Abstract
Purpose
To investigate the effect of orbital decompression surgery in thyroid orbitopathy (TO) on both refractive status and intraocular pressure (IOP).
Patients and methods
A prospective, multicentre, consecutive audit of patients undergoing thyroid decompression surgery. Indications for surgery included cosmetically unacceptable proptosis or corneal exposure. Exclusion criteria included the following: previous orbital surgery, glaucoma, corneal disease, steroid use in the preceding 12 months, or an acute optic neuropathy. Automated refraction, keratometry, pachymetry, Hertel exophthalmometry, and IOP were recorded at 1 month pre- and 3 months postoperatively. IOP using the Tono-Pen (mean of three readings) was measured in the primary, upgaze, and downgaze positions.
Results
Data were collected from 52 orbits of 33 patients (East Grinstead, New York, and Adelaide). There was no significant difference between pre- and postoperative data for sphere, cylinder, or central corneal thickness (CCT). The mean spherical equivalent was −0.43±1.49 D pre-operatively and −0.28±1.52 D postoperatively. The steepest meridian of corneal curvature was 93.1 degrees pre- and 94.2 degrees postoperatively, with no significant difference. Mean IOP significantly decreased when measuring by Goldmann applanation tonometry (GAT) (2.28 mm Hg, * P=0.001) and Tono-Pen (3.06 mm Hg, * P=<0.0001). IOP measured in upgaze was significantly greater than that in the primary position. Regression analysis between change in IOP and either Hertel exophthalmometry or the number of orbital walls decompressed was non-significant (*Student's t-test).
Conclusion
Patients with TO undergoing orbital decompression had, on average, with-the-rule astigmatism not affected by orbital decompression surgery. IOP was significantly reduced by decompression surgery although no relationship between IOP and the degree of decompression was observed.
Keywords: thyroid, orbital decompression, refraction, intraocular pressure, pachymetry
Introduction
Orbital manifestations of thyroid orbitopathy (TO) include soft-tissue swelling, proptosis, fibrosis, diplopia, and optic neuropathy. There is evidence that these changes can give rise to astigmatism1 and raised intraocular pressure (IOP). In addition, the extent of IOP elevation may correlate with the degree of proptosis.2, 3, 4, 5 It is well recognised that IOP will decrease following both fat and bony orbital decompression;6, 7, 8, 9 however, changes in refractive status have been less well investigated. The purpose of this study was to investigate the effect of a varying degree of orbital decompression on both refractive status and IOP in both primary and secondary (up and downgaze) positions.
Materials and methods
We performed a prospective, multicentre audit over 2 years of consecutively recruited patients undergoing thyroid decompression surgery by retrospective note and data-sheet review. We certify that all applicable institutional and governmental regulations concerning ethical practice were followed during this audit.
Where bilateral surgery was performed, the second orbit was decompressed 1 month after the first and data for each eye of the same person were considered as two separate data sets. Indications for surgery included cosmetically unacceptable proptosis or corneal exposure. Exclusion criteria included previous orbital surgery, glaucoma, corneal disease, previous steroid use (in the preceding 12 months), an acute optic neuropathy, or where 3-month follow-up data were not available.
Automated refraction (Topcon KR-8800), autokeratometry (Topcon KR-8800), pachymetry, Hertel exophthalmometry, and IOP were recorded at 1 month pre- and 3 months postoperatively. We planned surgery based on clinical findings; generally in cases of severe proptosis a three-walled decompression is performed to provide the maximal degree of globe retro-placement. In cases of mild/moderate proptosis, an intraconal fat excision is performed (assuming there is evidence of increased volume of fat on orbital imaging) either in isolation, or with a one- or two-walled bony decompression. When performing a one-walled decompression we usually decompress the lateral wall to reduce the risk of diplopia. If this is unlikely to provide enough globe retro-placement, we then opt for a two-walled decompression (medial and deep lateral walls).
Goldmann applanation tonometry (GAT) IOP was measured in the primary position in each eye by an ophthalmologist. The Goldmann tonometer was set to 0 mm Hg, applanation was performed and the dial was rotated, and then the reading was checked. The tonometer was then reset to 0 mm Hg and the procedure was repeated. If two readings differed by more than 2 mm Hg, a third reading was taken. For data analysis, the mean of two readings was taken, and if a third reading was necessary, the median was used as IOP.
The Tono-Pen XL (Medtronic Ophthalmics Inc., Jacksonville, FL, USA) was calibrated for each patient and readings were taken by trained nursing staff. Tonometry was performed in the primary gaze position, 30 degrees upgaze and 30 degrees downgaze. Readings were within the Tono-Pen's <5% error indicator. In each gaze position, two readings were taken to provide a mean. If these differed by more than 2 mm Hg, a third was taken as for GAT.
Objective extra-ocular movements and documentation of diplopia were also recorded. Subgroup analysis was performed analysing the effect of changing the degree of decompression surgery on refractive status and IOP. Patients were subdivided into two groups: Group-A (intraconal fat decompression alone or single-walled orbital decompression; n=19) and Group-B (two or three-walled orbital decompression; n=33). Groups were matched for age, gender, intraconal fat excised, pachymetry, and pre-operative automated refraction.
