Abstract
Advancements towards an improved vaccine against Bacillus anthracis, the causative agent of anthrax, have focused on formulations composed of the protective antigen (PA) adsorbed to aluminum hydroxide. However, due to the labile nature of PA, antigen stability is a primary concern for vaccine development. Thus, there is a need for a delivery system capable of preserving the immunogenicity of PA through all the steps of vaccine fabrication, storage, and administration. In this work, we demonstrate that biodegradable amphiphilic polyanhydride nanoparticles, which have previously been shown to provide controlled antigen delivery, antigen stability, immune modulation, and protection in a single dose against a pathogenic challenge, can stabilize and release functional PA. These nanoparticles demonstrated polymer hydrophobicity-dependent preservation of the biological function of PA upon encapsulation, storage (over extended times and elevated temperatures), and release. Specifically, fabrication of amphiphilic polyanhydride nanoparticles composed of 1,6-bis(p-carboxyphenoxy)hexane and 1,8-bis(p-carboxyphenoxy)-3,6-dioxaoctane best preserved PA functionality. These studies demonstrate the versatility and superiority of amphiphilic nanoparticles as vaccine delivery vehicles suitable for long-term storage.
Keywords: Protective antigen for anthrax, protein stability, polyanhydrides, nanoparticles
Introduction
Anthrax is a significant public health concern due to its potential as a bioterrorism and biowarfare agent. Use of the currently licensed alum-adjuvanted anthrax vaccine adsorbed (AVA) poses many concerns due to its high reactogenicity, multi-dose (five) immunization schedule followed by yearly boosters, and painful side effects1. The recombinant protective antigen (PA) from Bacillus anthracis, the key element of the AVA vaccine that confers immunity against an anthrax infection, has been the focus for new vaccines2. PA is the receptor-binding subunit for both lethal factor (LF) and edema factor (EF), which upon binding, lead to the formation of lethal toxin (LT) and edema toxin (ET), respectively3. Although highly immunogenic, PA is unfortunately a labile recombinant protein, especially in low pH and high temperature environments4–7. These stability concerns have led to manufacturing roadblocks during a Phase I clinical trial for a new anthrax vaccine based on PA8.
In addition to stability concerns during the vaccine manufacturing process, there are other obstacles for PA-based vaccines. PA circulating in the blood stream is eliminated within six hours;3, 9 this limited in vivo half-life may fail to induce a protective immune response. Studies by Zinkernagel and others have shown that antigen persistence is a key element associated with the development of a protective immune response10, 11. Several methods have been employed to increase PA availability to the immune system and improve its immunogenicity, including engineering recombinant PA, incorporating other antigens or adjuvants in the vaccine, evaluating alternate delivery routes, and using controlled delivery systems3. Currently, the AVA vaccine is administered intramuscularly and many murine studies have focused on subcutaneous delivery of PA. As an alternative, intranasal vaccination has been reported as the best route for induction of a protective immune response3, 12. While PA is a relatively good immunogen, it may be essential to use an adjuvant; however, well known mucosal adjuvants (e.g., cholera, pertussis, and edema toxins and CpG DNA) have limitations due to their potential toxicity when delivered by this route in humans3, 13.
This work focuses on the development and refinement of a controlled delivery system for PA based on biodegradable polyanhydride nanoparticles. Polyanhydrides are a class of biomaterials with excellent biocompatibility and have been extensively studied as vaccine delivery vehicles and adjuvants14–19. These polymer formulations provide safe parenteral delivery20, enhanced adjuvanticity16, 17, 21, sustained release of encapsulated antigens22–28, and a stabilizing environment for protein antigens during fabrication, storage, and release22–26, 28–30. Specifically, micro- and nanoparticles made of copolymers based upon sebacic anhydride (SA), 1,6-bis(p-carboxyphenoxy)hexane (CPH), and 1,8-bis(p-carboxyphenoxy)-3,6-dioxaoctane (CPTEG) are suitable for inhalation or injection. Moreover, they possess tunable antigen release kinetics22–28, 30 that provide an in vivo antigen depot, thereby allowing for sustained antigen exposure and eliminating the need for multiple administrations. These surface eroding polymers slowly release encapsulated antigen, minimizing exposure to unfavorable aqueous environments.
The overall goal of this work was to design nanoparticle-based formulations capable of encapsulating and releasing biologically functional PA that results in a robust, high avidity, neutralizing antibody response after a single administration. In this regard, nanoparticles based on 50:50 CPTEG:CPH, 20:80 CPTEG:CPH, 50:50 CPH:SA, and 20:80 CPH:SA were investigated for their ability to stabilize and release biologically active and immunogenic PA. In contrast to CPH:SA nanoparticles, amphiphilic CPTEG:CPH nanoparticles better preserved the functionality and immunogenicity of PA during nanoparticle fabrication, storage, and release. The use of amphiphilic polyanhydride nanoparticles as delivery vehicles presents a viable solution for long-term vaccine storage.
Experimental Section
Materials
Chemicals needed for polymerization, nanoparticle fabrication, and buffer preparation included acetic anhydride, chloroform, methylene chloride, petroleum ether, pentane, monobasic potassium phosphate, and dibasic potassium phosphate; all were purchased from Fisher Scientific (Fairlawn, NJ). Monomer synthesis utilized the following chemicals: 1,6-dibromohexane, tri-ethylene glycol, 4-hydroxybenzoic acid, and 1-methyl-2-pyrrolidinone; these were purchased from Sigma Aldrich (St. Louis, MO); 4-p-fluorobenzonitrile was purchased from Apollo Scientific (Cheshire, UK); and sulfuric acid, acetonitrile, dimethyl formamide, toluene, and potassium carbonate were obtained from Fisher Scientific. Deuterated chemicals for NMR (nuclear magnetic resonance) analysis, chloroform and dimethyl sulfoxide were purchased from Cambridge Isotope Laboratories (Andover, MA).
Polymer synthesis, nanoparticle fabrication, protein encapsulation, and characterization
The CPH and CPTEG monomers were synthesized as described previously31, 32. The SA monomer was purchased from Sigma Aldrich (St. Louis, MO). Pre-polymer and polymers were synthesized as described before28, 33. The CPTEG:CPH and CPH:SA copolymers were formed into nanoparticles as described previously17, 27, 29. Briefly, PA (NIH Biodefense and Emerging Infections Research Resources Repository, Manassas, VA) loaded nanoparticles (2% (w/w)) were fabricated by dissolving the desired polymer in methylene chloride at a concentration of 25 mg/mL. The desired amount of lyophilized PA was added to the dissolved polymer, the solution sonicated (40 Hz for 30 s), poured into a non-solvent (pentane) at a solvent to non-solvent ratio of 1 to 200, and then vacuum filtered to recover the PA-loaded nanoparticles (20–150 mg batch size). Polymer molecular mass, chemical structure, and chemical composition were determined with 1H NMR spectroscopy using a Varian VXR 300 MHz spectrometer (Varian Inc., Palo Alto, CA). Specifically, the molecular mass was determined by end group analysis of NMR spectra. Nanoparticle size and morphology were characterized with scanning electron microscopy (SEM; JEOL 840 A, JEOL Peabody, MA).
