Huey C, Jakobiec FA, Iwamoto T, Kennedy R, Farmer ER, Green WR. Discoid lupus erythematosus of the eyelids. Ophthalmology. 1983;90:1389–1398. doi: 10.1016/s0161-6420(83)34367-0. [DOI] [PubMed] [Google Scholar]
- Pandhi D, Singal A, Rohtagi J. Eyelid involvement in disseminated chronic cutaneous lupus erythematosus. Indian J Dermatol Venereol Leprol. 2006;72:370–372. doi: 10.4103/0378-6323.27756. [DOI] [PubMed] [Google Scholar]
- Donzis PB, Insler MS, Buntin DM, Gately LE. Discoid lupus erythematosus involving the eyelids. Am J Ophthalmol. 1984;98:32–36. doi: 10.1016/0002-9394(84)90185-5. [DOI] [PubMed] [Google Scholar]
- Frith P, Burge SM, Millard PR, Wojnarowska F. External ocular findings in lupus erythematosus: a clinical and immunopathological study. Br J Ophthalmol. 1990;74:163–167. doi: 10.1136/bjo.74.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams WL, Ramos-Caro FA. Acute periorbital mucinosis in discoid lupus erythematosus. J Am Acad Dermatol. 1999;41:871–873. doi: 10.1016/s0190-9622(99)70348-8. [DOI] [PubMed] [Google Scholar]
- Selva D, Chen C, James C, Huilgol S. Discoid lupus erythematosus presenting as madarosis. Am J Opthalmol. 2003;136:545–546. doi: 10.1016/s0002-9394(03)00231-9. [DOI] [PubMed] [Google Scholar]