Abstract
Background:
The management of the pediatric patient with an Anterior Cruciate Ligament (ACL) rupture is evolving towards earlier reconstruction. The rehabilitation progression and outcomes for skeletally immature individuals undergoing ACL reconstruction (ACL-R) are not well described in the literature. Differences in surgical procedure, age related physiology, and emotional maturity may have a significant impact on recovery and return to sports. The purpose of this case report is to present the rehabilitation and outcome of a skeletally immature patient that underwent an all-epiphyseal ACL-R, highlight important considerations in the rehabilitation process and present topics for future research.
Case Description:
Single subject case report of an 8 year-old boy who underwent all epiphyseal ACL-R after complete ACL rupture.
Outcomes:
The patient was able to achieve at least 90% strength symmetry and pass all necessary functional criteria to return to sports by 9 months post surgery. Two year follow up data indicated that the patient was able to make a full return to previous level of athletic activity, as well as maintain lower extremity strength and power over time.
Discussion:
Objective outcome measures, rehabilitation protocols and time frame for return to sports for skeletally immature patients following physeal sparing or all epiphyseal ACL-R are not well described in the literature. This case report outlines objective measures of strength and functional recovery in a patient from this unique population. As ACL-R in the skeletally immature patient is studied more, new information on rehabilitation progression and outcomes may alter the rehabilitation program and timeline for return to unrestricted activity.
Level of Evidence:
4, Case Report
Keywords: Anterior cruciate ligament, pediatric, rehabilitation, return to sports
BACKGROUND
Intrasubstance Anterior Cruciate Ligament (ACL) tears are being reported with increasing frequency in the pediatric skeletally immature population.1–2 Although there is no consensus regarding non-operative versus operative treatment, delaying treatment until closer to skeletal maturity has been associated with chronic instability leading to chondral and meniscal injuries.3–8 Traditional adult ACL reconstruction (ACL-R) techniques are not advisable in this population due to the possible risk of growth disturbance via disruption of the physis, commonly referred to as the growth plate.9 The physes of the distal femur and proximal tibia display extremely rapid growth during the adolescent growth spurt; with the distal femur contributing 40% and proximal tibia contributing 27% of the overall growth of the lower extremity.10–11 The femoral attachment of the ACL is only a few millimeters from the distal femoral physis and traditional tunnels used for ACL reconstruction in adults cross the physis obliquely and eccentrically.12–13 The tibial physis, while more distant from the tibial attachment, is also often crossed with the tunnels used in most standard adult ACL-R techniques. Tensioned grafts, rigid graft fixation, bone blocks that cross the physis and large drill holes in the physis have all been shown to increase the risk of causing a disturbance in the growth of the physis. This could lead to angular limb deformity or length disparity.1–2
Multiple techniques for surgical stabilization of the skeletally immature ACL deficient knee have been described.1–2 Recently an all epiphyseal ACL-R technique was described, that completely avoids the growth plates while still placing the ACL graft in the anatomical footprint of both the tibial and femoral attachments.9 This approach theoretically minimizes the risk of any growth abnormality due to surgery.
It is well recognized that the rate of ACL injury in the skeletally immature population is rising and with advancing surgical techniques there is a resulting increased need for post-operative physical therapy in this population.2–3 Physical rehabilitation from ACL-R in the adult population is well studied. Numerous authors have reported on successful outcomes and have identified objective performance data for rehabilitation progression and return to sports participation timeframe.14–16 However, research studying the outcomes of the skeletally immature patient after ACL-R is sparse and it remains unclear if these same recommendations and outcomes for the skeletally mature population apply in the pediatric population.3
Due to several key differences in the operative technique and age related tissue healing characteristics, modifications to the accepted evidence based rehabilitation scheme for adults are often utilized.17 Furthermore, cognitive, emotional and behavioral factors specific to the pediatric patient must be considered and can have a significant impact on the decision making process to elect surgical management and the rehabilitation program afterward.
The purpose of this case report is to present the rehabilitation and outcomes for an 8 year-old boy that underwent an all epiphyseal ACL-R. His experience will be used to highlight important considerations in the rehabilitation of these patients, to provide practical tips in approach, and introduce concepts for discussion and possible future research.
