Abstract
BACKGROUND
Neighborhood characteristics are associated with health and the perception of safety is particularly important to exercise and health among older adults. Little is known about the relationship between perception of neighborhood safety and functional decline in older adults.
OBJECTIVE
To determine the relationship between perceived neighborhood safety and functional decline in older adults.
DESIGN/SETTING
Longitudinal, community-based.
PARTICIPANTS
18,043 persons, 50 years or older, who participated in the 1998 and 2008 Health and Retirement Study.
MAIN MEASURES
The primary outcome was 10-year functional decline (new difficulty or dependence in any Activity of Daily Living, new mobility difficulty, and/or death). The primary predictor was perceived neighborhood safety categorized into three groups: “very safe”, “moderately safe”, and “unsafe.” We evaluated the association between perceived neighborhood safety and 10-year functional decline using a modified Poisson regression to generate unadjusted and adjusted relative risks (ARR).
KEY RESULTS
At baseline 11,742 (68.0%) participants perceived their neighborhood to be very safe, 4,477 (23.3%) moderately safe, and 1,824 (8.7%) unsafe. Over 10 years, 10,338 (53.9%) participants experienced functional decline, including 6,266 (50.2%) who had perceived their neighborhood to be very safe, 2,839 (61.2%) moderately safe, and 1,233 (63.6%) unsafe, P < 0.001. For the 11,496 (63.3%) of participants who were functionally independent at baseline, perceived neighborhood safety was associated with 10-year functional decline (moderately safe ARR 1.15 95% CI 1.09–1.20; unsafe ARR 1.21 95% CI: 1.03–1.31 compared to very safe group). The relationship between perceived neighborhood safety and 10-year functional decline was not statistically significant for participants who had baseline functional impairment.
CONCLUSION
Asking older adults about their perceived neighborhood safety may provide important information about their risk of future functional decline. These findings also suggest that future studies might focus on assessing whether interventions that promote physical activity while addressing safety concerns help reduce functional decline in older adults.
KEY WORDS: functional decline, disparities, neighborhood safety, elderly
INTRODUCTION
Neighborhood characteristics have a strong association with health. Summary measures of neighborhood deprivation based on sociodemographic factors such as race/ethnicity, education and income are associated with poor self-rated health,1,2 morbidity,3,4 and premature mortality (death under 65 years old) in adults of all ages.5 Perception of one’s personal safety is also intricately tied to health, quality of life, well-being and social engagement.6–9 Perception of safety and neighborhood characteristics appear to be particularly important among older adults. For instance, reported neighborhood deterioration is associated with poor self-rated health in older adults1 and older adults are more likely to report feeling unsafe than younger adults,10–12 despite being less likely to be victims of crime.13
For older adults, perception of poor neighborhood safety can negatively affect health. In one study, perception of poor neighborhood safety due to crime was associated with an 8-year mobility decline in impoverished older adults living in New Haven, Connecticut.14 In another one-county study of older adults, perception of adverse neighborhood characteristics (traffic, noise, crime, trash, lighting, public transportation) predicted accelerated physical decline over 1 year in lifting a large object and standing and walking up a flight of stairs.15 Other studies have shown that perceived poor neighborhood safety is associated with baseline physical inactivity.16,17 Such physical inactivity can lead to deconditioning and functional decline in older adults; both of which are strong predictors of high health care costs, high health care utilization, poor quality of life, and mortality.18,19 Yet, to our knowledge, there are no studies that have assessed the relationship between perceptions of neighborhood safety and long-term decline in Activities of Daily Living (bathing, eating, dressing, toileting, transferring), the most commonly used measure of functional ability in older adults. Moreover, previous studies were small, geographically limited, did not include a representative sample of the U.S. older adults population, and/or had short follow up.
Because little is known about the relationship between perceptions of neighborhood safety and long-term functional decline in older adults, the goals of this study were to determine: (1) the baseline relationship between perceived neighborhood safety, health and function in older adults, and (2) the association between perceived neighborhood safety and 10-year functional decline in a nationally representative sample of Americans aged 50 years or older.