Literature review
A systematic Medline search on National Institutes of Health's PubMed (http://www.ncbi.nlm.nih.gov/pubmed/; 15 May 2010) was conducted initially using the following keywords: thyroid eye disease, IOP, glaucoma, tonometry, orbital decompression, orbitopathy, astigmatism, and refraction. A list of the most relevant abstracts, and links to these abstracts, was compiled. Complete articles were obtained and reviewed. The references listed in the obtained articles were also reviewed for pertinent citations. The review relied primarily on articles written in English.
Surgical technique
All surgery was performed under general anaesthesia. Local anaesthetic (bupivicaine 0.5% with 1 : 200 000 adrenaline) was infiltrated at the lateral canthus, with medial and lateral peribulbar infiltration.
Swinging eyelid approach
The previously described swinging eyelid approach10, 11 was used to access the intraconal fat and lateral orbit. A standard intraconal fat excision was performed initially through the infero-temporal quadrant, taking care to preserve the lower eyelid fat pads and excise the lighter coloured posterior fat. Fat excision was also performed through the infero-medial quadrant in the same way. Approximately 2 ml of fat were removed with careful haemostasis and the volume was accurately recorded.
Medial orbital wall decompression by a transcaruncular approach
If a two-walled decompression was planned, a medial wall decompression was performed by a standard transcaruncular incision.12 On completion of the bony wall decompression, the medial periorbita was opened to allow further expansion of the orbital contents. When performing a three-walled orbital decompression, the postero-medial floor is decompressed by the transcaruncular approach. We maintain a strut of bone anteriorly at the ethmoid maxillary junction to reduce the risk of consecutive dipoplia and to allow the maxillary sinus to drain.
Lateral orbital wall decompression
The lateral orbital rim was exposed by blunt dissection of the sub-orbicularis plane from the lateral canthal tendon, extending superiorly. The periosteum was incised anterior to the border of the lateral rim and the sub-periosteal space entered in order to visualise the lateral wall from the lacrimal fossa down to the floor of the orbit, allowing full exposure of the greater wing of the sphenoid between the superior and inferior orbital fissures. A deep lateral bony decompression was performed in a standard manner with a diamond burr.11 Following completion of the deep lateral decompression, the periorbita was released and orbital fat prolapsed with blunt separation using curved artery forceps.
Statistical analysis
Two-tailed Student's t-test was used for parametric paired data and Wilcoxon signed-rank test was used for non-parametric, paired data to test for statistical difference pre- and post surgery. Mann–Whitney test was used for non-paired, non-parametric data. For any given parameter, cases were only included if both pre- and postoperative data were available. The XLstat software was used to analyse data.13
Results
Complete, consecutive data were collected for 52 orbits from 33 patients over the study period between three centres (East Grinstead, New York, and Adelaide). Mean age was 52.5±9.4 years. In all, 66.6% (n=22) of the patients were female, and bilateral decompression was performed in 11 (50%) females and 8 (72.7%) males.
Surgery involved intraconal fat only decompression (n=6), one-walled plus intraconal fat excision (n=13), two-walled plus intraconal fat excision (n=26), and three-walled orbital decompression with fat excision (n=7), achieving a globe retro-placement of 2.8±1.7, 4.8±1.9, 4.4±2.1, and 5.6±1.4 mm respectively. The mean number of orbital walls decompressed was 1.6±0.9 and the mean volume of intraconal fat excised was 1.6±0.4 ml. Eleven orbits of seven patients were decompressed because of thyroid-related compressive optic neuropathy, whereas other patients had stable, inactive orbitopathy with corneal exposure and/or proptosis, which was unacceptable to the patient.
Overall pre- and postoperative data
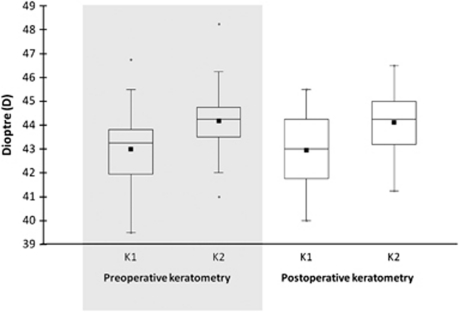
Complete pre- and postoperative refractive data were available for all eyes (Table 1). Mean sphere was +0.13±1.42 dioptres (D) pre-operatively and +0.20±1.45 D postoperatively. The mean pre-operative cylinder was −1.11±0.95 D and −0.97±1.32 D postoperatively. The mean spherical equivalent (SE) was −0.43±1.49 D pre-operatively and −0.28±1.52 D postoperatively. Paired Student's t-testing showed no significant difference between pre- and postoperative data for sphere, cylinder, or SE. Similarly, changes measured in keratometry readings did not reach statistical significance. K1 decreased from 43.00±1.58 to 42.95±1.52 D, whereas K2 decreased from 44.17±1.40 to 44.12±1.40 D (Figure 1). Complete data regarding K axis readings were available for 35 (67.3%) eyes; pre-operatively, the meridian of steepest of corneal curvature was 93.1±27.8 degrees compared with 94.2±22.5 degrees postoperatively, with no significant difference.
