Abstract
Purpose
Three column thoracic osteotomy (TCTO) is effective to correct rigid thoracic deformities, however, reasons for residual postoperative spinal deformity are poorly defined. Our objective was to evaluate risk factors for poor spino-pelvic alignment (SPA) following TCTO for adult spinal deformity (ASD).
Methods
Multicenter, retrospective radiographic analysis of ASD patients treated with TCTO. Radiographic measures included: correction at the osteotomy site, thoracic kyphosis (TK), lumbar lordosis (LL), sagittal vertical axis (SVA), pelvic tilt (PT), and pelvic incidence (PI). Final SVA and PT were assessed to determine if ideal SPA (SVA < 4 cm, PT < 25°) was achieved. Differences between the ideal (IDEAL) and failed (FAIL) SPA groups were evaluated.
Results
A total of 41 consecutive ASD patients treated with TCTO were evaluated. TCTO significantly decreased TK, maximum coronal Cobb angle, SVA and PT (P < 0.05). Ideal SPA was achieved in 32 (78%) and failed in 9 (22%) patients. The IDEAL and FAIL groups had similar total fusion levels and similar focal, SVA and PT correction (P > 0.05). FAIL group had larger pre- and post-operative SVA, PT and PI and a smaller LL than IDEAL (P < 0.05).
Conclusions
Poor SPA occurred in 22% of TCTO patients despite similar operative procedures and deformity correction as patients in the IDEAL group. Greater pre-operative PT and SVA predicted failed post-operative SPA. Alternative or additional correction procedures should be considered when planning TCTO for patients with large sagittal global malalignment, otherwise patients are at risk for suboptimal correction and poor outcomes.
Keywords: Spinopelvic alignment, Sagittal vertical axis, Osteotomy, Pedicle subtraction osteotomy, Thoracic, Vertebral column resection
Introduction
Fundamental to the principles of spinal deformity surgery is restoration of spinal alignment. The negative impact of sagittal malalignment with regard to disability, pain, and poor health related quality of life (HRQOL), has been well documented [1–8]. Sagittal spinal deformity is commonly assessed using the sagittal vertical axis (SVA; horizontal distance between a C7 plumbline and the posterior, superior aspect of S1) [9]. However, several authors have emphasized the importance of the pelvis in maintaining global spinal alignment [6, 10–13]. Pelvic retroversion, reflected by an increased pelvic tilt (PT), is a compensatory mechanism to correct positive sagittal malalignment. High PT has been shown to correlate with pain and poor HRQOL [5, 9]. In addition, high PT values can mask the measured amount of sagittal malalignment if pelvic measurements are neglected and only SVA is evaluated, potentially leading to under appreciation of the magnitude of sagittal imbalance and under correction of spinal deformity that may predispose to poor clinical outcomes [14, 15]. Consequently, increasing evidence suggests that SVA alone does not fully reflect the underlying pathology of sagittal malalignment and that assessment of global spino-pelvic alignment (SPA) provides a more complete picture of mechanisms used to maintain upright posture.
Spinal osteotomies are established surgical techniques to correct spino-pelvic malalignment [1, 16, 17]. Reports have demonstrated that improved sagittal spinal alignment following spinal osteotomies correlate with improved HRQOL scores [4]. Spinal osteotomies that provide the greatest amount of correction include osteotomies that involve all three columns of the spine [17], including pedicle subtraction osteotomy (PSO) and vertebral column resection (VCR). PSO typically includes removal of the posterior bony elements, pedicles, and a wedge of bone from the vertebral body, with the apex directed anteriorly. Closure of the osteotomy wedge via posterior column compression increases the degree of lordosis and reduces positive sagittal malalignment. In contrast, posterior VCR (PVCR) typically includes removal of all three spinal columns at the operative level. Correction of positive sagittal malalignment is typically achieved by placement of an undersized cage or interbody device into the anterior aspect of the corpectomy defect and closure of the VCR resection site. Three column osteotomies are most commonly performed in the lumbar spine, and the vast majority of reports have focused on the lumbar spine. Three column osteotomies can also be performed in the thoracic spine in the setting of rigid thoracic deformity [14, 15, 18]. Three column thoracic osteotomy (TCTO) is considerably more technically demanding than three column lumbar osteotomy, primarily due to the risks of spinal cord compromise. Consequently, there are few reports regarding the radiographic and clinical outcomes of TCTO, and existing reports are primarily based on small, single-surgeon or single-institution series [14–19].
