Abstract
Introduction
Leg length inequalities (LLI) are a common finding. Rasterstereography offers a non-invasive, contact-free and reliable method to detect the effects of LLIs on spinal posture and pelvic position.
Materials and methods
A total of 115 subjects were rasterstereographically examined during different artificially created leg length inequalities (5–15 mm) using a platform. The pelvic obliquity and torsion and the lateral and frontal deviation of the spine, as well as the surface rotation, were measured.
Results
Changes in platform height led to an increase of the pelvic tilt and torsion. Only minor changes in the spinal posture were found by different simulated leg length inequalities.
Conclusions
Our study showed that there was a correlation between an artificial leg length inequality up to 15 mm and pelvic tilt or torsion, but only minor changes in the spinal posture were measured. Further studies should investigate the effects of greater leg length inequalities on spine and pelvis.
Keywords: Leg length inequality, Posture, Rasterstereography, Pelvic tilt, Pelvic torsion
Introduction
Leg length inequality (LLI) is a condition in which paired limbs are noticeably unequal [14]. In an adult population, between 40 and 70% have an LLI [4, 13] and this may be greater than 2 cm in about 0.1% [13]. Although greater leg length differences are rare, leg length differences of more than 60 mm were found in 14% of the patients who needed treatment because of LLI (>20 mm) [13].
LLI is a common finding in every orthopaedic clinic, but there exists some controversy about the amount of LLI that has a clinical impact on patients [9, 12, 27]. Several authors have described multiple effects of LLI on the human body and the musculoskeletal apparatus. Cummings [4] noted in 1993 that LLI can be a predisposing factor for acute and chronic disorders of the sacroiliac joint. LLI can also be associated with a higher incidence of lumbar back pain [24, 28] and can cause problems in the kinematic chain of various joints [3, 28]. The diagnosis of LLI and its effects on pelvis position and spinal posture are carried out by clinical examination or radiological techniques such as X-ray, CT, ultrasound or MRI. Rasterstereography is a three-dimensional and radiation-free optical imaging procedure for the detection of LLI-related changes on pelvis position and spinal posture. Several studies have shown the high reliability and accuracy of this method [2, 5, 15, 17, 22].
The purpose of this study was to investigate how artificially created leg length inequalities, according to Hackenberg et al. [16], would immediately affect the spinal posture and pelvic position in a healthy collective.
Methods
Volunteers from our orthopaedic clinic were examined for this study. Healthy test subjects without pre-existing leg or spinal abnormalities were included. Exclusion criteria were a pelvic obliquity due to a functional leg length discrepancy and obesity with a body mass index (BMI) >35 kg/m2, which could impede the automatic detection of the anatomical landmarks by the measuring system. Another exclusion criterion was back pain during the previous year lasting longer than 2 days. None of the subjects had any serious medical condition. A total number of 115 subjects (34 male, 81 female) participated in this investigation (Table 1). All subjects were informed about the study both orally and in writing and were given the option to quit participation at any time. The protocol of this study was approved by the local human subject committee of the institute.
Table 1.
Epidemiological data of the subjects
| Parameter | Median | Range (min–max) |
|---|---|---|
| Height (m) | 1.70 | 0.48 (1.48–1.96) |
| Weight (kg) | 68 | 65 (40–105) |
| BMI (kg/m²) | 23.3 | 19 (16–35) |
| Age (years) | 38 | 57 (12–69) |
The three-dimensional analysis of the back surface was conducted with the rasterstereographic device formetric 4D® (Diers International GmbH, Schlangenbad, Germany). Rasterstereography is a method for stereophotogrammetric surface measuring of the back, which was developed in the 1980s by Hierholzer and Drerup [5]. Based on the principle of triangulation, it allows a contact- and radiation-free determination of the body surface [7, 10, 26]. Two cameras, from two different angles, record the back shape. In rasterstereographic measurements, a slide projector used as an optical equivalent of an inverse camera replaces one of the cameras. Parallel white light lines are projected on the back surface of the patient by the slide projector. The three-dimensional back shape leads to a deformation of the parallel light lines, which can be detected by the camera [21]. Anatomical landmarks are hereby automatically captured by assigning concave and convex areas to the curved light pattern [18]. With these anatomical fix points, the system is able to calculate a three-dimensional model of the human spine and clinically relevant parameters, such as the trunk inclination, kyphosis or lordosis angle of the spine, can be determined. The two lumbar dimples (DL and DR) are in close relation to the underlying posterior superior iliac spines [8]. Therefore, it is possible to use them to determine pelvic obliquity. From the orientation of the skin surface over the lumbar dimples, it is also possible to draw conclusions on pelvic torsion around the transverse axis [5].