CASE DESCRIPTION
Participant and History
The patient was an 8 year-old boy (height 144 cm; weight 42 kg; Body Mass Index 21 kg/m2) who injured his right knee while attempting to land from a jump in the terrain park while skiing. Upon landing, the patient remembers his right leg twisting, feeling a “pop” and immediate pain in his knee. Physical examination and subsequent magnetic resonance imaging (MRI) confirmed the diagnosis of a complete tear of the ACL. Since he was having a recurrent sense of instability following the injury and wished to continue with an active lifestyle, after considerable thought and discussion regarding the risks and benefits of operative versus non-operative management, the patient and his family elected he undergo surgical reconstruction.
Pre-operative physical therapy
The patient was referred to physical therapy prior to surgery for gait training, post-operative education, and assessment of motivation, maturity level and ability to comply with post-operative restrictions. The patient underwent gait training utilizing bilateral axillary crutches and was educated on toe touch weight bearing (TTWB) precautions, to be used immediately after surgery. The parents and patient were also educated in proper techniques for post-operative pain management, swelling reduction techniques and an initial exercise program. During this session, he displayed a good cognitive and physical understanding of his injury and the importance of the post-operative rehabilitation involved. He took directions well, had no problems with activity restrictions and easily learned the exercises. The authors have found that these are important characteristics that help to determine if the patient is an appropriate rehabilitation candidate in order to ensure good surgical outcomes.
The patient required one pre-operative treatment session as he had already met all the following pre-operative goals: no effusion, at least 4/5 quadriceps strength with manual muscle testing, full knee extension range of motion, at least 120° of active knee flexion range of motion, independence with gait maintaining weight bearing precautions, and independence with immediate post-operative exercise instructions.
Surgical Procedure
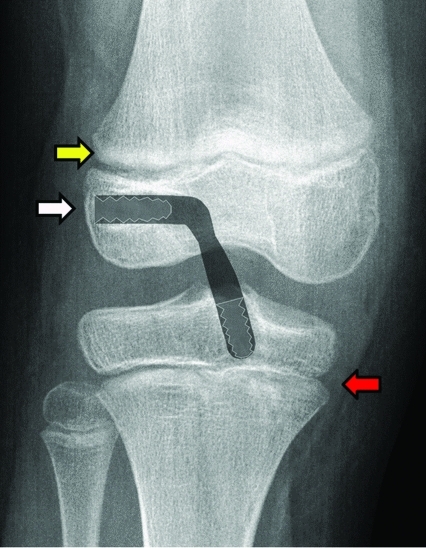
Approximately two months after initial injury, a fellowship trained pediatric and sports medicine orthopedic surgeon performed an all-epiphyseal ACL-R with a quadrupled autologous hamstring graft, using a newly described technique.9 This technique adheres to the generally accepted principles of ACL-R by placing the graft in the center of the native footprint of the ACL, but theoretically minimizes the risk to the growing physes by avoiding any fixation, large drill holes, or tensioning of the graft across the physes (Figure 1). During the procedure, an intra-operative computed tomography scan with 3-dimensional reconstruction is utilized to ensure safe and accurate placement of tunnels in the distal femoral and proximal tibial epiphyses avoiding the physes and the articular surfaces.
Figure 1.
Schematic representation of All Epiphyseal ACL Reconstruction. Post-operative x-ray image with schematic representation of the graft and interference screw fixation. The tunnels are drilled to the center of the femoral and tibial ACL footprints (white arrow). The tunnels, the graft material and graft fixation are contained entirely within the epiphysis. No large drill holes are made in the tibial (red arrow) or femoral (yellow arrow) physes, no fixation crosses the physis and the graft is not tensioned across the physis.
Postoperative Intervention
After surgery the patient was placed in a hinged postoperative knee brace locked in slight hyperextension. He was instructed to remain in the brace at all times, with the exception of while bathing or in physical therapy. Specific care was taken to make sure the patient understood he needed to wear the brace while sleeping. He used a continuous passive motion (CPM) machine for up to 6 hours per day. The range of motion was initially set from 0°-30° and he was instructed to progress his movement by 5°-10° of flexion per day as his pain permitted. The patient was restricted to TTWB utilizing bilateral axillary crutches as he had been instructed prior to surgery. An inpatient physical therapist reviewed gait training and ensured the patient was adherent to weight bearing restrictions and safe with ambulation prior to discharge.
