Abstract
Background
Heterotopic ossification (HO) is a well-known complication after total hip and knee arthroplasty. But limited studies have focused on prevalence of HO following cervical total disc arthroplasty (CTDA) and the published data show controversial results.
Objective
The purpose of this review is to investigate the prevalence of HO following CTDA by meta-analysis.
Methods
The literatures were collected from PubMed, Embase and Cochrane library by using keywords as ([disc or disk] and [arthroplasty or replacement]) and (HO or delayed fusion or spontaneous fusion). The original studies were eligible only if the prevalence of HO and of advanced HO (Grade 3–4 according to McAfee) were investigated. A meta-analysis was then performed on collected data. Statistical heterogeneity across the various trials was tested using Cochran’s Q, statistic and in the case of heterogeneity a random effect model was used. Tests of publication bias and sensitivity analysis were also performed.
Results
Our data showed that the pooled prevalence of HO was 44.6% (95% confidence interval (CI), 37.2–45.6%) 12 months after CTDA and 58.2% (95% CI, 29.7–86.8%) 24 months after CTDA, while the advanced HO was 11.1% (95% CI, 5.5–16.7%) and 16.7% (95% CI, 4.6–28.9%), respectively. A significant heterogeneity was obtained. There was no publication bias and individual study had no significant effect on the pooled prevalence estimate.
Conclusion
Higher prevalence of HO was observed following CTDA, although HO was reported to be unrelated to the clinical improvement. It suggests that cervical disc replacement should be performed cautiously before obtaining long-term supporting evidence.
Level of evidence
Prognostic level III.
Keywords: Heterotopic ossification, Meta-analysis, Prevalence, Cervical total disc arthroplasty
Introduction
Anterior cervical discetomy and fusion (ACDF) is a widely accepted intervention for patients with cervical radiculopathy and/or myelopathy who had not responded to conservative treatment [1]. However as a consequence of ACDF, there has been increased reported on adjacent segment degeneration (ASD) [2–4]. Although it is not confirmed that ASD resulted from the natural progression of degenerative disc-disease, it has been recognized that fusion causes increased stress at the adjacent levels [5, 6]. So the cervical total disc arthroplasty (CTDA) after anterior discectomy and decompression has been proposed alternatively to decrease the incidence of ASD through motion preservation at both the index and the adjacent segment [7–9].
Heterotopic ossification (HO) is a well-known complication following total hip and knee arthroplasty [10–12]. It has been considered to hinder the movement of large joint arthroplasty, and to be a main cause of prosthesis to lose the function. McAfee et al. [13] have described and classified HO after total lumbar disc arthroplasty. Their reports showed the prevalence of HO following total lumbar disc arthroplatsy ranged from 1.4 to 15.2% [13]. However, the incidence of HO after CTDA is still under debate. Several groups have reported the prevalence of HO [14, 15], but the results appear controversial. Some studies documented a high incidence of HO following cervical disc arthroplasty [14], while others reported a relatively low incidence [15]. The purpose of the present study is to investigate the incidence of HO in the first 2 years after CTDA in the literature.
Methods
Search strategy
This review was performed based on the standard MOOSE guideline [16]. The literatures were collected from database of PubMed, Embase and Cochrane library ending July 15 2010. The searching string was applied as ([disc or disk] and [arthroplasty or replacement]) and (HO or delayed fusion or spontaneous fusion). The papers eliminated from our data collection were: the papers in non-English publication, papers that focused on lumbar disc arthroplasty, inappropriate topics and review articles as well as case reports. Then from the chosen papers, that did not evaluate the HO as well as the report using the same group of patients, were also excluded. Finally from the remaining articles, the specific exclusion criteria were applied to exclude the study which has samples less than 20 cases, and/or follow-up less than 6 months, and/or the inclusion/exclusion criteria not clearly declared, and/or reporting improper group. We did not collect unpublished data.
Data collection
We recorded following information from each report: country that surgery was performed, published date, number of patients, total segment numbers of disc arthroplasty, criteria on grading HO, prevalence of total HO, prevalence of advanced HO (grade 3–4 according to McAfee et al. [13]), and follow-up periods. The other data, such as mean age of patient population, gender rate, type of prosthesis, single or multi level disc arthroplasty, and whether non-steroid anti-inflammatory drugs (NSAIDS) were used to prevent HO, were also collected.
