Abstract
Study Design:
Case Report
Background:
Femoral acetabular impingement (FAI) has been implicated in the etiology of acetabular labral tears. The rehabilitation of younger athletes following arthroscopic surgery for FAI and labral tears is often complex and multifactorial. A paucity of evidence exists to describe the rehabilitation of younger athletes who have undergone arthroscopic hip surgery.
Case Presentation:
This case report describes a four-phase rehabilitation program for a high school football player who underwent hip arthroscopy with a labral repair and chondroplasty.
Outcomes:
The player returned to training for football 16 weeks later and at the 4 month follow-up was pain free with no signs of FAI.
Discussion:
There is little evidence regarding the rehabilitation of younger athletes who undergo arthroscopic hip surgery. This case study described a four phase rehabilitation program for a high school football player who underwent hip arthroscopy and labral repair. The patient achieved positive outcomes with a full return to athletic activity and football. The overall success of these patients depends on the appropriate surgical procedure and rehabilitation program.
Key Words:
Femoral acetabular impingement (FAI), hip, hip impingement
Level of evidence:
4-Case report
BACKGROUND
Labral tears of the hip commonly occur with FAI (Femoral acetabular impingement).1–5 Recently, FAI has been diagnosed more frequently in younger active individuals with an etiology that is not well understood.1 In fact, Ochoa et al looked at the radiographic evidence of 155 young active patients' 18-50 years of age with complaints of hip pain presenting to primary care and orthopaedic clinics. In the aforementioned study it was reported that 87% of the subjects had evidence of FAI.1
FAI is commonly classified as a cam-type, pincer-type, or mixed cam-pincer. Cam-type impingement occurs when the femoral head is abnormally shaped and contacts a normal acetabulum. The abnormally shaped “bump” abuts the acetabular rim creating shearing and compressive forces that may result in tearing of the acetabular labrum and chondral injury to the femoral head and/or acetabular rim.1,2,6 Research has identified that males have a predilection for cam-type impingement.7,8 Reichenbach et al conducted a cross-sectional study on 1,080 young asymptomatic male subjects using magnetic resonance imaging (MRI) and found a cam-type deformity in every fourth male and in every second male with decreased hip internal rotation.8 Allen et al also found a prevalence of 77.8% bilateral cam-type impingement in a sample of 113 symptomatic males.9 Pincer-type impingement occurs when the acetabular rim is abnormally shaped, deep, or retroverted and contacts a normally shaped femoral head.1,7 This “over-coverage” often results in labral degeneration and tearing.1,2,10,11 Pincer-type impingement is more common in females.10 Reichenbach and colleagues conducted an MRI cross sectional study on 80 young females (18-19 years-old) and found a greater prevalence of pincer-type deformity compared to cam-type deformity.12 When both cam & pincer-type deformity occur it is commonly classified as mixed. Studies have shown that mixed impingement can occur in 57-85% of younger individuals.2,7,13
Damage to the acetabular labrum from FAI can affect overall hip function. The acetabular labrum has various functions including enhancing joint stability, shock absorption, proprioception, joint lubrication, pressure distribution, deepening of the joint, and creating a seal.14,15 Labral tears occur most frequently in the anterior quadrant.14 Researchers have postulated that the anterior labral region may be more susceptible to tears due the following three factors: (1) the anterior labrum has a low vascular supply which results in poor healing; (2) this region is mechanically weaker than other regions; (3) the anterior labrum may experience higher loads and shear forces than other regions of the labrum.14–16 The consequence of hip labral damage is destabilization of the hip joint and increased loading of the articular cartilage which may lead to degenerative joint disease.14 McCarthyet al have proposed a series of events that may lead to intraarticular joint disease: (1) traction or FAI that excessively loads the acetabular labrum at the extremes of joint motion, (2) fraying of the articular margin of acetabular labrum, tearing along the articular margin of the acetabular labrum, (3) delamination of the articular cartilage from the articular margin adjacent to the labral lesion, and (4) more global labral and articular cartilage degeneration.14,15
Arthroscopic surgery for FAI & labral tears has become an accepted procedure for many athletes of varied ages. Due to the emergence of new surgical techniques and advances in diagnostic capabilities there is a gap in the research regarding rehabilitation of younger athletic individuals following hip arthroscopy. The rehabilitation of these athletes can be complex and requires a systematic approach to ensure a successful return to activity. A recent search of the literature revealed various approaches to rehabilitation in which most of them described a four- phase rehabilitation approach, however all but one of the articles were narrative reviews.17–21 One case report was found that described the four phase approach for a 25-year-old professional football athlete who underwent arthroscopic debridement and labral repair.21 Due to the paucity of literature, there is a need for a more detailed description of this four phase rehabilitation approach with younger individuals. The purpose of this case report is to describe the rehabilitation program for an 18 year-old athlete who underwent arthroscopic surgery for left hip mixed FAI with an anterior superior labral tear.
