Abstract
Background and Purpose:
The ankle is the most commonly injured joint during athletic activity. While ankle sprains are certainly the most common injury, ankle fractures can occur frequently. One type of ankle fracture with a reportedly low incidence is the isolated posterior malleolar fracture. Because of the low incidence, isolated posterior malleolar fractures can present a diagnostic challenge. The purpose of this case report is to describe the diagnostic process used for this rare injury that occurred in a physically active college-aged female who injured her ankle when landing from a fall during performance on a military obstacle course.
Case Description:
A 19 year old female United States Military Academy cadet presented to a direct access physical therapy clinic. She was limping, not using any assistive device, and was wearing an ace bandage around her right ankle/foot. Two days earlier she fell from a “10 foot high” structure while performing the military obstacle course. She did not recall details of impact, but she was told by several bystanders that it appeared that she landed on her right foot followed immediately by a transition to her buttocks and then to her back.
Outcomes:
Ottawa Ankle Rules and ligamentous testing were negative; however, she was tender to palpation just anterior to the achilles tendon and lateral to the posterior edge of the medial malleolus. Based on mechanism of injury and tenderness of the posterior ankle, a potential posterior ankle fracture was suspected and subsequently confirmed by radiographic studies of the ankle including standard radiographs and computerized tomography.
Discussion:
While the Ottawa Ankle Rules are generally effective in detecting many types of ankle fractures, clinicians should not rely solely on such prediction rules. This case highlights the importance of completing a thorough history and performing a thorough physical examination. This case report focuses on differential diagnosis. It is important to consider all aspects of the patient evaluation process collectively instead of examination pieces individually.
Keywords: Direct access, Ottawa Ankle Rules, posterior malleolus fracture
INTRODUCTION
United States Military Cadets are a unique group of college-aged individuals who are required to perform high level athletic and physical activities on a regular basis. These activities often result in similar injuries as those sustained by high school and college athletes. Among these athletes, the ankle is the most commonly reported site of injury each year.1,2 Depending on the activity, a large amount of force can be imparted across the ankle joint, leading to fracture and/or ligament disruption.3,4 While sprains are certainly the most common injury to the ankle, ankle fractures are frequently seen in emergency rooms with an incidence of 1-2 per 1000 persons per year.5 With the increase of direct access in many health care facilities, it is paramount that clinicians recognize the need to obtain necessary radiographic images either via radiographic request or appropriate physician referral to correctly diagnose potential fractures of the ankle and ultimately provide proper care.
The Ottawa Ankle Rules (OAR) were developed to decrease cost of ordering extraneous radiographs while reducing the risk of missing fractures of the ankle or foot.6,7 The rules apply to any individual presenting to the emergency room or for medical care after a traumatic activity with tenderness to palpation of the posterior edge or tip of either malleoli (palpating 6 cm proximally) and/or inability to fully weight bear at least 4 steps.6,7 A modification called the Buffalo Ankle Rules found that tenderness to palpation of the mid body of the malleoli (palpating 6 cm proximally) was slightly more specific and equally sensitive.8 The OAR have demonstrated sensitivities of 95-100% for detecting medial and lateral malleolar fractures.6,7 Despite the success in facilitating the diagnosis of ankle fractures, the OAR have demonstrated mixed abilities with regard to ruling out certain ankle fractures such as isolated posterior malleolar fractures.6,7,9 Stiell et al7 found that in 17% of the cases in which the rules were interpreted as negative, the patients were diagnosed with a posterior malleolar fracture; however, less than 1% of the total injuries were diagnosed as posterior malleolar fractures.
Isolated posterior malleolar fractures can occur with high level activity but are rare entities. Lash et al10 found that only 4% of patients with confirmed ankle fractures over a year period had isolated posterior malleolar fractures. Neumaier et al10 performed a retrospective study of 2500 ankle lesions and found that only 25 were isolated posterior malleolar fractures. Posterior malleolar fractures usually occur in association with proximal fibular fractures (Maisonneuve), syndesmosis injuries, posterior tibiofibular ligament injury, and/or spiral tibial diaphyseal fractures. The posterior malleolus is defined as the posterior portion of the inferior articulating surface of the tibia. Volkmann's triangle and the posterior tibial plafond are other terms used to describe the posterior malleolus.