Quality rating
A published quality system was used to evaluate each study independently, based on a 5-point scale [17]. (1) The clarity of definition of “heterotopic ossification;” (2) the representativeness of the patients’ sample; (3) the credibility of diagnostic criteria of HO; (4) the credibility of diagnostic evaluation: confirm the diagnosis by CT scan; (5) the completeness of outcomes. Quality rated from 1 to 5 using published criteria [17] with one being best and five being worst quality. To avoid introducing bias, we only used articles matching our criteria in the analysis, and used the quality rating to explore the study quality on prevalence values [18].
Heterogeneity test and statistical analysis
In the present study, Cochran’s Q statistic was used to test the heterogeneity of the selected studies. However, because the test is susceptible to the number of trials included in the metaanalysis, we also calculated I2 [19]. I2, directly calculated from the Q statistic (I² = 100% × [Q − df]/Q), describes the percentage of variation across the studies that is due to heterogeneity rather than change. When I2 is <25%, low heterogeneity is assumed, and the effect is thought to be due to change. Conversely, when I2 exceed 25%, then heterogeneity is thought to exist, and the effect is random. We performed publication bias test using the funnel plots method and Begg rank correlation method, as well as Egger weighted regression method by prevalence of total HO and advanced HO. To evaluate the influence of particular article on the pooled estimate, sensitivity analysis (influence analysis) was also performed by which the pooled estimate was calculated by omitting one study each time. Meta-regression was used to analyze the probable origin of heterogeneity by disc arthroplasty level (single- or multi level), the published date of the study and the follow-up periods. All reported confidence intervals (CIs) represented 95% CIs. The statistical analysis was performed by software STATA (Version 10.0).
Results
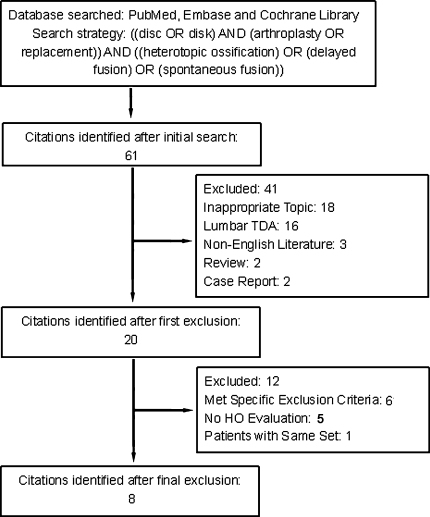
The procedure of data collection is summarized in Fig. 1. Through our search strategy, totally 61 articles were retrieved, and 20 of them were reviewed in the full text format. Finally, eight [14, 15, 20–25] of them matched the inclusion criteria. All these included studies showed the prevalence of HO 12 or 24 months after surgery of CTDA, except one study [20] which evaluated HO prevalence 11 months after surgery. But we still collected this report and assumed it as 12 months. We then separated these articles into 12 and 24 months’ group following CTDA. There was one article [23] where the HO prevalence was evaluated in 12, 24 and 48 months. So we collected it in both the groups. From each article the prevalence of total HO and advanced HO in both groups was extracted. The study did not evaluate either of the parameters was excluded from corresponding analysis group. Meanwhile, the study reported zero value of prevalence, which could not be used to calculate pooled data, was also excluded from the analysis group. The summarized information for each study is listed in Table 1.
Fig. 1.
The procedure and criteria to collect the data
Table 1.