METHODS
Study Design and Sample
The original sample for this longitudinal cohort study included 19,836 persons, aged 50 years or older, who participated in the 1998 Health and Retirement Study (HRS) and completed the Housing Questionnaire portion of the 1998 survey. The HRS is a national, population-based, longitudinal study of community-dwelling adults aged 50 or older.20 Because we were interested in the relationship between perceived neighborhood safety and functional decline, we excluded 27 (0.1%) individuals from our analytic sample who did not answer the question about perceived neighborhood safety in 1998 and 22 (0.1%) who did not answer all of the baseline questions about their Activities of Daily Living in 1998. We then excluded 1,708 (8.6%) individuals for whom we were not able to determine the combined outcome of ADL decline, mobility decline or death. Of these 1,708 participants, 489 (2.5%) ended their participation in the HRS before the 2008 interview and 1,219 (6.1%) individuals, while still a part of the HRS study, did not participate in the 2008 interview. Finally, we excluded 36 (0.2%) individuals who did not answer all the questions about Activities of Daily Living (ADL) (eating, dressing, transferring, toileting, bathing) or mobility (ability to walk several blocks or climb one flight of stairs) in 2008. The probability of exclusion was random with respect to the predictor (neighborhood safety). The resulting sample for our analyses was 18,043 individuals from 12,575 households.
Measures
Outcome Variables
Our outcome of interest was 10-year functional decline, a composite measure defined as decline in any ADL, decline in mobility, and/or death. The five ADL assessed included eating, dressing, transferring, toileting, and bathing. There were three classification strata for ADL ability: “independent” (no difficulty in any of the five ADL), “having difficulty” (difficulty with at least one ADL but not requiring help with it), and “dependent” (requiring help with an ADL). Mobility was defined as “independent” (no difficulty in ability to walk several blocks or climb one flight of stairs) or “having difficulty” (needing help with these activities). Change in 10-year functional ability included development of any new difficulty or progression to dependence in an ADL or new difficulty in mobility compared to baseline. We included death in our definition of functional decline because other research shows that most older persons decline in functional status prior to death.21,22 HRS tracks and confirms vital status with the National Death Index.
Predictor Variable
Our primary predictor was perceived neighborhood safety, assessed with the question “Would you say the safety of your neighborhood is excellent, very good, good, fair, or poor?” We categorized the responses excellent or very good as “very safe”, good as “moderately safe,” and fair or poor as “unsafe.” Others have used a similar categorization scheme.14
Other Variables
We also considered other variables that may confound the relationship between perceived neighborhood safety and functional decline. These included sociodemographics (age, sex, race/ethnicity, marital status, education, wealth, income, urban/rural residence); health status [depression, self-rated health, hypertension, diabetes mellitus, cancer (excluding non-metastatic skin cancers), lung disease, heart conditions, stroke, arthritis]; and baseline functional status. Studies have shown that sociodemographic characteristics are linked to neighborhood safety14–16 and to long-term functional outcomes.23–25 Baseline health and functional status can also have an impact on the perception of safety14,15 and long-term functional status.23–25
Race/ethnicity was categorized by participants’ response to two questions (1) “Do you consider yourself primarily white or Caucasian, black or African American, American Indian or Asian or something else?” and (2) “Do you consider yourself Hispanic or Latino?” All participants who answered “yes” to being Hispanic or Latino were categorized as Latino, regardless of race. In total, we used four race/ethnicity categories: black, white, Latino, and other (which included participants that self-identified as American Indian, Asian or something else). We categorized educational attainment as less than high school, high school graduate/General Educational Development certificate, or more than high school. We defined wealth as net worth, a comprehensive measure of all assets and debts. Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D) which has been used in various population-based studies.26 The HRS uses 8 items from the scale and a cutoff score of at least three was used to represent depression.27
Statistical Analyses
Characteristics of the study sample were compared according to perceived neighborhood safety using chi-square tests for categorical variables and trend tests for binary and continuous variables. We determined associations between perceived neighborhood safety and 10-year functional decline using a modified Poisson regression to generate unadjusted and adjusted relative risks. To control for potential confounding, we adjusted for sociodemographics and baseline health and functional status. To determine whether the relationship between perceived neighborhood safety and functional decline varied by baseline functional and socioeconomic status, we tested interaction terms between perceived neighborhood safety and baseline functional status and between neighborhood safety and wealth. In this instance, we categorized baseline function as a binary variable (independent vs. have any difficulty and/or dependence in at least one activity).
