Abstract
Purpose:
To provide an overview of the characteristics and timing of rotator cuff healing and provide an update on treatments used in rehabilitation of rotator cuff repairs. The authors' protocol of choice, used within a large sports medicine rehabilitation center, is presented and the rationale behind its implementation is discussed.
Background:
If initial nonsurgical treatment of a rotator cuff tear fails, surgical repair is often the next line of treatment. It is evident that a successful outcome after surgical rotator cuff repair is as much dependent on surgical technique as it is on rehabilitation. To this end, rehabilitation protocols have proven challenging to both the orthopaedic surgeon and the involved physical therapist. Instead of being based on scientific rationale, traditionally most rehabilitation protocols are solely based on clinical experience and expert opinion.
Methods:
A review of currently available literature on rehabilitation after arthroscopic rotator cuff tear repair on PUBMED / MEDLINE and EMBASE databases was performed to illustrate the available evidence behind various postoperative treatment modalities.
Results:
There is little high-level scientific evidence available to support or contest current postoperative rotator cuff rehabilitation protocols. Most existing protocols are based on clinical experience with modest incorporation of scientific data.
Conclusion:
Little scientific evidence is available to guide the timing of postsurgical rotator cuff rehabilitation. To this end, expert opinion and clinical experience remains a large facet of rehabilitation protocols. This review describes a rotator cuff rehabilitation protocol that incorporates currently available scientific literature guiding rehabilitation.
Keywords: Arthroscopic rotator cuff repair, rehabilitation, scientific rationale
INTRODUCTION
Rotator cuff (RC) disease is a frequent cause of shoulder pain and can result in weakness, alterations in glenohumeral kinematics, and shoulder instability in some circumstances.1 Symptomatic rotator cuff tears are thought to affect between 4% and 32% of the population and appear to be more prevalent with increasing age.2 Although patient age, activity level and tear size influence surgical decision-making, non-surgical management is frequently the preferred method of initial treatment after a rotator cuff tear. When non-surgical management of a symptomatic rotator cuff tear is not successful, operative repair is frequently necessary. Both open and arthroscopic repair of full or high-grade partial thickness rotator cuff tears have historically provided satisfactory pain relief and improvement in functional outcome scores.3–9
While successful arthroscopic rotator cuff repair requires meticulous surgical technique, it is also apparent that an individualized rehabilitation protocol supervised by skilled therapists is equally important. Rehabilitation protocols have traditionally varied considerably among providers with respect to timing of progression and appropriate therapeutic exercise.10 To this end, rehabilitation protocols are frequently based on clinical experience and expert opinion rather than scientific rationale.
The purpose of this clinical commentary, therefore, is to provide an update on current treatment strategies used in rotator cuff repair rehabilitation. The scientific rationale behind current treatment strategies is discussed where available.
ANATOMY AND BIOMECHANICS
The RC consists of the tendons of the subscapularis, supraspinatus, infraspinatus, and teres minor muscles. It functions to initiate glenohumeral joint abduction, provide internal and external rotation, and contributes to dynamic glenohumeral stability.2 It has been established that the rotator cuff is arranged histologically into five interlocking layers with distinct articular and bursal sides.11 The humeral insertion of the rotator cuff represents a confluence of the articular capsule, glenohumeral and coracohumeral ligaments, and the rotator cuff muscles.12–14
The coupled force vectors of the subscapularis and teres minor muscles contribute to depression of the humeral head in the glenoid cavity. This provides dynamic stability to the glenohumeral joint and prevents impingement of the humeral head with the acromion during deltoid activation. They also function to prevent superior translation of the humeral head after rotator cuff tear.15 Contrary to the rotator cuff tendons' ability to tolerate up to 100 N/mm of tensile strength, the tendons' endurance of compressive and shear forces is much less.16
The scapula also plays an important role in glenohumeral function by providing a stable base for muscle activation and load transfer within the kinetic chain. Alteration in normal scapular position or kinematics has been termed scapular dyskinesis and can affect rotator cuff function.17 Scapular dyskinesia has also been described following rotator cuff tears and is thought to represent a compensatory mechanism for glenohumeral motion deficits.18 Irritation and inflammation of the subacromial bursa, which is rich in nerve fibers, can also lead to pain inhibition of the rotator cuff.19
TENDON HEALING POTENTIAL
Though some partial-thickness and some small full thickness tears of the rotator cuff may heal spontaneously without surgical intervention, the natural history of rotator cuff injury appears to indicate that most small tears will enlarge if not surgically repaired.20 It remains unclear, however, over what time period this is likely to occur, but enlargement is typically associated with increased pain and dysfunction. Healing of ruptured rotator cuff tendons, therefore, only occurs when the tendon is surgically repaired back to its footprint on the proximal humerus.
Histological studies suggest that three phases of rotator cuff healing occur after surgical repair. These include an inflammatory phase, a proliferative or repair phase, and a remodeling phase.21 A firm understanding of the timing of these phases is important to safely individualize rehabilitation protocols after rotator cuff repair. Following surgical tendon-to-bone fixation, inflammatory cells followed by platelets and fibroblasts migrate into the repair site over the first week and begin to proliferate over the next 2–3 weeks. The cellular proliferation and matrix deposition of this phase is thought to be regulated by several growth factors and initially yields primarily type III collagen.22 Approximately three to four weeks following repair, the remodeling phase begins and scar tissue organizes through extracellular matrix turnover. The initial type III collagen deposition is slowly replaced by type I collagen, continuing until mature scar tissue is formed.22 Remodeling repair tissue does not reach maximal tensile strength for a minimum of 12–16 weeks post repair.22–23 The normal tendon to bone transition including unmineralized and mineralized fibrocartilage is not recreated during the remodeling phase.22,24–25 Rather, repairing the rotator cuff to its anatomic location facilitates the formation of scar tissue in a manner that secures the torn tendon to the greater tuberosity in a more anatomic location. This, in turn, allows the rotator cuff to function at an anatomic length and tension, which is important if normal function is to be restored.
SCIENTIFIC RATIONALE BEHIND POSTOPERATIVE TREATMENT MODALITIES
Allowing healing of the repaired rotator cuff tendon while minimizing stiffness and muscle atrophy are the primary goals of postsurgical rehabilitation. Unfortunately, there is a paucity of high-level evidence in the literature to support or develop various postoperative rehabilitation protocols.26 Millett et al27 previously reported a widely used protective rehabilitation protocol based on available scientific evidence. Koo and Burkhart28 similarly presented both protective and accelerated rehabilitation protocols utilized based on individual patient risk for developing postoperative stiffness. The protective protocol, in which muscle strengthening exercises are delayed, is applied after arthroscopic repair of rotator cuff tears greater than 5 cm or involving more than 2 tendons, poor tissue quality, or repairs with greater tension.28 Each of these protocols implement various treatment modalities at different times to maximize healing and minimize stiffness based on repair characteristics such as tissue quality and repair robustness. The following sections report on the available evidence behind these various postoperative treatment modalities. A review of currently available literature on rehabilitation after rotator cuff tear repair on PUBMED / MEDLINE and EMBASE databases was performed.