CASE DESCRIPTION
Patient History
The patient was an 18-year-old male high school athlete who underwent arthroscopic surgery for a left hip mixed FAI with an anterior superior labral tear in March 2011. The patient participated in high school football (at the free-safety position) and reported an insidious onset of left hip and groin pain for one year prior to formal diagnosis. The patient initially had intermittent “groin” pain and “clicking” during and after physical activity which eventually became more severe. As the severity increased, the patient began to feel anterolateral hip pain and had an observable antalgic gait. Aggravating activity included running, twisting or turning, sit to stand transitions, and stair ambulation. The patient managed his pain with ice and heat; however, increasing pain prompted him to see an orthopaedic surgeon. Diagnosis was confirmed by MR arthrogram (Tesla 3T from Phillips) which revealed a left mixed cam-pincer femoroacetabular impingement with an anterosuperior labral tear. The patient's symptoms were recalcitrant to physical therapy, activity modification, and medical management. Given the persistence of symptoms, lack of success with conservative management, and inability to participate in physical activity and sports without pain, he elected to undergo surgical intervention. The surgical intervention included an acetabular and femoral head osteoplasty & chondroplasty, a capsular synovectomy, and an anterior superior labral repair via two arthroscopic portals. The patient's primary goals were to return to pain-free physical activity and begin college football in the fall.
INITIAL EXAMINATION
The patient was seen for initial examination two days after surgery. The patient appeared to be a healthy 18-year-old male with a mixed endomorphic-mesomorphic build (Body mass-92.53 kg, Height-182.9 cm, Body mass index-27.7).
Functional Status
This patient came to the appointment ambulating on two crutches with “touch down” weight bearing precautions, which were to be continued for 6 weeks from the date of surgery in order to protect the labral repair site. The patient was restricted from flexing the hip beyond 90 degrees for the first 3 weeks post-operatively to protect the healing joint capsule. The patient was instructed to use a Continuous Passive Motion Machine (CPM) from 0-90 degrees of hip flexion for 4-6 hours per day for the first 4 weeks based on the surgeon's goal of enhancing joint motion and nutrition.
System Review
A review of the patient's history and the interview revealed no current or prior medical issues that would impede rehabilitation. Family history was negative for any cardiovascular risk factors or family history of hip pathology. Inspection of the incision site revealed adequate healing with the steri- strips intact over the mid anterior and anterolateral portals. A neurovascular screen of the lower extremity revealed no significant findings.
TEST AND MEASURES
Pain
During the initial examination, an 11-point numerical pain rating scale (0 no pain to 10 the worst pain imaginable) was used to elicit an objective ranking of the patients pain level.23,24 The patient reported a 2/10 pain at rest, 4/10 pain with prolonged ambulation, and an increase to 5/10 with combined hip flexion & internal rotation. The patient's overall pain was decreased to a 2/10 pain with pain medication (Vicodin).
Gait
A general gait assessment was conducted for crutch ambulation. The patient was able to ambulate using two crutches with a step through gait pattern and touch down weight bearing on the left lower extremity.
Range of Motion
The patient's hip, knee, and ankle range of motion (ROM) were tested both actively and passively as described by Norkin & White.25 Bilateral lower extremity measurements were WNL and symmetrical with the exception of the left hip.The patient was apprehensive with actively moving the left hip but agreed to assessment of passive range of motion (PROM). PROM of the left hip revealed the following: flexion 90 degrees, internal & external rotation 30 degrees, abduction 25 degrees, adduction 10 degrees, and hip extension 0 degrees. Motions were limited due to the patient's pain level.
Muscle Performance
The patient's muscle performance was measured using manual muscle testing as described by Hislop and Montgomery.26 All testing was conducted manually by the same clinician in a pain free manner. The left hip was tested within post-op ROM guidelines and the available pain free range of motion. Muscle performance results can be found in Table 1.
Table 1.
Muscle performance testing.
| Muscle Groups Tested | Right | Left |
|---|---|---|
| Hip flexors | 5/5 | 3/5 |
| Hip extensors | 5/5 | 3/5 |
| Hip abductors | 5/5 | 3+/5 |
| Hip adductors | 5/5 | 3/5 |
| Hip external rotators | 5/5 | 3+/5 |
| Hip internal rotators | 5/5 | 3+/5 |
| Knee extensors | 5/5 | 5/5 |
| Knee flexors | 5/5 | 5/5 |
| Ankle Dorsiflexors | 5/5 | 5/5 |
| Ankle Plantarflexors | 5/5 | 5/5 |
Muscle Length Assessment
Muscle length was tested on the patient's lower extremities. The patient's right lower extremity tested positive for the following: Ober's test for iliotibial band length and 90/90 test for hamstring muscle length.The patient's left lower extremity tested positive for the following tests: Ober's test, 90/90 hamstring test, and Ely's test for rectus femoris length. The Thomas test was not performed on the left hip due to patient's level of discomfort with hip extension.