All reported analyses were weighted to account for the complex design of the HRS. Statistical analyses were completed using STATA software, version 10.1 (StataCorp, College Station, TX), and SAS software, version 9.2 (SAS Institute, Cary, North Carolina).
RESULTS
Subject Characteristics
Overall, 18,043 HRS participants (aged 50 to 105 years) were included in this study. The mean age of participants was 65.4 years, 44.8% were male, 83.1% were white, and 25.0% received less than a high school education. The median wealth was $129,000, 64.6% were married, 30.1% resided in a rural environment. At baseline, 66.3% of participants were independent (reported having no difficulty) in all ADL and mobility measures and 5.9% of participants were dependent (required help) in at least one ADL or mobility measure.
Baseline characteristics of the 18,043 HRS participants according to perceived neighborhood safety are described in Table 1. Overall, 68.0% perceived their neighborhood to be very safe, 23.3% perceived it to be moderately safe, and 8.7% perceived it to be unsafe. These 3three groups differed significantly by sociodemographic characteristics, health and functional status. Those who perceived their neighborhoods to be very safe were more likely to be men, married, white, and to have a high school degree or higher. Those in the very safe group were also more likely to have more wealth, fewer chronic conditions (except cancer), and lower baseline rates of ADL or mobility impairment.
Table 1.
Baseline Characteristics of Study Sample According to Perceived Neighborhood Safety* (N = 18,043) †
| Characteristic | Very Safe (N = 11,742) | Moderately Safe (N = 4,477) | Unsafe (N = 1,824) | p-value‡ |
|---|---|---|---|---|
| Mean age, Yrs ( ± SD) | 65.0 (10.2) | 66.3 (11.2) | 65.3 (11.8) | 0.014 |
| Male, % | 46.0 | 42.3 | 42.0 | <0.001 |
| Married, % | 68.8 | 58.8 | 47.6 | <0.001 |
| Race / Ethnicity, % | <0.001 | |||
| White | 89.4 | 75.4 | 54.4 | |
| Black | 5.2 | 13.7 | 28.4 | |
| Latino | 3.9 | 9.1 | 15.1 | |
| Other § | 1.5 | 1.8 | 2.1 | |
| Education, % | <0.001 | |||
| < High school diploma | 19.1 | 34.7 | 45.2 | |
| High school or GED | 36.0 | 36.8 | 31.8 | |
| Some college or higher | 44.9 | 28.5 | 23.0 | |
| Median net worth, in thousands (K), (IQR) | 174K (67K-395K) | 81K (22K-206K) | 31K (2K-91K) | <0.001 |
| Median income, in thousands (K), (IQR) | 38K (20K-71K) | 24K (13K-45K) | 17K (9K-35K) | <0.001 |
| Urban residence, % | 69.7 | 68.8 | 73.8 | 0.486 |
| Chronic Medical Conditions, % | ||||
| High blood pressure | 39.6 | 45.1 | 51.9 | <0.001 |
| Diabetes | 10.9 | 14.8 | 18.3 | <0.001 |
| Cancer | 10.5 | 9.6 | 10.0 | 0.186 |
| Lung disease | 6.4 | 8.1 | 9.9 | <0.001 |
| Heart Condition | 19.1 | 21.2 | 24.2 | <0.001 |
| Stroke | 6.0 | 7.3 | 9.9 | <0.001 |
| Arthritis | 44.8 | 51.4 | 56.1 | <0.001 |
| Depression║ | 12.2 | 19.7 | 29.5 | <0.001 |
| Self-rated Health, % | ||||
| Good, Very Good, Excellent | 76.0 | 62.2 | 46.7 | <0.001 |
| Baseline Functional Status¶, % | <0.001 | |||