Summary characteristics of different studies: subgroup analysis for pooled prevalence of HO, advanced HO and lost function segments
| References | Journal | Year of publication | Area or country | No. of patients | No. of female patients (%) |
Mean age | Total number of TDA segments | HO criteria | No. and prevalence of HO (95% CI) | No. and prevalence of advanced HO (95% CI) | Level of arthroplasty | Follow-up (month) | Prothesis type | Use of NSAIDS | Study quality* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Leung et al. [15] | Neurosurgery | 2005 | Six European countries | 90 | 39 (43.3) | 45 | 90 | McAfee | 16, 0.178, (0.097–0.258) | 6, 0.067 (0.016–0.118) | Single | 12 | Bryan | Ua | 2b |
| Mehren et al. [14] | Spine | 2006 | Germany/Czech | 54 | U | U | 77 | McAfee | 61, 0.662 (0.556–0.768) | 15, 0.195 (0.107–0.283) | Multi | 12 | ProDisc-C | U | 2b |
| Heidecke et al. [25] | Acta Neurochirurgica | 2008 | Germany | 54 | 32 (59.3) | 46.7 | 59 | McAfee | 17, 0.288 (0.172–0.404) | 5, 0.085 (0.012–0.157) | Multi | 24 | Bryan | U | 2b |
| Beaurain et al. [24] | European Spine Journal | 2009 | France | 68 | 41 (60.1) | 43.9 | 76 | McAfee | 51, 0.671 (0.565–0.777) | 9, 0.118 (0.046–0.191) | Multi | 24 | Mobi-C | U | 2b |
| Suchomel et al.b[23] | European Spine Journal | 2010 | Czech | 54 | 27 (50.0) | 45.3 | 65 | McAfee | 47, 0.723 (0.613–0.833) | 15, 0.231 (0.127–0.335) Multi | 12 | ProDisc-C | Not regularly used | 2b | |
| Suchomel et al.b[23] | European Spine Journal | 2010 | Czech | 54 | 27 (50.0) | 45.3 | 65 | McAfee | 51, 0.785 (0.685–0.885) | 21, 0.323 (0.209–0.437) | Multi | 24 | ProDisc-C | Not regularly used | 2b |
| Yi et al. [21] | Spine | 2010 | Korea | 170 | 65 (38.2) | 43.5 | 172 | McAfee | 69, 0.401 (0.328–0.475) | 15, 0.087 (0.045–0.129) | Multi | >12 | Bryan, Prodics-C,Mobi-C | U | 2b |
| Lee et al. [20] | The Spine Journal | 2010 | Korea | 48 | 21 (43.7) | 44 | 48 | McAfee | 13, 0.271 (0.143–0.398) | 2, 0.042 (−0.015–0.099) | Single | 11 | Bryan and Prestige | 27/48 patients used >3 m | 2b |
| Reyes-Sanchez et al. [22] | SAS Journal | 2010 | Mexico | 25 | 23 (92.0) | 45 | 38 | U | 0 | 0 | Multi | 24 | M6-C | Every patients used 10–14d | 4b |
HO heterotopic ossification, TDA total disc arthroplasty, CI confidence interval, NSAIDS non-steroidal antiinflammatory drugs
* Quality rated from 1 to 5 using published criteria [17] with 1 being best and 5 being worst quality
aUndescribed in the paper
bThese two series were in the same set of patients and published in the same paper
Prevalence of HO 12 months after surgery
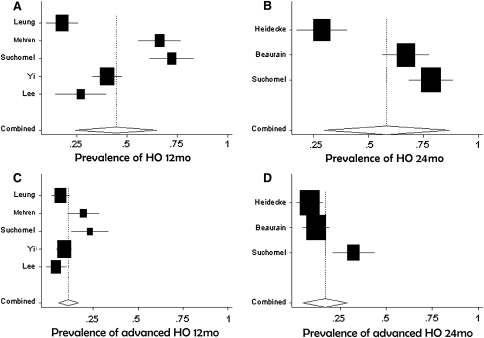
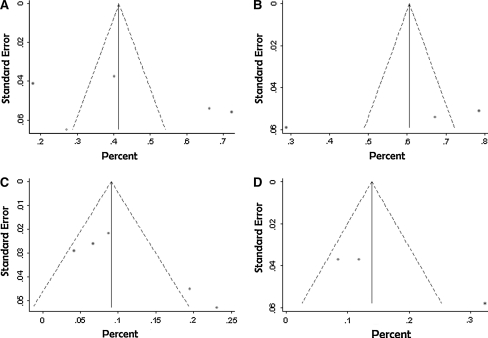
Among all articles, there are five studies [14, 15, 20, 21, 23], which reported the prevalence of total HO and advanced HO 12 months after CTDA, were analyzed based on our criteria. Our data showed that the occurrence of total HO ranged from 17.8 to 72.3% while the pooled prevalence was 44.6% (95% CI, 37.2–45.6%) analyzed by random effect model (Fig. 2). The occurrence of advanced HO ranged from 4.2 to 23.1%, and the pooled prevalence was 11.1% (95% CI, 5.5–16.7%). In Fig. 3 and Table 4, the funnel plots, Begg’s and Egger’s methods show negligible evidence of publication bias (Fig. 3; Tables 2, 3, 4, 5).
Fig. 2.
The prevalence of heterotopic ossification (HO) with 95% confidence intervals (CIs). The prevalence of total HO (a, b) and advanced HO (c, d) was depicted by Forest plots on 12 months group (a, c) and 24 months group (b, d). The vertical line of each plot represented the pooled prevalence. Each study symbol is proportional to the size of the study
Fig. 3.