In vitro protein release kinetics
PA-loaded nanoparticles at a concentration of approximately 50 mg/mL were incubated with 0.1 M PBS buffer (pH 7.4) in capped microcentrifuge tubes. Samples were sonicated to ensure uniform nanoparticle distribution and placed in a shaker/incubator at 37°C. Sample supernatants were removed (entire volume) incrementally to measure the amount of released PA (PArel), which was analyzed using a micro-bicinchoninic acid (BCA) assay. Once supernatants were removed, equivalent volumes of PBS buffer were added back to maintain perfect sink conditions. Data is presented as cumulative percentage of PA released, which was determined by normalizing the cumulative amount released at each time point by the total amount encapsulated into the nanoparticles22–28, 30.
In vitro pH change upon nanoparticle degradation
Blank nanoparticles at a concentration of approximately 100 mg/mL were incubated with 0.1 M PBS buffer (pH 7.6) in microcentrifuge tubes. Samples were sonicated to ensure uniform nanoparticle distribution and placed in a shaker/incubator at 37°C. The pH measurements were carried out at various time points with a pH probe to monitor the buildup of acidic degradation products.
In vitro release of PA for analysis of bioactivity, antigenicity, and structure
Treatment groups tested for their effect on PA stability were 20:80 CPTEG:CPH, 50:50 CPTEG:CPH, 20:80 CPH:SA, and 50:50 CPH:SA nanoparticles, native PA (i.e., positive control stored at −20°C), and protein exposed to nanoparticle fabrication conditions (NFC) which included sonication (40 Hz for 30 s), solvent exposure (methylene chloride and pentane), and vacuum drying. All groups were sonicated and incubated with 0.1 M PBS buffer (pH 7.4) in microcentrifuge tubes in a shaker/incubator at 37°C. In order to accumulate enough of the PArel for characterization, PA-loaded nanoparticles were incubated for two days. Following release, supernatants were removed and the concentration, antigenicity, bioactivity, and structural alterations of the PArel were assessed.
Circular dichroism: secondary structure
Far UV circular dichroism (CD) (190–250 nm) was used to study the changes in protein secondary structure of the PArel. All CD spectra were collected for samples on a Jasco J-170 Spectropolarimeter (Easton, MD). The emission spectrum from 200–260 nm was analyzed for shifts in molar ellipticity and wavelength, which are indicative of alterations in protein secondary structure. The experiments were performed in triplicate using a 200 μL sample volume.
Fluorescence spectroscopy: tertiary structure
Fluorescence spectroscopy was used to study the changes in tertiary structure of the PArel with a Cary Eclipse fluorescence spectrometer (Varian, Inc., Palo Alto, CA). Samples were excited at a wavelength of 280 nm and a voltage of 800 V, which resulted in an emission spectrum that corresponds to the tryptophan and tyrosine residues of the protein. The emission spectrum from 300–500 nm was analyzed for shifts in peak intensity and wavelength that are indicative of alterations in protein tertiary structure. The experiments were performed in triplicate.
In vitro release of PA for in vivo administration of the PArel
PA-loaded nanoparticle (2% w/w) samples (200 mg) were incubated in 0.1 M PBS (pH 7.4) for 14 days at 4°C in dialysis cassettes (4,000 Da MWCO) to accumulate enough of the PArel for immunization. This release was carried out at 4°C to prevent temperature induced instability. Protein concentration was determined with a micro-BCA assay and all samples were adjusted to a final concentration of 200 μg/mL. Equal amounts of PA released from 20:80 CPTEG:CPH, 50:50 CPTEG:CPH, 20:80 CPH:SA, and 50:50 CPH:SA nanoparticles and native PA were adsorbed to Imject Alum (Fisher Scientific). A/J mice (Jackson Laboratories, Bar Harbor, Maine) were immunized subcutaneously in the nape of the neck with a dose of 10 μg of the PArel or native PA (3 or 4 mice per group). Each mouse was given a second immunization on day 15 with 10 μg of the PArel or native PA corresponding to the primary immunization regimen, euthanized on day 21, and serum collected. All animal procedures were conducted with the approval of the Iowa State University Institutional Animal Care and Use Committee.
Enzyme-linked immunosorbent assay (ELISA): PA-specific serum antibody response
PA-specific serum antibody response (total IgG [H+L]) and PArel antigenicity were analyzed via ELISA using a previously described method with modifications19. High-binding 96 well ELISA plates (Fisher Scientific) were coated in PBS buffer (pH 7.2, 0.05M) with 0.5 μg/mL native PA or PArel overnight at 4°C. After washing with buffer (PBS containing 0.5% Tween 20 (PBS-T)), plates were blocked for 2 h (PBS containing 0.5 % Tween 20 (PBS-T) and 2% gelatin) at room temperature, washed three times in PBS-T, and incubated with mouse serum (from individual mice, not pooled) for 24 h at dilutions from 1:1,000 to 1:1,000,000 overnight at 4°C. The following day, plates were washed three times in PBS-T, incubated with alkaline phosphatase-conjugated goat anti- IgG [H+L] antibody (Jackson ImmunoResearch Laboratories, West Grove, PA) for 2 h at room temperature, washed again, and incubated with alkaline phosphatase substrate buffer (Sigma Aldrich) for 2 h at room temperature. Absorbance was measured at an optical density (OD) of 405 nm using a Spectramax 190 Plate Reader (Molecular Devices, Sunnyvale, CA). Each sample was analyzed in triplicate.
ELISA for serum antibody avidity
Serum antibody avidity was determined by modifying an ELISA method described previously19. The avidity assay was performed similarly to the serum antibody response protocol described above. Following serum incubation for 24 h at a dilution of 1:1,000,000, the chaotropic agent, sodium thiocyanate, was added to the wells using incremental increases over a concentration range from 0 to 5 M. Plates were incubated for 20 min at room temperature and then washed four times in PBS-T. The detection of bound serum antibody was performed as described above. Relative avidity index is defined as the concentration of sodium thiocyanate required to decrease the optical density by 50% of that obtained for each control well (i.e., no sodium thiocyanate). Antibody titers were too low to measure the avidity of the antibody response for serum samples obtained from mice immunized with PA released from the CPH:SA nanoparticles.