| Independent | 70.9 | 59.8 | 47.3 | |
| 1+ Difficulty, no dependence | 24.4 | 32.7 | 41.8 | |
| 1+ Dependence | 4.7 | 7.5 | 10.9 | |
*Neighborhood Safety categorized according to self-report (very safe = excellent or very good; moderately safe = good; unsafe = fair or poor)
†All percentages reported take into account the sampling weights of the HRS survey
‡p-value calculated using chi-square for categorical variables and trend tests for binary and continuous variables
§Other race/ethnicity includes Native American, Asian and those who identify as “other”
║Depression was measured on non-proxy respondents
¶Functional status includes Activities of Daily Living, walking several blocks, climbing one flight of stairs
Neighborhood Safety, Baseline Functional Status and 10-year Functional Decline
Over 10 years, 10,338 (53.9%) individuals experienced the composite outcome of functional decline (new ADL difficulty or dependence, new mobility difficulty, and/or death). Overall, when compared to perception of a very safe neighborhood, the perception of an unsafe or moderately safe neighborhood at baseline was associated with higher rates of 10-year functional decline. Individuals who perceived their neighborhood to be very safe were less likely to experience functional decline (50.2%) compared to those who perceived their neighborhood to be moderately safe (61.2%) or unsafe (63.6%), P for trend <0.001.
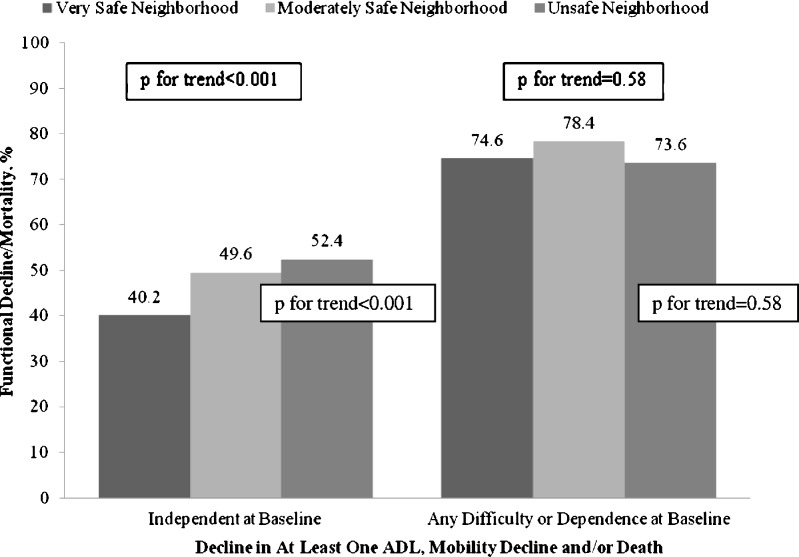
While the relationship between perceived neighborhood safety and functional decline did not differ by wealth (p for interaction = 0.09), the association did differ according to baseline functional status, P for interaction <0.001. Overall, functional decline was experienced by 42.9% of participants who were independent at baseline and 75.5% of individuals who had any ADL or mobility difficulty or dependence at baseline, Figure 1. For participants who were functionally independent at baseline, those who considered their neighborhood to be moderately safe were 15% more likely to experience 10-year functional decline compared to participants who considered their neighborhood to be very safe, even after accounting for sociodemographic and health differences, Table 2. Likewise, participants who were functionally independent at baseline and considered their neighborhood to be unsafe were 21% more likely to experience 10-year functional decline compared to those who perceived their neighborhood to be very safe. For participants who reported any functional impairment at baseline, the relationship between perceived neighborhood safety and 10-year functional decline was not statistically significant, Table 2. Additionally, we performed a sensitivity analysis to determine whether the association between perceived neighborhood safety and functional decline was similar even when we limit our analyses to those that did not move neighborhoods; we found a similar association between perceived neighborhood safety and functional decline in the sensitivity analysis.