Lauge-Hansen devised a classification system for ankle injuries based on foot position and the force applied during the injury.11 A pronation-abduction injury was suggested as a mechanism for isolated posterior malleolar fractures.11 However, in an attempt to validate this classification system biomechanically utilizing cadaveric ankles, Michelson et al12 did not detect any posterior malleolar fractures after dissection of the cadaver specimen. The characteristic self-reported mechanism of injury for an isolated posterior malleolar fracture is hyper-plantar flexion with an axial load such as may occur with slipping and falling.6,7,10,13 Because of the low incidence, isolated posterior malleolar fractures can present a diagnostic challenge. The purpose of this case report is to describe the diagnostic process used for this rare injury that occurred in a physically active college-aged female who injured her ankle when landing from a fall during performance on a military obstacle course.
CASE DESCRIPTION
History/Subjective
A 19 year old female United States Military Academy cadet presented to a direct access physical therapy clinic wearing an ace bandage around her right ankle/foot and ambulating with a slightly antalgic weight-bearing gait without an assistive device. The cadet was participating in military field training located in a remote area. A physical therapist was present who provided musculoskeletal evaluations and applicable care for 2-3 hours daily to augment the remote primary medical care services. The subject's verbal pain rating was 0/10 at rest, 1-2/10 with ambulation on a level surface, and 5/10 with ambulation going downhill. She stated that two days earlier she fell from a “10 foot high” structure during performance on the military obstacle course. She did not recall what happened to her ankle at impact, but she was told by several bystanders that it appeared that she landed on her right foot followed immediately by landing on her buttocks and then her back. Onsite medical management included ice and an ace wrap for a sprained ankle. The patient was told that she could gradually increase activity as tolerated but to follow up if she did not notice remarkable improvement after a couple of days. While the ankle did improve gradually over the next two days, she was still having pain (mostly posterior and posterolateral) with ambulation especially when walking down hills, pivoting, and weight bearing on her right lower extremity. Past medical history revealed one previous right ankle sprain one year prior to this injury, which completely resolved. The subject was taking Ibuprofen 200 mg three times a day which seemed to decrease her pain. She denied numbness and tingling, significant night pain, weight change, feeling ill, or “giving way” of the ankle.
Physical Examination
The patient entered the clinic displaying a minimal to moderate antalgic gait with a lack of push off from midstance although she was able to plantar flex slightly at terminal stance. Visual inspection of the right ankle and foot revealed moderate edema and significant ecchymosis of the lateral and posterolateral leg/ankle (Figure 1). There was no tenderness or reported discomfort at the distal lateral and medial malleoli, despite palpable edema. There was no tenderness at the proximal fibula, base of the fifth metatarsal, navicular, or calcaneus. Active range of motion and passive range of motion was full with pain reported as 3 out of 10 at end range plantar flexion. Special tests including the fibular syndesmosis squeeze, external rotation test, and anterior drawer tests were negative with slight discomfort of the anterolateral ankle during each test, as reported by the subject. Ankle manual muscle testing was normal except for 4/5 with resisted plantar flexion with pain reported posteriorly. Because of the findings of the physical examination and the posterior ankle complaints when walking down hill, further palpation was performed which revealed tenderness just anterior to the Achilles tendon and lateral to the posterior edge of the medial malleolus that reproduced her symptoms.
Figure 1.
Subject's right ankle swelling and ecchymosis as visualized at initial examination.
Differential Diagnosis
Differential diagnoses considered at that time included posterior malleolar fracture, lateral malleolar avulsion fracture, or severe ankle sprain. Initially there was a low suspicion of fracture, because the typical application of Ottawa Ankle Rules were negative, as the patient could ambulate with low to moderate pain, no tenderness to palpation at the malleoli, and overall she was improving. Additionally, ligamentous testing was negative and pain free. Given the extent of edema and ecchymosis, a fall from a height approximately 10 feet, pain located posteriorly, and a possible forced ankle plantar flexion with axial load mechanism a posterior malleolar fracture became the leading suspected diagnosis. A concomitant Maisonneuve fracture was not suspected, because the patient was not tender at the proximal fibula and she did not report pain or crepitus with the fibular squeeze test.