Lethal toxin in vitro cytotoxicity assay
The lethal toxin in vitro cytotoxicity assay was modified from a previously described method6. The murine macrophage-like cell line RAW 264.7 obtained from ATCC (Manassas, VA) was maintained in culture at 37°C in a 5% CO2 humidity using high glucose DMEM medium (Invitrogen, Carlsbad, CA) supplemented with 10% heat-inactivated FBS (Valley Biomedical, Winchester, VA), 100 IU/ml penicillin and 10 μg/ml streptomycin (Mediatech, Herndon, VA). For the lethal toxin in vitro cytotoxicity assay, RAW cells were transferred to a 96-well plate (100,000 cells per well) grown to approximately 90% confluency in 100 μL medium over two days. Approximately 12 μL of each treatment (PArel, PA-loaded nanoparticles, blank nanoparticle controls, medium only control (negative control and 100% cell survival), native PA (positive control and 100% cell death), LF (NIH Biodefense and Emerging Infections Research Resources Repository, Manassas, VA) control, and cell lysis buffer) diluted in RAW medium were added to the cells with 0.3 μg/mL LF for no more than 6 h. The amount of PA released from the nanoparticles was calculated from the release curve in Figure 1. This assay was also utilized to investigate antibody neutralization and shelf life (i.e., PA stability) of the PA-loaded nanoparticles. For antibody neutralization assessment, individual serum samples (dilutions ranging from 1:100 to 1:204800) from the different immunized mouse groups (described in the in vitro release of PA for in vivo administration of the PArel section) were added to the cells along with native PA (0.8 μg/mL) and LF (0.3 μg/mL). For antibody neutralization assessment, the positive control was medium only (100% cell survival) and the negative control was native PA (100% cell death). Samples were then allowed to incubate for up to 6 h, after which the CellTiter 96® Non-Radioactive Cell Proliferation Assay (MTT) (Promega, Madison, WI) was used to determine cell viability. Optical density (OD) was measured at 570 nm with a background (690 nm) subtraction as recommended by the manufacturer’s protocol. Antibody neutralization was considered significant when measured OD values fell below 50% of the positive control OD value. Data are presented as % residual activity, as determined by Equation 1:
| Eq. 1 |
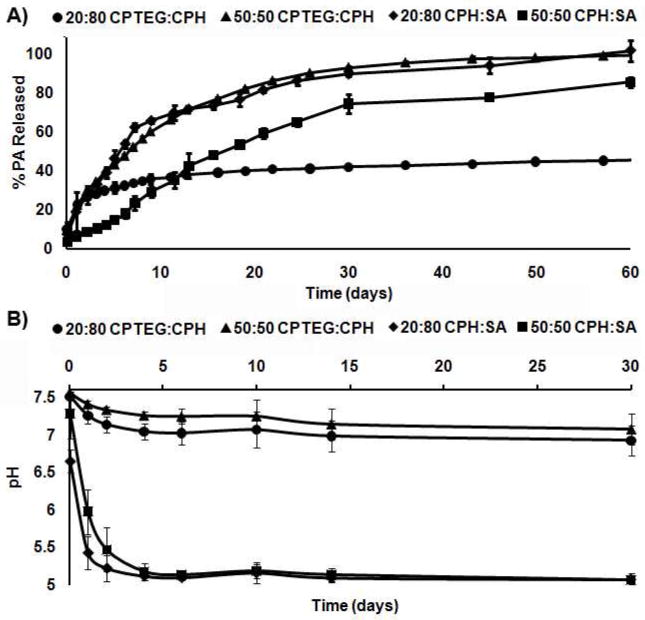
Figure 1.
PA was released from polyanhydride nanoparticles in a chemistry dependent manner. A) Release of PA from polyanhydride nanoparticles over 60 days and B) the change in pH of PBS buffer (pH 7.6, 0.1 M) from nanoparticle degradation over 30 days. Error bars represent standard deviation of three replicates performed in three independent experiments.
Thermal stability of stored dry powder PA-loaded nanoparticle formulations
Bioactivity was tested with the lethal toxin in vitro cytotoxicity assay6 to determine the ability of each formulation to preserve and release active PA. The thermal stability upon storage was studied in formulations that included PA loaded into the nanoparticles (dry) (labeled by polymer chemistry), PA dissolved in PBS buffer (labeled “PBS”), or PA absorbed to alum (labeled “Alum”). All formulations were stored under desiccant at four different temperatures, 40, 25, 4, and −20°C, for four months. Following storage, the formulations were tested at prescribed times for their ability to preserve PA activity using the lethal toxin in vitro cytotoxicity assay as described previously6. PA-loaded nanoparticle bioactivity was evaluated at a concentration of 125 μg/mL for 6 h. This nanoparticle dose was chosen because after 6 h of release (assay incubation time) the resultant PA concentration was the same as that administered in the positive control (i.e. 0.8 μg/mL native PA). It is important to note that nanoparticle formulations investigated in this study were stored dry and were not added to aqueous buffers or medium until initiation of the cytotoxicity study, which lasted for 6 h. This is in contrast to the PA controls (i.e., PBS and Alum), which were stored in solution to mimic the current storage strategy of the AVA vaccine. The nanoparticle storage conditions in this study are distinctly different from those in the studies investigating PA release, activity, structure, antigenicity, and immunogenicity (Figures 1–4) in which the nanoparticles were incubated in an aqueous environment for extended time periods (see previous methods) to enable sufficient release of the encapsulated protein.
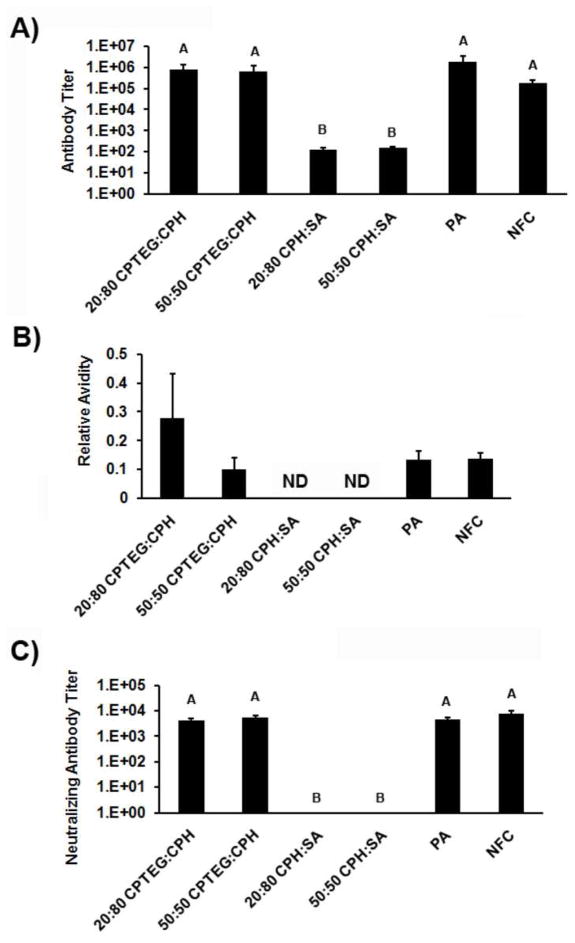
Figure 4.
Mice immunized with PA released from 50:50 and 20:80 CPTEG:CPH, adjuvanted with alum, developed the highest antibody titers, the most avid antibody response, and highest neutralizing antibody titers. A) Antibody titers, B) antibody avidity (ND (not determined) for 20:80 and 50:50 CPH:SA because antibody titers were too low), and C) antibody neutralization titers of serum samples from immunized mice. Data is presented as the mean ± SEM of three replicates. All serum samples were evaluated individually. Treatments with different letters are significantly different from one another at p < 0.0001.
Statistical analysis
Statistical analyses performed using JMP® 7 (Cary, NC) and comparisons between treatments were made with Tukey’s HSD (Honestly Significant Difference) to determine statistical significance and p-values ≤ 0.05 were considered significant.
Results
Polymer and nanoparticle characterization
Consistent with previous work, polymer characterization by 1H NMR indicated that the polymer molecular weights were within the desired ranges of 9,000–15,000 Da31, 33, 34. The structure and composition of the polymers were also confirmed using NMR. SEM images (data not shown) indicated that protein-loaded and blank nanoparticles resulted in similar size (212 ± 43 nm) and morphology as previously reported16, 19, 27, 29, 35. Particle yield was approximately 80% (recovery after filtration).