For the measurements, the subjects were placed on a platform, the height of which could be controlled by the measuring device to simulate different leg lengths (Fig. 1). The weight distribution between the left and the right leg was quantified by the simulation platform prior to the measurement to ensure an almost equal weight distribution between both legs. All subjects waited 60 s to adapt to the simulated leg length discrepancy before starting the measurement. After the recording, the subjects were given 5 min of normal walking time between the measurements to return to a relaxed posture. The recordings were performed whilst subjects were standing in a relaxed posture with fully extended knees on the platform (neutral position). The following leg length differences (right and left leg) were simulated by lifting the platform prior to the rasterstereographic examination: +5, +10 and +15 mm. For purposes of this paper, it is necessary to define certain terms regarding the parameters that were measured with the device:
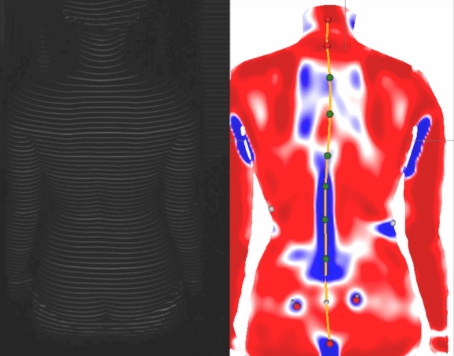
Fig. 1.
A rasterstereographic measurement of a female test subject with a simulated LLI of +15 mm on the right side. The left image shows the back surface of the female test subject with the projected horizontal light lines. This image is then analysed by the computer and transformed into a 3-D surface map of the back surface (right image). The red colour on the back surface represents a convex surface area, while the blue colour stands for a concave surface area
Pelvic tilt (mm)
The different height of the two lumbar dimples (DL to DR) to each other in millimeters. Notation: for a positive value, the right dimple is higher than the left based on a horizontal of the surrounding system.
Pelvic torsion (°)
The torsion of the surface normals on the two lumbar dimples. Notation: a positive pelvic torsion signifies that the right hip bone is oriented further anterior than the left one.
Maximal lateral deviation of the spine (°)
The maximum deviation of the midline of the spine from the direct connection of the VP and DM (DM: middle between DL and DR) in the frontal plane.
Frontal deviation of the spine (mm)
The frontal deviation is the symmetry line of the spine (line between VP and DM) shown in a p.a. view. A positive prefix means a shift of the VP to the right side, a negative prefix to the left side.
Surface rotation of the spine (°)
The maximum value of the horizontal components of the surface normals on the symmetry line.
Data analysis
All data were checked for Gaussian distribution by the Chi-square test and presented as means with standard deviations. Unifactorial ANOVA was calculated to check for changes in the values. The level of significance was set at p < 0.05. Correlation between the measured parameters was calculated using the Pearson correlation. Statistical analysis and graphic presentation were prepared using software SPSS 12.0® (SPSS Inc., Chicago, USA).
Results
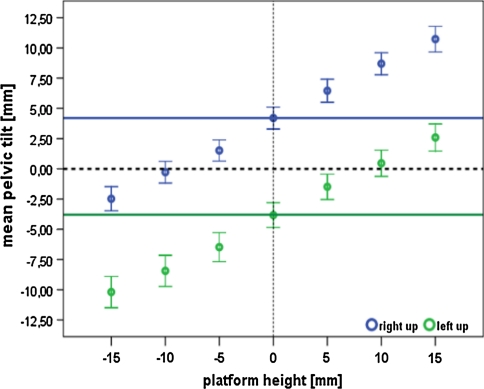
The immediate effects of different simulated leg lengths on spinal posture and pelvis position were evaluated in 115 subjects during this study. We divided all subjects into two groups, based on whether they had a pelvic tilt to the left (left up) or to the right side (right up) in the neutral position of the platform. The mean pelvic tilt in the right-up group was 4.20 mm (3.76–21 mm), and 3.83 mm (3.41–13 mm) in the left-up group for the neutral platform height. Increasing the platform height leads to an increase in pelvic tilt as shown in Fig. 2. Using a paired comparison test, the pelvic tilt changes significantly (p < 0.05 level) in the right-up group between the simulated leg lengths of 0 mm (neutral) and +15 mm. In the left-up group significant changes occur between 0 mm (neutral) and all of the three simulated height differences (+5, +10, +15 mm). For all subjects in both groups, the correlation between pelvic tilt and an increase in platform height is r = 0.63 (p < 0.0001).