Figure 1.
The relationship between perceived neighborhood safety and 10-year functional decline according to baseline functional status. While the relationship between perceived neighborhood safety and functional decline differed according to baseline functional status. Overall, functional decline was experienced by 42.9% of participants who were independent at baseline and 75.5% of individuals who had any ADL or mobility difficulty or dependence at baseline. For participants who were functionally independent at baseline, worse perceived neighborhood safety was associated with a higher 10-year prevalence of functional decline (p for trend <0.001). For participants who reported any functional impairment at baseline, worse perceived neighborhood safety was not associated with a higher prevalence of 10-year functional decline, p for trend = 0.58.
Table 2.
Neighborhood Safety* Was Associated with 10-year Functional Declie for Those Who Were Independent with no Functional Difficulty or Dependence at Baseline
| Baseline Functional Status | Very Safe Neighborhood* (N = 11,742) | Moderately Safe Neighborhood* (N = 4,477) RR (95% CI) | Unsafe Neighborhood* (N = 1,824) RR (95% CI) | |
|---|---|---|---|---|
| Independent† (No difficulty or dependence) | Unadjusted | Reference | 1.23 (1.17, 1.30) | 1.30 (1.19, 1.42) |
| Adjusted‡,§ | Reference | 1.15 (1.09, 1.20) | 1.21 (1.13, 1.31) | |
| Any difficulty or dependence† | Unadjusted | Reference | 1.05 (1.01, 1.09) | 0.99 (0.93, 1.04) |
| Adjusted‡,§ | Reference | 1.00 (0.97, 1.04) | 0.97 (0.92, 1.02) | |
*Neighborhood Safety categorized according to self-report (very safe = excellent or very good; moderately safe = good; unsafe = fair or poor). Participants perceiving their neighborhood to be very safe served as the reference
†Categories of Baseline Functional Status include “Independent” – defined as having no difficulty and no dependence in any ADL or mobility at baseline; versus “Any difficulty or dependence” in any one or more ADL or mobility task
‡Adjusted Relative Risk was generated through a modified Poisson Regression
§Adjusted for age, race/ethnicity, gender, marital status, rural/urban region, education, income, wealth, hypertension, cancer (excluding non-metastatic skin cancers), diabetes mellitus, stroke, lung disease, and heart disease
DISCUSSION
We found that over 1 in 3 older U.S. Americans perceived their neighborhood safety to be fair, poor or good, rather than very good or excellent. We also found that this perception was associated with increased 10-year functional decline for those who were functionally independent at baseline. This relationship remained strong even after accounting for baseline sociodemographics, health and functional status; and it did not differ according to wealth.
To put these findings into context in the current body of research, there are many mechanisms through which perception of poor neighborhood safety could lead to functional decline among older adults. Perception of living in an unsafe neighborhood is associated with physical inactivity16,17 and could lead individuals to become deconditioned, homebound, and/or limit their life-space mobility, all of which have been linked to functional decline.28,29 Our finding that perception of neighborhood safety was associated with 10-year functional decline in older adults who were functionally independent at baseline supports this proposed mechanism. Additionally, perception of an unsafe neighborhood could increase social isolation and depression, experiences which also have been linked to future functional decline.23,24,30,31 Indeed, our findings highlight the association between reported depression and perception of poor neighborhood safety, although the causal direction of this relationship is unclear.