In vitro PA release and pH of nanoparticle degradation were dictated by chemistry
Release of PA and change in pH due to nanoparticle degradation were evaluated as a function of time. As shown in Figure 1, polymer chemistry-dependent protein release kinetics and buffer acidification were observed. Increasing the content of SA or CPTEG relative to the CPH content resulted in a more rapid release of encapsulated PA (Figure 1A). The 20:80 CPTEG:CPH particles provided the slowest PA release profile. This is consistent with previously published studies demonstrating chemistry-dependent release profiles of other proteins from polyanhydride nanoparticles22–25, 27, 28, 30, 36. The effect of the polymer chemistry is also reflected in the pH profile of the degrading nanoparticles, as shown in Figure 1B. The acidic monomers produced from the degradation of CPH:SA nanoparticles have been shown to be water soluble25 and result in a greater decrease in pH (ΔpH = 2.5) as compared to that of the CPTEG:CPH monomers (ΔpH = 0.6). In these experiments, an even greater pH decrease (ΔpH = 5.0) was observed upon degradation of poly(lactic-co-glycolic acid) (PLGA) nanoparticles (data not shown).
Protein activity and structural stability were preserved by amphiphilic CPTEG:CPH nanoparticles
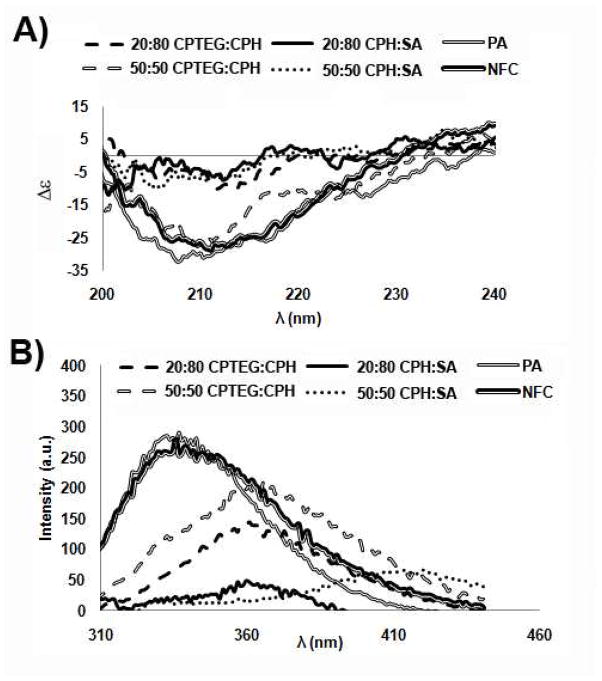
To evaluate PA stability upon release from nanoparticles, a detailed structural evaluation of the PArel was performed (Figure 2). In this study, we analyzed the structural integrity of the PArel that accumulated over 48 h. During this time, the protein was continually exposed to the acidic microenvironments caused by the degradation of the polymers in an aqueous environment. The CD spectrum for native PA revealed a minimum at approximately 208–210 nm and a shoulder at 215–217 nm (Figure 2A). These findings were consistent with the known CD spectra reported previously for the secondary structure of PA, and indicate that PA consists mainly of a mixture of α-helices and β-sheets6, 37. Only the PA exposed to NFC or released from 50:50 CPTEG:CPH nanoparticle formulations maintained the native secondary structure (Figure 2A). PA released from all other formulations (20:80 CPTEG:CPH, 20:80 CPH:SA, and 50:50 CPH:SA) resulted in a significant increase in molar ellipticity (Δε), indicating a loss of secondary structure.
Figure 2.
50:50 CPTEG:CPH best preserved the structural integrity of PA while CPH:SA nanoparticle chemistries cause a loss in secondary and tertiary structural integrity. A) Secondary structure as measured by circular dichroism (CD) and B) tertiary structure as measured by fluorescence spectroscopy after two days of release from polyanhydride nanoparticles.
Tertiary structure analysis, performed with fluorescence spectroscopy, revealed a red shift in peak position for the PA released from all the nanoparticle formulations (Figure 2B). This peak shift indicates exposure to a more polar environment indicative of protein unfolding6. However, PA peak intensity was best preserved by encapsulation into and release from the amphiphilic 50:50 CPTEG:CPH nanoparticles and to a lesser extent by encapsulation into and release from 20:80 CPTEG:CPH nanoparticles. The nanoparticle fabrication conditions appeared to have no detrimental effects on the tertiary structure of PA. In contrast, the encapsulation of PA into and release from CPH:SA formulations resulted in a loss of tertiary structure.
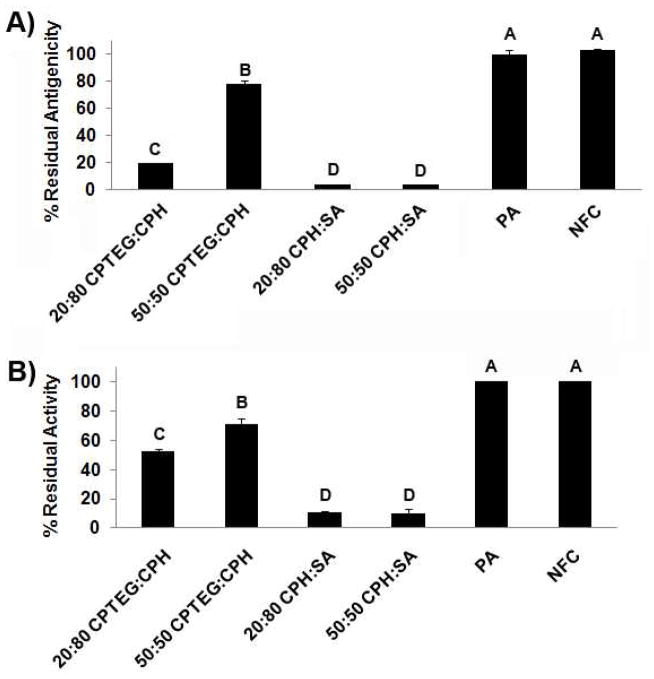
Following the structural evaluation, the relative antigenicity and bioactivity were assessed for the PArel. The results of this study, which were used to identify lead candidate formulations for stabilizing PA, are summarized in Figure 3. PA released from amphiphilic 50:50 CPTEG:CPH nanoparticles retained almost 80% of its antigenicity (Figure 3A) and functional activity (Figure 3B). PA released from 20:80 CPTEG:CPH nanoparticles retained 52% of its activity but only 20% of its antigenicity, while CPH:SA-containing nanoparticles preserved very little PA activity and antigenicity. Nanoparticle fabrication conditions had little or no detrimental effect on the antigenicity or activity of PA (Figure 3).
Figure 3.
CPTEG:CPH nanoparticle chemistries released biologically active and antigenic PA. A) Residual antigenicity and B) residual activity of PA after two days of release from polyanhydride nanoparticles. The direct ELISA was performed with 0.5 μg/mL PArel from the nanoparticles. The biological assay was performed by incubating 6.4 μg/mL PArel from polyanhydride nanoparticles with 0.3 μg/mL LF with RAW cells for 6 h. Error bars represent standard deviation of 3 replicates. Treatments with different letters are significantly different from one another at p < 0.05.