Immobilization
Postoperative stiffness is reportedly the most common complication occurring after surgical repair of the rotator cuff, regardless of an arthroscopic or open technique, and is likely to occur with prolonged immobilization.28–32 Animal models, however, indicate that postoperative immobilization can minimize the tension on rotator cuff repairs and may lead to improved collagen orientation and visco-elastic properties as compared to immediate postoperative exercise treatment.33–34
The optimal duration of immobilization following rotator cuff repair, therefore, continues to be controversial. Though some advocate early (passive) mobilization to reduce the rate of postoperative stiffness,29,35–36 a recent study suggests that longer immobilization periods, often recommended to protect surgical repairs, may not increase the incidence of post-operative stiffness.37 In addition, recent animal studies suggest that immobilization after rotator cuff repair of at least two weeks duration results in significantly less postoperative stiffness and increased active motion.38–39 The theory behind this assertion is that passive motion increases scar formation in the subacromial space resulting in decreased range of motion and increased stiffness.39
The arm position during immobilization is also of importance during the early healing phase of the tendon repair. The use of an abduction immobilizer is currently widely used because of evidence suggesting that vascularization is improved and tension on the repaired tendon(s) is minimized in this position.40 Therefore, immobilization of the shoulder for 4–6 weeks in a slightly abducted position may minimize tension and maximize vascularization of the repair. The patient may come out of the immobilizer for supervised passive motion exercises in phase I of the rehabilitation, approximately week 1–4 postoperatively, and active assisted range of motion when commencing to phase II, usually week 4–6 postoperatively.
Continuous Passive Motion (CPM)
Continuous passive motion has been shown to minimize postoperative pain while maintaining range of motion following articular cartilage treatments and joint arthroplasty of the knee.41–42 The potential benefit after shoulder surgery, however, is less clear. Researchers performing several prospective controlled trials reported no significant difference in clinical outcome of a group of patients treated with CPM during the first 3–4 weeks following rotator cuff repair compared to a control group treated without CPM.35–36 Additionally, Dockery et al found no difference in activity of rotator cuff muscles between mechanical CPM and manually-assisted CPM in an electromyographic study. Higher muscle activity was noted during patient self-assisted range of motion exercises as compared to mechanical CPM.43 To this end, CPM may be used to help maintain motion gains after glenohumeral manipulation while minimizing muscle activity; however its long term benefit is unclear and is otherwise not routinely prescribed.
Cryotherapy
Cryotherapy is used post-surgically to decrease pain, swelling, muscle spasm, and minimize the inflammatory response. Speer et al44 examined the use of cryotherapy in a prospective, randomized, controlled clinical trial that showed decreased pain and narcotic medication requirement during the first 24 postoperative hours. In addition, these patients had fewer pain complaints with therapy 10 days postoperatively and were better able to tolerate their rehabilitation. Others confirm these findings and report increased comfort and improved ability to sleep.45–46 Some evidence suggests that the use of pneumatic compression in conjunction with cryotherapy may enhance the effectiveness of both modalities.47 It is important to note, however, that high-quality, well-controlled studies examining the use of cryotherapy in conjunction with pneumatic compression do not exist. Based on this evidence the authors recommend the use of a home cryotherapy device for 10–14 days after surgery.
Joint mobilization
Joint mobilization techniques can be used to address joint stiffness and passive range of motion (PROM) deficits. Muraki et al demonstrated that glenohumeral distraction as well as anterior and posterior translational glides do not significantly alter stress on repaired supraspinatus tendons with the arm in resting position (30 degrees abduction in the scapular plane).48 In particular, posterior translational glides have shown to significantly increase external rotation range of motion in patients with stiff shoulders. These mobilizations are performed after positioning the extremity in the maximum available abduction and external rotation.49 The glides can be included in the early stages of rehabilitation at lower grades to assist in decreasing pain and guarding. Once the patient has progressed to 4–6 weeks after surgery, the mobilizations can be progressed to higher grades with the extremity positioned into maximum available abduction and external rotation.
Joint exercises and healing phases
Rehabilitation protocols are frequently divided into four phases; progressing from a maximum protection phase to a minimum protection phase. Within each phase, the patient experiences a gradual rotator cuff loading progression. Within each phase, the patient experiences a gradual rotator cuff loading progression based on studies detailing electromyography (EMG) activation of the rotator cuff during specific activities.
Activities resulting in minimal EMG activity begin in earlier phases when repair integrity and avoidance of stresses to the repair which could induce gapping is critical, whereas strengthening exercises that create higher EMG activity begin in later phases.50–53 By following this gradual progression of increasing EMG activity the authors facilitate protection of repair during the inflammation and proliferative phase when repaired tissue is immature and collagen reorganization in later phases once a threshold of stability is achieved. Pain, passive and active range of motion (ROM), and strength goals must be achieved within the present phase prior to initiating subsequent rehabilitation phases.
Some debate exists regarding early mobilization versus immobilization following arthroscopic rotator cuff repair. Denard et al performed a systematic review of articles related to postoperative stiffness following arthroscopic rotator cuff repair. They found stiffness to be more common in patients who were immobilized when compared to patients treated with an immediate passive range-of-motion protocol or a modified protocol that included early closed chain passive overhead stretching for patients who were in the at-risk group for postoperative stiffness.54 However, the authors suggest there may be a positive relationship between stiffness and rotator cuff healing with stiffness being considered a complication and recurrent rotator cuff tear a failure. Therefore the authors recommend a period of immobilization to encourage rotator cuff healing with modifications of rehabilitation protocols based on risk factors for post-operative stiffness that include: (1) small tear size; (2) worker's compensation; (3) age <50; (4) calcific tendinitis; (5) adhesive capsulitis and, finally, (6) concomitant labral repair.
The following protocol incorporates gentle, partner-assisted, oscillatory passive range of motion to gradually increase patient range of motion while minimizing pain and stress to the repair. By avoiding any stretching into the end ranges of motion the authors believe that it is possible to avoid stressing the repair and limit any un-necessary increase in the inflammatory response. The patient is advanced to the next phase once the patient has achieved passive and active range of motion goals in addition to meeting the established time lines required for progression to next phase of rehabilitation.