Palpation
Palpation of the left hip musculature was assessed using a 5 point pain scale (Grade 0-4) as described by Hubbard & Berkoff.27 The grading criterion is as follows: Grade 0: no tenderness; Grade I: mild tenderness without grimace or flinch; Grade II: moderate tenderness plus grimace or flinch; Grade III: severe tenderness plus marked flinch or withdrawal; Grade IV: unbearable tenderness, patient withdrawals with light touch.27 Palpation of the patient's hip revealed grade II (moderate) tenderness along the iliacus, common iliopsoas tendon, adductors, and muscle belly of the tensor fascia lata. The patient also had grade I (mild) palpable tenderness around the surgical portals and proximal iliotibial band. There was no palpable tenderness of the hip external rotators.
Assessment
At the time of examination, the patient was two days post-surgical with the prescribed ROM and weight bearing precautions. The posture and ROM assessment revealed a compensatory right trunk shift away from the left lower extremity and decreased left hip ROM in all planes due to pain and apprehension by the patient. Strength & muscle length testing revealed general weakness and decreased length of the hip musculature which may have been linked to weight bearing precautions, disuse, and pain. Palpation also revealed tenderness in the anterior hip musculature. In the authors experience, anterior hip tenderness is a common and expected clinical finding following this type of hip surgery.
Plan of Care
The rehabilitation program (Table 2, a & b) was based on the hip arthroscopic post-operative protocol from the referring surgeon who utilizes the four phase rehabilitation program described in this case report.17–19,22 Trunk stabilization and general lower kinetic chain exercises were integrated into the program consistent with the regional interdependence model.28
Table 2.
Four phase rehabilitation program.
| Phases of Rehabilitation | |
| Phase T: Initial | Focus: protect the repaired tissue, restore ROM, control pain & inflammation, and restore neuromuscular control.17–20, 22 |
| Criteria for Phase IT: full weight bearing, minimal pain with phase T activity. ROM > 75% of the uninvolved side, and proper muscle firing patterns.17–19 | |
| Precautions: avoid hip flexor pain and follow ROM & weight bearing restriction.19 | |
| Range of Motion: upright bike riding, ankle pumps, towel slides, prone lying, quadruped rocking, and standing IR/ER with chair. | |
| Strengthening: isometrics for the hip and leg (e.g. Quad sets, hamstring sets), resisted prone TR/ER, three way leg raises (abduction, adduction, and hip extension), sidelying clams, double leg bridges, and leg press. | |
| Stretching: gluteals. hamstrings, and piriformis, hip flexor & adductor stretching began at 4 weeks. | |
| Manual Therapy: passive range of motion and joint mobilization began at 5 weeks | |
| Home Program: daily prone lying and passive range of motion. | |
| Phase II: Intermediate | Focus: protect the repaired tissue, restore ROM, restore a normal gait pattern, and progressively increase muscle strength.17–19,22 |
| Criteria for Phase III: pain-free gait, full ROM, hip flexion strength >60% of the uninvolved side, all other hip motion (abd, add, ext, IR, ER) strength >70%.17–19 | |
| Precautions: avoid forceful or ballistic stretching, no treadmill, and prevent hip flexor and joint irritation.19 | |
| Range of Motion: phase I activity | |
| Strengthening: phase I activity with the addition of closed kinetic chain (CKC) exercises which included: bilateral squats, side stepping, and ¼ lunges (sagittal & frontal plane). | |
| Abdominal Core: basic core strengthening (e.g. planks) exercises. | |
| Stretching: phase 1 stretching continued with the addition of self-myofascial release with the foam roll | |
| Cardiovascular: elliptical & stationary bicycle | |
| Manual Therapy: passive range of motion and joint mobilization | |
| Home Program: phases I & II activity and the addition of cardiovascular conditioning with the elliptical and stationary bike. | |
| Phases of Rehabilitation | |
| Phase III: Advanced | Focus: further restore muscular endurance & strength, improve cardiovascular endurance, and optimize neuromuscular control, balance, and proprioception.17–19,22 |
| Criteria for Phase IV: hip flexion strength >70% of the uninvolved side, all other hip motion fabd, add, ext, IR, ER) strength >80% of the uninvolved side, cardiovascular fitness equal to pre-injury level, and ability to participate in controlled initial agility drills.17–19 | |
| Precautions: avoid forceful or ballistic stretching, no treadmill, prevent hit) flexor and joint irritation, and avoid contact sports.19 | |
| Range of Motion: phases I & II activity | |