In vivo immunization with the PA released from amphiphilic CPTEG:CPH nanoparticles resulted in high titer, high avidity, neutralizing antibody
Upon completion of the structural, antigenicity and bioactivity studies, it was hypothesized that the amphiphilic CPTEG:CPH nanoparticles would be the most viable candidates for preserving the PArel, thus enabling a primed PA-specific antibody response when administered in vivo. In order to determine the immunogenicity of the released protein, separate groups of mice were immunized with alum adjuvanted PArel from the four nanoparticle formulations. We hypothesized that if PA was degraded upon release from a particular nanoparticle formulation, as seen for the PA released from the CPH:SA nanoparticle chemistries (Figures 2 and 3), there would be a loss in the immunogenicity of the PA. Antibody responses induced by the released protein were characterized in terms of titer (Figure 4A), relative avidity (Figure 4B), and neutralizing antibody titer (Figure 4C). The data indicated that the PA released from CPH:SA nanoparticles induced a weak humoral response, while the PA released from the CPTEG:CPH nanoparticles or PA exposed to the nanoparticle fabrication conditions resulted in the induction of high titer and avid antibody responses that were statistically similar to those induced by native PA. Overall, these data indicate that the immunogenicity of PA released from the amphiphilic CPTEG:CPH nanoparticles was better preserved than that of PA released from CPH:SA nanoparticles, as evidenced by the 4 log10 difference in antibody titer.
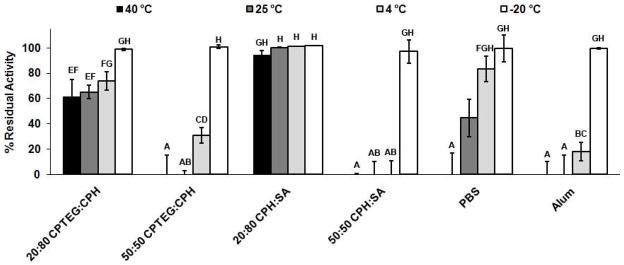
Shelf life stability of PA encapsulated into 50:50 CPTEG:CPH, 20:80 CPTEG:CPH, and 20:80 CPH:SA was superior to that of PA conjugated to alum
The ability of a PA-based vaccine to retain full immunogenicity upon storage is a major concern. As a measure of PA stability, an in vitro cytotoxicity assay was employed to assess the preservation of the biological activity of PA upon storage and immediate release from polyanhydride nanoparticles. This study was also an assessment of the thermal stability of the nanoparticles at various temperatures. During optimization of the cytotoxicity assay, we determined that co-incubating 125 μg/mL of 0.8% PA-loaded nanoparticles for 6 h with RAW 264.7 cells resulted in a concentration of PArel that was equivalent to that of the positive control (i.e., 0.8μg/mL native PA). Because there was no statistical difference in the amount of PA released between the different nanoparticle chemistries in the first 6 h (Figure 1), direct comparisons between the various polyanhydride formulations can be made. In this study, the shelf life storage capabilities of i) PA loaded into polyanhydride nanoparticles (dry), ii) PA in PBS buffer (pH 7.6), or iii) PA adsorbed to alum were investigated at multiple time points following storage at 40, 25, 4, and −20°C. It is known that adjuvant solutions containing alum have acidic bulk conditions (pH = 5.6)38, so a PBS buffer group was included to investigate the effect of storage temperature at a neutral pH on the bioactivity of PA.
In order to assess the preservation of the biological activity after dry storage for the desired amount of time (1, 7, 14, 30, 60, and 120 days – only long term data are presented in this manuscript), PA-loaded nanoparticles were directly applied to cultures of RAW 264.7 cells at the initiation of a lethal toxin cytotoxicity assay. By employing these assay conditions, any of the PArel was immediately available to bind to the host cell receptor, thus avoiding any detrimental effects of accumulated acidic degradation products on the PArel. This is an important difference between these studies and the stability studies described in Figures 2–4 in which the PArel was accumulated over several days in an aqueous environment before assessing structural and antigenic integrity, and biological activity. After one week of storage at 40°C, the biological activity of PA adsorbed to alum and PA stored in PBS buffer was undetectable (Supplementary Figures 2A and B). Following two weeks and four months of storage at 25°C, PA adsorbed to alum and PBS retained only half of its original bioactivity respectively. After one month at 25°C, PA absorbed to alum lost all of its bioactivity (Supplementary Figure 2A). After two months of storage at 40°C, PA encapsulated into 20:80 and 50:50 CPTEG:CPH or 20:80 CPH:SA nanoparticles retained from 60 to 90% of its biological activity (Supplementary Figure 1). After four months of storage, PA encapsulated into 20:80 CPTEG:CPH and CPH:SA retained a significant portion of its bioactivity (Figure 5). PA adsorbed to alum lost all its bioactivity after two months of storage at all temperatures except −20°C (Figure 5 and Supplementary Figure 2A). When stored as a dry powder, 20:80 CPH:SA nanoparticles were capable of preserving nearly 100% of the bioactivity of PA at all temperatures studied for 4 months. In contrast, dry storage of 50:50 CPH:SA nanoparticles was ineffective at stabilizing PA under most of the storage conditions tested. It is important to note that all nanoparticle chemistries were successful in preserving PA bioactivity when stored at −20°C and could be viable vaccine carriers when cold storage is available.
Figure 5.
Dry powder formulations of PA-loaded 20:80 CPTEG:CPH and CPH:SA polyanhydride nanoparticles were capable of preserving the activity of PA for four months when stored at 40, 25, 4, and −20°C. The biological assay was performed by incubating 125 μg/mL nanoparticles with 0.3 μg/mL LF with RAW cells for 6 h. Error bars represent standard deviation of 3 replicates. Treatments with different letters are significantly different from one another at p < 0.05.
Discussion
Next-generation anthrax vaccines need to possess several attributes, including storage stability and improved immunogenicity to reduce the need for multiple booster injections. In this work, we have demonstrated that polyanhydride nanoparticle-based delivery systems can stabilize PA and enhance the shelf life of PA-based vaccines. In particular, these studies have shown that amphiphilic polyanhydride nanoparticles provide controlled antigen release over several weeks, the release of immunogenic protein capable of inducing high titer, neutralizing antibody, and extended shelf life storage at tropical and/or desert temperatures (e.g., 40°C).
Long term or repeated antigen exposure (depot effect) is essential for the development of immunological memory, which is a part of the rationale for the current immunization regimen for the AVA vaccine (i.e., five immunizations with yearly boosters)3. In the event of a bioterrorism attack, this protracted vaccination strategy may not be viable for treating a naïve population. A need therefore exists for a vaccine capable of inducing levels of neutralizing anti-PA antibody similar to that induced by the current immunization regimen, but in a single dose, that will also improve patient compliance. The nanoparticle-based delivery system described in this work demonstrated sustained release kinetics for over two months, dictated by polymer chemistry (Figure 1A), thereby offering an improved method for delivery of biowarfare vaccines.