Formal outpatient physical therapy was initiated on post-operative day 11 and treatment was progressed based upon our all epiphyseal ACL-R post-operative protocol (Appendix 1). Our current protocol is based upon the integration of known ACL healing characteristics in the adult population and surgeon expertise. The protocol utilizes both time and criteria based benchmarks for progression through the phases of rehabilitation.
The patient's pain was assessed utilizing a visual analog scale where a score of 0 represents “no pain” and a score of 10 representing “worst pain imaginable”. The patient rated his pain 0/10 at the initial visit, with the worst pain being 6/10 since surgery. A moderate joint effusion was present with a difference of 0.8 cm side to side in circumference measurement. Active knee extension-flexion range of motion (ROM) was 0°-65° and passive range of motion was 0°-85°. Trace quadriceps activation was present on the involved leg and he was unable to perform a straight leg raise (SLR) without an extensor lag. The patient was started on a basic program consisting of active and passive ROM exercises, quadriceps sets and straight leg raises with the brace locked in extension. The patient was fitted with a knee compression sleeve and educated in effusion management. The patient was given specific instructions to elevate his leg for 15 minutes every hour while in school. A note was issued to his teacher detailing this program.
By the end of post-operative week 3, the patient had achieved 0-90° of passive knee ROM. He went on to recover full passive ROM of 0-150° by week 7. Quadriceps function returned quickly and the patient was able to perform a SLR with no lag during the 2nd post-operative visit. As quadriceps strength improved, the patient was able to ambulate without knee buckling or hyperextension in stance phase. At this point, the patient had achieved sufficient muscular control of the knee to unlock his post-operative brace and begin weaning off crutches. Table 1 details the timeline for gait and brace weaning progression used for this patient. By post-operative week 5, the patient had met the proposed functional criteria of knee ROM greater than 0-100° and ability to perform a single limb squat to at least 30° of knee flexion, which would allow him to discontinue use of his hinged knee brace. However, according to the protocol, the patient is not permitted to discontinue brace usage until 6 weeks post-operative. Adherence to the use of bracing was causing the patient to become frustrated and his parents reported this was leading to some behavioral difficulties. As a compromise, the patient was allowed to ambulate without the brace at home, but was still advised to continue to wear the hinged brace when in public and at school.
Table 1.
Sequence of brace management and gait progression.
| Post-op Week | Brace Status | Weight Bearing |
|---|---|---|
| Week 0-3 | Locked at 0° | Toe-Touch |
| Week 4 | Open 0°-50° | Partial Weight Bearing (PWB) |
| Week 5 | No Brace (at home) | FWB |
| Open 0°-90° | FWB | |
| Week 6 | No Brace | FWB |
Open kinetic chain knee extension and flexion exercises were held until after post-operative week 10. After that, the remainder of the progression followed the protocol of accelerated rehabilitation based on established guidelines for strengthening and dynamic stabilization training derived from guidelines following adult ACL-R.
According to the protocol, the following criteria were used for advancement to running and dynamic activity: 1) The patient should be tolerating all rehab progression with no adverse reactions 2) satisfactory physician clinical and radiograph exam 3) less than 25% peak torque quad deficit with isokinetic testing at 180° and 300° per second and 4) less than 3 mm translation with KT-1000 (MEDmetric® Corporation, San Diego, CA) knee arthrometer testing. Formal evaluation for advancement was performed at 14 weeks post-operatively. Due to the patient's physical size, the KT-1000 unit would not fit appropriately and therefore did not yield a reliable measurement. Thus, this criterion for advancement could not contribute to clinical decision making. Utilizing the unaffected limb as a control, isokinetic testing revealed a peak torque quadriceps deficit of 6.3% and 10.9% at 180 and 300 degrees per second respectively. The patient had been tolerating all rehabilitation exercises without complication and satisfied all physical therapy clinical testing criteria for advancement. Physician follow-up examination for progression was not scheduled until post-operative week 16. Formal physical therapy was temporarily discontinued and the patient continued performing his established home exercise program supervised by his parents. After a satisfactory physician examination, he was cleared for advancement by the physician.
The patient was progressed through running and agility exercises beginning in straight planes with double leg activities and progressing to multidirectional drills. Plyometric training began at 19 weeks post-operatively with low-level bilateral training. The therapist focused instruction of technique emphasizing limiting ground impact forces and limiting any dynamic knee valgus at takeoff or landing. As the patient demonstrated proper mechanics, the demand of plyometric training was increased from bilateral to unilateral tasks and finally to multiplanar jumps. At this point in time, the patient was fitted with a DonJoy™ Full Force functional ACL brace (DJO Global, LLC, Vista, CA). The recommendation by the surgeon is that the brace be worn with all sports activity for at least 2 years following surgery.