| Strengthening: phase 11 activity with the addition of multidirectional closed kinetic chain (CKC) exercises and basic movements on the TRX© suspension training system were introduced including (e.g. single leg squats, side lunges). | |
| Abdominal Core: progressive core exercises using the TRX© suspension training system (e.g. suspended planks, gluteal bridges). | |
| Stretching: basic stretching and self-myofascial release techniques were continued with emphasis on the rectus femoris, hip flexors, tensor fascia lata, and adductors. | |
| Cardiovascular: elliptical & stationary bike | |
| Manual Therapy: passive range of motion and joint mobilization | |
| Home Program: phases I to III activity, continue cardiovascular conditioning with the elliptical and stationary bike. | |
| Phase IV: Sports Specific | Focus: for the patient to work towards returning to competition.17–19,22 |
| Criteria for Phase IV: hip flexion strength >85% of the uninvolved side, full pain-free ROM. ability to perform sports specific drills at full speed, and successful completion of any sports related testing.17–19 | |
| Precautions: pain free activity | |
| Range of Motion: phases I to III activity as needed. | |
| Strengthening: phases 1 to 111 activity as needed. Begin sports specific activity including low level plyometrics, multi-directional agility drills, and circuit training. | |
| Abdominal Core: advanced core strengthening exercises on the TRX© (e.g. mountain climbers). | |
| Stretching: phases I to III activity as needed with the addition of a dynamic warm-up. | |
| Cardiovascular: elliptical, stationary bike, & progressive jogging (12 weeks) | |
| Manual Therapy: passive range of motion and joint mobilization as needed. | |
| Home Program: phases I to III activity and the introduction of jogging for cardiovascular conditioning. |
POST-OPERATIVE REHABILITATION
Phase I: Initial
The focus of phase one was to protect the repaired tissue, restore ROM, control pain & inflammation, and restore neuromuscular control.17–20,22 Phase I typically last from 4 to 6 weeks depending on the specific details of the surgical procedure and weight bearing guidelines.17–19 The recommended criteria for progressing from phase I to phase II included full weight bearing, minimal pain with phase I activity, ROM ≥ 75% of the uninvolved side, and proper muscle firing patterns (e.g. proper muscle recruitment with activity).17–19 Recommended precautions include: avoiding hip flexor pain and following ROM & weight bearing restrictions.19
During this phase, physical therapy interventions included the following ROM activities: upright bike riding (foot straps used), ankle pumps, towel slides, prone lying, quadruped rocking, and standing IR/ER with chair (Figure 1), assisted active and passive range of motion within post-operative guidelines in all planes of motion. Prone lying, which has been recommended to prevent hip flexion contractures,19,22 was also prescribed. Physical therapy also consisted of isometrics for the hip and leg (e.g. quad sets, hamstring sets), resisted prone IR/ER, active movement in three way leg raises (abduction, adduction, and hip extension), sidelying clamshells, double leg bridges, and leg press, initiated at week 6. In some cases, leg press may be introduced earlier but the surgical protocol should dictate such progressions. Basic core activities (e.g. the abdominal drawing in maneuver) were introduced during this phase. Gentle stretching for the gluteals, hamstrings, and piriformis were also done to improve muscle length while respecting mobility precautions. Hip flexor & adductor stretching was initiated at post-operative week 4 in order to avoid any myotendinous irritation.19,22 In the authors experience, early stretching and increased activity of the hip flexors and adductors can lead to inflammatory type pain at the tendons. These findings are supported by other authors who have reported similar results.22 Manual therapy focused on restoring mobility to the hip joint through passive range of motion and joint mobilization. It has been recommended to passively move the hip through all motions including circumduction to prevent intracapsular adhesions.17–19,22 Recently, Beck found adhesion formation that occurs between the joint capsule and the resected femoral neck may lead to soft tissue impingement by squeezing the acetabular labrum during hip flexion and internal rotation.29 These findings support the initiation of early passive hip motion and the monitoring of post-operative groin pain. Joint mobilization began at post-operative week 5 and consisted of anterior to posterior graded mobilization and long-axis distraction. A portion of each therapy session consisted of soft tissue mobilization, passive range of motion (PROM), and graded joint mobilization. PROM activity should be pain free and absent of any signs of impingement (e.g. pinching sensation) especially with circumduction.