One strength of this work is the inclusion of individuals at all levels of functional status at baseline (independent, difficulty, or dependence), which allowed us to track 10-year functional decline even in individuals with a functional deficit at baseline. Notably, we found that the perception of neighborhood safety was not associated with long-term functional outcomes for those who had functional difficulties or dependence at baseline. This finding might reflect a floor-effect: these individuals started at a lower baseline and therefore did not have as far to decline. However, our use of multiple levels of functional ability enabled us to capture a dynamic process in which individuals who developed a new difficulty or dependence in any ADL or mobility measure were categorized as experiencing functional decline. Others have suggested that life-space restriction (the amount of space that an individual moves through each day) could be an early sign in the development of functional disability.32 In this regard, another explanation for the lack of association between perceived neighborhood safety and functional decline is that that older adults with a functional limitation at baseline are less likely to interact with their environment both at baseline and subsequently such that any perception of their neighborhood’s safety has less of a physical impact on them.
Numerous studies show that exercise-based interventions can improve functional ability, physical functioning, and can lessen functional decline in community-dwelling older adults.33–35 Such interventions might be particularly useful once misconceptions about an inherent relationship between old age and physical inactivity are addressed36 and for those who are beginning to restrict their life space. Our findings suggest that an important next step is to determine whether optimization and targeting of exercise interventions and safe outings to functionally independent older adults who fear for their safety has an impact on their long-term functional health.
We did not find that the relationship between perceived neighborhood safety and functional decline differed by wealth. Wealth has been shown to most fully capture SES in the elderly.37,38 Our finding contrasts those of Clark and colleagues who found that perceived neighborhood crime was only associated with increased 8-year mobility disability in adults aged 65–74 living below the federal poverty line.14 This discrepancy may be due to differences between perception of neighborhood safety and neighborhood crime (perception of neighborhood safety may capture neighborhood conditions beyond crime), differences in our measures of SES, and/or the limited geographic region studied by Clark et al. Since some of the wealthy older adults that perceived their neighborhood to be unsafe may actually live in objectively safe neighborhoods, our finding suggests that it may be the perception of being unsafe, and not just objective measures of an unsafe neighborhood, that affects long-term functional decline.
Several limitations should be considered when interpreting our results. First, HRS uses self-report to collect all data, however self-report is considered a robust measure of disease burden and functional impairment.39,40 Second, perceived neighborhood safety was simply that – a perception – and did not include other objective measures of neighborhood safety such as crime rates or traffic accidents. While this might be viewed as a limitation, we were most interested in the relationship of perception of safety and functional decline, since the mere perception of being unsafe, regardless of objective measures, might lead to differential activity choices and behaviors. Moreover, studies have found that self-reported neighborhood characteristics correspond well with objective neighborhood indicators.15,41,42
This is the first study, to our knowledge, to explore the association between perceived neighborhood safety and long-term functional decline in a large, national population of older Americans. Our findings suggest that asking older patients about their neighborhood safety may provide important information about risk of future functional decline. Moreover, an important next step is to determine whether public health interventions to promote physical activity while addressing safety concerns can help to reduce long-term functional decline in independent older adults.
Acknowledgments
Author Contributions
Study Concept and Design: Sun, Williams.
Acquisition of Data: Williams, Stijacic-Cenzer.
Analysis and Interpretation of Data: Sun, Stijacic-Cenzer, Kao, Ahalt and Williams.
Preparation of Manuscript and Critical Review: Sun, Stijacic-Cenzer, Kao, Ahalt and Williams.
No other parties contributed substantially to this research or to preparation of this manuscript.
Funders
Dr. Williams is supported by the National Institute of Aging (K23AG033102), The UCSF Hartford Center of Excellence, The Jacob and Valeria Langeloth Foundation, and the UCSF Program for the Aging Century. Vivien Sun received funding from the National Institute on Aging and the American Federation for Aging Research through the Medical Student Training in Aging Research (MSTAR) Program. These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. Dr. Williams is an employee of the Department of Veterans Affairs. The opinions expressed in this manuscript may not represent those of the VA.