Table 1. Comparison of Group-A (intraconal fat with or without a one-walled orbital decompression) versus Group-B (2- to 3-walled orbital decompression).
| Overall data | Group-A | Group-B | P-value | |
|---|---|---|---|---|
| Number of eyes | 52 | 19 | 33 | — |
| Age | 52.5 (9.4) | 51.9 (11.5) | 52.8 (8.1) | 0.84a |
| Gender (% female) | 66.6 | 78.9 | 54.5 | 0.75b |
| Number of walls decompressed | 1.6 (0.9) | 0.7 (0.5) | 2.2 (0.4) | <0.0001a |
| Mean volume of intraconal fat excised (ml) | 1.6 (0.4) | 1.6 (0.6) | 1.5 (0.3) | 0.75a |
| Sphere (Dioptres (D)) | ||||
| Pre-operative | 0.13 (1.42) | 0.14 (0.16) | 0.12 (1.13) | 0.88a |
| Postoperative sphere | 0.20 (1.45) | 0.56 (1.84) | 0.01 (0.12) | 0.10a |
| Difference | 0.07 | 0.38 | −0.11 | |
| P-valuec | 0.79 | 0.47 | 0.73 | |
| Cylinder (D) | ||||
| Pre-operative | −1.11 (0.95) | −1.09 (0.83) | −1.12(1.39) | 0.78a |
| Postoperative | −0.97 (1.31) | −1.14 (1.32) | −0.87 (1.32) | 0.65a |
| Difference | 0.14 | −0.05 | 0.25 | |
| P-valuec | 0.56 | 0.88 | 0.44 | |
| Spherical equivalent (D) | ||||
| Pre-operative | −0.43 (1.49) | −0.40 (1.78) | −0.26 (0.82) | 0.98a |
| Postoperative | −0.28 (1.52) | −0.01 (1.88) | −0.44 (1.30) | 0.10a |
| Difference | 0.15 | 0.39 | −0.18 | |
| P-valuec | 0.62 | 0.52 | 0.52 | |
| Keratometry (K1) (D) | ||||
| Pre-operative | 43.00 (1.58) | 42.51 (1.38) | 43.29 (1.63) | 0.10a |
| Postoperative | 42.95 (1.52) | 42.81 (1.39) | 43.02 (1.60) | 0.07a |
| Difference | 0.05 | 0.3 | −0.27 | |
| P-valuec | 0.85 | 0.51 | 0.51 | |
| Keratometry (K2) (D) | ||||
| Pre-operative | 44.17 (1.40) | 43.75 (1.03) | 44.41 (1.53) | 0.04a |
| Postoperative | 44.12 (1.40) | 43.84 (1.18) | 44.26 (1.51) | 0.55a |
| Difference | −0.05 | 0.09 | −0.15 | |
| P-valuec | 0.85 | 0.77 | 0.26 | |
| K axis (degrees) | ||||
| Pre-operative | 93.1 (27.8) | 89.4 (26.2) | 96.7 (29.5) | 0.29a |
| Postoperative | 94.2 (22.5) | 91.2 (21.7) | 97.1 (23.5) | 0.39a |
| Difference | 1.1 | 1.8 | −0.4 | |
| P-valuec | 0.86 | 0.83 | 0.64 | |
| Hertel exophthalmometry (mm) | ||||
| Pre-operative | 24.1 (2.8) | 22.6 (2.5) | 24.8 (2.7) | 0.01a |
| Postoperative | 19.5 (2.16) | 18.5 (1.8) | 20.1 (2.2) | 0.28a |
| Difference | 4.6 | 4.1 | 4.7 | |
| P-valuec | <0.0001 | <0.0001 | <0.0001 | |
| Pachymetry (μm) | ||||
| Pre-operative | 542.9 (32.8) | 540.6 (41.9) | 547.3 (26.6) | 0.766a |
| Postoperative | 544.4 (29.2) | 540.9 (39.8) | 547.1 (21.1) | 0.61a |
| Difference | 1.5 | 0.3 | 0.2 | |
| P-valuec | 0.83 | 0.85 | 0.97 | |
Mann–Whitney test (two-tailed).
Fisher's exact test.
Student's t-test.
Significant P-values are indicated in bold.
Figure 1.
Univariate plot highlighting the keratometry readings pre- and post orbital decompression surgery. With-the-rule astigmatism was present both pre- (mean axis 93.1 degrees) and post decompression surgery (mean axis 94.2 degrees). Mean values are illustrated (▪).
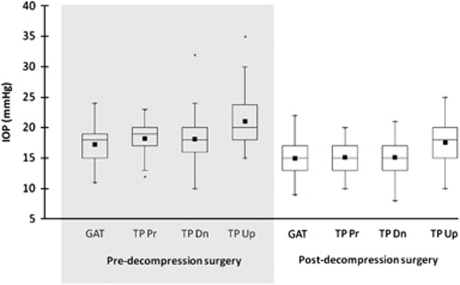
Mean central corneal thickness (CCT) was 542.9±32.8 μm pre- and 544.4±29.2 μm post surgery (n=45, P=0.83). The mean GAT measured in the primary position decreased by 2.28 mm Hg, from 17.26±2.96 to 14.97±2.60 mm Hg (n=39, P=0.001) (Figure 2). Tono-Pen primary position IOP reduced by 3.06 mm Hg, from 18.16±2.67 mm Hg before surgery to 15.10±2.59 mm Hg following surgery (n=51, P=<0.0001). For all primary position readings, Tono-Pen was, on average, 0.71 mm Hg greater than GAT, which was not significant (n=83, P=0.13).