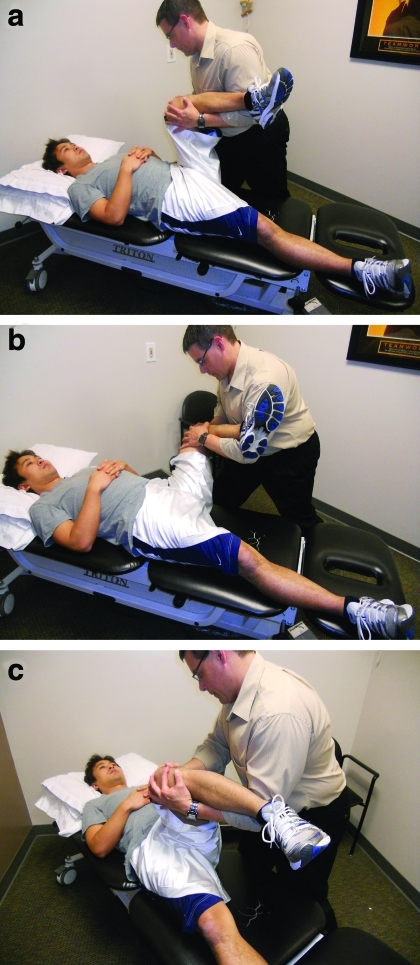
Figure 1.
Standing IR/ER with chair.
The patient's home exercise program also included daily prone lying and passive range of motion. Also, the patient's family was taught various assisted pain free passive hip movements which included passive hip flexion to 90°, circumduction (Figure 2 a,b,c), internal rotation, and external rotation, to be performed three times per day. The patient was seen for physical therapy an average of two times per week. After 6 weeks of physical therapy, the patient had met all criteria and was progressed to Phase II.
Figure 2.
Hip circumduction (a,b,c)
Phase II: Intermediate
The focus of phase II was to protect the repaired tissue, restore ROM, restore a normal gait pattern, and progressively increase muscle strength.17–19,22 Phase II typically begins between 4 to 6 weeks post-surgery depending on the surgical procedure and weight bearing guidelines.17–19 The recommended criteria for progressing from phase II to phase III included pain-free gait with full-weight bearing, full ROM, hip flexion strength >60% of the uninvolved side, all other hip motion (abd, add, ext, IR, ER) strength >70% of the uninvolved side.17–19 Recommended precautions include: avoiding forceful or ballistic stretching, no use of the treadmill, and preventing hip and joint irritation.19
The patient quickly progressed through this phase. Physical therapy included basic ROM & strengthening activities continued from Phase I with the addition of the elliptical trainer and mini trampoline marching for cardiovascular conditioning. The patient's program also included a progression of closed kinetic chain (CKC) exercises which included: bilateral squats, side stepping, and ¼ lunges. These movements were limited to the sagittal and frontal plane in order to avoid increased stress in the hip. Consistent with the regional interdependence model, core strengthening (e.g. planks) exercises were introduced during this phase given the interrelationship between proximal stability and the lower kinetic chain. Balance activity was introduced which included single leg stance on the ground and foam pad. Stretching activities from Phase I continued with the addition of self-myofascial release with the foam roll.
Manual therapy by the physical therapist focused on the soft tissue management of the anterior hip musculature with emphasis on the illiopsoas, tensor fascia lata, and adductors. These muscles had become overactive and shortened which was confirmed upon phase II re-examination of muscle length (e.g. Thomas test, etc.). Manual treatment also included graded anterior to posterior and long-axis distraction joint mobilization, and PROM.
The patient's home exercise program included Phase I & II activity with the addition of cardiovascular conditioning with the elliptical and stationary bike. At 8 weeks post-operative, the patient met all criteria and was progressed to Phase III.
Phase III: Advanced
The focus of Phase III was to further restore muscular endurance & strength, improve cardiovascular endurance, and optimize neuromuscular control, balance, and proprioception.17–19,22 Phase III is typically started between 6 to 8 post-operative weeks depending on the patient status.17–19 The recommended criteria for progressing from phase III to phase IV includes hip flexion strength >70% of the uninvolved side, all other hip motions (abd, add, ext, IR, ER) strength >80% of the uninvolved side, cardiovascular fitness equal to pre-injury level, and ability to participate in controlled initial agility drills.17–19 Recommended precautions include: avoiding forceful or ballistic stretching, no use of the treadmill, preventing hip flexor and joint irritation, and avoiding contact sports.19 In the authors experience, the treadmill is often withheld due to the change in gait (e.g. stride length) that may occur. Moreover, the authors believe that this change in gait may cause increased demands to the hip musculature and surgical site.
