Abstract
Purpose
The objective of this study was to evaluate the overall incidence and total burden of successful litigation relating to the management of spinal disease across the National Health Service (NHS) in England.
Methods
The study design comprised a retrospective review of the NHS Litigation Authority (NHSLA) database, retrieving all successful claims relating to spinal disease between 2002 and 2010—a total of 235 (144 acute, 91 elective).
Results
The general trend for successful claims with relation to spinal surgery has actually been decreasing steadily over the last few years. The total value of these claims during the period was £60.5 million, comprising £42.8 million (£28.6 million relating to acute diagnoses, £16.1 million for elective) in damages and £17.7 million in legal costs (31% relating to NHS legal costs, the remainder claimants costs).
Conclusions
Spinal litigation remains a source of significant cost to the NHS. The complexity of resolving these cases is reflected in the associated legal costs.
Keywords: Malpractice, Spinal, Surgery, NHS, Litigation
Introduction
The Oxford English Dictionary defines negligence as ‘a want of attention to what ought to be done or looked after’, and ‘a failure to match up to required standards of performance’. The law of negligence requires a three stage test: that the doctor owed the patient a duty of care, that the duty was breached, and that the doctor caused the breach. If any of these cannot be proved then the case will fail. Essentially, the standard of care has to have fallen below what is acceptable. Recent judgements, such as Chester vs Afshar (2004) [1] have raised the threshold for what is deemed acceptable and patients are becoming more informed of their right to redress.
Medical negligence claims are an increasing feature of clinical practice in the UK. Although medicine in Britain is still much less litigious than in the United States, medical negligence is on the increase. It is reported that thousands of patients die or are seriously injured every year as a result of medical errors and 1 in 10 suffers an ‘adverse affect’ due to hospital accidents, diagnostic errors and operating mistakes [2].
In 1995, the National Health Service Litigation Authority (NHSLA) was established to centralise the management of claims made against NHS trusts within England, essentially functioning as an in-house insurance firm. There are separate arrangements in Scotland and Wales. Since 2002, all claims regardless of size have been referred to the NHSLA. With regards to case management, there is a 3-year statute of limitations (with a few exceptions), and the average time to close a case currently stands at around 18 months [3]. The annual burden of litigation indemnity payments to the NHS was £863 million in 2010/11, and this figure has been rising every consecutive year since the inception of the NHSLA [4].
There have been no published systemic studies evaluating the clinical negligence claims relating to the treatment of spinal disease within the NHS. Whilst allegations of malpractice, and the associated litigation is an issue that spans centuries of medical practice [5], the available information relates to American experience [6], or NHS experience of other specialities [7]. Spinal surgeons remain in the highest risk group (1a) with regards to indemnity cover in the independent sector [8].
We present a national overview of litigation relating to spinal disease spanning a nine year period.
Methods
The NHSLA has a remit to centralise and standardise the management of claims. Since 2002, all claims made against trusts have been notified to the NHSLA. Using the Freedom of Information Act (2000), we obtained data relating to the number of successful claims filed with the NHSLA relating to the spine—both spinal surgery and acute diagnoses (including trauma) from the duration of the financial years 2002–2010. The data was made available with a short précis of the case from which data was extracted relating to the specialty of the clinician involved, the underlying pathology, severity of injury, nature of the misadventure and the size of the claim.
Data relating to the number of elective spinal procedures performed per year (excluding all injections), as well as hospital admissions relating to spinal disease, were obtained from http://www.hesonline.nhs.uk (Table 1).
Table 1.
Numbers of elective and emergency spinal procedures performed within the NHS in England (2002–2010)
| Year | Total admissions | Emergency admissions | Emergency procedures | Elective procedures |
|---|---|---|---|---|
| 2009/10 | 115,498 | 32,553 | 4,433 | 19,364 |
| 2008/09 | 108,445 | 31,015 | 4,074 | 19,490 |
| 2007/08 | 93,404 | 26,420 | 3,984 | 18,369 |
| 2006/07 | 77,277 | 20,797 | 3,741 | 17,687 |
| 2005/06 | 69,410 | 17,854 | 3,573 | 17,344 |
| 2004/05 | 59,346 | 15,258 | 3,394 | 15,806 |
| 2003/04 | 55,126 | 13,379 | 3,302 | 15,842 |
| 2002/03 | 52,580 | 12,908 | 3,289 | 14,991 |
| 2001/02 | 45,390 | 10,584 | 3,421 | 13,105 |
Results
A total of 235 closed claims were reviewed covering the time period from 2002 to 2010—144 related to spinal trauma/acute care and 91 to elective spinal care (Table 2). The most litigated specialties depended on the nature of the presentation. Regarding acute cases, Emergency Physicians were the most common defendants (63), followed by orthopaedic surgeons (41) and general physicians (internal medicine) (20). For elective care, the most common defendants were orthopaedic surgery (55), followed by neurosurgery (17), reflecting the division of operative spinal care between the two specialties.