In the military, physical therapists work closely with physicians and have the opportunity to be trained and credentialed with clinical privileges to order certain radiographic studies. The therapist in this case, having imaging privileges, ordered a three view (A/P, lateral and oblique views) ankle radiograph series for the right ankle due to the suspicion of posterior malleolar fracture. The patient was issued crutches and trained in non-weight bearing ambulation.
Outcome
Radiographs confirmed the presence of an isolated posterior malleolar fracture (Figure 2). An orthopedic surgeon was immediately consulted for further evaluation and treatment of a posterior tibial fracture. The surgeon ordered a Computed Tomography (CT), which confirmed a non-displaced isolated posterior malleolar fracture (Figure 3). The CT scan has been advocated as the modality of choice for assessment of stability and extent of posterior malleolar fractures.14–16 The patient was placed in a non-weight bearing short leg cast with use of bilateral axillary crutches for 6 weeks. Healing of the fracture was noted on radiographs taken 6 weeks later and at that time the patient was placed in a walking boot for 2 additional weeks.
Figure 2.
Radiographs of the subject's right ankle. Note the isolated, non-displaced fracture of the posterior malleolus on the lateral view (far right).
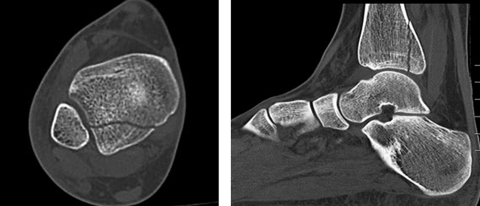
Figure 3.
Computerized Tomographic evaluation of the lower leg. Note the isolated, non-displaced fracture of the posterior malleolus. Left image= Sagittal view, Right image= Axial view.
Stationary biking, range of motion exercises, and theraband strengthening exercises were initiated once the cast was removed. Swimming, a variety of balance exercises, and gait training were added when the walking boot was removed. A walk to jog program was added within 2 weeks of boot removal and by 12 weeks the patient was running without difficulty. At that time, her ankle range of motion and strength were normal, balance appeared equal bilaterally, and hopping was painless and symmetrical when compared to the uninjured side. The patient was instructed to gradually increase all activity as tolerated and to follow-up as needed. The patient reported in an email follow-up 2 months later (20 weeks after initial evaluation) that she was completely back to full activity without limitations.
DISCUSSION
Diagnosing posterior malleolar fractures is typically more challenging than diagnosing other ankle fractures. Ankle fractures from trauma usually include the lateral malleolus, medial malleolus or a combination. The hallmark palpations for the OAR are inclined toward these common fracture sites.6,7 Because of the OAR's predisposition toward more common fractures, the proper diagnosis of isolated posterior malleolar via physical examination is difficult, and establishing the diagnosis via standard radiographs has shown to be more difficult than most other ankle fractures.6,7,14,17
This case highlights the importance of completing a thorough history and performing a thorough physical examination in order to formulate the most likely diagnosis after a unique injury such as the one sustained by the subject of this case. In this case, exact details of foot position at impact were not entirely clear. However, a common mechanism of injury for posterior malleolar fractures includes extreme plantar flexion of the foot combined with an axial load such as may occur with slipping or falling.17 Additionally, falls from a height of greater than 4 feet increase the risk for major injuries such as fractures in young active females.18 In this case the information from the history, along with physical examination findings of posterior and posteromedial ankle tenderness, the presence of significant edema and ecchymosis, and the functional limitations, made the therapist consider the differential diagnosis of an isolated posterior malleolar fracture.