PROPOSAL OF AN EVIDENCE-BASED APPROACH TO ROTATOR CUFF REHABILITATION
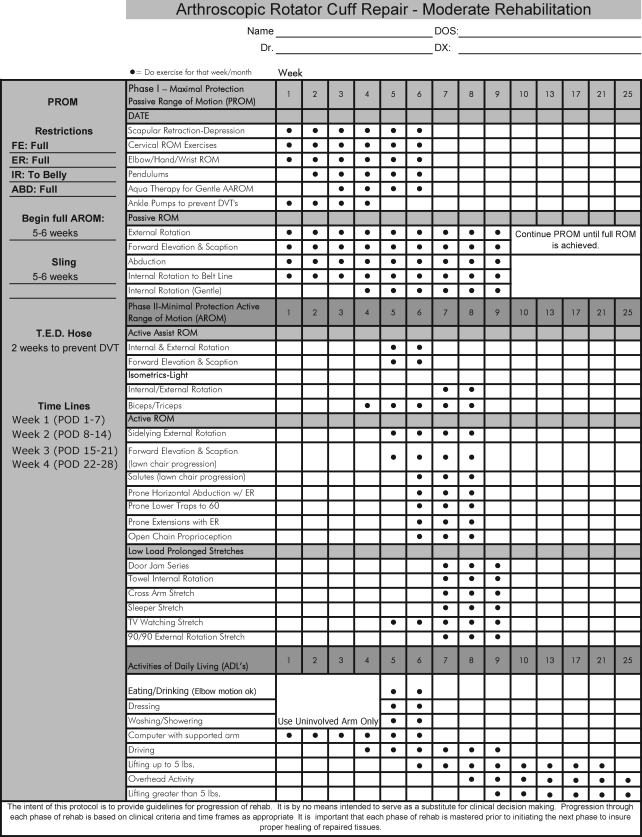
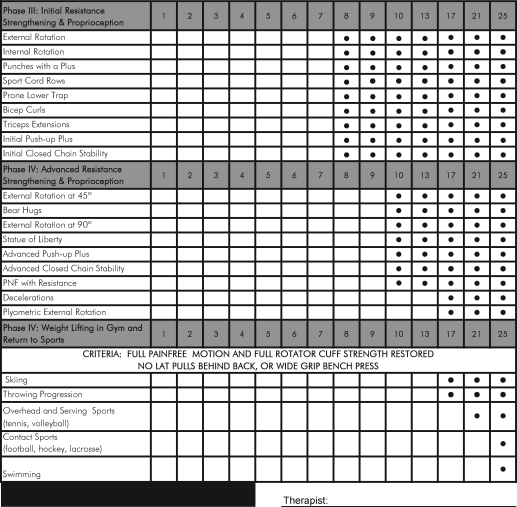
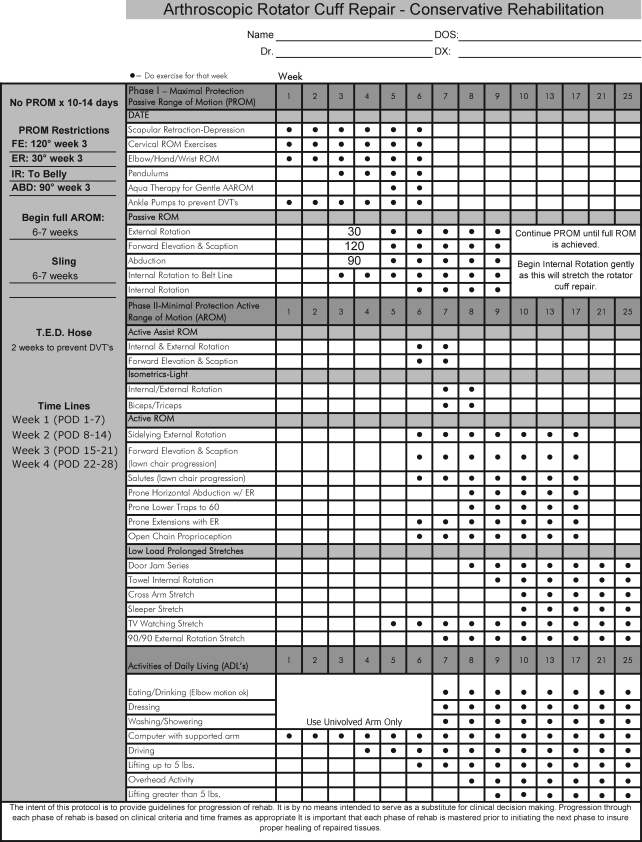
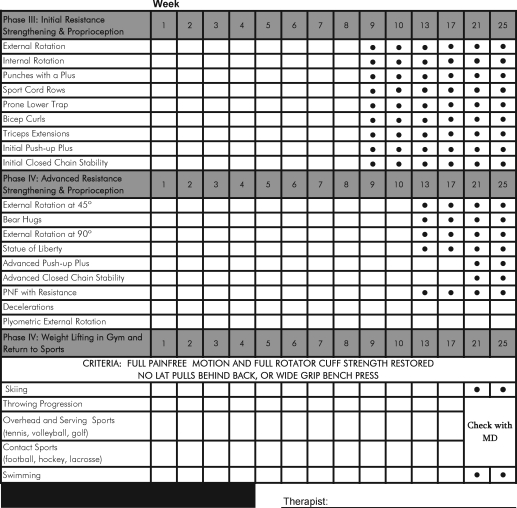
Postoperative rehabilitation following RC repair begins with close communication between the surgeon, his or her medical staff, and the physical therapy team. A review of surgical findings, such as the size of the tear, which tendons are involved, tissue quality, repair method, and concomitant procedures performed, is mandatory to establish rehabilitation guidelines. This communication continues throughout the recovery process and is an essential component in ensuring a successful outcome. Once the post-operative restrictions have been established, either a moderate (Appendix A) or conservative (Appendix B) rehabilitation protocol is selected and customized based on patient age, tear size, tissue quality, security of repair and additional procedures performed. Geriatric patients with large tears or poor tissue quality often require a conservative protocol, while younger patients with good tissue quality or a small tear would be appropriate for a moderate approach. Ultimately, the surgeon must communicate important findings so the course of treatment is appropriate for the patient.
The conservative protocol is characterized by either a delay in the initiation of and/or restriction of passive range of motion (PROM). It is common for PROM restrictions to last for 2–4 weeks. The aim is to minimize stress placed on the repaired tissues to facilitate early tissue healing. The moderate protocol is characterized by initiating PROM on postoperative day 1 while maintaining tolerable pain levels.
A home exercise program (HEP) should be incorporated into each phase of rehabilitation taking into account the post-operative restrictions that may apply. Initial HEP may include cervical, elbow, wrist, and hand AROM. A HEP should be provided regularly and individualized to address the observed impairments during periodic assessments throughout the phases.
Phase I
Regardless of the determined protocol, protection of the repaired tissue should be the focus of the initial phase of post-operative rotator cuff rehabilitation. However, there should be equilibrium between the promotion of tendon healing and preventing the development of postoperative adhesions. As previously mentioned, solid communication between surgeon and rehabilitation provider is mandatory. Depending on the integrity or location of the repair, certain passive motions (e.g. internal and external rotation, flexion, and abduction) may be restricted to protect sensitive repairs.
Directly following the repair the integrity of the repair relies mainly on the suture construct. Soon afterwards, collagen deposition and growth factors increase, with a peak increase around 10 days after surgery and a plateau phase is reached 28–56 days after the repair.22,25 The newly formed collagen network at this point still requires gentle stresses to positively affect fiber orientation however, the repair should not be exposed to the excessive forces imposed by active motion.
Within both the conservative and moderate treatment guidelines, passive range of motion of the glenohumeral joint begins as soon as it is deemed safe to minimize potential joint stiffness.29 Gentle joint oscillations in short-arm traction can be a useful technique to reduce muscle guarding and pain (Figure 1 A–D). PROM is progressed with caution, understanding that therapist-assisted passive motion (Figure 2) may be safer than other more active techniques due to the inherent increase in muscle activation present with other more active activities (i.e. use of pullies).43,55 Passive motion continues until symmetrical and pain free motion is achieved compared to the contralateral shoulder. In cases where the contralateral shoulder is symptomatic, PROM is continued until pain free motion is achieved that falls within established norms.56,57
Figure 1 A–D.
Gentle joint oscillations in short-arm traction and various degrees of rotation with the arm in slight abduction.
Figure 2.
Therapist-assisted passive range of motion exercise of forward flexion.
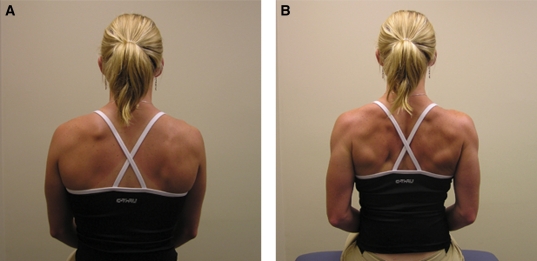
When the shoulder is at rest, a neutral rotation sling is used throughout the first phase of rehabilitation. It is prudent during this phase to introduce prophylactic active motion of the elbow, wrist, hand, and cervical spine as well as postural education. Acute periscapular activation in the form of isolated scapular depression, protraction performed from a neutral position and back to neutral after each repetition, are appropriate and has shown to exhibit minimal posterior RC cuff activity (Figure 3 A–B).58 Scapular clock exercises and scapular retraction should be prescribed with discretion as these have been shown to increase EMG activity of the supraspinatus muscle to unsafe levels.58 Pendulum exercises can also be performed if done with small concentric circles of approximately 20 cm in diameter. This generates less than 15% of maximum voluntary isometric contraction activity in the supraspinatus and infraspinatus muscles.59
Figure 3 A–B.