Table 2.
Causes of alleged negligence in the 235 closed cases and average damages paid out regarding acute spinal diagnoses and the 151,998 elective procedures performed over 9 years
| Diagnosis | Frequency (%) | Average damages (£ sterling) |
|---|---|---|
| Acute | ||
| Missed fracture post-fall | 38 (26.4%) | 76,578 |
| Missed fracture post-RTA | 22 (15.3%) | 122,171 |
| Missed cauda equina | 34 (23.6%) | 268,515 |
| Missed infection | 17 (11.8%) | 433,296 |
| Incorrect diagnosis | 21 (14.6%) | 111,809 |
| Delay to surgery | 10 (7%) | 149,645 |
| Post-operative care | 2 (1.4%) | 7,550 |
| Elective | ||
| Damage to spinal cord | 18 (19.8%) | 367,972 |
| Post-operative care | 14 (15.4%) | 51,241 |
| Infection | 10 (11%) | 32,180 |
| Surgical failure | 9 (9.9%) | 212,555 |
| Wrong level | 9 (9.9%) | 119,825 |
| Cauda equina syndrome | 9 (9.9%) | 332,496 |
| Foreign body retention | 5 (5.5%) | 27,000 |
| Delayed management | 5 (5.5%) | 136,078 |
| Incorrect diagnosis | 4 (4.4%) | 91,125 |
| Non-op site injury | 3 (3.3%) | 29,166 |
| On-going pain | 2 (2.2%) | 59,250 |
| Thrombo-embolic | 2 (2.2%) | 163,237 |
| Non-union | 1 (1.1%) | 55,000 |
The most common pathologies leading to a successful claim in the context of acute care were missed fractures- either following a fall (23) or road traffic accident (RTA) (22), cauda equina syndrome secondary to prolapsed intervertebral disc disease (38), or infections of the spine (34). With regards to elective care, the most common complaints were neurological damage (18) and failures in post operative care (14). The full results are reproduced in Table 2, including the average financial damages paid to successful litigants.
Costings and litigation trends
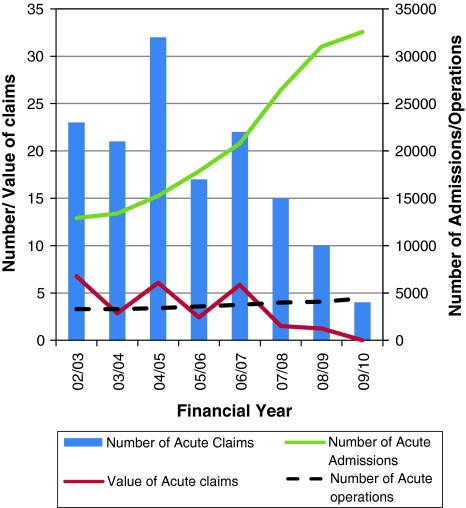
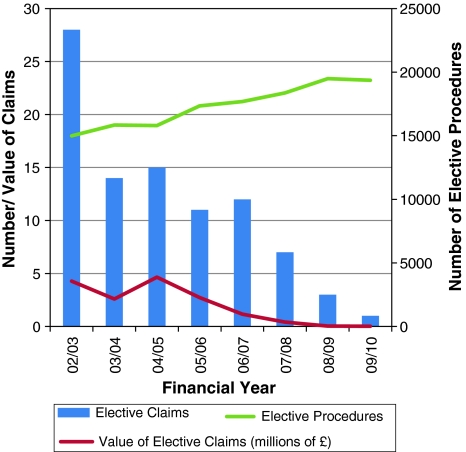
The average legal costs associated with a successful claim were £75,320, comprising of NHS costs of £23,350 and plaintiffs costs of £51,970 (Table 1). The rates of litigation were compared graphically to the number of elective spinal procedures, emergency procedures and emergency admissions in Figs. 1 and 2. Numbers of emergency procedures and emergency spinal admissions were used as proxies for acute spinal diagnoses—covering such a diverse range of diagnoses that we were unable to ascertain true figures (many of those with acute spinal concerns will be admitted under another specialty—or not at all, as demonstrated by the breakdown of defendants).
Fig. 1.
Graph demonstrating the number and value of claims per year, compared against number of emergency admissions and emergency operations performed
Fig. 2.
Graph demonstrating the number and value of claims relating to elective operations
Discussion
Fear of litigation has become a constant companion to all medical professionals, and spinal surgery is no exception. The NHS has seen a significant increase in the number of patients undergoing spinal procedures over the last decade. This does not seem to be accompanied by a concomitant increase in rates of litigation. It is, however, too early to draw any firm conclusions as given the 3-year statute of limitations and average duration of a claim prevents us from comprehensively examining data from the last 5 years. The question, therefore, arises of the overall incidence of claims—not merely the closed cases. On this occasion, the NHSLA were unable to readily obtain the information pertaining to every claim for the period in question, preventing direct comparison in this case.