During this phase, the patient continued the basic ROM & strengthening activities in phase II with the addition of more advanced activity. Multidirectional closed kinetic chain (CKC) exercises and basic movements on the TRX® Suspension training system (TRX®) (Fitness Anywhere LLC, San Francisco, CA) were introduced including single leg squats (Figure 3) and side lunges. Exercise variables that were manipulated include repetitions, speed of movement, and surface stability. More progressive core exercises were performed including suspended planks (Figure 4) and gluteal bridges (Figure 5) on the TRX®. The aforementioned TRX® exercises provide an alternative to traditional bodyweight exercise. However, if such equipment is unavailable, it is not unreasonable to assume traditional bodyweight activity or use of a physioball could be just as effective. Alternatives for the lower extremity exercises mentioned above may include single leg squats and side lunges with dumbells and alternatives for the core exercises may include planks or glut bridges on a physioball. Balance activity was progressed using the BOSU® (Team BOSU, Canton, OH). The authors utilized more qualitative assessment to measure balance (e.g. time) and neuromuscular control (e.g. use of ankle & hip strategy). Basic stretching and self-myofascial release techniques were continued with emphasis on the rectus femoris, hip flexors, tensor fascia lata, and adductors. Manual therapy continued with soft tissue management of the hip musculature and graded joint mobilization. Graded joint mobilization was continued in order to maintain joint mobility.
Figure 3.
Single leg squat on TRX©
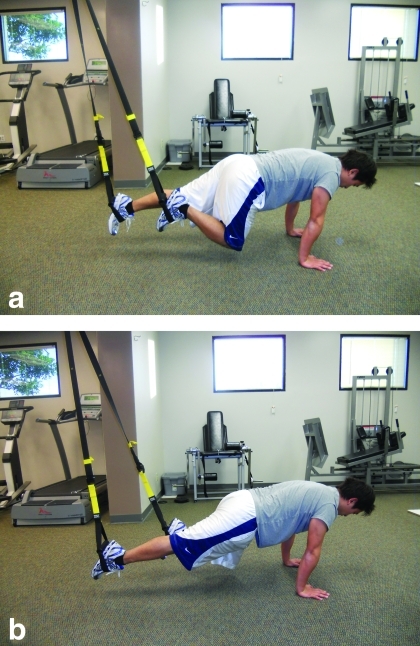
Figure 4.
Suspended plank on TRX©
Figure 5.
Gluteal Bridge on TRX©
The patient's home exercise program included Phase III activity with the elliptical & stationary bike for cardiovascular conditioning. At 12-weeks post-operative the patient met all criteria and was progressed to Phase IV.
Phase IV: Sports Specific
The focus of Phase IV is for the patient to work towards returning to competition.17–19,22 This phase typically begins between 8 to 16 weeks depending on the patients status.17–19 The recommended criteria for progressing from Phase IV to unrestricted sports activity includes: hip flexion strength >85% of the uninvolved side, full pain-free ROM, ability to perform sports specific drills at full speed, and successful completion of any sports related testing.17–19 Recommended precautions at this phase include maintaining activities at the pain free level.
During this phase, the patient continued the muscle performance activities from Phase III with the addition of more advanced activity. The patient began sports specific activity including low level plyometrics (e.g. jump rope), multidirectional agility drills (e.g. ladder drills), and circuit training. Examples of the exercise variables manipulated included speed of movement, planes of motion, and work to rest ratios. Emphasis was placed on proper lower kinetic chain mechanics through the hip, knee, and foot during multidirectional movements. This ensured that the lower extremity was functioning as an efficient interdependent system during ballistic activity.
Progressive jogging activity began at post-operative week 12 with a combination of distance running and short sprints. Advanced core strengthening was introduced including advanced TRX© exercises such as mountain climbers (Figure 6 a,b). An alternative would be to do this movement with hands on the ground or on a bench. Advanced balance activity was introduced by challenging the patient's visual, vestibular, and somatosensory systems. Examples of activities included ball tossing on unstable surface (air filled disc), single leg balance with eyes closed, and diagonal eye and head movements while standing on the BOSU® ball. Dynamic warm-ups were introduced prior to activity and basic stretching and self-myofascial release techniques for the lower extremity were continued after physical activity. The overall focus was to prepare the patient for advanced training by improving dynamic balance and eccentric control. As needed, manual therapy was performed to manage any residual soft-tissue or joint restrictions.
Figure 6.