Although controlled release kinetics enable long-term antigen exposure, it is also essential that the antigen remain stable during fabrication and long-term storage to maintain its immunogenicity. Alum, an adjuvant that is currently approved for human use in the U.S., is known to produce an acidic bulk-environment that can be detrimental for pH-sensitive proteins38. While the adsorbed antigen would experience a less acidic microenvironment on the surface of alum38, many pH-sensitive protein immunogens in the bulk would be denatured and rendered ineffective by the acidic conditions (pH~5.6). PA is a highly labile protein that is not only sensitive to acidic environments, but also to increased temperature - an effect that is exacerbated as the conditions become more acidic6. In this work, we demonstrated the superior PA stabilization capabilities of a nanoparticle-based delivery system that preserved the biological activity of PA during fabrication, delivery, and storage/thermal stability, thereby overcoming several of the problems associated with the use of alum-based vaccines.
Because of the absence of water in the process, nanoparticle fabrication conditions (solvent exposure, sonication, and vacuum drying) had no detectable effect on the structure, antigenicity, or activity of PA. This demonstrates the utility of the polyanhydride nanoparticle fabrication process for labile proteins, including PA, and is in agreement with similar results for other proteins exposed to these conditions29. However, low pH and elevated temperature have been reported to have more detrimental impact on the structural stability and bioactivity of PA5–7, 37, 39. As shown in Figure 1B, the pH, due to CPTEG:CPH nanoparticle erosion, only decreased to approximately 7.0 and was maintained at that value for over 30 days. In contrast, the erosion of CPH:SA nanoparticles decreased the pH to 5.2, which was similar to pH changes caused by alum. The acidic micro-environment caused by degradation of the CPH:SA nanoparticles correlated with the losses in structure (Figure 2), antigenicity and bioactivity (Figure 3) of PA released from these nanoparticles. The PA released from CPH:SA nanoparticle formulations also failed to prime an immune response capable of producing high titer, neutralizing serum antibody (Figure 4). Detailed structural analysis demonstrated that significant alterations in the secondary and tertiary structure of the PArel (Figure 2) were important determinants associated with the loss in immunogenicity, bioactivity, and quality (i.e., avidity) of the antibody response (Figure 4). Consistent with these results, it has been reported that thermally induced ellipticity changes in PA occur in acidic environments5–7, 39. In addition, at low pH and high temperature conditions, PA is structurally modified to a molten globular state6. As observed in this work, this loss of structural integrity rendered PA biologically inactive and poorly immunogenic.
Amphiphilic CPTEG:CPH nanoparticles, specifically 50:50 CPTEG:CPH, provided an effective stabilizing environment for PA. While nearly 80% of PA antigenicity and activity was preserved upon release from 50:50 CPTEG:CPH nanoparticles (Figure 3), less antigenicity and activity were preserved (20% and 50%, respectively) upon release from 20:80 CPTEG:CPH nanoparticles (Figure 3). From the detailed structural analysis, it is likely that the alterations in the secondary and tertiary structure of PA released from the 20:80 and 50:50 CPTEG:CPH nanoparticles (Figure 2C) may be responsible for the loss in antigenicity and bioactivity (Figure 3). These alterations may result from the slight decrease in pH at 37°C, consistent with what was reported by Jiang et al.6, which occurred as the acidic degradation products built up over the duration of the in vitro stability study. However, these polyanhydride chemistries did not prove to be detrimental to the immunogenicity of PA. The total and neutralizing antibody titers as well as the antibody avidity for mice immunized with PA released from 20:80 or 50:50 CPTEG:CPH nanoparticles were statistically indistinguishable from those induced by native PA (Figure 4). Thus, even in such “worst case” conditions (i.e., buildup of an acidic micro-environment in a microcentrifuge tube), the amphiphilic polyanhydride chemistries were not deleterious to PA.
One of the most difficult challenges to overcome in vaccine design and development is long-term storage and maintenance of bioactivity. This is an immediate concern in developing countries with limited infrastructure for cold storage. In this work, we tested the thermal stability of PA-loaded nanoparticles, PA adsorbed to alum, and PA in PBS for four months over a 60-degree temperature range (−20 to 40°C) while under dry storage. The changes observed in PA stored with alum are hypothesized to be a result of the acidic pH environment combined with the storage temperature. In contrast, PA stored in PBS buffer at a neutral pH is only likely to be affected by storage temperature. After two months of dry storage, all polyanhydride chemistries, except for 50:50 CPH:SA, outperformed the alum group in preserving the stability of PA at 40, 25, and 4°C (Supplementary Figure 1). After four months of dry storage, PA released from 20:80 CPTEG:CPH and CPH:SA nanoparticles retained its bioactivity (Figure 5). In these studies, it is important to note that dry formulations were evaluated while the studies described in Figures 2–4 tested PA-loaded nanoparticles that were incubated in an aqueous environment (to obtain the PArel). The dry storage conditions largely eliminate the build-up of acidic degradation products. This may explain why the 20:80 CPH:SA nanoparticles preserved PA bioactivity under these conditions.
Furthermore, these results indicate that the thermal properties of the copolymers, mainly the glass transition temperature (Tg), may play an integral role in particle shelf life over prolonged periods at elevated temperatures. Nanoparticles with Tgs close to or lower than the storage temperature may lose their particle structure due to their transition to a rubbery phase. The Tg values of 20:80 CPTEG:CPH, 50:50 CPTEG:CPH, 20:80 CPH:SA, and 50:50 CPH:SA have been reported to be 18, 8, 50, and 11°C, respectively31, 40, 41. This may explain why the polymers with the two lowest Tgs (i.e., 50:50 CPTEG:CPH and 50:50 CPH:SA) are unable to release bioactive PA upon extended storage at 25 or 40°C. In addition, the hydrophobic 50:50 CPH:SA chemistry may induce non-covalent hydrophobic interactions with PA that may lead to aggregation and loss of bioactivity. The 20:80 CPTEG:CPH and 20:80 CPH:SA nanoparticles revealed similar abilities to preserve PA at 40 and 25°C for 4 months, demonstrating enhanced nanoparticle thermal stability and subsequent protein stabilization similar to lyophilized PA stored with stabilizers after only one month6. While protein released from the 20:80 CPH:SA nanoparticles was not able to induce a robust antibody response following immunization, these formulations provided a suitable dry storage formulation at elevated temperatures. In contrast, the amphiphilic 20:80 CPTEG:CPH nanoparticles were able to induce robust antibody responses following immunization and provide for the preservation of a labile protein during long-term storage at tropical temperatures. The preliminary studies described herein have demonstrated a novel strategy for the design and development of a next-generation anthrax vaccine formulation with long-term stable storage capabilities.
Conclusions
Together, the studies reported herein demonstrate the potential use of a polyanhydride nanoparticle platform in next-generation vaccines employing recombinant proteins. These polyanhydride nanoparticles provide the ability to control PA antigen release, which would provide an in vivo antigen depot capable of long-term antigen presentation. Additionally, amphiphilic polyanhydride nanoparticles demonstrated superior thermal shelf life stability and the ability to withstand “worst case” conditions, thus making them capable of preserving PA bioactivity upon fabrication and storage at elevated temperatures. Of the four formulations tested, the amphiphilic 20:80 CPTEG:CPH nanoparticles demonstrated the best combination of characteristics to facilitate the stabilization of labile proteins, such as PA, making them excellent candidates for next-generation single-dose anthrax vaccines.