The publication bias of the analysis. The publication bias of analysis on total (a, b) and advanced (c, d) heterotopic ossification (HO) were expressed by Funnel plots as 12 months group (a, c) and 24 months group (b, d) after CTDA, respectively. No evidence of publication bias was observed
Table 4.
Results of testing for publication bias with the Begg’s test and Egger’s test
| Analysis (months) | Begg’s test | Egger’s test | ||||
|---|---|---|---|---|---|---|
| Kendall’s score | z | P (p > |z|) | Coef. | t | P (p > |t|) | |
| HO (12) | 2 | 0.24 | 0.81 | 8.79 | 0.80 | 0.48 |
| HO (24) | −4 | 1.02 | 0.31 | −13.64 | −1.37 | 0.30 |
| Advanced HO (12) | 4 | 0.73 | 0.46 | 4.74 | 2.33 | 0.10 |
| Advanced HO (24) | 2 | 0.61 | 0.54 | 10.54 | 5.41 | 0.12 |
Table 2.
Results of heterogeneity test with the Cochran’s Q statistic
| Analysis (months) | Q | df | P | I2 |
|---|---|---|---|---|
| HO (12) | 89.77 | 4 | 0.00 | 95.5 |
| HO (24) | 42.74 | 2 | 0.00 | 95.3 |
| Advanced HO (12) | 16.08 | 4 | 0.00 | 75.1 |
| Advanced HO (24) | 12.53 | 2 | 0.00 | 84.0 |
Table 3.
Results of pooled prevalence
| Analysis(months) | Pooled data | Model | |
|---|---|---|---|
| Pooled prevalence (%) | 95% CI (%) | ||
| HO (12) | 44.6 | 37.2–45.6 | Random effect |
| HO (24) | 58.2 | 29.7–86.8 | Random effect |
| Advanced HO (12) | 11.1 | 5.5–16.7 | Random effect |
| Advanced HO (24) | 16.7 | 4.6–28.9 | Random effect |
Table 5.
Results of meta-regression test on impact factors
| Analysis | P value (p > |z|) of meta-regression | ||
|---|---|---|---|
| Level | Published year | Follow-up term | |
| HO | 0.092 | 0.681 | 0.928 |
| Advanced HO | 0.233 | 0.948 | 0.986 |
Prevalence of HO 24 months after surgery
There are three studies [23–25] reporting the prevalence of both total and advanced HO 24 months after CTDA. We showed here the occurrence of total HO ranged from 28.8% up to 78.5% and the pooled prevalence was 58.2% (95% CI, 29.7–86.8%) by random effect model (Fig. 2). The occurrence of advanced HO ranged from 8.5 to 32.3%, and the pooled prevalence was 16.7% (95% CI, 4.6–28.9%). Similarly to 12 months’ group, the funnel plots, Begg’s and Egger’s methods showed negligible evidence of publication bias (Fig. 3; Table 4).
Sensitivity analysis
Through sensitivity analysis, the present study showed that no individual study had marked effect on the pooled prevalence.
Meta-regression
Meta-regression (Table 4) demonstrated that the disc arthroplasty level (single- or multi level), the year of publication and follow-up period did not affect the heterogeneity significantly.
Discussion
The overall outcomes of CTDA were promising compared to ACDF [7, 9], and several studies with randomized controlled trials (RCT) have demonstrated a comparable or even better clinical result in the group of CTDA than that in the control groups treated with ACDF [7–9]. However, due to the ultimate consequence of arthrodesis which results in the loss of movement of the prosthesis, increasing reports started to focus on HO after arthroplasty. As a well-known complication of total hip and knee arthroplasty, HO following total cervical disc arthroplasty is limitedly studied, especially with the large sample and randomized controlled trials. There was a study which indicated that HO is less important in the absence of clinical deterioration [26, 27], while others believed a fused implant in an incorrect position would likely result in overload of the adjacent segment, even worse than ACDF segment [22].