Fig. 2.
The mean pelvic tilt (with SD) in mm for the simulated different platform heights (0, 5, 10, 15 mm) for the right-up and left-up group. The figure demonstrates an increase in the mean pelvic tilt by raising the platform height. The blue and green horizontal lines show the mean pelvic tilt for both groups in the neutral position. Negative values of the platform height mean an elevation of the platform on the left side, and positive values mean an elevation on the ride side
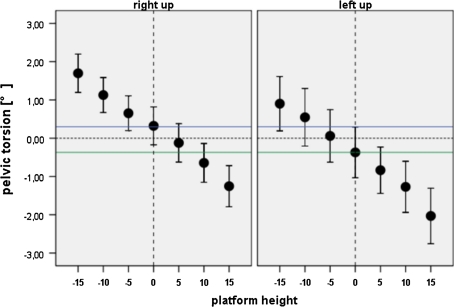
A mean pelvic torsion of 0.32° in the right-up group and of 0.37° in the left-up group was found in the neutral position (Fig. 3). Figure 3 shows that with increasing platform heights, the pelvic torsion increases as well. The correlation for all groups between pelvic torsion and an increase in pelvic tilt is r = −0.40 (p = 0.0001).
Fig. 3.
The mean pelvic torsion in degrees for the different platform heights. For both groups an increase in pelvic torsion by raising the platform can be found
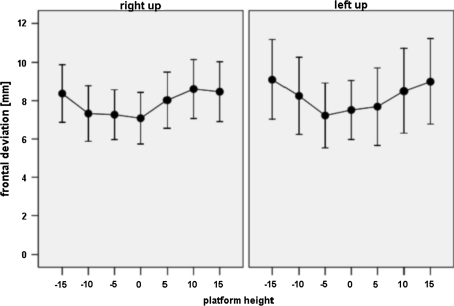
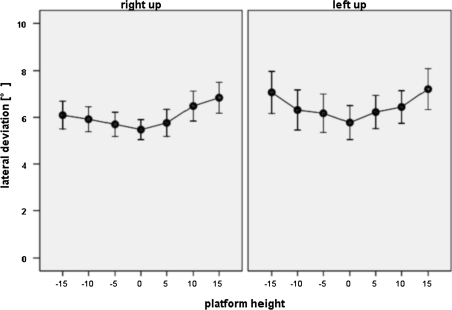
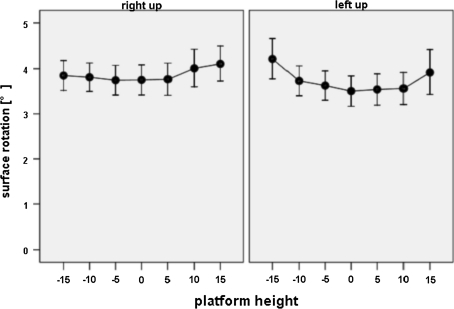
The effects of different leg lengths on the spinal posture were rasterstereographically measured by the frontal (Fig. 4) and lateral deviation (Fig. 5) as well as the surface rotation (Fig. 6). For all different simulated leg lengths, we measured only minor changes (non-significant) in the frontal deviation of the spine, without any linear correlation (Fig. 4). No significant changes and no correlation between different leg lengths and the lateral deviation of the spine were found (Fig. 5). Only greater leg length differences provoked a slight, non-significant, increase of the lateral deviation (Fig. 5). The surface rotation, as an important indicator for scoliosis, was not significantly influenced by different simulated leg lengths (Fig. 6). The measured surface rotation averaged 4° for all different leg lengths in both groups (Fig. 6).
Fig. 4.
Only minor changes of the mean frontal deviation in both groups for the different simulated platform heights
Fig. 5.
Only minor changes of the mean lateral deviation in both groups for the different simulated platform heights
Fig. 6.