Supplementary Material
Supplementary Figure 1: Dry powder formulations of PA-loaded polyanhydride nanoparticles were capable of preserving the activity of PA for two months when stored at 40, 25, 4, and −20°C. After two months of storage nanoparticle made of 20:80 and 50:50 CPTEG:CPH and 20:80 CPH:SA best preserved the functionality of PA under all conditions tested. The biological assay was performed by incubating 125 μg/mL nanoparticles with 0.3 μg/mL LF with RAW cells for 6 h. Error bars represent standard deviation of three replicates. Treatments with different letters are significantly different from one another at p < 0.05.
Supplementary Figure 2: PA activity was sensitive to high temperature when adsorbed to alum A) or in PBS buffer B) over incremental time points (7, 14, 28, 58, and 120 days). The biological assay was performed by incubating the storage groups (at a concentration of 0.1 μg/mL PA) with 0.3 μg/mL LF and RAW cells for 6 h. Error bars represent standard deviation of three replicates. Treatments with different letters are significantly different from one another at p < 0.05.
Acknowledgments
This material is based upon work supported by the National Institutes of Health (R03 AI076855-01A1). The LF and PA were obtained through the NIH Biodefense and Emerging Infections Research Resources Repository, NIAID, NIH.
References
- 1.Institute of Medicine. The anthrax vaccine: is it safe? Does it work? National Academy Press; Washington, DC: 2002. [Google Scholar]
- 2.Leppla SH, Robbins JB, Schneerson R, Shiloach J. Development of an improved vaccine for anthrax. J Clin Invest. 2002;110:141–144. doi: 10.1172/JCI16204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tournier JN, Ulrich RG, Quesnel-Hellmann A, Mohamadzadeh M, Stiles BG. Anthrax, toxins and vaccines: a 125-year journey targeting Bacillus anthracis. Expert Rev Anti Infect Ther. 2009;7:219–236. doi: 10.1586/14787210.7.2.219. [DOI] [PubMed] [Google Scholar]
- 4.Singh S, Ahuja N, Chauhan V, Rajasekaran E, Mohsin Waheed S, Bhat R, Bhatnagar R. Gln277 and Phe554 residues are involved in thermal inactivation of protective antigen of Bacillus anthracis. Biochem Biophys Res Comm. 2002;296:1058–1062. doi: 10.1016/s0006-291x(02)02049-1. [DOI] [PubMed] [Google Scholar]
- 5.Singh S, Aziz MA, Khandelwal P, Bhat R, Bhatnagar R. The osmoprotectants glycine and its methyl derivatives prevent the thermal inactivation of protective antigen of Bacillus anthracis. Biochem Biophys Res Comm. 2004;316:559–564. doi: 10.1016/j.bbrc.2004.02.083. [DOI] [PubMed] [Google Scholar]
- 6.Jiang G, Joshi SB, Peek LJ, Brandau DT, Huang J, Ferriter MS, Woodley WD, Ford BM, Mar KD, Mikszta JA, Hwang CR, Ulrich R, Harvey NG, Middaugh CR, Sullivan VJ. Anthrax vaccine powder formulations for nasal mucosal delivery. J Pharm Sci. 2006;95:80–96. doi: 10.1002/jps.20484. [DOI] [PubMed] [Google Scholar]
- 7.Castelan-Vega J, Corvette L, Sirota L, Arciniega J. Reduction of immunogenicity of anthrax vaccines subjected to thermal stress, as measured by a toxin neutralization assay. Clin Vaccine Immunol. 2010;18:349–351. doi: 10.1128/CVI.00267-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiss MM, Weiss PD, Weiss JB. Anthrax vaccine and public health policy. Am J Public Health. 2007;97:1945–1951. doi: 10.2105/AJPH.2006.102749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moayeri M, Wiggins JF, Leppla SH. Anthrax protective antigen cleavage and clearance from the blood of mice and rats. Infect Immun. 2007;75:5175–5184. doi: 10.1128/IAI.00719-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zinkernagel RM, Hengartner H. On immunity against infections and vaccines: credo 2004. Scand J Immunol. 2004;60:9–13. doi: 10.1111/j.0300-9475.2004.01460.x. [DOI] [PubMed] [Google Scholar]
- 11.Zinkernagel RM. Localization dose and time of antigens determine immune reactivity. Semin Immunol. 2000;12:163–171. doi: 10.1006/smim.2000.0253. [DOI] [PubMed] [Google Scholar]
- 12.Holmgren J, Czerkinsky C. Mucosal immunity and vaccines. Nat Med. 2005;11:S45–S53. doi: 10.1038/nm1213. [DOI] [PubMed] [Google Scholar]
- 13.Heikenwalder M, Polymenidou M, Junt T, Sigurdson C, Wagner H, Akira S, Zinkernagel R, Aguzzi A. Lymphoid follicle destruction and immunosuppression after repeated CpG oligodeoxynucleotide administration. Nat Med. 2004;10:187–192. doi: 10.1038/nm987. [DOI] [PubMed] [Google Scholar]
- 14.Carrillo-Conde B, Song EH, Chavez-Santoscoy A, Phanse Y, Ramer-Tait A, Pohl NL, Wannemuehler M, Narasimhan B. Mannose-modified “pathogen-like” polyanhydride nanoparticles target C-type lectin receptors on dendritic cells. Mol Pharm. 2011;8:1877–1886. doi: 10.1021/mp200213r. [DOI] [PubMed] [Google Scholar]
- 15.Kipper MJ, Wilson JH, Wannemuehler MJ, Narasimhan B. Single dose vaccine based on biodegradable polyanhydride microspheres can modulate immune response mechanism. J Biomed Mater Rest A. 2006;76A:798–810. doi: 10.1002/jbm.a.30545. [DOI] [PubMed] [Google Scholar]
- 16.Petersen LK, Ulery BD, Broderick S, Kong CS, Ramer-Tait A, Wannemuehler M, Rajan K, Narasimhan B. Activation of innate immune responses in a pathogen-mimicking manner by amphiphilic polyanhydride nanoparticle adjuvants. Biomaterials. 2011;32:6815–6822. doi: 10.1016/j.biomaterials.2011.05.063. [DOI] [PubMed] [Google Scholar]
- 17.Petersen LK, Xue L, Wannemuehler MJ, Rajan K, Narasimhan B. The simultaneous effect of polymer chemistry and device geometry on the in vitro activation of murine dendritic cells. Biomaterials. 2009;30:5131–5142. doi: 10.1016/j.biomaterials.2009.05.069. [DOI] [PubMed] [Google Scholar]
- 18.Torres MP, Wilson-Welder J, Lopac SK, Phanse Y, Carrillo-Conde B, Ramer-Tait A, Bellaire B, Wannemuehler MJ, Narasimhan B. Polyanhydride microparticles enhance dendritic cell antigen presentation and activation. Acta Biomater. 2011;7:2857–2864. doi: 10.1016/j.actbio.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ulery BD, Kumar D, Ramer-Tait A, Metzger DW, Wannemuehler MJ, Narasimhan B. Design of a protective single-dose intranasal nanoparticle-based vaccine platform for respiratory infectious diseases. PLoS ONE. 2011;6:e17642. doi: 10.1371/journal.pone.0017642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huntimer L, Ross K, Petersen LK, Walz K, O’Neill K, Ramer-Tait A, Hostetter J, Narasimhan B, Wannemuehler MJ. Biodistribution and safety of polyanhydride nanoparticles as vaccine delivery vehicles. ACS Nano. 2011 to be submitted. [Google Scholar]