The reported prevalence of HO following total hip arthroplasty ranged from 30.9 to 57% [10, 11, 28]. Based on a large sample prospective study [29], the prevalence of HO 24 months after total lumbar disc arthroplasty was 4.3%, while the prevalence of advanced HO was zero. Compared to above reports, we showed in the present study that the pooled prevalence of total HO is around 44.6% 12 months after CTDA and 58.2% at 24 months. Among this, morbidity of advanced HO is 11.1 and 16.7%, respectively, at 12 and 24 months. It suggests that the pooled prevalence of HO after CTDA is similar to that of total hip arthroplasty, but much higher than that of total lumbar disc arthroplasty. Although the HO prevalence decreased apparently compared with before [30] and HO was reported not to be related with the hinder of clinical improvement [14, 15, 20–25], this result will challenge the principal advantage of cervical arthroplasty to improve the activity of cervical vertebra since advanced HO mostly correlated with loss of function of the implanted prosthesis [14, 15, 23–25]. But till now, no evidence has shown how many mild HO would finally develop to advanced HO, even spontaneous fusion. In addition, there was also no data to assert that non-symptomatic HO indeed has no negative effect on the adjacent segments in the long term. In another words, the potential complications of HO will be against fundamental goal of the CTDA.
The detailed mechanism of ectopic bone formation around joint arthroplasty has not been elucidated yet. Tortolani et al. [29] indicated that the relative low incidence of HO after lumbar arthroplasty was due to minimal retraction and no splitting of the “periarticular” muscle, the iliopsoas. Limited motion of prosthesis might also affect the occurrence of HO [20]. The other study even speculated the existence of somatic or genetic factors on the prevalence of HO [21]. NSAIDs were also reported to be an effective prevention from HO in total hip arthroplasty [31, 32]. However, the most selected publications in our study had no information on the use of NSAIDs (shown in Table 1). Thus, further study should be performed to evaluate the effect of NSAIDs on the incidence of HO.
In summary, the present study observed a higher prevalence of HO following CTDA and advanced HO has been shown to indeed limit the activity of cervical vertebra [14, 15, 23–25]. But we still do not understand the long-term relevance of HO with clinical improvement, since there are still so many confusions on CTDA need to be answered, for example, how many mild HO will develop finally into advanced HO, whether non-symptomatic HO has any effect on the cervical vertebra in the long term, as well as many other important confusions indicated by others [33]. Furthermore, CTDA is also quite expensive for the individual. Based on all these issues, artificial disc in the cervical spine should be applied critically before getting long-term supporting evidences.
Footnotes
C. Jian and W. Xinwei equally contributed to this work.
References
- 1.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discetcomy and arthrodesis for cervical radiculopathy: long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75(9):1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30(19):2138–2144. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 3.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3(6):417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 4.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81(4):519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Reitan CA, Hipp JA, Nguyen L, Esses SI. Changes in segmental intervertebral motion adjacent to cervical arthrodesis: a prospective study. Spine (Phila Pa 1976) 2004;29(11):E221–E226. doi: 10.1097/00007632-200406010-00022. [DOI] [PubMed] [Google Scholar]
- 6.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27(22):2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Goffin J, Calenbergh F, Loon J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Sgrambiglia R, Pointillart V. Intermediate follow-up after treatment of degenerative disc disease with the Bryan cervical disc prosthesis: single-level and bi-level. Spine (Phila Pa 1976) 2003;28(24):2673–2678. doi: 10.1097/01.BRS.0000099392.90849.AA. [DOI] [PubMed] [Google Scholar]
- 8.Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2005;30(10):1165–1172. doi: 10.1097/01.brs.0000162441.23824.95. [DOI] [PubMed] [Google Scholar]
- 9.Pimenta L, McAfee PC, Cappuccino A, Bellera FP, Link HD. Clinical experience with the new artificial cervical PCM (Cervitech) disc. Spine J. 2004;4(6 Suppl):315–321. doi: 10.1016/j.spinee.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Nayak KN, Mulliken B, Rorabeck CH, Bourne RB, Woolfrey MR. Prevalence of heterotopic ossification in cemented versus noncemented total hip joint replacement in patients with osteoarthrosis: a randomized clinical trial. Can J Surg. 1997;40(5):368–374. [PMC free article] [PubMed] [Google Scholar]