Isolated scapular depression and protraction.
The criteria to progress from phase I to phase II include: (1) passive forward flexion to at least 125 degrees; (2) passive external rotation in scapular plane to at least 75 degrees; (3) passive internal rotation in scapular plane to at least 75 degrees; (4) passive glenohumeral abduction to at least 90 degrees in the scapular plane.
Phase II
Phase two begins when the patient is cleared by the surgical team to begin active assisted range of motion (AAROM) followed by active range of motion (AROM). Rehabilitation criteria should include adequate PROM for advancement, minimal substitution patterns with PROM exercises (i.e. shoulder hiking with elevation) and minimal pain with PROM.
This phase typically commences 4–8 weeks after surgery, but may be delayed, depending on the age of the patient60, comorbidities,61 and quality and size of the repair.62,63 From a histological perspective, the inflammatory and repair phases should have passed, and the healing progressed to the remodeling phase. The application of low level forces during this timeframe aids in orienting the fibers within the collagen matrix and enhancing the tensile strength of the repair.22–23
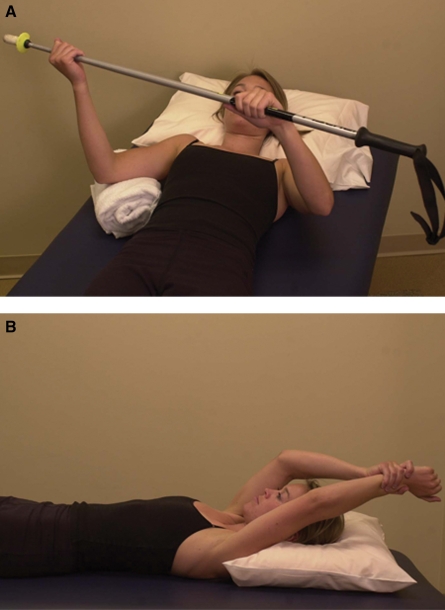
The authors suggest the use of AAROM during this timeframe, including supine glenohumeral external and internal rotation with a cane as well as supine flexion with the assistance of the uninvolved limb (Figure 4 A–B). An alternative AAROM technique is having the patient perform circles on a physioball placed on a table as the patient stands facing the ball with his hand and forearm resting on the ball. The authors believe this technique to incorporate most cardinal plane motions in one exercise. With the extremity supported on the ball, rotator cuff activity is likely diminished.
Figure 4 A–B.
Active-assisted range of motion exercises of internal rotation with the aid of a cane (A) and forward flexion with the help of the uninvolved limb (B).
At this time, slow AROM exercises performed while submerged in neck deep water can also be a viable adjunct to land-based rehabilitation to improve glenohumeral joint range of motion.64 Active forward elevation performed in the scapular plane in a pool at 30° per second has shown to have less rotator cuff EMG activity, in terms of percent of maximal voluntary isometric contraction65, than various land-based AAROM exercises performed in the same plane.66 This offers patients a supported and safe environment to perform various active motions that will not place healing tissue in jeopardy.
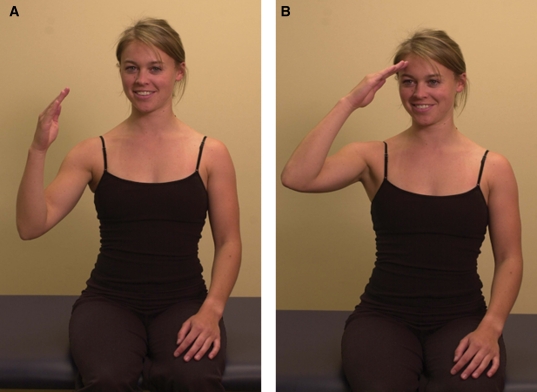
Establishing proper neuromuscular control of the musculature of the shoulder girdle is essential to regaining full function following a rotator cuff repair. There is inherent risk in the post-operative shoulder for development of impaired scapulothoracic kinematics. If normal scapulothoracic kinematics are not restored, impingement syndrome may re-emerge.52,67 Muscle force production and timing of contractions must be considered. The authors suggest using the prone position to help initiate proper muscle fiber activity patterns, particularly in the rhomboids and trapezius muscles. Scapular retraction/depression can help to deemphasize an often dominant upper trapezius muscle (Figure 5). The serratus anterior can be initially emphasized in the supine position with scapular protraction in 90 degrees of glenohumeral joint flexion, which is progressed to protraction at 120 degrees of flexion. Furthermore, the un-weighted bench press series serves as a good systematic progression to address active forward elevation and functional impairments; beginning in supine, then reclined and semi-reclined, and then upright sitting position as tolerated. Side lying external rotation, when performed properly, incorporates scapular stabilization with high infraspinatus and teres minor activity.53 Scapular plane elevation (scaption) with a flexed elbow, also known as “the salute exercise”, is an effective way to initiate recruitment of the supraspinatus muscle fibers (Figure 6 A–B). This exercise can be progressed to “the full can activity”, which is known to exhibit high supraspinatus muscle activity.52–53
Figure 5.
Stimulation of scapulothoracic musculature in the prone position.
Figure 6 A–B.
The ‘salute’ exercise. Beginning (A) and ending (B) positions.
In addition, sub-maximal isometric external and internal rotation exercises and open-chain proprioceptive activities can be initiated at this time. These activities will gradually restore muscle strength and proprioception thereby establishing muscular balance. The exercises are performed with the arm below shoulder height, elbow flexed to approximately 90 degrees, held in a neutral rotation position with a towel roll placed between the elbow and trunk. The patient is asked to generate a force into internal rotation or external rotation, resisting with their uninvolved upper extremity, starting at approximately 25% of maximal effort and gradually increasing to 50–75% of maximal effort without reproducing pain. Open chain proprioceptive exercises are performed with the patient lying supine with the involved shoulder held in 90° of forward elevation (Figure 7). The patient is then instructed to draw circles and the alphabet in the air utilizing small, controlled motions. Also during this phase, any PROM, AROM, or soft tissue flexibility limitations must continue to be addressed as needed. To progress from phase II to phase III, the patient must have full active range of motion as compared to the contralateral shoulder with no signs of scapular dyskinesia.
Figure 7.
Open chain proprioceptive exercise with the patient in supine position and the involved upper extremity held in 90° of forward elevation.
Phase III
Phase three is characterized by initial rotator cuff strengthening. This phase may begin when the patient demonstrates adequate passive and active glenohumeral range of motion, absent of substitution patterns, with acceptable scapulothoracic kinematics. The initiation of this phase is dependent on factors mentioned previously, such as tear size, tissue quality, and timing restrictions presented by the surgeon, as well as the clinical discretion of the therapist. Typically, this phase may begin between 8–12 weeks after surgery. At this point, tendon-to-bone healing should be able to endure the initiation of strengthening exercises. PROM and AROM exercises are continued if necessary, based upon therapist discretion.