- 21.Ulery BD, Petersen LK, Phanse Y, Broderick S, Kong CS, Ramer-Tait A, Bellaire B, Wannemuehler M, Rajan K, Narasimhan B. Rational design of pathogen-mimicking nanoparticle adjuvant platform. Sci Rep. 2011;1:198. doi: 10.1038/srep00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carrillo-Conde B, Schiltz E, Yu J, Chris Minion F, Phillips GJ, Wannemuehler MJ, Narasimhan B. Encapsulation into amphiphilic polyanhydride microparticles stabilizes Yersinia pestis antigens. Acta Biomater. 2010;6:3110–3119. doi: 10.1016/j.actbio.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 23.Determan AS, Graham JR, Pfeiffer KA, Narasimhan B. The role of microsphere fabrication methods on the stability and release kinetics of ovalbumin encapsulated in polyanhydride microspheres. J Microencapsul. 2006;23:832–843. doi: 10.1080/02652040601033841. [DOI] [PubMed] [Google Scholar]
- 24.Determan AS, Trewyn BG, Lin VS, Nilsen-Hamilton M, Narasimhan B. Encapsulation, stabilization, and release of BSA-FITC from polyanhydride microspheres. J Control Rel. 2004;100:97–109. doi: 10.1016/j.jconrel.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Determan AS, Wilson JH, Kipper MJ, Wannemuehler MJ, Narasimhan B. Protein stability in the presence of polymer degradation products: consequences for controlled release formulations. Biomaterials. 2006;27:3312–3320. doi: 10.1016/j.biomaterials.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 26.Petersen LK, Determan AS, Westgate C, Bendickson L, Nilsen-Hamilton M, Narasimhan B. Lipocalin-2-loaded amphiphilic polyanhydride microparticles accelerate cell migration. J Biomater Sci Polym Ed. 2011;22:1237–1252. doi: 10.1163/092050610X502776. [DOI] [PubMed] [Google Scholar]
- 27.Petersen LK, Sackett CK, Narasimhan B. A novel, high throughput method to study in vitro protein release from polymer nanospheres. J Com Chem. 2010;12:51–56. doi: 10.1021/cc900116c. [DOI] [PubMed] [Google Scholar]
- 28.Torres MP, Determan AS, Anderson GL, Mallapragada SK, Narasimhan B. Amphiphilic polyanhydrides for protein stabilization and release. Biomaterials. 2007;28:108–116. doi: 10.1016/j.biomaterials.2006.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Petersen LK, Sackett CK, Narasimhan B. High-throughput analysis of protein stability in polyanhydride nanoparticles. Acta Biomater. 2010;6:3873–3881. doi: 10.1016/j.actbio.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Lopac SK, Torres MP, Wilson-Welder JH, Wannemuehler MJ, Narasimhan B. Effect of polymer chemistry and fabrication method on protein release and stability from polyanhydride microspheres. J Biomed Mater Res B. 2009;91:938–947. doi: 10.1002/jbm.b.31478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torres MP, Vogel BM, Narasimhan B, Mallapragada SK. Synthesis and characterization of novel polyanhydrides with tailored erosion mechanisms. J Biomed Mater Res A. 2006;76:102–110. doi: 10.1002/jbm.a.30510. [DOI] [PubMed] [Google Scholar]
- 32.Vogel BM, Mallapragada SK. Synthesis of novel biodegradable polyanhydrides containing aromatic and glycol functionality for tailoring of hydrophilicity in controlled drug delivery devices. Biomaterials. 2005;26:721–728. doi: 10.1016/j.biomaterials.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 33.Kipper MJ, Shen E, Determan A, Narasimhan B. Design of an injectable system based on bioerodible polyanhydride microspheres for sustained drug delivery. Biomaterials. 2002;23:4405–4412. doi: 10.1016/s0142-9612(02)00181-3. [DOI] [PubMed] [Google Scholar]
- 34.Adler AF, Petersen LK, Wilson JH, Torres MP, Thorstenson JB, Gardner SW, Mallapragada SK, Wannemuehler MJ, Narasimhan B. High throughput cell-based screening of biodegradable polyanhydride libraries. Comb Chem High Through Screen. 2009;12:634–645. doi: 10.2174/138620709788923764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ulery BD, Phanse Y, Sinha A, Wannemuehler MJ, Narasimhan B, Bellaire BH. Polymer chemistry influences monocytic uptake of polyanhydride nanospheres. Pharm Res. 2009;26:683–690. doi: 10.1007/s11095-008-9760-7. [DOI] [PubMed] [Google Scholar]
- 36.Xue L, Petersen L, Broderick S, Narasimhan B, Rajan K. Identifying factors controlling protein release from combinatorial biomaterial libraries via hybrid data mining methods. ACS Comb Sci. 2011;13:50–58. doi: 10.1021/co100019d. [DOI] [PubMed] [Google Scholar]
- 37.Radha C, Salotra P, Bhat R, Bhatnagar R. Thermostabilization of protective antigen--the binding component of anthrax lethal toxin. J Biotechnol. 1996;50:235–242. doi: 10.1016/0168-1656(96)01569-6. [DOI] [PubMed] [Google Scholar]
- 38.Wittayanukulluk A, Jiang D, Regnier FE, Hem SL. Effect of microenvironment pH of aluminum hydroxide adjuvant on the chemical stability of adsorbed antigen. Vaccine. 2004;22:1172–1176. doi: 10.1016/j.vaccine.2003.09.037. [DOI] [PubMed] [Google Scholar]
- 39.Singh S, Singh A, Aziz MA, Waheed SM, Bhat R, Bhatnagar R. Thermal inactivation of protective antigen of Bacillus anthracis and its prevention by polyol osmolytes. Biochem Biophys Res Comm. 2004;322:1029–1037. doi: 10.1016/j.bbrc.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 40.Shen E, Pizsczek R, Dziadul B, Narasimhan B. Microphase separation in bioerodible copolymers for drug delivery. Biomaterials. 2001;22:201–210. doi: 10.1016/s0142-9612(00)00175-7. [DOI] [PubMed] [Google Scholar]
- 41.Shen E, Kipper MJ, Dziadul B, Lim MK, Narasimhan B. Mechanistic relationships between polymer microstructure and drug release kinetics in bioerodible polyanhydrides. J Control Rel. 2002;82:115–125. doi: 10.1016/s0168-3659(02)00125-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Dry powder formulations of PA-loaded polyanhydride nanoparticles were capable of preserving the activity of PA for two months when stored at 40, 25, 4, and −20°C. After two months of storage nanoparticle made of 20:80 and 50:50 CPTEG:CPH and 20:80 CPH:SA best preserved the functionality of PA under all conditions tested. The biological assay was performed by incubating 125 μg/mL nanoparticles with 0.3 μg/mL LF with RAW cells for 6 h. Error bars represent standard deviation of three replicates. Treatments with different letters are significantly different from one another at p < 0.05.
Supplementary Figure 2: PA activity was sensitive to high temperature when adsorbed to alum A) or in PBS buffer B) over incremental time points (7, 14, 28, 58, and 120 days). The biological assay was performed by incubating the storage groups (at a concentration of 0.1 μg/mL PA) with 0.3 μg/mL LF and RAW cells for 6 h. Error bars represent standard deviation of three replicates. Treatments with different letters are significantly different from one another at p < 0.05.