Planning for TCTO often focuses on regional correction at the deformity site within the thoracic spine. However, planning for TCTO must also account for the need to achieve global sagittal SPA. The factors important for TCTO surgical planning and the ability of TCTO to restore anatomic sagittal spinal alignment have not been well defined. The objective of the present study was to evaluate risk factors for failure to achieve ideal sagittal SPA following TCTO for adult spinal deformity (ASD) based on a multicenter, consecutive series of patients.
Materials and methods
Patient population
This study was conducted through the International Spine Study Group (ISSG), a multicenter group consisting of 10 sites at which complex ASD surgery is commonly performed. The ISSG has established a prospective, consecutive case spinal osteotomy database for assessing outcomes following complex reconstructive spinal surgery. Prior to enrollment of patients and prior to each study using the database, each study site obtained appropriate Institutional Review Board approval.
This is a multi-center retrospective radiographic analysis of patients treated with TCTO, either thoracic PSO (TPSO) or thoracic PVCR (TPVCR), at ISSG centers. All procedures were performed via a posterior approach, and no osteotomies were performed from an anterior approach. Inclusion criteria included: adults (>18 years) treated for ASD with TCTO (TPSO or TPVCR), and availability of pre- and post-operative full-length antero-posterior (AP) and lateral standing X-rays that included visible femoral heads. Patients with ankylosing spondylitis or spinal deformity resulting from neuromuscular conditions, tumor, or infection were excluded from analysis.
Data collection and radiographic analysis
Pre- and post-operative full-length radiographs were performed with patients in a free-standing posture with elbows flexed at approximately 45° and fingertips on the clavicles [20, 21]. Radiographic measurements were performed using SpineView software (SurgiView®, Paris, France) [22, 23]. Focal coronal and sagittal degrees of correction achieved by the osteotomy were assessed using the Cobb angle between the inferior endplate of the vertebra above the TCTO level and the superior endplate of the vertebra below the TCTO level (Fig. 1). Regional radiographic measurements of sagittal alignment included thoracic kyphosis (TK, T4-T12 Cobb angle), thoracolumbar kyphosis (TLK, T10-L1 Cobb angle), and lumbar lordosis (LL, L1-S1 Cobb angle; Fig. 2). Global radiographic measurements included sagittal vertical axis (SVA), T1 spinopelvic inclination (T1-SPI), and T9 spinopelvic inclination (T9-SPI; Fig. 2). Pelvic parameters measured included: pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS; Fig. 3). To facilitate analysis, patients were divided into the primary plane of spinal deformity; sagittal, coronal or mixed plane deformity.
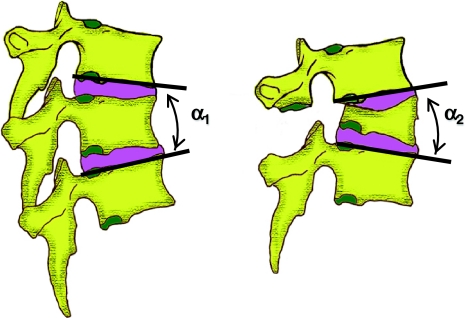
Fig. 1.