If a posterior malleolar fracture is suspected, plain radiographs may be insufficient to rule out this fracture.14,17 The CT scan, therefore, has been advocated as the modality of choice to accurately assess for the presence of an isolated posterior malleolar fracture. When plain film radiography was compared to CT there was only a sensitivity of 63%.14 Haraguchi et al15 reviewed both plain film and CT imaging with posterior malleolar fractures and classified the fractures into three categories: Type I, a fracture through the posterior lateral portion of the tibia; Type II, a fracture through posterior lateral portion and into the medial malleolus; and Type III, one or more small shell fractures of the posterior lip. This classification was proposed because CT imaging allowed better visualization of the fracture, including the presence of small fragments.14,15,17 Association with posterior subluxation/dislocation of the talocrural joint was 30% for type I, 60% for type II and 11% for Type III fractures. In this case, the patient had a type I posterior malleolar fracture with less than 25% of the joint surface affected, with no talocrural subluxation (Figure 3) and was thus treated with cast stabilization.
While patients who have sustained isolated posterior malleolar fractures have responded well to non-surgical and surgical treatment, long-term subjective function has been shown to be less favorable when compared to outcomes following other fractures of the ankle.13,19 If the fracture encompasses greater than 25%-33% the joint surface then surgery is usually indicated.12,13,15,19–21 Fractures that involve greater than 25% of the joint surface tend to have slightly worse outcomes (ROM, pain and functional outcome measures).5 However, surgical fixation has allowed for earlier weight bearing when compared to conservative treatment. Early weight bearing has been shown to potentially improve outcomes with internal fixation of ankle fractures.20–23 In the presence of additional fractures or multiple fragments, fixation may be necessary for overall ankle stability.
This case report presents the process used for differential diagnosis of a sub-acute traumatic injury to the ankle of a female cadet. It is important to consider all aspects of the patient evaluation process collectively instead of using individual components of the examination in isolation. For example, concluding that this patient did not need imaging because the OAR was negative would have been a mistake. Instead, each part of the history and physical examination is a piece that needs to be grouped together to be considered collectively to develop a “clinical picture” in order to form a list of most likely diagnoses until a definitive diagnosis is achieved.
CONCLUSION
This case report illustrates the examination and clinical decision making process that led to the diagnosis of an isolated posterior malleolus fracture of the ankle, a fairly unique injury. While the findings of the OAR did not indicate that a fracture was likely, plain radiographs were obtained due to the combination of other examination findings (i.e., a fall from a considerable height, significant edema and ecchymosis, location of tenderness, and lack of pain with ligamentous testing). If a posterior malleolar fracture is suspected, visualization of a fracture may be evident on the lateral view of a radiograph, but a CT scan is of greater value for diagnosis of this fracture.
References
- 1.Nelson AJ, Collins CL, Yard EE, Fields SK, Comstock RD. Ankle injuries among United States high school sports athletes, 2005-2006. J Athl Train. Jul-Sep 2007;42(3):381–387 [PMC free article] [PubMed] [Google Scholar]
- 2.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. Oct 1998;19(10):653–660 [DOI] [PubMed] [Google Scholar]
- 3.Jelinek JA, Porter DA. Management of unstable ankle fractures and syndesmosis injuries in athletes. Foot Ankle Clin. Jun 2009;14(2):277–298 [DOI] [PubMed] [Google Scholar]