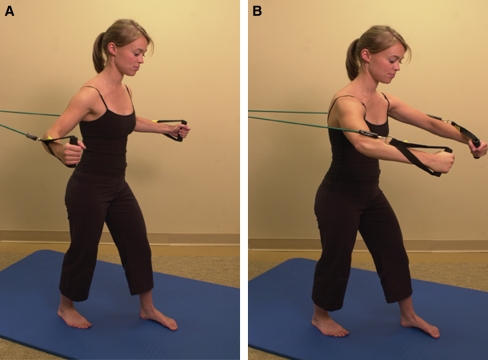
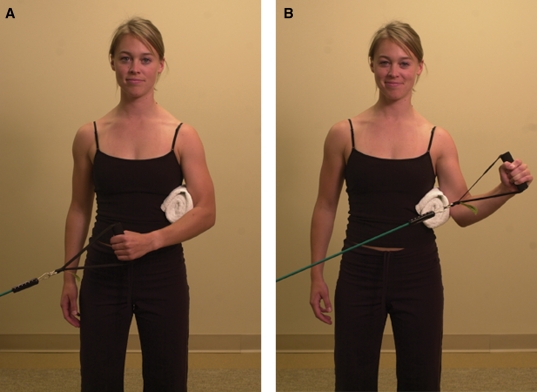
During this phase, the patient progresses to isotonic and light closed chain stability exercises. The shoulder external and internal rotators are strengthened by performing said motions with the arm below shoulder height utilizing elastic resistance and with a towel roll placed between the arm and trunk to encourage proper technique, thereby minimizing substitution patterns. To initiate strengthening of the serratus anterior muscle, a bear hug exercise using elastic resistance is performed similar to the dynamic hug test described by Decker et al.50 The bear hug exercise is performed while standing with the back toward the wall, knees slightly bent, and the feet shoulder-width apart. The elbows are flexed to 45°, the arms are abducted 60° out from the trunk, and the shoulder is internally rotated to 45°. The patient then performs horizontal adduction of both upper extremities, following an imaginary arc at approximately 60 degrees of elevation until they obtain maximum scapular protraction by touching their fists together as to mimic a hugging motion around a cylindrical object (Figure 8 A–B). The patient then slowly returns to the starting position as described above.
Figure 8 A–B.
‘Bear hug test’; horizontal adduction of both upper extremities in an axial plane, following an imaginary arc at approximately 60 degrees of elevation until maximum scapular protraction is obtained by touching fists together (B).
The standing sport cord row exercise is used to strengthen the trapezius and rhomboid musculature (Figure 9), both important scapular stabilizers, in a fashion similar to the prone rowing type exercise that has been reported to elicit high levels of trapezius and rhomboid muscle activity in EMG studies.51,68 The prone lower trapezius exercise is similar to the prone full can exercise described by Ekstrom et al and was shown to elicit the greatest amount of EMG activity in the lower trapezius muscle.51
Figure 9.
The standing sport cord row exercise in order to strengthen the trapezius and rhomboid musculature.
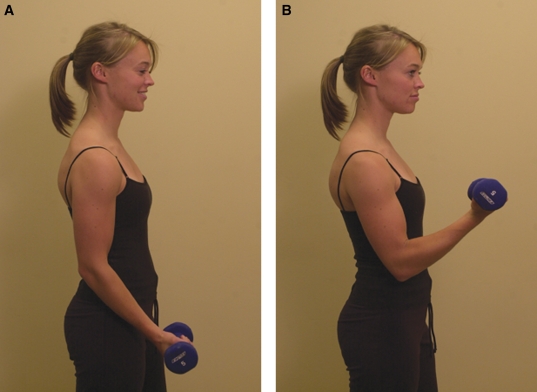
To address the biceps and triceps brachii muscles, conventional biceps curl and triceps extension exercises are used with either isotonic free weight resistance or elastic tubing (Figures 10 A–B and 11 A–B). Besides its role in forward flexion of the glenohumeral joint, the contribution of the long head of the biceps tendon to the stability of the glenohumeral joint (due to its' intra-articular insertion) is unclear and the results of in vitro studies and recent in vivo studies contradict.69,70 The triceps brachii acts as both a shoulder and elbow extensor and is active in closed-chain isotonic exercises like a chest press or in closed-chain stability exercises that are performed in the plank or quadraped positions.71
Figure 10 A–B.
Conventional biceps curl exercises with free weight resistance.
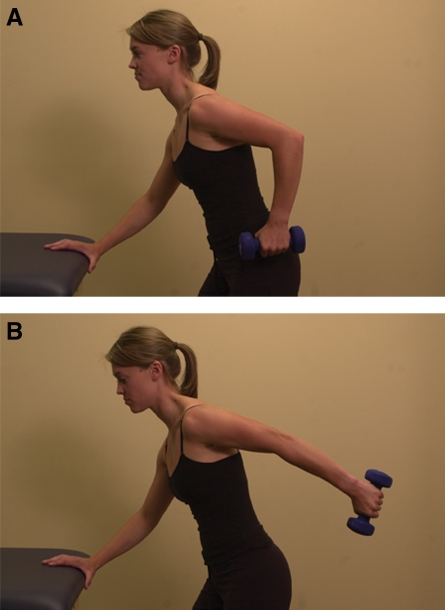
Figure 11 A–B.
Triceps extension exercises with free weight resistance.
Initial closed chain stability exercises are started to improve neuromuscular control of the shoulder complex. Rhythmic stabilization in the quadruped position utilizing weight shifts and perturbations can be utilized to improve static control through compressive forces acting through the glenohumeral joint, which increase muscle activation and improve static stability of the shoulder complex.72 Once the patient is pain-free with activities of daily living and demonstrates ability to tolerate all phase III strengthening exercises without pain they can be progressed to phase IV.
Phase IV
The advanced strengthening phase can typically be initiated approximately 12–16 weeks following rotator cuff repair. At this point, the remodeling phase is close to completion and the repaired rotator cuff tissue is relatively mature, therefore able to withstand greater stresses as compared with stresses encountered in earlier phases. The patient should be pain-free with activities of daily living and demonstrate the ability to tolerate all phase III strengthening exercises without pain or substitution. In addition, the patient should be able to perform active motions at multiple angles without signs of scapular dyskinesia. This phase is a progression of the previous phase and a transition to sport-specific rehabilitation activities and endurance of maximum tensile strength.22–23
Progressive strengthening of the posterior cuff muscles is accomplished in a standing position while performing external rotation of the shoulder at 45 degrees of abduction utilizing elastic resistance (Figure 12 A– B). This ensures high levels of infraspinatus and teres minor activation. By performing external rotation exercises at 90 degrees of abduction, supraspinatus muscle activity is optimally generated.67,73
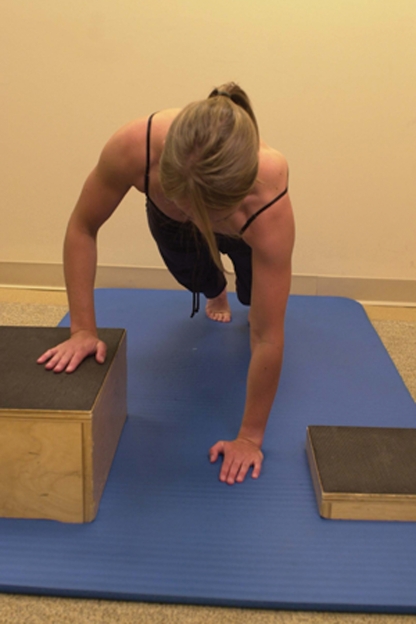
Figure 12 A–B.
Strengthening of the posterior rotator cuff by performing external rotation against elastic resistance with the arm in 45° of abduction.