Method used to calculate degree of sagittal correction at the osteotomy site. The difference between the two angles, α1 and α2, reflects the degree of focal sagittal correction. The degree of coronal correction at the osteotomy site was determined using a similar approach based on antero-posterior imaging
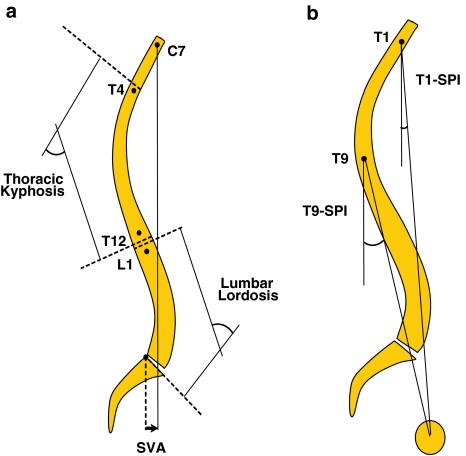
Fig. 2.
Definition of sagittal spino-pelvic parameters, including thoracic kyphosis, lumbar lordosis, and sagittal vertical axis (SVA) in (a), and T1 spino-pelvic inclination (T1-SPI) and T9 spino-pelvic inclination (T9-SPI) in (b). Circle in bottom right corner of b depicts the femoral head. (Reprinted with permission from: Schwab F, et al. Gravity line analysis in adult volunteers. Spine 31(25):E959–E967, 2006)
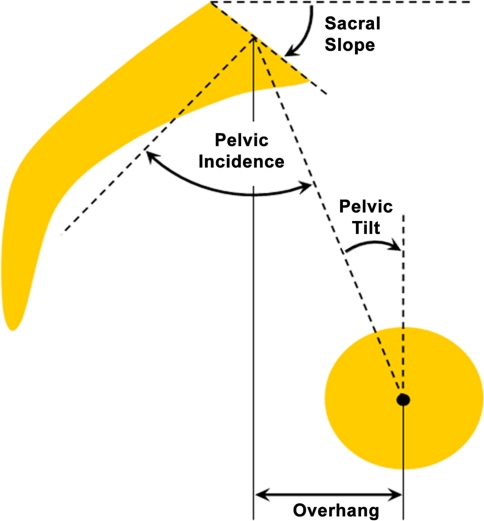
Fig. 3.
Definition of pelvic parameters, including sacral slope (SS), pelvic incidence (PI), and pelvic tilt (PT), based on the center of the femoral head (dark, solid circle) and the sacrum. (Reprinted with permission from: Schwab F, et al. Gravity line analysis in adult volunteers. Spine 31(25):E959–E967, 2006)
Statistical analysis
Demographic, surgical, and radiographic parameters were evaluated using descriptive statistics of means, standard deviations, and 95% confidence intervals. The Shapiro-Wilks test was used to assess the normality of the data. Post-operative SVA and PT were assessed for each patient to determine sagittal SPA and to define two patient groups. Patients with ideal post-operative SPA (SVA < 4 cm and PT < 25°) were classified as IDEAL, and patients with SVA > 4 cm and PT > 25° were classified as FAIL. Demographic, surgical, and radiographic parameters were compared between the IDEAL and FAIL groups, as well as between patients treated with PSO versus VCR, using a t test, with threshold of significance set at P < 0.05.
Results
Demographic and operative data
Between 2003 and 2009, 41 consecutive patients, mean age 39.1 years (SD = 18.3 years), received 43 TCTOs. Eighteen patients received TPSO and 23 patients received TPVCR. The patient group included 31 women and 10 men. 26 (63%) patients had no prior spine surgery. Diagnoses included: adult idiopathic scoliosis (n = 19), thoracic hyperkyphosis (n = 14), congenital scoliosis (n = 4), proximal junctional kyphosis (n = 2), and deformity following compression fracture (n = 2). The primary plane of deformity at the time of surgery was sagittal (n = 21), coronal (n = 13), or multi-planar (n = 7). Minimum one osteotomy was performed at every level of the thoracic spine from T2 through T12 (Fig. 4). The mean number of fused levels was 13.5 (SD = 3.4). Based on the Shapiro-Wilk test all parameters assessed were normally distributed (P > 0.05).