Prior Presentations
This paper was presented as a poster abstract at the 34th Annual Meeting of the Society for General Internal Medicine on May 5, 2011.
Conflicts of Interest
None disclosed.
REFERENCES
- 1.Krause N. Neighborhood deterioration and self-rated health in later life. Psychol Aging. 1996;11(2):342–352. doi: 10.1037/0882-7974.11.2.342. [DOI] [PubMed] [Google Scholar]
- 2.Malmstrom M, Sundquist J, Johansson SE. Neighborhood environment and self-reported health status: a multilevel analysis. Am J Public Health. 1999;89(8):1181–1186. doi: 10.2105/AJPH.89.8.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 4.Eachus J, Williams M, Chan P, et al. Deprivation and cause specific morbidity: evidence from the Somerset and Avon survey of health. BMJ. 1996;312(7026):287–292. doi: 10.1136/bmj.312.7026.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eames M, Ben-Shlomo Y, Marmot MG. Social deprivation and premature mortality: regional comparison across England. BMJ. 1993;307(6912):1097–1102. doi: 10.1136/bmj.307.6912.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–276. doi: 10.2307/3090214. [DOI] [PubMed] [Google Scholar]
- 7.Stafford M, Chandola T, Marmot M. Association between fear of crime and mental health and physical functioning. Am J Public Health. 2007;97(11):2076–2081. doi: 10.2105/AJPH.2006.097154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitley R, Prince M. Fear of crime, mobility and mental health in inner-city London, UK. Soc Sci Med. 2005;61(8):1678–1688. doi: 10.1016/j.socscimed.2005.03.044. [DOI] [PubMed] [Google Scholar]
- 9.Chandola T. The fear of crime and area differences in health. Health Place. 2001;7(2):105–116. doi: 10.1016/S1353-8292(01)00002-8. [DOI] [PubMed] [Google Scholar]
- 10.Scarborough BK, Like-Haislip TZ, Novak KJ, Lucas WL, Alarid LF. Assessing the relationship between individual characteristics, neighborhood context, and fear of crime. J Crim Justice. 2010;38(4):819–826. doi: 10.1016/j.jcrimjus.2010.05.010. [DOI] [Google Scholar]
- 11.Newhart Smith L, Hill GD. Victimization and fear of crime. Crim Justice Behav. 1991;8(2):217–239. doi: 10.1177/0093854891018002009. [DOI] [Google Scholar]
- 12.Killias M, Clerici C. Different measures of vulnerability and their relation to different dimensions of fear of crime. Br J Criminol. 2000;40(3):437–450. doi: 10.1093/bjc/40.3.437. [DOI] [Google Scholar]
- 13.(Office of Justice Programs). Crimes against persons age 65 and older, 1992–1997. 2000.
- 14.Clark CR, Kawachi I, Ryan L, Ertel K, Fay ME, Berkman LF. Perceived neighborhood safety and incident mobility disability among elders: the hazards of poverty. BMC Publ Health. 2009;9:162. doi: 10.1186/1471-2458-9-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155(6):507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 16.Neighborhood safety and the prevalence of physical inactivity--selected states, 1996. MMWR Morb Mortal Wkly Rep. 1999;48(7):143–6. [PubMed]
- 17.Perceptions of neighborhood characteristics and leisure-time physical inactivity--Austin/Travis County, Texas, 2004. MMWR Morb Mortal Wkly Rep. 2005;54(37):926–8. [PubMed]
- 18.Hebert R. Functional decline in old age. CMAJ. 1997;157(8):1037–1045. [PMC free article] [PubMed] [Google Scholar]
- 19.Carey EC, Covinsky KE, Lui LY, Eng C, Sands LP, Walter LC. Prediction of mortality in community-living frail elderly people with long-term care needs. J Am Geriatr Soc. 2008;56(1):68–75. doi: 10.1111/j.1532-5415.2007.01496.x. [DOI] [PubMed] [Google Scholar]
- 20.Growing Older in America: The Health and Retirement Study. [cited September 9, 2011]; Available from: http://hrsonline.isr.umich.edu/docs/databook/index.php?p=dbook.