Progression to sports specific rehabilitation activities is typically allowed between weeks 24-36 and is dependent upon the patient satisfying the following criteria: 1) pain free with all activity thus far 2) quadriceps peak torque deficit less than 10% 3) functional hop test scores of less than 10% deficit 4) satisfactory lower extremity control and alignment during jumping task. The patient was tested at 6 months post surgery. Isokinetic testing results demonstrated a 9.3% peak torque quadriceps deficit at 180° and a 3.1% strength advantage on his operated leg at 300° per second. Functional hop testing consisted of a single leg hop, single leg triple hop, single leg vertical jump and single leg side-to-side jump. As outlined in Table 2, the patient was able to achieve at least 90% symmetry with all functional hop tests, with the exception of timed side to side hop, which was 88% symmetrical. He demonstrated excellent landing form with no valgus movement of the knee upon landing or take off, ability to cushion impact descending into approximately 20-30° hip and knee flexion upon landing and stable balance with landing.
Table 2.
Functional Hop Test Results at 6 months post-surgical follow up.
| Functional Hop Test | Involved leg | Uninvolved Leg | Involved / Uninvolved | Percentage Deficit |
|---|---|---|---|---|
| Single Leg Jump | 109 cm | 101 cm | 1.07 | +7% |
| Single Leg Triple Jump | 300 cm | 295 cm | 1.02 | +2% |
| Single Leg Vertical Jump | 16.5 cm | 18.3 cm | .90 | −10% |
| Single Leg Timed side to side Jump* | 15 ground contacts | 17 ground contacts | .88 | −12% |
The patient is instructed to jump side to side as fast as they can over two lines 12” apart for a period of 20 seconds. The number of successful ground contacts the patient has on each leg within 20 seconds is counted.
Outcomes
The patient had achieved all clinical criteria necessary to return to sports within 6 months of ACL-R, however as outlined in the protocol unrestricted return to competitive sports was held until the patient is 9 months post-op. The patient had already been performing a home program that consisted of running, agility and plyometric training. He was discharged from physical therapy and advised to continue this program until his 9-month follow up with his surgeon. In the interim, he was allowed to participate in modified gym class and recess activity that did not involve any contact, as long he wore his functional ACL brace. He was advised to refrain from high-risk activities such as jumping on trampolines, skateboarding, and wrestling with his brothers.
The patient returned for long term follow-up at approximately 2 years post surgery. He had returned to all recreational activities including competitive baseball and skiing. He reported no feelings of knee instability with any activity. Upon isokinetic testing patient demonstrated a strength advantage of 19.3% and 12.5% for peak torque extension force at 180 and 300 degrees per second respectively. Functional hop testing revealed the patient was able to maintain criteria of at least 90% symmetry between limbs over time. Please see Table 3 for more specific details of hop testing data.
Table 3.
Functional Hop Test Results at 2 year post-surgical follow up.
| Functional Hop Test | Involved leg (cm) | Uninvolved Leg (cm) | Involved / Uninvolved | Percentage Deficit |
|---|---|---|---|---|
| Single Leg Jump | 117 cm | 117 cm | 1.00 | 0% |
| Single Leg Triple Jump | 363 cm | 401 cm | 0.91 | −9% |
| Single Leg Vertical Jump | 17 cm | 17.5 cm | 0.97 | −3% |
| Single Leg Timed side to side Jump* | 22 ground contacts | 21 ground contacts | 1.05 | +5% |
The patient is instructed to jump side to side as fast as they can over two lines 12” apart for a period of 20 seconds. The number of successful ground contacts the patient has on each leg within 20 seconds is counted.