Mountain Climbers on TRX© (a,b)
OUTCOMES
Discharge
The patient was discharged in August 2011 after completing 16 weeks of physical therapy with reports of 0/10 pain with activities of daily living, weight training, and sports activity (e.g. jogging, football drills). The left hip had full pain-free motion and all hip & knee manual muscle tests were graded a 5/5. The authors did not have access to a hand held dynamometer or isokinetic device which would have provided a more objective measurement of the patients muscle strength. Muscle length was normal except for mild hip flexor tightness confirmed with the Thomas test. The patient had adequate neuromuscular control with single leg and multidirectional activity demonstrated by little compensatory movements at the hip, knee, and ankle. This patient met all goals for Phase IV except for sports specific testing thus was immediately scheduled to begin advanced sports specific and agility training in preparation for the next football season. This included sports specific testing and creation of a periodization program.
Follow-Up (1-month)
At the one month follow-up, the patient reported pain-free sports specific training, weight lifting, agility training, and jogging. The re-examination revealed the same findings at discharge with normal hip ROM, hip muscle strength 5/5, and no signs of hip impingement with the Flexion-Adduction-Internal Rotation (FADIR) test. The patient still had adequate neuromuscular control with single leg squats and multidirectional movements. The patient had mild muscle length deficits in the hamstrings and hip flexors. The patient's home flexibility program was reviewed including self-myofascial release techniques utilizing a foam roll.
Follow-Up (4-months)
At the four month follow-up, the patient had reduced his body mass to 83.91 kg and presented with a mesomorphic build. The patient had also returned to full pain-free unrestricted activity that included running, power lifting, and football training at college. The re-examination revealed normal active and passive range with all hip motions and no hip impingement signs with the FADIR test. All hip & knee muscle tests were graded at 5/5 and muscle length was normal throughout the hip and lower extremity. The patient also had adequate neuromuscular control with full squats, single leg balance, single leg squats and multiplanar movements.
DISCUSSION
The presence of FAI in younger football players may be more prevalent than previously suspected. In fact, Kapron et al looked at the radiographic prevalence of FAI in 65 male collegiate football players (age, 21±1.9 yrs) and found that 95% had a least one sign of cam or pincer impingement and 57% had signs of both (mixed).3 Despite the advances in diagnostics and surgical interventions there still is a dearth in the literature addressing the rehabilitation of these individuals. Currently only one case study was found that examined the rehabilitation of a 25 year-old professional football player.22
This case report outlined a four phase rehabilitation program for a high school football athlete who underwent arthroscopic surgery for a mixed FAI impingement and an anterosuperior labral tear. The patient achieved successful outcomes with a full return to athletic activity and football after 16 weeks of structured rehabilitation. The overall success of these patients depends on the appropriate surgical procedure and rehabilitation program. This is supported by findings from Philippon and colleagues who examined the outcomes of 45 professional athletes who underwent hip arthroscopic FAI decompression, labral repair, and prescribed rehabilitation.11 At the average 1.6 year follow-up, 42 (93%) of the athletes had returned to professional competition.11
It is critical for the clinician to understand that each phase in the rehabilitation process builds upon the previous, which allows for a safe progression. Early phases of rehabilitation should emphasize hip PROM to avoid intraarticular adhesions29 and isolated muscle strengthening in order to regain appropriate neuromuscular control.19 Later phases should emphasize dynamic muscular control and preparation for sports specific activity.19 Each phase should be criterion based in order to consider the patient's individual healing process and any barriers (e.g. co-morbidities) that may be present. The clinician may want to standardize their muscle performance testing procedures for each phase. The use of MMT is often subjective and may be difficult to assess (e.g. 60 vs. 70%) between phases.30,31 If available, the use of dynamometry or isokinetic strength testing may provide a more objective interpretation.31 The authors also recommended the use of an objective functional outcome measure such as the Lower Extremity Functional Scale (LEFS) at the initial consult and at discharge to provide a more comprehensive outcomes assessment. This was a limitation of the current case report.
For younger football players, future studies should focus on risk factors for the development of FAI that may be related to position, training methods, and maturation. Future research should also focus on the outcomes of the four phase rehabilitation program for younger athletes in specific sports including: dance, hockey, and soccer.
The outcomes of this case study, using the four phase protocol, were based on the authors' clinical experience with this type of surgery. There is a definite need to establish evidence based specifics regarding the timing and implementation of the four phase protocol or any interventions used for the management of post-operative FAI. Such evidence would help to guide the clinician in developing effective and sports specific rehabilitation programs.
CONCLUSION
There is little evidence regarding the rehabilitation of younger athletes who undergo arthroscopic hip surgery. This case report described a four phase rehabilitation program for a high school football player who underwent hip arthroscopy and labral repair. The success of the rehabilitation program was based upon a systematic progression and introduction of interventions at the appropriate time.