Previously presented data from the corresponding author (NAQ) examined the distribution and eventual outcome of 68 claims of malpractice made against NHS spinal surgeons 2000–2009 [9]. They found that the majority of complaints related to intra/post op complications (59%), with delay to treatment/diagnosis (28%), inaccurate consent/assessment (9%) and anaesthetic problems (4%). Eighty percent of all cases were the result of ‘routine’ operations (decompression/fusion at any level). The overall outcome showed that over the decade analysed, only 20 of these 68 claims were closed—with 35% closed in favour of the claimant, which relates well to previously published evidence from the US [6]—the remainder were still outstanding. This would imply that whilst the outcomes are generally favourable for the spinal surgeon, the claims are of a prolonged nature, leaving the claimant unsatisfied and the defendant exposed to the ongoing negative effects of litigation, including increased suicidal ideation, depression and reduced job satisfaction [10].
The Medical Defence Union (MDU), the UK’s biggest provider of medical indemnity and insurance to doctors, paid out nearly £9 million in damages and legal costs to compensate patients harmed as a result of spinal surgery in the independent sector over a recent 10-year period. The MDU’s analysis of 255 claims from orthopaedic surgeons’ independent practice, revealed that spinal surgery was the most expensive category of settled orthopaedic claims and the most common, comprising nearly a quarter of the total (22%) [8]. The 56 spinal operative claims arose following procedures such as decompression, discectomy and fusion surgery. The size of settlements across the orthopaedic specialty ranged from £800 for a retained swab to just over £1 million which was awarded to a patient who suffered partial paralysis following shoulder surgery. Overall, the most common reasons for claims were an unsatisfactory outcome (49 cases), missed or incorrect diagnosis (33 cases), nerve damage (32 cases) and surgery being carried out on the wrong site or the wrong procedure being carried out (26 cases).
There are many potential confounding factors that may prevent us from drawing firm conclusions from the data available; in particular, the NHSLA data does not cover countries outside of England, private practice or the work of the major medical defence unions. However, the majority of spinal procedures continue to be performed in the public sector and so this is likely to be a reasonably balanced snapshot of reality.
Despite the common perception of the US as a particularly litigious society with disproportionate legal costs and awards, our data would show that our average payout of £257,445 is not dramatically different from the $485,182 (£309,033) average award following lumbar surgery complications [6] and our legal costs are considerably higher—£75,320 for each successful case versus $45,433. It is unknown how many lawyers worked on a percentage basis, but on the face of the available evidence the legal costs associated with spinal litigation are considerably higher in England than in New York.
The key point to note is that more than 60% of all claims for acute spinal diagnoses were directed at non-surgical specialties, underpinning the vital and ongoing need for education regarding spinal disorders across the breadth of medical professionals, as well as the need for constant awareness for these rare, yet devastating diagnoses.
Conclusion
We have presented the results of the first systematic review of successful malpractice claims for spinal disease within the NHS in England. Whilst complications and claims are infrequent, the associated costs are considerable. It will be necessary to review this data in 5 years time to examine the ongoing trends in litigation, and to ensure that as a profession we continue to do our utmost to limit harm to our patients through failures of practice.
Conflict of interest
None.
Contributor Information
N. A. Quraishi, Email: nasquraishi@hotmail.com
T. C. Hammett, Phone: +44-115-9249924, FAX: +44-115-9709991
References
- 1.Chester vs Afshar. UKHL 2004:41
- 2.Vincent C, Neale G, Woloshynowych M. Patient safety incidents in British hospitals: preliminary retrospective record review. BMJ. 2001;322:517–519. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NHSLA Framework Document. http://www.nhsla.com (accessed 23rd January 2012)
- 4.NHSLA report and accounts 2010–2011. http://www.nhsla.com (accessed 23rd January 2012)
- 5.Richards P, Kennedy IM, Woolf L. Managing medical mishaps. BMJ. 1996;313:243–244. doi: 10.1136/bmj.313.7052.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rovit RL, Simon AS, Drew J, Murali R, Robb J. Neurosurgical experience with malpractice litigation: an analysis of closed claims against neurosurgeons in New York State, 1999 through 2003. J Neurosurg. 2007;106:1108–1114. doi: 10.3171/jns.2007.106.6.1108. [DOI] [PubMed] [Google Scholar]
- 7.McNeill A. Neurological negligence claims in the NHS from 1995 to 2005. Eur J Neurol. 2007;14:399–402. doi: 10.1111/j.1468-1331.2007.01677.x. [DOI] [PubMed] [Google Scholar]
- 8.Roberts K (2007) Managing risk in orthopaedics. Independent Practitioner July 2007
- 9.Quraishi NA, Porter IR (2010) litigation in spine surgery—analysis of 10 years data from the NHSLA. JBJS Proceedings 2011
- 10.Balch CM, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213(5):657–667. doi: 10.1016/j.jamcollsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]