Only minor changes of the mean surface rotation in both groups for the different simulated platform heights
Discussion
With rasterstereography, anatomical landmarks on the back surface can be measured with high accuracy by surface curvature analysis [5, 15, 17]. Drerup and Hierholzer [5] showed that the lumbar dimples can be localised by rasterstereography with a standard deviation of ±1 mm. They also stated that the lumbar dimples are in close relation to the pelvis (in particular to the posterior superior iliac spines) and that they can therefore be taken as an indirect indicator for pelvic movements. This thesis was proved by a high correlation (r: 0.99) between lumbar dimple and pelvic movements [6]. In the present study, we have decided to focus on absolute differences of leg lengths independent of the body height and the minimal pre-existing LLDs, to be able to detect directly the effects of different LLDs on the kinematic chain of the dependent body joints.
The mean pelvic tilt was 4.02 mm (4.20 mm for the right-up group and 3.83 mm for the left-up group) in a collective of 115 healthy subjects in our study. Knutson [19, 20] analysed in his review about LLI a total number of 2,731 subjects in nine different studies and found a mean LLI of 5.2 mm in healthy collectives. In a study of Froh et al. [11], a mean LLI of 6.5 mm in 40 patients with a range of 0.5–15 mm was radiologically measured. Brinke et al. [29] have found a mean LLI of 5.4 mm (n = 132) in their study, investigating the influence of LLI and back pain in patients with lumbar herniated discs. One limitation of our study is that our results could not be directly compared with the present literature since we refused to radiologically measure the actual leg length of the healthy subjects due to the accompanying radiation exposure.
There are some studies on the influence of different LLIs on pelvic tilt and pelvic torsion. Lifting one foot induced an anterior rotation of the contralateral hip in a study by Cummings et al. [4] in 1993. They also noted that individual differences in response do exist. Young et al. [30] reported in 2000 that an artificially created LLI significantly increased the pelvic torsion. Other authors, like Pitkin [25] and Beaudoin [1], also confirmed these observations. Our measurements are in accordance with these findings. An artificially induced LLI led to an increase in pelvic tilt and pelvic torsion. But it must be noted that the changes in pelvic tilt occurred in a non-proportional matter, as only approximately half of the simulated lift was passed on the pelvic tilt and even less on the pelvic torsion. These findings were first described by Drerup et al. [8] who stated that the effects of different LLIs are difficult to predict due to complex interactions in the kinematic chain of the lower extremity and the pelvis. Different simulated leg lengths are not always directly transferred to the pelvis. One explanation could be a torsion occurring in the sacroiliac joints. Other explanations could be an anatomical asymmetry of the pelvis or hypertonic suprapelvic muscles [19, 20]. Therefore an over-correction of LLIs could be necessary to level the pelvis. Our study demonstrates that an artificially created LLI leads to an increase of the pelvic tilt and pelvic rotation. A possible explanation might be that due to the artificially induced LLI, the pelvis is pushed down on the femoral heads and must therefore rotate [8, 19, 20]. These findings indicate that a correction of the pelvic obliquity cannot solely be done by levelling the lumbar dimples. A correction of the pelvic torsion seems also to be necessary. Therefore, the pelvic torsion can be helpful to figure out why a correction of an LLI is not passed on to the pelvis.
LLI can not only influence the pelvis, but also spine and posture. With rasterstereography it is possible to detect these effects as well. Our investigation with 115 healthy subjects is one of the largest studies that have examined the immediate effects of an artificially created LLI on pelvis and spine. In 1983, Friberg [9] radiologically examined healthy soldiers and found out that due to LLI and the associated pelvic obliquity, a lateral imbalance of the erected spine can occur [9]. In most cases, this is compensated by a functional scoliosis, with a lumbar convexity to the short leg side. Papaionnou [23] stated in 1982 that the pattern of scoliosis associated with LLI is compensatory, non-structural and non-progressive. When Papaionnou [23] in his study tried to level the pelvis by correcting the LLI, the spine did not become completely straight and an under-correction of the scoliosis was found. In our study, an artificially induced LLI led to only minor changes in the spinal posture. Compared to Papaionnou [23], we found no direct correlation between the amount of LLI and a lateral or frontal deviation of the spine as well as in the surface rotation. An explanation might be that we have only created LLIs between 5 and 15 mm. Although many authors suggest that even small LLIs can create significant changes, it must be assumed that in our study the induced LLIs (5–15 mm) were too small to create changes in posture [1, 4, 8, 9] and that follow-up studies will have to investigate the influence of greater LLIs.