- 4.van den Bekerom MP, Haverkamp D, Kloen P. Biomechanical and clinical evaluation of posterior malleolar fractures. A systematic review of the literature. J Trauma. Jan 2009;66(1):279–284 [DOI] [PubMed] [Google Scholar]
- 5.De Vries JS, Wijgman AJ, Sierevelt IN, Schaap GR. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. May-Jun 2005;44(3):211–217 [DOI] [PubMed] [Google Scholar]
- 6.Lucchesi GM, Jackson RE, Peacock WF, Cerasani C, Swor RA. Sensitivity of the Ottawa rules. Ann Emerg Med. Jul 1995;26(1):1–5 [DOI] [PubMed] [Google Scholar]
- 7.Stiell I, Wells G, Laupacis A, et al. Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle injuries. Multicentre Ankle Rule Study Group. BMJ. Sep 2 1995;311(7005):594–597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leddy JJ, Smolinski RJ, Lawrence J, Snyder JL, Priore RL. Prospective evaluation of the Ottawa Ankle Rules in a university sports medicine center. With a modification to increase specificity for identifying malleolar fractures. The American journal of sports medicine. Mar-Apr 1998;26(2):158–165 [DOI] [PubMed] [Google Scholar]
- 9.Miller J, Gerber JP. Posterior distal tibial fracture in a military trainee. J Orthop Sports Phys Ther. 2011;41(8):615. [DOI] [PubMed] [Google Scholar]
- 10.Neumaier Probst E, Maas R, Meenen NM. Isolated fracture of the posterolateral tibial lip (Volkmann's triangle). Acta Radiol. May 1997;38(3):359–362 [DOI] [PubMed] [Google Scholar]
- 11.Arimoto HK, Forrester DM. Classification of ankle fractures: an algorithm. AJR Am J Roentgenol. Nov 1980;135(5):1057–1063 [DOI] [PubMed] [Google Scholar]
- 12.Michelson J, Solocoff D, Waldman B, Kendell K, Ahn U. Ankle fractures. The Lauge-Hansen classification revisited. Clin Orthop Relat Res. Dec 1997(345):198–205 [PubMed] [Google Scholar]
- 13.Lash N, Horne G, Fielden J, Devane P. Ankle fractures: functional and lifestyle outcomes at 2 years. ANZ J Surg. Oct 2002;72(10):724–730 [DOI] [PubMed] [Google Scholar]
- 14.Haapamaki VV, Kiuru MJ, Koskinen SK. Ankle and foot injuries: analysis of MDCT findings. AJR Am J Roentgenol. Sep 2004;183(3):615–622 [DOI] [PubMed] [Google Scholar]
- 15.Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. May 2006;88(5): 1085–1092 [DOI] [PubMed] [Google Scholar]
- 16.Kukkonen J, Heikkila JT, Kyyronen T, Mattila K, Gullichsen E. Posterior malleolar fracture is often associated with spiral tibial diaphyseal fracture: a retrospective study. J Trauma. May 2006;60(5): 1058–1060 [DOI] [PubMed] [Google Scholar]
- 17.Buchler L, Tannast M, Bonel HM, Weber M. Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma. Mar 2009;23(3):208–212 [DOI] [PubMed] [Google Scholar]
- 18.Shields BJ, Smith GA. Epidemiology of cheerleading fall-related injuries in the United States. J Athl Train. Nov-Dec 2009;44(6):578–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Streubel PNM J.J., Gardner M.J. The posterior malleolus: should it be fixed and why? Current Orthopaedic Practice. 2011;22(1):17–24 [Google Scholar]
- 20.Mingo-Robinet J, Lopez-Duran L, Galeote JE, Martinez-Cervell C. Ankle fractures with posterior malleolar fragment: management and results. J Foot Ankle Surg. Mar-Apr 2011;50(2):141–145 [DOI] [PubMed] [Google Scholar]
- 21.Papachristou G, Efstathopoulos N, Levidiotis C, Chronopoulos E. Early weight bearing after posterior malleolar fractures: an experimental and prospective clinical study. J Foot Ankle Surg. Mar-Apr 2003;42(2):99–104 [DOI] [PubMed] [Google Scholar]
- 22.Honigmann P, Goldhahn S, Rosenkranz J, Audige L, Geissmann D, Babst R. Aftertreatment of malleolar fractures following ORIF – functional compared to protected functional in a vacuum-stabilized orthesis: a randomized controlled trial. Arch Orthop Trauma Surg. Apr 2007;127(3):195–203 [DOI] [PubMed] [Google Scholar]
- 23.Simanski CJ, Maegele MG, Lefering R, et al. Functional treatment and early weightbearing after an ankle fracture: a prospective study. J Orthop Trauma. Feb 2006;20(2):108–114 [DOI] [PubMed] [Google Scholar]