Figure 2.
Univariate plot illustrating pre- and post orbital decompression surgery IOP measurements with GAT and Tono-Pen XL (TP) in the primary (Pr), downgaze (Dn), and upgaze positions (Up). Mean values are illustrated (▪).
Mean pre-operative IOP in downgaze was 18.13±3.78 mm Hg compared with 15.08±3.39 mm Hg postoperatively, a reduction of 3.04 mm Hg (n=48, P=<0.0001). Downgaze IOP did not significantly vary from primary position IOP, either pre- or post surgery. Moreover, the actual reduction in IOP (in downgaze) was not significantly different from that measured in the primary position.
Mean pre-operative IOP in upgaze was 21.04±4.42 mm Hg compared with 17.56±3.54 mm Hg postoperatively, an improvement of 3.8 mm Hg (n=50, P=<0.0001). Pre-operative (P=0.001) and postoperative IOP (P=0.0003) recorded in upgaze were significantly higher than in the primary position. The change in IOP was again not significantly different from change in the primary position IOP.
Preoperative diplopia was present in 12 patients (36.4%), which resolved in six following orbital decompression. For patients with persistent diplopia, either strabismus surgery was performed between 6 and 18 months after decompression surgery (n=4), which resulted in resolution of diplopia, or patients were successfully managed with prisms alone (n=2). Two (6.1%) patients had new-onset diplopia (grade-4) present at 6 months post decompression surgery (constantly present in both primary and secondary gaze), with one requiring subsequent muscle recession surgery and one treated with prisms alone. Five patients experienced new-onset diplopia in secondary gaze, which spontaneously resolved in within 6 months of surgery.
Preoperative K2 was significantly higher in Group-B vs Group-A (43.75 vs 44.41 D, P=0.04). There was no statistical difference between groups for postoperative change in sphere, cylinder, SE, or keratometry.
In Group-A, IOP in the primary, downgaze, and upgaze positions improved by 3.28±2.02, 3.06±3.44, and 3.94±3.23 mm Hg, respectively. In Group-B, IOP in the primary, downgaze, and upgaze positions improved by 2.94±3.45, 3.03±4.73, and 3.22±4.98 mm Hg, respectively. GAT in Group-A improved by 2.47±2.26 mm Hg vs 2.17±3.32 mm Hg in Group-B. There was no statistical difference between groups for postoperative improvement in IOP when measuring with the Tono-Pen in the primary and secondary positions, or for GAT in the primary position. Regression analysis revealed no significant association between either the degree of retro-placement (R2=0.042) and change in IOP, or the number of orbital walls decompressed and IOP (R2=0.016).
Discussion
The aim of this study was to investigate the effect of orbital decompression surgery on refractive status and IOP. Patients with TO requiring decompression surgery had, on average, with-the-rule astigmatism. Decompression surgery did not significantly alter the refractive status or the central corneal thickness. We highlight the use of the Tono-Pen in measuring IOP in TO patients particularly in secondary gaze positions enabling central corneal applanation. Using this technique we conclude that orbital decompression significantly reduces IOP in both the primary and secondary positions, but does not seem to affect refractive status.
There have been relatively few reports in the literature on the effect of TO and decompression surgery on refraction. Mombaerts et al1 reviewed corneal astigmatism retrospectively in 109 patients with inactive Graves' ophthalmopathy. They found significantly increased with-the-rule astigmatism when compared with a control group, which was not influenced by orbital, strabismus, or eyelid surgery. They postulated that the cause was soft tissue fibrosis in the supero-orbital region and that three processes can lead to corneal astigmatism of the cornea, including changes in the corneal epithelium, alteration in corneal thickness, and external compression by intra-orbital forces. In their study, 32 patients underwent orbital decompression, of which 73% had no change in astigmatism postoperatively at 5 months. The degree of orbital decompression, however, was not described. We also found pre- and postoperative with-the-rule astigmatism using automated keratometry, with the steepest meridian of corneal curvature at 93.1 and 94.2 degrees, respectively, with no significant difference demonstrated post surgery. Kwitko et al14 found that SE increased postoperatively by a mean of 0.53±0.30 D in patients who underwent inferior rectus recession with or without medial rectus recession for TO, although this change was not found to be clinically significant. They concluded that mass changes around the globe, including that of the eyelid and within the orbit, in TO can produce changes in corneal curvature. They hypothesised that it may be a change in the IOP that might actually cause flattening of the cornea. Jankauskiene et al15 reviewed 105 patients with TO and compared with a control group of 23 normal subjects. They reported that patients were more likely to be myopic in the thyroid group particularly if proptosis of ⩾17 mm Hg was present. Sagili et al16 also found that, pre-operatively 72% of eyes were myopic, with no statistical difference in SE postoperatively. We similarly found that 61.5% of eyes were pre-operatively myopic (mean SE −0.43 D), although the degree of myopia was not affected by the level of proptosis. Our cohort was a select group of patients with TO who required orbital decompression, and so direct comparisons between the studies cannot be made. Chandrasekaran et al17 performed a retrospective observational case series in five patients with progressive TO. They found an acquired hypermetropic shift prior to orbital decompression in one patient. Postoperatively they reported an induced myopic shift of 1.00–2.50 D in all patients, concluding that thyroid eye disease (TED) has a significant effect on the refractive state of patients, and proposed that this was due to flattening of the posterior globe, which is reversible in the event of orbital decompression. This was obviously a small cohort of non-consecutive patients and therefore may not be representative of the majority of patients. We conversely found a non-significant, mean hypermetropic shift of 0.15 D from pre- to post orbital decompression. In our study, patients who underwent either a one-walled decompression or intraconal fat excision alone had a postoperative hypermetropic shift of 0.39 D compared with the two- and three-walled group who had a myopic shift of 0.18 D, although this difference was not significant. We also found no significant differences in keratometry or pachymetry between groups.