Simulating an acute artificial leg length discrepancy in otherwise healthy individuals without leg length discrepancy does not necessarily correspond to a situation in a real longstanding discrepancy with adaption to it and must therefore be interpreted carefully. Since to our best knowledge there does not exist any data on how artificially created leg length inequalities immediately influence the spinal posture and pelvic position measured with an optoelectronic system, we therefore consider it necessary to examine the effects of different leg lengths in a large healthy collective with an adequate sample size to determine the normal data in a representative population. This reference data will allow further studies to draw conclusions on how real leg length inequalities can be compensated and how the compensation mechanisms may differ from a normal collective. It cannot be excluded that the measured values in this study depend on the age of the subjects. However, it was a collective of healthy volunteers without any limitations in the range of motion due to degenerative joint disease or osteoarthritis. We therefore consider it rather unlikely that there were differences in flexibility and proprioception between the measured individuals.
We are aware that standing on both feet with a 50:50 weight distribution is a rather artificial situation that is rarely the case in daily living. But in clinical practice “at the doctors”, the diagnosis of a pelvic tilt or an LLD still takes place in a static situation. Therefore, we adopted our method to this clinical static situation. Rather often small pelvic tilts are “corrected” by insoles, but in most cases an objective quantification of the pelvic tilt does not take place prior to the prescription of the insoles. In such patients, rasterstereography might be helpful for a recommendation of the height of the shoe insole that has to be used.
Conclusion
With rasterstereography, it seems to be possible to measure the effects of LLI on pelvis and spine. Our study showed that there was a correlation between an artificial LLI up to 15 mm and changes in pelvic tilt and torsion. Only minor changes in the spinal posture were measured for different simulated LLIs up to 15 mm. Further studies should therefore investigate the effects of greater LLIs on spine and pelvis.
Acknowledgments
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
None.
References
- 1.Beaudoin L, Zabjek KF, Leroux MA, Coillard C, Rivard CH. Acute systematic and variable postural adaptations induced by an orthopaedic shoe lift in control subjects. Eur Spine J. 1999;8:40–45. doi: 10.1007/s005860050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Betsch M, Wild M, Jungbluth P, Thelen S, Hakimi M, Windolf J, Horstmann T, Rapp W (2010) The rasterstereographic-dynamic analysis of posture in adolescents using a modified Matthiass test. Eur Spine J 19(10):1735–1939 [DOI] [PMC free article] [PubMed]
- 3.Brunet ME, Cook SD, Brinker MR, Dickinson JA. A survey of running injuries in 1,505 competitive and recreational runners. J Sports Med Phys Fitness. 1990;30:307–315. [PubMed] [Google Scholar]
- 4.Cummings G, Scholz JP, Barnes K. The effect of imposed leg length difference on pelvic bone symmetry. Spine (Phila Pa 1976) 1993;18:368–373. doi: 10.1097/00007632-199303000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Drerup B, Hierholzer E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J Biomech. 1987;20:961–970. doi: 10.1016/0021-9290(87)90325-3. [DOI] [PubMed] [Google Scholar]
- 6.Drerup B, Hierholzer E. Movement of the human pelvis and displacement of related anatomical landmarks on the body surface. J Biomech. 1987;20:971–977. doi: 10.1016/0021-9290(87)90326-5. [DOI] [PubMed] [Google Scholar]
- 7.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines–Part I. Measurement of position and orientation of vertebrae and assessment of clinical shape parameters. J Biomech. 1992;25:1357–1362. doi: 10.1016/0021-9290(92)90291-8. [DOI] [PubMed] [Google Scholar]
- 8.Drerup B, Ellger B, Meyer zu Bentrup FM, Hierholzer E. Functional rasterstereographic images. A new method for biomechanical analysis of skeletal geometry. Orthopade. 2001;30:242–250. doi: 10.1007/s001320050603. [DOI] [PubMed] [Google Scholar]
- 9.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine (Phila Pa 1976) 1983;8:643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Frobin W, Hierholzer E. Analysis of human back shape using surface curvatures. J Biomech. 1982;15:379–390. doi: 10.1016/0021-9290(82)90059-8. [DOI] [PubMed] [Google Scholar]