DISCUSSION
Numerous authors have reported on successful rehabilitation after adult ACL-R and functional testing programs have been developed to help guide rehabilitation and determine readiness for return to sports participation.16 However, few authors have reported on similar outcomes in the pediatric population.3 Most outcome studies focus primarily on determination of any adverse effects on skeletal growth and define functional success based mostly on self report scales.4,18 Bonnard et al reported on 57 cases of physeal sparing ACL-R with mean age at surgery of 12.2 years and a minimum of 2 year follow-up. They found that mean time for return to sport was 11 months (range 6-18 months) and that 90% had excellent or good results based on subjective assessment using the International Knee Disability Classification (IKDC) score. The IKDC is a knee specific patient reported outcome measurement tool that has demonstrated adequate psychometric properties for use in the adult population, however it has not been validated for use in children or adolescents.19 Thus, the use of this scale as the primary outcome measure for this population may not yield the most reliable outcome data. Furthermore Bonnard et al do not report on specific objective outcome measures in order to demonstrate functional return of strength, power and physical ability. The case presented here demonstrates successful achievement of all return to sports criteria within 6 months of surgery and presents specific objective data about strength and functional performance throughout the recovery timeline in an 8 year old patient. This patient was able to return to sports participation at 9 months post surgery. Although this case demonstrates a successful outcome, there are many questions regarding rehabilitation in this population that remain unanswered.
Due to the unique nature of this procedure, tissue healing characteristics are not well studied in the pediatric patient after ACL-R. Physiological healing differences may account for variations seen in rehabilitation and return to activity timelines between physeal sparing and adult ACL reconstruction.16 Early weight bearing is typically advocated following adult ACL reconstruction, however many surgeons advise a period of limited weight bearing for physeal sparing procedures.10 The recommendation for limited weight bearing in our protocol is largely based on surgeon expertise, mostly respecting the behavioral challenges that accompany this population but also acknowledging possible stress concentration across the physis, due to the location of the femoral tunnel. The pediatric patient may not possess the patience and self-control necessary to ambulate WBAT with proper gait mechanics. In such a child, excessive early weight bearing and poor gait mechanics could risk the health of the graft tissue, cause increased joint effusion and pain, and lead to lasting gait abnormalities or arthrofibrosis. Femoral tunnel placement within a few millimeters of the growth plate, while not directly disturbing the physis, may nonetheless cause stress concentration in other areas of the physis. For these reasons, it may be more beneficial to restrict weight bearing in this population in order to avoid these possible complications. The therapist familiar with this population will be able to use experience and clinical milestones such as quadriceps strength, knee stability in closed chain tasks and effusion level, to properly progress the patient's weight bearing and gait status. These recommendations may change as physeal stress reactions and mechanisms of healing are studied further.
The physiology of strength development in the prepubescent child must also be considered during the rehab process. Prepubescent children lack circulating androgens and strength gains seen in this population are not always associated with muscle hypertrophy, as in the adult population.20 Neural adaptations, such as increased motor unit activation and improved motor unit coordination, are primarily responsible for strength gains in children.21–22 Quadriceps atrophy is common after ACL reconstruction and return of muscle function and strength is an essential component of rehabilitation. Although the mechanism for strength increase in children may be different, this case demonstrates full return of quadriceps strength was achieved within 6 months of surgery. This is consistent with findings of prior studies within a teenage population,23 however future research is needed to determine if the rate and magnitude of strength return is the same for the pediatric population.
Several emotional and behavioral factors make the rehabilitation of pediatric or adolescent patients following physeal sparing ACL reconstruction challenging to physical therapists responsible for their successful outcomes.3,9 Although pediatric specialists are well aware of these factors and well versed in coping with them, the authors have found that many children who receive physeal sparing ACL-R are being rehabilitated in classically adult physical therapy settings. Therefore the therapist treating this population, unfamiliar with these factors, may need additional guidance and assistance.
The level of emotional maturity in pediatric patients undergoing physeal sparing ACL-R must be considered as a factor during the decision making process of choosing surgical versus nonsurgical management. The parents, surgeon, and therapist must work together with the patient, to decide if the patient is mature enough to comply safely with the post-operative restrictions and motivated enough to work toward a successful outcome. Currently, this is a highly subjective process and the authors are not aware of any objective measures available to guide this decision making process. The authors currently utilize a team approach that encompasses parental opinion and observational opinion from different practitioners during physician office visits and pre-operative therapy education training. This way the team can judge in different environments and at different snapshots in time, whether the child possesses the proper level of maturity to achieve successful rehabilitation.