The scapulothoracic articulation is also addressed using several exercises chosen to specifically target the scapular stabilizers. To further strengthen the serratus anterior muscle, a punch with a plus exercise utilizing elastic resistance is performed. This exercise combines the bench press and the supine scapular protraction exercises used for AROM in phase II that have shown to elicit high EMG activity of the serratus anterior muscle. This exercise is performed standing, facing away from the elastic resistance attachment with the hands held at shoulder width and chest height, holding onto the resistance band or cord. The upper extremities are then extended forward away from the body similar to a bench press motion at approximately 120 degrees of forward elevation followed by protraction of the scapula.50–51 Additionally, the push-up with a plus progression is a more advanced exercise that strengthens the serratus anterior muscle (Figure 13).50 It gradually increases gravity resistance and begins with pressing against a wall, progressing to the edge of a table, and finally to the floor.
Figure 13.
The push-up plus progression exercise.
Advanced rhythmic stabilization training is instituted having the patient stabilize their upper extremity in a position of 90° of external rotation and 90° of forward elevation in the scapular plane (“statue of liberty position”). Once in this position the patient is challenged to maintain this position against elastic resistance while performing rapid oscillations with a rubber bar (Figure 14). This exercise can be modified by rotating around the patient, altering the direction of pull, as they perform the exercise. Additionally, advanced closed chain stability exercises are performed in the quadruped position while stepping on and off steps of various heights and angles. Manual resisted proprioceptive neuromuscular facilitation through diagonal resistance exercises can be implemented at this time to continue the progression of rhythmic stabilization with the added benefit of the physical therapist being able to apply varying amounts of resistance in multiple planes of movement.
Figure 14.
The ‘Statue of Liberty’ exercise.
Finally, plyometrics for the upper extremity may be initiated towards the end of this phase to train the shoulder and upper extremity musculature to dissipate forces similar to what would be encountered once the patient returns to sport. Typically the patient will start by performing bilateral throws and progress to unilateral throws against a wall, rebounder, or by involving a partner using progressively heavier weighted balls. These exercises should start at positions at or near shoulder height progressing to the overhead position (Figure 15 A–B). Due to the aggressive nature of these exercises, collaborating with the orthopedic team to evaluate the appropriateness of these exercises is necessary. The patient's age, the sport he or she is returning to, and the integrity and size of the cuff repair should all be carefully considered before implementing these exercises into a plan of care.
Figure 15 A–B.
Throwing exercises against a rebounder starting at or near shoulder height (A) progressing to the overhead position (B).
Return to sport
A gradual, progressive return to sport rehabilitation plan is initiated after completing phase IV and prior to returning to competitive sporting activities. The interval sports program should begin only after the patient has been cleared by the surgeon and has achieved symmetric motion and strength, normalized scapulothoracic kinematics, and has no complaints of pain at rest or with activities.
Sports specific training exercises should only be commenced when the patient is fully rested and after a 5–10 minute cardiovascular warm-up. The program should be performed three times per week with at least one rest day in-between sessions. To advance to the next level the patient must be able to complete the prior level without pain or limitations. A maintenance exercise program focusing on cardiovascular endurance and flexibility along with scapulothoracic, rotator cuff, lower extremity, and core strength should be performed on alternate days.
An interval golf program is an example of a return to sport program that should be completed prior to returning to full, unrestricted golf play. The program is initiated with putting and chipping and gradually works through short, medium, and long distance irons and woods. Once the patient is able to work through all clubs and equal the approximate number of strokes expected in 9-holes of golf without pain or soreness, then they can play 9-holes of golf on a course. If they can successfully complete 3 rounds of 9-holes without pain or soreness they may then progress to playing 18-holes.74
An interval tennis program is another example of a return to sport program that should be utilized prior to returning to full, unrestricted tennis play. The program for tennis players progresses from limited number of forehand and backhand ground strokes progressing to overhead serves and culminating in a return to competitive matches occurring over a 4 week period.75
CONCLUSIONS
This review describes a rotator cuff rehabilitation protocol that incorporates currently available scientific literature guiding rehabilitation. To this end, expert experience remains a large facet of rehabilitation protocols.
Postoperative rehabilitation following RC repair begins with close communication between the surgeon, his or her medical staff, the patient, and the physical therapy team. A review of surgical findings is mandatory to establish rehabilitation guidelines. This communication continues throughout the recovery process and is an essential component in ensuring a successful outcome. Once the post-operative restrictions have been established, either a conservative or moderate rehabilitation protocol is selected and customized based on surgical findings. The conservative protocol is characterized by either a delay in the initiation of and/or restriction of passive range of motion. It is common for restrictions to last for 2–4 weeks. The aim is to minimize stress placed on the repaired tissues to facilitate early tissue healing. The moderate protocol is characterized by initiating passive range of motion on postoperative day 1 while maintaining tolerable pain levels.
LIMITATIONS AND FUTURE RESEARCH
Rehabilitation protocols have traditionally varied considerably between providers with respect to timing of progression and appropriate therapeutic exercise. Rehabilitation protocols are frequently based on clinical experience and expert opinion rather than scientific rationale. Future research could be focused on more detailed timing and quality of progression through rehabilitation.
APPENDIX A. Moderate rehabilitation protocol following arthroscopic rotator cuff repair.
APPENDIX B. Conservative rehabilitation protocol following arthroscopic rotator cuff repair.
References
- 1.Lin J.C., Weintraub N., Aragaki D.R. Nonsurgical treatment for rotator cuff injury in the elderly. J Am Med Dir Assoc. 2008. 9(9): p. 626–32 10.1016/j.jamda.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Boykin R.E., Heuer H.J., Vaishnav S., Millett P.J. Rotator Cuff Disease: Basics of diagnosis and treatment. Rheumatology Reports. 2010(2:e1): p. 1–12 [Google Scholar]