- 11.Froh R, Yong-Hing K, Cassidy JD, Houston CS. The relationship between leg length discrepancy and lumbar facet orientation. Spine (Phila Pa 1976) 1988;13:325–327. doi: 10.1097/00007632-198803000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Gross RH. Leg length discrepancy: how much is too much? Orthopedics. 1978;1:307–310. doi: 10.3928/0147-7447-19780701-08. [DOI] [PubMed] [Google Scholar]
- 13.Guichet JM, Spivak JM, Trouilloud P, Grammont PM (1991) Lower limb-length discrepancy. An epidemiologic study. Clin Orthop Relat Res, 235–241 [PubMed]
- 14.Gurney B. Leg length discrepancy. Gait Posture. 2002;15:195–206. doi: 10.1016/S0966-6362(01)00148-5. [DOI] [PubMed] [Google Scholar]
- 15.Hackenberg L, Hierholzer E, Liljenqvist U. Accuracy of rasterstereography versus radiography in idiopathic scoliosis after anterior correction and fusion. Stud Health Technol Inform. 2002;91:241–245. [PubMed] [Google Scholar]
- 16.Hackenberg L, Hierholzer E, Bullmann V, Liljenqvist U, Gotze C. Rasterstereographic analysis of axial back surface rotation in standing versus forward bending posture in idiopathic scoliosis. Eur Spine J. 2006;15:1144–1149. doi: 10.1007/s00586-005-0057-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hierholzer E, Hackenberg L. Three-dimensional shape analysis of the scoliotic spine using MR tomography and rasterstereography. Stud Health Technol Inform. 2002;91:184–189. [PubMed] [Google Scholar]
- 18.Huysmans T, Audekercke R, Vander Sloten J, Bruyninckx H, Perre G. A three-dimensional active shape model for the detection of anatomical landmarks on the back surface. Proc Inst Mech Eng H. 2005;219:129–142. doi: 10.1243/095441105X9309. [DOI] [PubMed] [Google Scholar]
- 19.Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part II. The functional or unloaded leg-length asymmetry. Chiropr Osteopat. 2005;13:12. doi: 10.1186/1746-1340-13-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: prevalence, magnitude, effects and clinical significance. Chiropr Osteopat. 2005;13:11. doi: 10.1186/1746-1340-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liljenqvist U, Halm H, Hierholzer E, Drerup B, Weiland M. 3-dimensional surface measurement of spinal deformities with video rasterstereography. Z Orthop Ihre Grenzgeb. 1998;136:57–64. doi: 10.1055/s-2008-1044652. [DOI] [PubMed] [Google Scholar]
- 22.Melvin M, Sylvia M, Udo W, Helmut S, Paletta JR, Adrian S. Reproducibility of rasterstereography for kyphotic and lordotic angles, trunk length, and trunk inclination: a reliability study. Spine (Phila Pa 1976) 2010;35:1353–1358. doi: 10.1097/BRS.0b013e3181cbc157. [DOI] [PubMed] [Google Scholar]
- 23.Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. J Bone Joint Surg Am. 1982;64:59–62. [PubMed] [Google Scholar]
- 24.Perttunen JR, Anttila E, Sodergard J, Merikanto J, Komi PV. Gait asymmetry in patients with limb length discrepancy. Scand J Med Sci Sports. 2004;14:49–56. doi: 10.1111/j.1600-0838.2003.00307.x. [DOI] [PubMed] [Google Scholar]
- 25.Pitkin HC PH (1936) Sacrarthrogenetic telalgia: II. A study of sacral mobility. J Bone Joint Surg Am, 365–374
- 26.Schulte TL, Hierholzer E, Boerke A, Lerner T, Liljenqvist U, Bullmann V, Hackenberg L. Raster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. J Spinal Disord Tech. 2008;21:23–28. doi: 10.1097/BSD.0b013e318057529b. [DOI] [PubMed] [Google Scholar]
- 27.Soukka A, Alaranta H, Tallroth K, Heliovaara M. Leg-length inequality in people of working age. The association between mild inequality and low-back pain is questionable. Spine (Phila Pa 1976) 1991;16:429–431. doi: 10.1097/00007632-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Subotnick SI. Limb length discrepancies of the lower extremity (the short leg syndrome) J Orthop Sports Phys Ther. 1981;3:11–16. doi: 10.2519/jospt.1981.3.1.11. [DOI] [PubMed] [Google Scholar]
- 29.ten Brinke A, Aa HE, Palen J, Oosterveld F. Is leg length discrepancy associated with the side of radiating pain in patients with a lumbar herniated disc? Spine (Phila Pa 1976) 1999;24:684–686. doi: 10.1097/00007632-199904010-00013. [DOI] [PubMed] [Google Scholar]
- 30.Young RS, Andrew PD, Cummings GS. Effect of simulating leg length inequality on pelvic torsion and trunk mobility. Gait Posture. 2000;11:217–223. doi: 10.1016/S0966-6362(00)00048-5. [DOI] [PubMed] [Google Scholar]