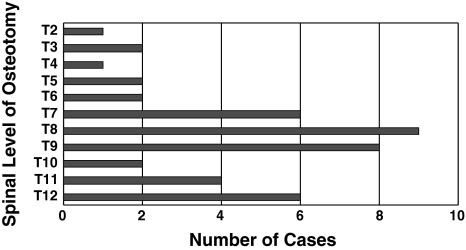
Fig. 4.
Distribution of 43 TCTO procedures performed in 41 adults for treatment of spinal deformity
Radiographic outcomes
The mean focal coronal correction achieved at the osteotomy level was 9.5° (SD = 8.2°) for all patients, and was 14.8° (SD = 8.1°) for patients with primarily coronal or multi-planar deformity. The mean focal sagittal correction achieved at the osteotomy level was 14.4° (SD = 14.6°) for all patients and was 20.8° (SD = 11.8°) for patients with primarily sagittal or multi-planar deformity. Post-operative TK, TLK, maximum coronal Cobb angle, SVA, and PT improved from pre-operative values (Table 1). Pre and post-operative PI and LL were similar.
Table 1.
Comparison of pre- and post-operative radiographic parameters in 41 adults with spinal deformity treated with three column thoracic osteotomy
| Radiographic parameter (SD) | Pre-operative | Post-operative | P* |
|---|---|---|---|
| Thoracic kyphosis (°) | −62 (25) | −37 (12) | <0.001 |
| Thoracolumbar kyphosis (°) | −15 (24) | −6 (11) | 0.006 |
| Maximum coronal Cobb angle (°) | 56 (32) | 24 (17) | <0.001 |
| Sagittal vertical axis (mm) | 24 (74) | −2 (51) | 0.002 |
| Pelvic incidence (°) | 51 (12) | 51 (12) | 0.829 |
| Pelvic tilt (°) | 15 (13) | 11 (12) | <0.001 |
| Lumbar lordosis (°) | 63 (18) | 60 (13) | 0.314 |
* P values based on two-tailed, paired t test
The mean coronal correction at the osteotomy site was similar for patients treated with TPSO (n = 18, mean = 9.4°, SD = 9.5°) and patients treated with TPVCR (n = 23, mean = 9.7°, SD = 7.3°; P = 0.923). The mean sagittal correction at the osteotomy site was similar for patients treated with TPSO (n = 18, mean = 12.8°, SD = 14.4°) and patients treated with TPVCR (n = 23, mean = 15.6°, SD = 14.9°; P = 0.559).
Ideal post-operative SPA was achieved in 32 (78%) patients (Fig. 5). Nine patients (22%) were classified as FAIL SPA (mean post-operative SVA = 4.6 cm, SD = 6.1 cm; mean post-operative PT = 25.8°, SD = 8.8°).
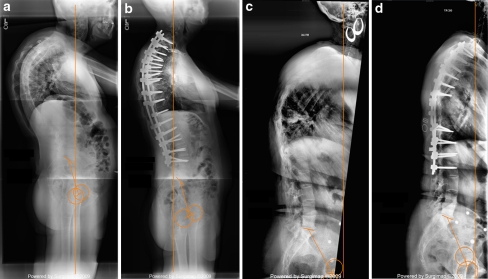
Fig. 5.