Raised IOP is a well-recognised complication of TO. Mechanisms for elevation of IOP include congestive orbitopathy with secondary elevation of episcleral venous pressure,18 increased retrobulbar pressure,19 contraction of extra-ocular muscles with increased pressure on the globe,20, 21 increased mucopolysaccharide deposition within the trabecular meshwork, genetic predisposition, and rarely angle closure glaucoma.4, 22 The primary association of primary open-angle glaucoma (POAG) and thyroid dysfunction has been disputed, with a prevalence of between 0 and 6.5%. Most reports, however, have not found a significant association between thyroid dysfunction and POAG (Table 2).2, 23, 24, 25, 26, 27 No patients were excluded from this audit because of a diagnosis of POAG, nor were any patients treated on ocular anti-hypertensive treatments prior to decompression surgery.
Table 2. A summary of previous studies evaluating the association between thyroid disease, and OHT and OAG.
| Study | Review group | No. | Prevalence of thyroid dysfunction | Prevalence of raised IOP | Control | Significant association |
|---|---|---|---|---|---|---|
| Behrouzi et al23 | TO | 233 (E) | — | 8.5% OHT 2.5% POAG | Yes Yes | Yes No |
| Cheng and Perkins2 | Thyroid dysfunction | 155 | — | 1.3% POAG | No | No |
| Cockerham et al28 | TO | 500 (P) | — | 24% OHT | Yes | — |
| Cross et al41 | Thyroid dysfunction | 1472 (P) | — | 6.5% POAG | Yes | Yes |
| Gillow et al24 | POAG | 100 (P) | 4% | — | Yes | No |
| Kalmann and Mourits7 | TO | 482 (P) | — | 0.8% POAG | No | No |
| Karamadis et al25 | Hypothyroid | 100 (P) | — | 0% POAG | No | No |
| Lee et al26 | Thyroid dysfunction | 324 (P) | — | 4.6% POAG | Yes | No |
| Motsko and Jones27 | POAG | 4728 (P) | 17.2% | — | Yes | No |
| Ohtsuka8 | TO | 190 (E) | — | 22.1% OHT | No | — |
| Smith et al42 | POAG | 64 (P) | 23.4% | — | Yes | Yes |
Abbreviations: E, number of eyes; OHT, ocular hypertension; P, number of patients; POAG, primary open-angle glaucoma.
Cockerham et al28 in a study of 500 consecutive patients with TO found raised IOP (22–30 mm Hg) in 24% of the patients, reporting that the duration of active orbital involvement was significantly linked to the progression of glaucomatous damage. Pre-operatively, 19.6% of patients in our study had an IOP of between 21 and 30 mm Hg. Orbital decompression surgery as one would expect is known to reduce IOP, and this is reflected in this audit and in the published literature (Table 3). The most accepted theory explaining this reduction in IOP relates to a decrease in intra-orbital volume, reducing retrobulbar and episcleral venous pressure.19
Table 3. A review of studies evaluating change in IOP after orbital decompression surgery.
| Study | Type | No. | Type of decompression | Mean pre-operative IOP | Mean postoperative IOP | Follow-up | Significance |
|---|---|---|---|---|---|---|---|
| Danesh-Meyer et al6 | R | 116 | 2 wall (inferior/medial) | 21.6±4.6 | 17.5±3.0 | 2–6 weeks | Yes |
| Dev et al43 | R | 22 | 2–3 wall | 19.8 | 16.8 | 10 weeks | Yes |
| Ohtsuka8 | ? | 6 | 2 wall (inferior/medial) | 23.23 | 18.82 | 3–52 weeks | Yes |
| Robert et al9 | P | 64 | Intraconal fat only | 19.3±4.4 | 15.9±3.7 | 6 months | Yes |
| Sagili et al16 | R | 18 | Intraconal fat±2–3 wall | 17.6±2.8 | 16.3±2.9 | 3 months | No |
Abbreviations: P, prospective; R, retrospective.