- 11.Rama KR, Vendittoli PA, Ganapathi M, Borgmann R, Roy A, Lavigne M. Heterotopic ossification after surface replacement arthroplasty and total hip arthroplasty: a randomized study. J Arthroplasty. 2009;24(2):256–262. doi: 10.1016/j.arth.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Dalury DF, Jiranek WA. The incidence of heterotopic ossification after total knee arthroplasty. J Arthroplasty. 2004;19(4):447–452. doi: 10.1016/j.arth.2003.12.064. [DOI] [PubMed] [Google Scholar]
- 13.McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16(4):384–389. doi: 10.1097/00024720-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 2006;31(24):2802–2806. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]
- 15.Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 2005;57(4):759–763. doi: 10.1227/01.NEU.0000175856.31210.58. [DOI] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 17.Richardson WS, Polashenski WA, Robbins BW. Could our pretest probabilities become evidence based? A prospective survey of hospital practice. J Gen Intern Med. 2003;18(3):203–208. doi: 10.1046/j.1525-1497.2003.20215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282(11):1054–1060. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JH, Jung TG, Kim HS, Jang JS, Lee SH. Analysis of the incidence and clinical effect of the heterotopic ossification in a single-level cervical artificial disc replacement. Spine J. 2010;10(8):676–682. doi: 10.1016/j.spinee.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 21.Yi S, Kim KN, Yang MS, Yang JW, Kim H, Ha Y, Yoon do H, Shin HC. Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976). 2010;35(16):1556–1561. doi: 10.1097/BRS.0b013e3181c6526b. [DOI] [PubMed] [Google Scholar]
- 22.Reyes-Sanchez A, Miramontes V, Olivarez LMR, Aquirre AA, Quiroz AO, Zarate-Kalfopulos B. Initial clinical experience with a next-generation artificial disc for the treatment of symptomatic degenerative cervical radiculopathy. SAS J. 2010;4(1):9–15. doi: 10.1016/j.esas.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suchomel P, Jurak L, Benes V, III, Brabec R, Bradac O, Elgawhary S. Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4-year follow-up. Eur Spine J. 2010;19(2):307–315. doi: 10.1007/s00586-009-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, Steib JP, Vital JM, Aubourg L, Vila T. Intermediate clinical and radiological results of cervical TDR (Mobi-C) with up to 2 years of follow-up. Eur Spine J. 2009;18(6):841–850. doi: 10.1007/s00586-009-1017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heidecke V, Burkert W, Brucke M, Rainov NG. Intervertebral disc replacement for cervical degenerative disease: clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir. 2008;150(5):453–459. doi: 10.1007/s00701-008-1552-7. [DOI] [PubMed] [Google Scholar]
- 26.Bertagnoli R. Heterotopic ossification at the index level after Prodisc-C surgery: what is the clinical relevance? Spine J. 2008;8(5 Suppl):123S. doi: 10.1016/j.spinee.2008.06.687. [DOI] [Google Scholar]
- 27.Janssen M, Goldstein J, Murrey D, Delamarter R. Heterotopic ossifiction at the index level after Prodisc-C: What is the clinical significance? Spine J. 2007;7(5 Suppl):48S–49S. doi: 10.1016/j.spinee.2007.07.117. [DOI] [Google Scholar]
- 28.Nollen JG, Douveren FQ. Ectopic ossification in hip arthroplasty. A retrospective study of predisposing factors in 637 cases. Acta Orthop Scand. 1993;64(2):185–187. doi: 10.3109/17453679308994567. [DOI] [PubMed] [Google Scholar]
- 29.Tortolani PJ, Cunningham BW, Eng M, McAfee PC, Holsapple GA, Adams KA. Prevalence of heterotopic ossification following total disc replacement: a prospective, randomized study of two hundred and seventy-six patients. J Bone Joint Surg Am. 2007;82(1):82–88. doi: 10.2106/JBJS.F.00432. [DOI] [PubMed] [Google Scholar]
- 30.Pointillart V. Cervical disc prosthesis in humans: first failure. Spine (Phila Pa 1976) 2001;26(5):E90–E92. doi: 10.1097/00007632-200103010-00005. [DOI] [PubMed] [Google Scholar]
- 31.Fijn R, Koorevaar RT, Brouwers JR. Prevention of heterotopic ossification after total hip replacement with NSAIDs. Pharm World Sci. 2003;25(4):138–145. doi: 10.1023/A:1024830213832. [DOI] [PubMed] [Google Scholar]
- 32.Sodemann B, Persson PE, Nilsson OS. Prevention of heterotopic ossification by nonsteroid antiinflammatory drugs after total hip arthroplasty. Clin Orthop Relat Res. 1988;237:158–163. [PubMed] [Google Scholar]
- 33.Bartels RH, Donk R, Verbeek AL. No justification for cervical disk prostheses in clinical practice: a meta-analysis of randomized controlled trials. Neurosurgery. 2010;66(6):1153–1160. doi: 10.1227/01.NEU.0000369189.09182.5F. [DOI] [PubMed] [Google Scholar]