- 21.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 22.Murphy TE, Han L, Allore HG, Peduzzi PN, Gill TM, Lin H. Treatment of death in the analysis of longitudinal studies of gerontological outcomes. J Gerontol A Biol Sci Med Sci. 2011;66(1):109–114. doi: 10.1093/gerona/glq188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48(4):445–469. doi: 10.1016/S0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 24.Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52(4):1274–1282. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarkisian CA, Liu H, Gutierrez PR, Seeley DG, Cummings SR, Mangione CM. Modifiable risk factors predict functional decline among older women: a prospectively validated clinical prediction tool. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48(2):170–178. doi: 10.1111/j.1532-5415.2000.tb03908.x. [DOI] [PubMed] [Google Scholar]
- 26.Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 27.Steffick DE. Documentation of affective functioning measures in the health and retirement study. Ann Arbor: HRS Health Working Group; 2000. [Google Scholar]
- 28.Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58(12):2358–2362. doi: 10.1111/j.1532-5415.2010.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peel C, Sawyer Baker P, Roth DL, Brown CJ, Brodner EV, Allman RM. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85(10):1008–1119. [PubMed] [Google Scholar]
- 30.Kamper AM, Stott DJ, Hyland M, Murray HM, Ford I. Predictors of functional decline in elderly people with vascular risk factors or disease. Age Ageing. 2005;34(5):450–455. doi: 10.1093/ageing/afi137. [DOI] [PubMed] [Google Scholar]
- 31.Wang L, Belle G, Kukull WB, Larson EB. Predictors of functional change: a longitudinal study of nondemented people aged 65 and older. J Am Geriatr Soc. 2002;50(9):1525–1534. doi: 10.1046/j.1532-5415.2002.50408.x. [DOI] [PubMed] [Google Scholar]
- 32.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 33.Kemmler W, von Stengel S, Engelke K, Haberle L, Mayhew JL, Kalender WA. Exercise, body composition, and functional ability: a randomized controlled trial. Am J Prev Med. 38(3):279–87. [DOI] [PubMed]
- 34.Morey MC, Snyder DC, Sloane R, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA. 2009;301(18):1883–1891. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim H, Yoshida H, Suzuki T. The effects of multidimensional exercise on functional decline, urinary incontinence, and fear of falling in community-dwelling elderly women with multiple symptoms of geriatric syndrome: A randomized controlled and 6-month follow-up trial. Arch Gerontol Geriatr. 2011;52(1):99–105. doi: 10.1016/j.archger.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 36.Sarkisian CA, Prohaska TR, Davis C, Weiner B. Pilot test of an attribution retraining intervention to raise walking levels in sedentary older adults. J Am Geriatr Soc. 2007;55(11):1842–1846. doi: 10.1111/j.1532-5415.2007.01427.x. [DOI] [PubMed] [Google Scholar]
- 37.Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. Am J Prev Med. 2007;33(3):250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 38.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 39.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 40.Reuben DB, Siu AL, Kimpau S. The predictive validity of self-report and performance-based measures of function and health. J Gerontol. 1992;47(4):M106–M110. doi: 10.1093/geronj/47.4.m106. [DOI] [PubMed] [Google Scholar]
- 41.Elo IT, Mykyta L, Margolis R, Culhane JF. Perceptions of neighborhood disorder: the role of individual and neighborhood characteristics. Soc Sci Q. 2009;90(5):1298. doi: 10.1111/j.1540-6237.2009.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carp FM, Carp A. Perceived environmental quality assessment scales and their relation to age and gender. J Environ Psychol. 1982;2:295–312. doi: 10.1016/S0272-4944(82)80029-7. [DOI] [Google Scholar]