Some studies do not either record IOP in the secondary position or comment on the method of IOP measurement.6, 28, 29 In the secondary position we believe that the Tono-Pen should be considered as a suitable alternative to GAT, allowing central corneal applanation (which is not possible using GAT).
This audit standardises for CCT, which has not been well described previously5, 6, 7, 8, 9, 16, 28, 29 and is known to significantly affect IOP.30 Goldberg31 commented that in patients with TO, central corneal thickness is a confounder for accurate tonometry, and that apparent changes in IOP could be simply due to increases in CCT. By contrast, we found that orbital decompression did not significantly affect CCT, so would dispute this theory, but acknowledge that CCT is important in determining whether or not to commence ocular anti-hypertensive therapy.
We highlight the use of the Tono-Pen, which we found easier to use than GAT and supported by Rahman et al.32 We found the Tono-Pen particularly useful for measuring IOP in secondary gaze positions. Rahman et al32 found no statistical difference between IOP measured using the Tono-Pen XL and GAT in 31 thyroid patients with restrictive eye disease. Frenkel et al33 found 63% of the Tono-Pen readings to be within ±2 mm Hg of the GAT readings. They concluded that Tono-Pen IOP measurements correspond well with GAT in the 11- to 20-mm Hg interval, and moderately well in the 21- to 30-mm Hg interval, but poorly in the 31- to 45-mm Hg interval. We found similar overall results in this study, with a mean, non-significant difference between Tono-Pen and GAT in the primary position of 0.71 mm Hg. One known drawback of the Tono-Pen is the degree of variability and repeatability;30 we aimed to reduce this by taking a mean of two IOP readings. We then took a third reading if the initial two readings were >2 mm Hg apart and used the median.
It is well recognised that IOP in normal subjects will change with globe position, and Wessely34 in 1918 first described increased IOP in upgaze in patients with TO. Fishman and Benes20 reviewed IOP in upgaze specifically in patients with TO, finding that there was a difference in IOP of greater than or equal to 3 mm Hg in at least one eye of 91% of patients. A raised IOP in upgaze should alert the examiner of likely muscle restriction, rather than using subjective forced duction testing.33, 35
We had no direct surgical complications in this study, although we did observe persistent new-onset diplopia at 6 months post decompression in 2 (6.1%) patients, which is similar to other reports.36, 37, 38, 39, 40
This audit was of a prospective design but not blinded and this should be recognised, along with the limitations that this carries. In addition, several trained nursing staff took measurements using the Tono-Pen and ophthalmologists used the GAT. We have not calculated inter-observer variability, which again should be acknowledged. As discussed, the relationship between raised IOP and thyroid dysfunction has been well reported. However, relatively few authors have described the changes in IOP and refractive status following orbital decompression, and pachymetry data in these patients are not well reported. This is one of only a few studies to investigate changes in refractive status in TO and one of the first to analyse IOP measurements in all three positions of gaze using the Tono-Pen. We did consider using the Perkins tonometer for this purpose, which would perhaps more accurately reflect GAT, but found the Tono-Pen to be a more practical option in the clinical setting. Perhaps further studies could investigate the use of Perkins tonometry in patients with TO and compare with Tono-Pen in secondary positions. We reviewed patients at 3 months post surgery; it would be interesting to have a longer term follow-up in terms of IOP to see if there is a refractory upward trend with time.
Conclusion
This study confirms that patients with TO have, on average, with-the-rule astigmatism, and orbital decompression does not seem to significantly affect refraction status or central corneal thickness. IOP was significantly reduced by decompression surgery, although no relationship between IOP and the degree of decompression was observed. We also conclude that the Tono-Pen is a useful and accurate tool in measuring IOP both in the primary and secondary positions.
Acknowledgments
We thank Vikesh Patel for help with the study.
The authors declare no conflict of interest.