Maturity level also impacts rehabilitation for this population during the decision making process to discontinue use of the post-operative brace. In adult ACL-R rehabilitation the decision to discontinue the use of a brace is based solely upon physiological characteristics such as graft integrity, quadriceps function, range of motion, and gait characteristics. In the rehabilitation of the child with ACL-R, the therapist must also consider other extrinsic factors as well. In this case, the patient was allowed to discontinue use of the post-operative brace earlier at home, but he was required to continue with use at school and while in public. This was done for safety considerations. It was felt that keeping the brace on in school would decrease the chances of injury from patient participation in horse-play or careless behavior on the part of his classmates. His classmates may not have remembered that the patient just had surgery without the reminder of him wearing the brace. In this way, the maturity level of not only the patient, but his peers as well, has an impact on the overall rehabilitation scheme.
ACL-R rehabilitation requires a level of dedication and commitment that can prove challenging for even the most dedicated and mature athletes. Pediatric patients participating in rehabilitation after physeal sparing ACL-R will require the therapist to be dynamic and flexible in their approach to treatment. It is important to keep the patient actively engaged in all activities while ensuring that the activity remains fresh and fun. Maintaining motivation over time can be important in enabling them to maximize their physical potential.3
Parental post-operative education is one aspect of complete care that cannot be neglected. Parents must be educated in realistic expectations of the rehabilitation process in order to prevent unnecessary patient directed stress during recovery. At the author's facility, we have occasionally seen issues arise when parents base their expectation of rehabilitation on what they see in the media about professional athletes and recovery from ACL-R. Parents can sometimes place undue pressure on the child to recover or perform. This could lead to poor outcomes or actually delayed recovery. Being aware of this possibility and addressing parent questions early is a key factor to avoiding this scenario.
While the physical therapist and parent must be knowledgeable about activity restrictions after ACL-R, it is also very important to understand what type of activities are permissible. It is important for children to have an outlet for energy, creativity, and play. Post-operative restrictions can impact many aspects of the child's life and restoring some type of activity balance is essential for emotional and psychological wellbeing. Birthday parties, school recess, family vacations and amuse-ment parks are some situations commonly faced by the pediatric sports medicine specialist. Parents and patients rely on the expertise of the physical therapist for recommendations that will allow the child the satisfaction of participation, but at the same time limiting risk of injury or rehabilitation complications.