- 3.Bennett W.F. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003. 19(4): p. 380–90 10.1053/jars.2003.50131 [DOI] [PubMed] [Google Scholar]
- 4.Brox J.I., Gjengedal E., Uppheim G., et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg. 1999. 8(2): p. 102–11 [DOI] [PubMed] [Google Scholar]
- 5.Budoff J.E., Nirschl R.P., Guidi E.J. Debridement of partial-thickness tears of the rotator cuff without acromioplasty. Long-term follow-up and review of the literature. J Bone Joint Surg Am. 1998. 80(5): p. 733–48 [DOI] [PubMed] [Google Scholar]
- 6.Cofield R.H., Parvizi J., Hoffmeyer P.J., et al. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. 2001. 83-A(1): p. 71–7 [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie-Harris D.J., Wiley A.M. Arthroscopic surgery of the shoulder. A general appraisal. J Bone Joint Surg Br. 1986. 68(2): p. 201–7 [DOI] [PubMed] [Google Scholar]
- 8.Park J.Y., Yoo M.J., Kim M.H. Comparison of surgical outcome between bursal and articular partial thickness rotator cuff tears. Orthopedics. 2003. 26(4): p. 387–90; discussion 390 [DOI] [PubMed] [Google Scholar]
- 9.Snyder S.J., Pachelli A.F., Del Pizzo W., et al. Partial thickness rotator cuff tears: results of arthroscopic treatment. Arthroscopy. 1991. 7(1): p. 1–7 [DOI] [PubMed] [Google Scholar]
- 10.Noyes F.R., DeMaio M., Mangine R.E. Evaluation-based protocols: a new approach to rehabilitation. Orthopedics. 1991. 14(12): p. 1383–5 [DOI] [PubMed] [Google Scholar]
- 11.Clark J.M., Harryman D. T., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992. 74(5): p. 713–25 [PubMed] [Google Scholar]
- 12.Dugas J.R., Campbell D.A., Warren R.F., et al. Anatomy and dimensions of rotator cuff insertions. J Shoulder Elbow Surg. 2002. 11(5): p. 498–503 [DOI] [PubMed] [Google Scholar]
- 13.Mochizuki T., Sugaya H., Uomizu M., et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008. 90(5): p. 962–9 10.2106/JBJS.G.00427 [DOI] [PubMed] [Google Scholar]
- 14.Ruotolo C., Fow J.E., Nottage W.M. The supraspinatus footprint: an anatomic study of the supraspinatus insertion. Arthroscopy. 2004. 20(3): p. 246–910.1016/j.arthro.2004.01.002 [DOI] [PubMed] [Google Scholar]
- 15.Halder A.M., Zhao K.D., Odriscoll S.W., et al. Dynamic contributions to superior shoulder stability. J Orthop Res. 2001. 19(2): p. 206–12 10.1016/S0736-0266(00)00028-0 [DOI] [PubMed] [Google Scholar]
- 16.Reilly P., Amis A.A., Wallace A.L., et al. Supraspinatus tears: propagation and strain alteration. J Shoulder Elbow Surg. 2003. 12(2): p. 134–8 10.1067/mse.2003.7 [DOI] [PubMed] [Google Scholar]
- 17.Kibler W.B., Ludewig P.M., McClure P., et al. Scapular Summit 2009: introduction. July 16, 2009, Lexington, Kentucky. J Orthop Sports Phys Ther. 2009. 39(11): p. A1–A13 10.2519/jospt.2009.0303 [DOI] [PubMed] [Google Scholar]
- 18.Kibler W.B., McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003. 11(2): p. 142–51 [DOI] [PubMed] [Google Scholar]
- 19.Ide K., Shirai Y., Ito H. Sensory nerve supply in the human subacromial bursa. J Shoulder Elbow Surg. 1996. 5(5): p. 371–82 [DOI] [PubMed] [Google Scholar]
- 20.Yamanaka K., Matsumoto T. The joint side tear of the rotator cuff. A followup study by arthrography. Clin Orthop Relat Res. 1994(304): p. 68–73 [PubMed] [Google Scholar]
- 21.Gulotta L.V., Rodeo S.A. Growth factors for rotator cuff repair. Clin Sports Med. 2009. 28(1): p. 13–23 10.1016/j.csm.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 22.Carpenter J.E., Thomopoulos S., Flanagan C.L., et al. Rotator cuff defect healing: a biomechanical and histologic analysis in an animal model. J Shoulder Elbow Surg. 1998. 7(6): p. 599–605 [DOI] [PubMed] [Google Scholar]
- 23.Lewis C.W., Schlegel T.F., Hawkins R.J., et al. The effect of immobilization on rotator cuff healing using modified Mason-Allen stitches: a biomechanical study in sheep. Biomed Sci Instrum. 2001. 37: p. 263–8 [PubMed] [Google Scholar]
- 24.Cohen D.B., Kawamura S., Ehteshami J.R., et al. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006. 34(3): p. 362–9 10.1177/0363546505280428 [DOI] [PubMed] [Google Scholar]
- 25.Galatz L.M., Sandell L.J., Rothermich S.Y., et al. Characteristics of the rat supraspinatus tendon during tendon-to-bone healing after acute injury. J Orthop Res. 2006. 24(3): p. 541–50 10.1002/jor.20067 [DOI] [PubMed] [Google Scholar]
- 26.Baumgarten K.M., Vidal A.F., Wright R.W. Rotator Cuff Repair Rehabilitation: A level I and II Systematic Review. Sports Health: A Multidisciplinary Approach. 2009. 1: p. 125 10.1177/1941738108331200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Millett P.J., Wilcox R.B., 3rd, O'Holleran J.D., et al. Rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg. 2006. 14(11): p. 599–609 [DOI] [PubMed] [Google Scholar]
- 28.Koo S.S., Burkhart S.S. Rehabilitation following arthroscopic rotator cuff repair. Clin Sports Med. 2010. 29(2): p. 203–11, vii 10.1016/j.csm.2009.12.001 [DOI] [PubMed] [Google Scholar]
- 29.Brislin K.J., Field L.D., Savoie F.H., 3rd Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007. 23(2): p. 124–8 10.1016/j.arthro.2006.09.001 [DOI] [PubMed] [Google Scholar]
- 30.Severud E.L., Ruotolo C., Abbott D.D., et al. All-arthroscopic versus mini-open rotator cuff repair: A long-term retrospective outcome comparison. Arthroscopy. 2003. 19(3): p. 234–8 10.1053/jars.2003.50036 [DOI] [PubMed] [Google Scholar]
- 31.Tauro J.C. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006. 22(6): p. 581–6 10.1016/j.arthro.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 32.Warner J.J., Greis P.E. The treatment of stiffness of the shoulder after repair of the rotator cuff. Instr Course Lect. 1998. 47: p. 67–75 [PubMed] [Google Scholar]
- 33.Gerber C., Schneeberger A.G., Perren S.M., et al. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am. 1999. 81(9): p. 1281–90 [DOI] [PubMed] [Google Scholar]
- 34.Thomopoulos S., Williams G.R., Soslowsky L.J. Tendon to bone healing: differences in biomechanical, structural, and compositional properties due to a range of activity levels. J Biomech Eng. 2003. 125(1): p. 106–13 [DOI] [PubMed] [Google Scholar]
- 35.Lastayo P.C., Wright T., Jaffe R., et al. Continuous passive motion after repair of the rotator cuff. A prospective outcome study. J Bone Joint Surg Am. 1998. 80(7): p. 1002–11 [DOI] [PubMed] [Google Scholar]
- 36.Raab M.G., Rzeszutko D., O'Connor W., et al. Early results of continuous passive motion after rotator cuff repair: a prospective, randomized, blinded, controlled study. Am J Orthop. 1996. 25(3): p. 214–20 [PubMed] [Google Scholar]
- 37.Parsons B.O., Gruson K.I., Chen D.D., et al. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg. 2010. 19(7): p. 1034–9 10.1016/j.jse.2010.04.006 [DOI] [PubMed] [Google Scholar]
- 38.Gimbel J.A., Van Kleunen J.P., Williams G.R., et al. Long durations of immobilization in the rat result in enhanced mechanical properties of the healing supraspinatus tendon insertion site. J Biomech Eng. 2007. 129(3): p. 400–4 10.1115/1.2721075 [DOI] [PubMed] [Google Scholar]