References
- Mombaerts I, Vandelanotte S, Koornneef L. Corneal astigmatism in Graves' ophthalmopathy. Eye (Lond) 2006;20 (4:440–446. doi: 10.1038/sj.eye.6701898. [DOI] [PubMed] [Google Scholar]
- Cheng H, Perkins ES. Thyroid disease and glaucoma. Br J Ophthalmol. 1967;51 (8:547–553. doi: 10.1136/bjo.51.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad HM. Tonography and visual fields in endocrine exophthalmos. Report on 29 patients. Am J Ophthalmol. 1967;64 (1:63–67. doi: 10.1016/0002-9394(67)93344-2. [DOI] [PubMed] [Google Scholar]
- Manor RS, Kurz O, Lewitus Z. Intraocular pressure in endocrinological patients with exophthalmos. Ophthalmologica. 1974;168 (4:241–252. doi: 10.1159/000307046. [DOI] [PubMed] [Google Scholar]
- Pohjanpelto P.The thyroid gland and intraocular pressure. Tonographic study of 187 patients with thyroid disease Acta Ophthalmol (Copenh) 196897(Suppl): 1–70. [PubMed] [Google Scholar]
- Danesh-Meyer HV, Savino PJ, Deramo V, Sergott RC, Smith AF. Intraocular pressure changes after treatment for Graves' orbitopathy. Ophthalmology. 2001;108 (1:145–150. doi: 10.1016/s0161-6420(00)00477-2. [DOI] [PubMed] [Google Scholar]
- Kalmann R, Mourits MP. Prevalence and management of elevated intraocular pressure in patients with Graves' orbitopathy. Br J Ophthalmol. 1998;82 (7:754–757. doi: 10.1136/bjo.82.7.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuka K. Intraocular pressure and proptosis in 95 patients with Graves ophthalmopathy. Am J Ophthalmol. 1997;124 (4:570–572. doi: 10.1016/s0002-9394(14)70883-9. [DOI] [PubMed] [Google Scholar]
- Robert PY, Rivas M, Camezind P, Rulfi JY, Adenis JP. Decrease of intraocular pressure after fat-removal orbital decompression in Graves disease. Ophthal Plast Reconstr Surg. 2006;22 (2:92–95. doi: 10.1097/01.iop.0000203737.67334.d3. [DOI] [PubMed] [Google Scholar]
- Paridaens D, Lie A, Grootendorst RJ, van den Bosch WA. Efficacy and side effects of ‘swinging eyelid' orbital decompression in Graves' orbitopathy: a proposal for standardized evaluation of diplopia. Eye (Lond) 2006;20 (2:154–162. doi: 10.1038/sj.eye.6701827. [DOI] [PubMed] [Google Scholar]
- Rootman J, Stewart B, Goldberg RA. Orbital Surgery: a Conceptual Approach. Lippincott-Raven: Philadelphia; 1995. Decompression for thyroid orbitopathy; pp. 353–384. [Google Scholar]
- Shorr N, Baylis HI, Goldberg RA, Perry JD. Transcaruncular approach to the medial orbit and orbital apex. Ophthalmology. 2000;107 (8:1459–1463. doi: 10.1016/s0161-6420(00)00241-4. [DOI] [PubMed] [Google Scholar]
- www.XLstat.com (accessed on February 2010).
- Kwitko S, Feldon S, McDonnell PJ. Corneal topographic changes following strabismus surgery in Grave's disease. Cornea. 1992;11 (1:36–40. doi: 10.1097/00003226-199201000-00005. [DOI] [PubMed] [Google Scholar]
- Jankauskiene J, Jakstaite V, Smalinskas V. Changes of vision and refraction in patients with thyroid pathology. Medicina (Kaunas) 2009;45 (5:378–381. [PubMed] [Google Scholar]
- Sagili S, Desousa JL, Malhotra R. Intraocular pressure and refractive changes following orbital decompression with intraconal fat excision. Open Ophthalmol J. 2008;2:73–76. doi: 10.2174/1874364100802010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekaran S, Petsoglou C, Billson FA, Selva D, Ghabrial R. Refractive change in thyroid eye disease (a neglected clinical sign) Br J Ophthalmol. 2006;90 (3:307–309. doi: 10.1136/bjo.2005.078295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinreb RN, Karwarowski W.Glaucoma associated with raised episcleral venous pressureIn: Ritch R, Shields MB, Krupin T (eds).The Glaucomas CV Mosby: St Louis; 19961143–1155. [Google Scholar]
- Otto AJ, Koornneef L, Mourits MP, Deen-van Leeuwen L. Retrobulbar pressures measured during surgical decompression of the orbit. Br J Ophthalmol. 1996;80 (12:1042–1045. doi: 10.1136/bjo.80.12.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman DR, Benes SC. Upgaze intraocular pressure changes and strabismus in Graves' ophthalmopathy. J Clin Neuroophthalmol. 1991;11 (3:162–165. [PubMed] [Google Scholar]
- Saunders RA, Helveston EM, Ellis FD. Differential intraocular pressure in strabismus diagnosis. Ophthalmology. 1981;88 (1:59–70. doi: 10.1016/s0161-6420(81)35076-3. [DOI] [PubMed] [Google Scholar]
- Goldberg I. Thyroid eye disease and glaucoma. J Glaucoma. 2003;12 (6:494–496. doi: 10.1097/00061198-200312000-00010. [DOI] [PubMed] [Google Scholar]