CONCLUSION
The management of skeletally immature children with knee instability due to ACL rupture is evolving towards earlier ACL reconstruction.4 There are adverse effects associated with delaying surgical reconstruction until the patient is skeletally mature and advances in surgical techniques allow for anatomical ACL-R in the skeletally immature athlete while minimizing the risk of premature physeal closure.4–7,17,24 The rehabilitation progression in this population has some differences from traditional ACL rehabilitation programs for adults due to behavioral and physiological characteristics. Due to the lack of rehabilitation based outcome studies in the literature, the current timeline of rehabilitation progression is largely based upon integration of known ACL healing characteristics in the adult population and surgeon expertise. Future research is needed to identify the time line and magnitude of strength return, if functional performance measures used in adult ACL-R are appropriate in the skeletally immature and if so, what is the normal performance in this population. Additionally, long term objective outcome studies are necessary to determine percentage of patients that achieve successful outcomes over time.
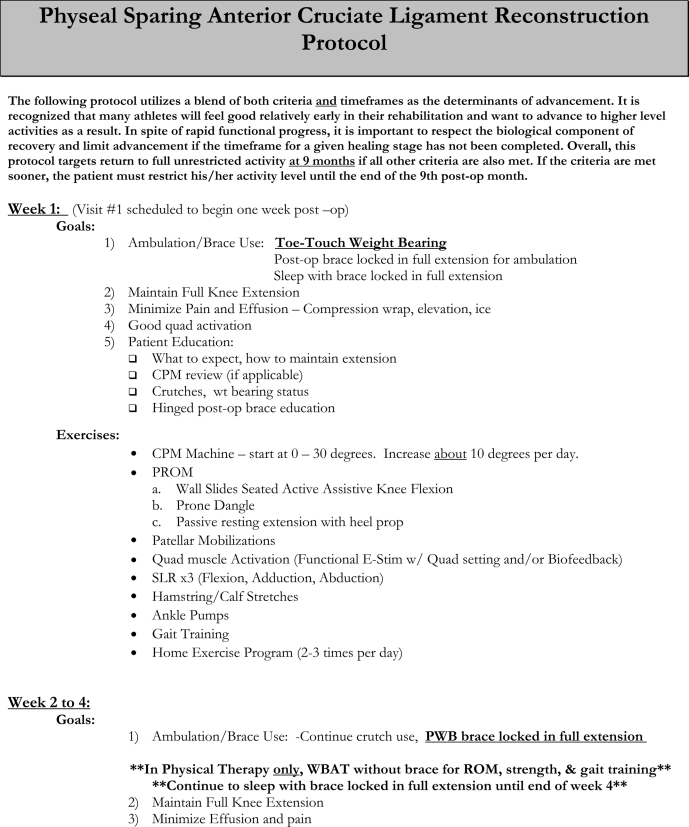
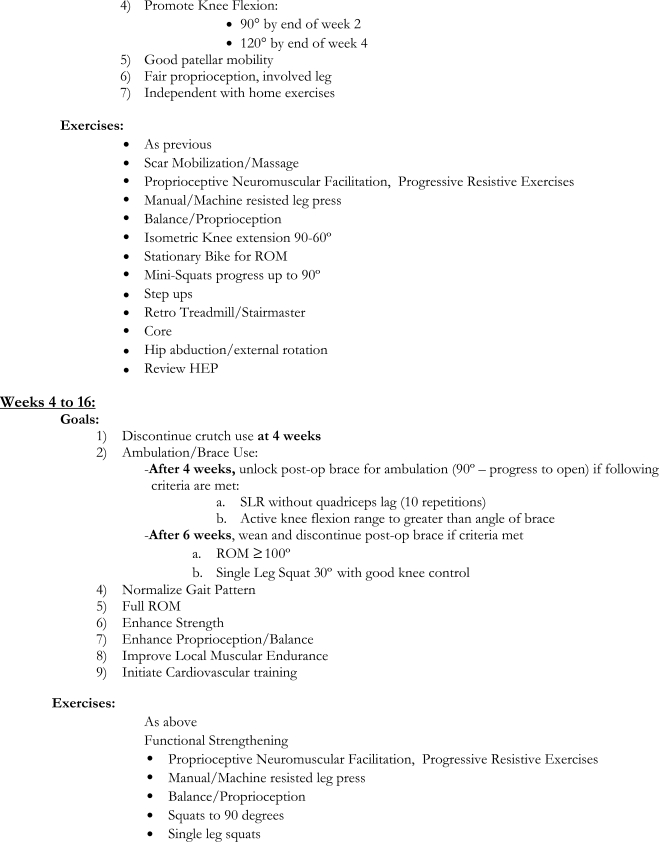
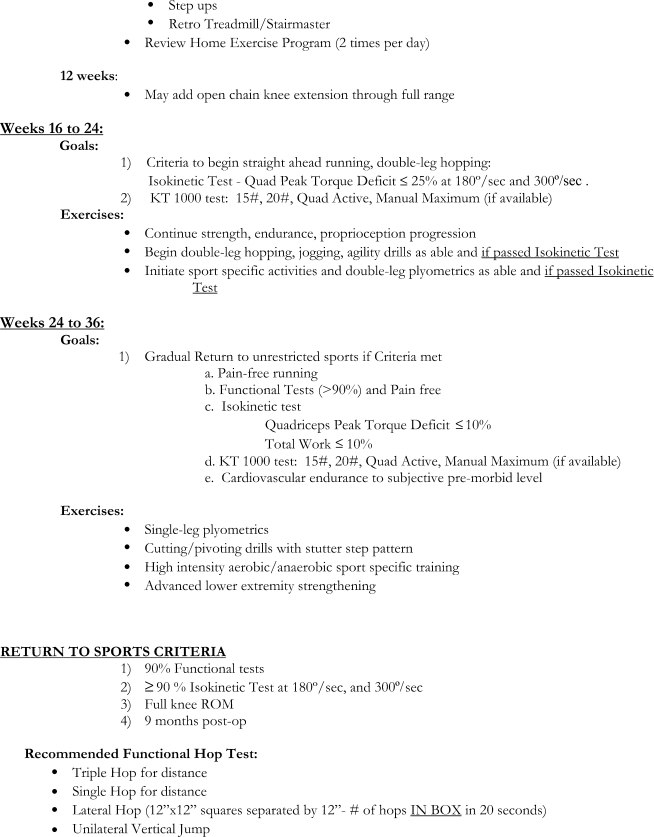
APPENDIX 1
References
- 1.Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. Nov 2005;87(11):2371–2379 [DOI] [PubMed] [Google Scholar]
- 2.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop. Jul-Aug 2002;22(4):452–457 [PubMed] [Google Scholar]
- 3.Wojtys EM, Brower AM. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. Sep-Oct 2010;45(5):509–512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy. May 2011;27(5):704–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohtadi N, Grant J. Managing anterior cruciate ligament deficiency in the skeletally immature individual: a systematic review of the literature. Clin J Sport Med. Nov 2006;16(6):457–464 [DOI] [PubMed] [Google Scholar]
- 6.Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg Br. Jan 2002;84(1):38–41 [DOI] [PubMed] [Google Scholar]
- 7.Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8(2):229–233 [DOI] [PubMed] [Google Scholar]
- 8.Lawrence JTR, Agrawal N, Ganley TJ. Degeneration of the Knee Joint in Skeletally Immature Patients With a Diagnosis of an Anterior Cruciate Ligament Tear: Is There Harm in Delay of Treatment? Am J of Sports Med. 2011;39(12):2582–2587 [DOI] [PubMed] [Google Scholar]