- 39.Peltz C.D., Dourte L.M., Kuntz A.F., et al. The effect of postoperative passive motion on rotator cuff healing in a rat model. J Bone Joint Surg Am. 2009. 91(10): p. 2421–9 10.2106/JBJS.H.01121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rathbun J.B., Macnab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg Br. 1970. 52(3): p. 540–53 [PubMed] [Google Scholar]
- 41.Coutts R.D., Kaita J.H., Barr R., et al. The role of continuous passive motion in the rehabilitation of the total knee patient. Orthop Trans. 1982. 6: p. 277–8 [Google Scholar]
- 42.Salter R.B., Hamilton H.W., Wedge J.H., et al. Clinical application of basic research on continuous passive motion for disorders and injuries of synovial joints: a preliminary report of a feasibility study. J Orthop Res. 1984. 1(3): p. 325–42 10.1002/jor.1100010313 [DOI] [PubMed] [Google Scholar]
- 43.Dockery M.L., Wright T.W., LaStayo P.C. Electromyography of the shoulder: an analysis of passive modes of exercise. Orthopedics. 1998. 21(11): p. 1181–4 [DOI] [PubMed] [Google Scholar]
- 44.Speer K.P., Warren R.F., Horowitz L. The efficacy of cryotherapy in the postoperative shoulder. J Shoulder Elbow Surg. 1996. 5(1): p. 62–8 [DOI] [PubMed] [Google Scholar]
- 45.Osbahr D.C., Cawley P.W., Speer K.P. The effect of continuous cryotherapy on glenohumeral joint and subacromial space temperatures in the postoperative shoulder. Arthroscopy. 2002. 18(7): p. 748–54 [DOI] [PubMed] [Google Scholar]
- 46.Singh H., Osbahr D.C., Holovacs T.F., et al. The efficacy of continuous cryotherapy on the postoperative shoulder: a prospective, randomized investigation. J Shoulder Elbow Surg. 2001. 10(6): p. 522–5 10.1067/mse.2001.118415 [DOI] [PubMed] [Google Scholar]
- 47.Capps SG, M.B. Cryotherapy and Intermittent Pneumatic Compression for Soft Tissue Trauma. Human Kinetics. 2009. 14(1): p. 2–4 [Google Scholar]
- 48.Muraki T., Aoki M., Uchiyama E., et al. Strain on the repaired supraspinatus tendon during manual traction and translational glide mobilization on the glenohumeral joint: a cadaveric biomechanics study. Man Ther. 2007. 12(3): p. 231–9 10.1016/j.math.2006.06.017 [DOI] [PubMed] [Google Scholar]
- 49.Johnson A.J., Godges J.J., Zimmerman G.J., et al. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther. 2007. 37(3): p. 88–99 [DOI] [PubMed] [Google Scholar]
- 50.Decker M.J., Hintermeister R.A., Faber K.J., et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med. 1999. 27(6): p. 784–91 [DOI] [PubMed] [Google Scholar]
- 51.Ekstrom R.A., Donatelli R.A., Soderberg G.L. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003. 33(5): p. 247–58 [DOI] [PubMed] [Google Scholar]
- 52.Escamilla R.F., Yamashiro K., Paulos L., et al. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med. 2009. 39(8): p. 663–854 10.2165/00007256-200939080-00004 [DOI] [PubMed] [Google Scholar]
- 53.Reinold M.M., Wilk K.E., Fleisig G.S., et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004. 34(7): p. 385–94 [DOI] [PubMed] [Google Scholar]
- 54.Denard PJ, Ladermann A, Burkhart SS. Prevention and Management of Stiffness After Arthroscopic Rotator Cuff Repair: Systematic Review and Implications for Rotator Cuff Healing. Arthroscopy 27(6);2011, 842–848 [DOI] [PubMed] [Google Scholar]
- 55.Uhl T.L., Muir T.A., Lawson L. Electromyographical assessment of passive, active assistive, and active shoulder rehabilitation exercises. PM R. 2010. 2(2): p. 132–41 10.1016/j.pmrj.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 56.Gulotta LV, Nho SJ, Dodson CC, Adler AS, Altchek DW, MacGillivray JD; HSS Arthroscopic Rotator Cuff Registry. J Shoulder Elbow Surgery. 2011;20(6):941–6 [DOI] [PubMed] [Google Scholar]
- 57.Lee BG, Cho NS, Rhee YG. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercises. Arthroscopy. 2012;28(1):34–42 [DOI] [PubMed] [Google Scholar]
- 58.Smith J., Dahm D.L., Kaufman K.R., et al. Electromyographic activity in the immobilized shoulder girdle musculature during scapulothoracic exercises. Arch Phys Med Rehabil. 2006. 87(7): p. 923–7 10.1016/j.apmr.2006.03.013 [DOI] [PubMed] [Google Scholar]
- 59.Long J.L., Ruberte Thiele R.A., Skendzel J.G., et al. Activation of the shoulder musculature during pendulum exercises and light activities. J Orthop Sports Phys Ther. 2010. 40(4): p. 230–7 10.2519/jospt.2010.3095 [DOI] [PubMed] [Google Scholar]
- 60.Boileau P., Brassart N., Watkinson D.J., et al. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005. 87(6): p. 1229–40 10.2106/JBJS.D.02035 [DOI] [PubMed] [Google Scholar]
- 61.Boissonnault W.G., Badke M.B., Wooden M.J., et al. Patient outcome following rehabilitation for rotator cuff repair surgery: the impact of selected medical comorbidities. J Orthop Sports Phys Ther. 2007. 37(6): p. 312–9 [DOI] [PubMed] [Google Scholar]
- 62.Charousset C., Grimberg J., Duranthon L.D., et al. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008. 24(1): p. 25–33 10.1016/j.arthro.2007.07.023 [DOI] [PubMed] [Google Scholar]
- 63.Harryman D.T., 2nd, Mack L.A., Wang K.Y., et al. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991. 73(7): p. 982–9 [PubMed] [Google Scholar]
- 64.Brady B., Redfern J., MacDougal G., et al. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: a feasibility study. Physiother Res Int. 2008. 13(3): p. 153–61 10.1002/pri.403 [DOI] [PubMed] [Google Scholar]
- 65.Kelly BT, Roskin LA, Kirkendall DT, Speer KP. Shoulder muscle activation during aquatic and dry land exercises in nonimpaired subjects. J Orthop Sports Phys Ther. 2000;30(4):204–10 [DOI] [PubMed] [Google Scholar]
- 66.Uhl TL, Muir TA, Lawson L. Electromyographical assessment of passive, active assisted, and active shoulder rehabilitation exercises. PM&R. 2010;2(2):132–41 [DOI] [PubMed] [Google Scholar]
- 67.Reinold M.M., Escamilla R.F., Wilk K.E. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009. 39(2): p. 105–17 10.2519/jospt.2009.2835 [DOI] [PubMed] [Google Scholar]
- 68.Moseley J.B., Jr., Jobe F.W., Pink M., et al. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992. 20(2): p. 128–34 [DOI] [PubMed] [Google Scholar]
- 69.Giphart J.E., Elser F., Dewing C.B., Torry M.R., Millett P.J. The Long Head Biceps had minimal effect on in vivo Glenohumeral Kinematics: a biplane fluoroscopy study. Am J Sports Med. 2012. 40(1):202–12 Epub 2011 Sep 30. [DOI] [PubMed] [Google Scholar]
- 70.Elser F., Braun S., Dewing C.B., et al. Anatomy, function, injuries, and treatment of the long head of the biceps brachii tendon. Arthroscopy. 2011. 27(4): p. 581–92 10.1016/j.arthro.2010.10.014 [DOI] [PubMed] [Google Scholar]
- 71.Tucci H.T., Ciol M.A., Araa Jo R.C., et al. Muscle Activation of Selected Shoulder Muscles During Unilateral Wall Bench Press Tasks Under Submaximal Isometric Effort. J Orthop Sports Phys Ther. 2011. 10.2519/jospt.2011.3418 [DOI] [PubMed] [Google Scholar]
- 72.Uhl TL, Carver TJ, Mattacola SD, et al. Shoulder Musculature Activation During Upper Extremity Weight-Bearing Exercise. J Orthop Sports Phys Ther. 2003;33(3):109–117 [DOI] [PubMed] [Google Scholar]
- 73.Wilk K.E., Meister K., Andrews J.R. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002. 30(1): p. 136–51 [DOI] [PubMed] [Google Scholar]
- 74.Kim D.H., Millett P.J., Warner J.J., et al. Shoulder injuries in golf. Am J Sports Med. 2004. 32(5): p. 1324–30 10.1177/0363546504267346 [DOI] [PubMed] [Google Scholar]
- 75.Wilk KE, Andrews Jr RM. The Athlete's Shoulder. 2 ed. 2009, Philadelphia: Churchill Livingstone Elsevier [Google Scholar]