- Behrouzi Z, Rabei HM, Azizi F, Daftarian N, Mehrabi Y, Ardeshiri M, Mohammadpour M. Prevalence of open-angle glaucoma, glaucoma suspect, and ocular hypertension in thyroid-related immune orbitopathy. J Glaucoma. 2007;16 (4:358–362. doi: 10.1097/IJG.0b013e31802e644b. [DOI] [PubMed] [Google Scholar]
- Gillow GT, Shah P, O'Neill EC. Primary open angle glaucoma and hypothyroidism: chance or true association. Eye. 1997;11 (Pt 1:113–114. doi: 10.1038/eye.1997.22. [DOI] [PubMed] [Google Scholar]
- Karadimas P, Bouzas EA, Topouzis F, Koutras DA, Mastorakos G. Hypothyroidism and glaucoma. A study of 100 hypothyroid patients. Am J Ophthalmol. 2001;131 (1:126–128. doi: 10.1016/s0002-9394(00)00724-8. [DOI] [PubMed] [Google Scholar]
- Lee AJ, Rochtchina E, Wang JJ, Healey PR, Mitchell P. Open-angle glaucoma and systemic thyroid disease in an older population: The Blue Mountains Eye Study. Eye. 2004;18 (6:600–608. doi: 10.1038/sj.eye.6700731. [DOI] [PubMed] [Google Scholar]
- Motsko SP, Jones JK. Is there an association between hypothyroidism and open-angle glaucoma in an elderly population? An epidemiologic study. Ophthalmology. 2008;115 (9:1581–1584. doi: 10.1016/j.ophtha.2008.01.016. [DOI] [PubMed] [Google Scholar]
- Cockerham KP, Pal C, Jani B, Wolter A, Kennerdell JS. The prevalence and implications of ocular hypertension and glaucoma in thyroid-associated orbitopathy. Ophthalmology. 1997;104 (6:914–917. doi: 10.1016/s0161-6420(97)30207-3. [DOI] [PubMed] [Google Scholar]
- Adenis JP, Robert PY, Lasudry JG, Dalloul Z. Treatment of proptosis with fat removal orbital decompression in Graves' ophthalmopathy. Eur J Ophthalmol. 1998;8 (4:246–252. doi: 10.1177/112067219800800408. [DOI] [PubMed] [Google Scholar]
- Tonnu PA, Ho T, Sharma K, White E, Bunce C, Garway-Heath D. A comparison of four methods of tonometry: method agreement and interobserver variability. Br J Ophthalmol. 2005;89:847–850. doi: 10.1136/bjo.2004.056614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg I. Thyroid eye disease and glaucoma. J Glaucoma. 2003;12 (6:494–496. doi: 10.1097/00061198-200312000-00010. [DOI] [PubMed] [Google Scholar]
- Rahman I, Cannon PS, Sadiq SA. Tonopen versus Goldmann applanation tonometry for detecting restrictive thyroid eye disease. Ophthal Plast Reconstr Surg. 2010;26 (1:36–38. doi: 10.1097/IOP.0b013e3181b80fcb. [DOI] [PubMed] [Google Scholar]
- Frenkel RE, Hong YJ, Shin DH. Comparison of the Tono-Pen to the Goldmann applanation tonometer. Arch Ophthalmol. 1988;106 (6:750–753. doi: 10.1001/archopht.1988.01060130820030. [DOI] [PubMed] [Google Scholar]
- Wessely K. Discussion of Hertel E. Weiterer Beitrag zur Lehre von Augendruck. Ber Dtsch Ophthalmol Ges. 1918;41:80–81. [Google Scholar]
- Zappia RJ, Winkelman JZ, Gay AJ. Intraocular pressure changes in normal subjects and the adhesive muscle syndrome. Am J Ophthalmol. 1971;71 (4:880–883. doi: 10.1016/0002-9394(71)90259-5. [DOI] [PubMed] [Google Scholar]
- Roberts CJ, Murphy MF, Adams GG, Lund VJ. Strabismus following endoscopic orbital decompression for thyroid eye disease. Strabismus. 2003;11 (3:163–171. doi: 10.1076/stra.11.3.163.16652. [DOI] [PubMed] [Google Scholar]
- Cruz AA, Leme VR. Orbital decompression: a comparison between trans-fornix/transcaruncular inferomedial and coronal inferomedial plus lateral approaches. Ophthal Plast Reconstr Surg. 2003;19 (6:440–445. doi: 10.1097/01.IOP.0000092796.43025.B1. [DOI] [PubMed] [Google Scholar]
- Liao SL, Kao SC, Hou PK, Chen MS. Results of orbital decompression in Taiwan. Orbit. 2001;20 (4:267–274. doi: 10.1076/orbi.20.4.267.2615. [DOI] [PubMed] [Google Scholar]
- McNab AA. Orbital decompression for thyroid orbitopathy. Aust N Z J Ophthalmol. 1997;25 (1:55–61. doi: 10.1111/j.1442-9071.1997.tb01276.x. [DOI] [PubMed] [Google Scholar]
- Paridaens DA, Verhoeff K, Bouwens D, van Den Bosch WA. Transconjunctival orbital decompression in Graves' ophthalmopathy: lateral wall approach ab interno. Br J Ophthalmol. 2000;84 (7:775–781. doi: 10.1136/bjo.84.7.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross JM, Girkin CA, Owsley C, McGwin G.JrThe association between thyroid problems and glaucoma. Br J Ophthalmol 200892(111503–1505. [DOI] [PMC free article] [PubMed]
- Smith KD, Arthurs BP, Saheb N. An association between hypothyroidism and primary open-angle glaucoma. Ophthalmology. 1993;100 (10:1580–1584. doi: 10.1016/s0161-6420(93)31441-7. [DOI] [PubMed] [Google Scholar]
- Dev S, Damji KF, DeBacker CM, Cox TA, Dutton JJ, Allingham RR. Decrease in intraocular pressure after orbital decompression for thyroid orbitopathy. Can J Ophthalmol. 1998;33 (6:314–319. [PubMed] [Google Scholar]