- 9.Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res. Jul 2010;468(7):1971–1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinton RY, Sharma KM. Anterior Cruciate Ligament Injuries. In: Micheli LJ, Kocher MS, eds. The Pediatric and Adolescent Knee. Philadelphia: Saunders Elsevier; 2006:317–376 [Google Scholar]
- 11.Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. Jan 1963;45-A:1–14 [PubMed] [Google Scholar]
- 12.Kocher MS, Hovis WD, Curtin MJ, Hawkins RJ. Anterior cruciate ligament reconstruction in skeletally immature knees: an anatomical study. Am J Orthop (Belle Mead NJ). Jun 2005;34(6):285–290 [PubMed] [Google Scholar]
- 13.Behr CT, Potter HG, Paletta GA., Jr. The relationship of the femoral origin of the anterior cruciate ligament and the distal femoral physeal plate in the skeletally immature knee. An anatomic study. Am J Sports Med. Nov-Dec 2001;29(6):781–787 [DOI] [PubMed] [Google Scholar]
- 14.Barber SD, Noyes FR, Mangine R, DeMaio M. Rehabilitation after ACL reconstruction: function testing. Orthopedics. Aug 1992;15(8):969–974 [DOI] [PubMed] [Google Scholar]
- 15.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. Aug 1994;20(2):60–73 [DOI] [PubMed] [Google Scholar]
- 16.Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. Apr 2010;40(4):A1–A37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCarroll JR, Rettig AC, Shelbourne KD. Anterior cruciate ligament injuries in the young athlete with open physes. Am J Sports Med. Jan-Feb 1988;16(1): 44–47 [DOI] [PubMed] [Google Scholar]
- 18.Bonnard C, Fournier J, Babusiaux D, Planchenault M, Bergerault F, de Courtivron B. Physeal-sparing reconstruction of anterior cruciate ligament tears in children: results of 57 cases using patellar tendon. J Bone Joint Surg Br. Apr 2011;93(4):542–547 [DOI] [PubMed] [Google Scholar]
- 19.Kocher M, et al. Reliability, Validity and Responsivement of a Modified International Knee Documentation Committee Subjective Knee Form in Children With Knee Disorders. Am Jour of Sport Med. 2011;39(5):933–939 [DOI] [PubMed] [Google Scholar]
- 20.Guy JA, Micheli LJ. Strength training for children and adolescents. J Am Acad Orthop Surg. Jan-Feb 2001;9(1):29–36 [DOI] [PubMed] [Google Scholar]
- 21.Ozmun JC, Mikesky AE, Surburg PR. Neuromuscular adaptations following prepubescent strength training. Med Sci Sports Exerc. Apr 1994;26(4):510–514 [PubMed] [Google Scholar]
- 22.Ramsay JA, Blimkie CJ, Smith K, Garner S, MacDougall JD, Sale DG. Strength training effects in prepubescent boys. Med Sci Sports Exerc. Oct 1990;22(5):605–614 [DOI] [PubMed] [Google Scholar]
- 23.Wells L, Dyke JA, Albaugh J, Ganley T. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. Jul-Aug 2009;29(5):486–489 [DOI] [PubMed] [Google Scholar]
- 24.Mizuta H, Kubota K, Shiraishi M, Otsuka Y, Nagamoto N, Takagi K. The conservative treatment of complete tears of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg Br. Nov 1995;77(6):890–894 [PubMed] [Google Scholar]