References
- 1.Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010. October; 468(10): 2710–2714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phillipon M, Schenker ML. Arthroscopy for the treatment of femoral acetabular impingement in the athlete. Clin Sports Med. 2006; 29:299–308 [DOI] [PubMed] [Google Scholar]
- 3.Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players. J Bone Joint Surg AM. 2011;93:e111(1–10). [DOI] [PubMed] [Google Scholar]
- 4.Wenger DE, Kendell KR, Miner MR, et al. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004. Sep (426):145–50 [DOI] [PubMed] [Google Scholar]
- 5.Meermans G, Konan S, Haddad FS, et al. Prevalence of acetabular cartilage lesions and labral tears in femoroacetabular impingement. Acta Orthop Belg. 2010. Apr;76(2):181–8 [PubMed] [Google Scholar]
- 6.Kelly BT, Weiland DE, Schenker ML, et al. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–504 [DOI] [PubMed] [Google Scholar]
- 7.Hack K, Di Primio G, Rakhra K, et al. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010. Oct 20;92 (14):2436–44 [DOI] [PubMed] [Google Scholar]
- 8.Reichenback S, Juni P, Werlen S, et al. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care & Res. 2010;62 (9): 1319–1327 [DOI] [PubMed] [Google Scholar]
- 9.Allen D, Beaulé PE, Ramadan O, et al. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009; 91-B: 589–594 [DOI] [PubMed] [Google Scholar]
- 10.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol. 2007. Jun;188 (6): 1540–1552 [DOI] [PubMed] [Google Scholar]
- 11.Philippon M, Schenker M, Briggs K, et al. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007; 15(7): 908–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reichenback S, Juni P, Werlen S, et al. Prevalence of cam and pincer-type deformities on hip mri in a swiss female population: a cross-sectional study. Arthritis Rheum. 2011;63 Suppl 10:1077. [DOI] [PubMed] [Google Scholar]
- 13.Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018 [DOI] [PubMed] [Google Scholar]
- 14.McCarthy JC, Noble PC, Schuck MR, et al. The otto e. aufranc award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001. Dec;(393):25–37 [DOI] [PubMed] [Google Scholar]
- 15.Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009; 2:105–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;170–177 [PubMed] [Google Scholar]
- 17.Garrison JC, Osler MT, Singleton SB. Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther. 2007. November; 2(4): 241–250 [PMC free article] [PubMed] [Google Scholar]
- 18.Wahoff M, Ryan M. Rehabilitation after hip femoralacetabular impingement arthroscopy. Clin Sports Med. 2011. Apr;30(2):463–82 [DOI] [PubMed] [Google Scholar]
- 19.Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25: 337–357 [DOI] [PubMed] [Google Scholar]
- 20.Enseki KR, Martin R, Kelly BT. Rehabilitation after arthroscopic decompression for femoroacetabular impingement. Clin Sports Med. 2010; 29: 247–255 [DOI] [PubMed] [Google Scholar]
- 21.Eneski KR., et al. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36(7):516–525 [DOI] [PubMed] [Google Scholar]
- 22.Philippon MJ, Christensen JC, Wahoff MS. Rehabilitation after arthroscopic repair of intra-articualr disorders of the hip in a professional football athlete. J of Sports Rehab. 2009;18:118–134 [DOI] [PubMed] [Google Scholar]
- 23.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126 [DOI] [PubMed] [Google Scholar]
- 24.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74 [DOI] [PubMed] [Google Scholar]
- 25.Norkin C., White D. Measurement of Joint Motion: A Guide to Goniometry. 4thed. Philadelphia: F. A. Davis; 2009 [Google Scholar]
- 26.Hislop HJ, Montgomery J. Daniels and Worthingham's Muscle Testing: Techniques of Manual Examination. 7th ed. Philadelphia, Pa: WB Saunders Co; 2002 [Google Scholar]
- 27.Hubbard DR, Berkoff GM. Myofascial trigger points show spontaneous needle emg activity. Spine. 1993;18:1803–1807 [DOI] [PubMed] [Google Scholar]
- 28.Wainner R, Whitman J, Cleland J, et al. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37(11):658–660 [DOI] [PubMed] [Google Scholar]
- 29.Beck M. Groin pain after open fai surgery. Clin Orthop Relat Res. (2009) 467:769–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knepler C, Bohannon RW. Subjectivity of forces associated with manual-muscle test grades of 3+, 4-, and 4. Percept Mot Skills. 1998. Dec; 87(3 Pt 2):1123–8 [DOI] [PubMed] [Google Scholar]
- 31.Bohannon RW. Quantitative testing of muscle strength: issues and practical options for the geriatric population. Top Geriatr Rehabil. 2002;18(2):1–17 [Google Scholar]