Pre- (a) and post-operative (b) full length sagittal radiographs of a patient with fixed thoracic kyphosis with good post-operative spino-pelvic alignment following thoracic pedicle subtraction osteotomy (TPSO). Pre- (c) and post-operative (d) full length sagittal radiographs of a patient with fixed thoracic kyphosis with poor post-operative spino-pelvic alignment following TPSO. Note the substantial positive sagittal malalignment, high pelvic tilt, and relative lack of lumbar lordosis for the patient in (c). Vertical line is the C7 plumb line. Circles represent femoral heads
Comparison of IDEAL and FAIL patient groups
One patient in the FAIL group (11%) was treated with TPSO and 8 (89%) were treated with TPVCR. 17 patients in IDEAL (53%) were treated with TPSO and 15 (47%) were treated with TPVCR. The osteotomy level was T2–T6 in 2 (22.2%) and T7–T12 in 7 (77.8%) of the patients in the FAIL group and was T2–T6 in 5 (15.6%) and T7-T12 in 27 (84.4%) of the patients in the IDEAL group (P = 0.637). The IDEAL and FAIL groups had similar numbers of spine levels fused (P = 1.000), similar percentage of patients fused to the sacrum (IDEAL = 87.5%, FAIL = 66.7%, P = 0.165), similar coronal correction at the osteotomy site (IDEAL = 10.2°; FAIL = 7.1°; P = 0.327) and similar sagittal correction at the osteotomy site (IDEAL = 13.0°; FAIL = 19.1°; P = 0.336). IDEAL and FAIL groups had similar pre- and post-operative TK and similar change in TK following TCTO (Table 2). Correction of SVA, PT, LL, and PI-LL mismatch following TCTO was similar between IDEAL and FAIL (Table 2). The FAIL group had significantly greater pre- and post-operative SVA, PT, PI, and PI-LL mismatch and had significantly lower pre- and post-operative LL than IDEAL (Table 2).
Table 2.
Comparison of pre- and post-operative radiographic parameters in 41 adults with spinal deformity treated with three column thoracic osteotomy, stratified based on success of achieving ideal post-operative sagittal spino-pelvic alignment
| Parameter (SD) | Pre-operative | Post-operative | Change | ||||||
|---|---|---|---|---|---|---|---|---|---|
| IDEAL | FAIL | P** | IDEAL | FAIL | P** | IDEAL | FAIL | P** | |
| Sagittal vertical axis (°) | 6 (53) | 89 (103) | 0.002 | −16 (39) | 46 (61) | 0.001 | −22 (43) | −43 (75) | 0.272 |
| Pelvic tilt (°) | 11 (10) | 31 (8) | <0.001 | 7 (9) | 26 (9) | <0.001 | −4 (5) | −5 (6) | 0.667 |
| Thoracic kyphosis (°) | −60 (27) | −67 (19) | 0.465 | −37 (12) | −37 (16) | 0.875 | 24 (23) | 30 (25) | 0.486 |
| Lumbar lordosis, LL (°) | 66 (16) | 50 (21) | 0.021 | 63 (10) | 50 (17) | 0.005 | −3 (13) | −1 (24) | 0.712 |
| Pelvic incidence, PI (°) | 49 (12) | 59 (9) | 0.018 | 49 (11) | 59 (10) | 0.011 | 0 (2) | 0 (2) | 0.696 |
| PI - LL (°) | −17 (20) | +9 (10) | 0.001 | −15 (12) | +10 (9) | <0.001 | +3 (14) | +1 (22) | 0.753 |
IDEAL and FAIL reflect patients in which ideal post-operative sagittal spino-pelvic alignment was and was not achieved, respectively. See text for definitions. SD = standard deviation
** P values based on two-tailed, paired t test. Significant P values are shown in bold
Discussion
This study provides a radiographic assessment of factors associated with failure to achieve adequate post-operative sagittal spino-pelvic alignment following TCTO for ASD. TCTO significantly decreased the mean TK, maximum coronal Cobb angle, SVA and PT. However, 22% of patients had spino-pelvic malalignment following TCTO, a finding known to correlate with poorer clinical outcome [5, 9]. IDEAL and FAIL patients had similar operative procedures and similar degrees of regional correction, however FAIL patients had greater pre-operative sagittal malalignment. Consequently, these data suggest that additional or alternative correction procedures should be considered when planning TCTO for patients with large spino-pelvic malalignment to reduce the risk of residual post-operative deformity and poor outcomes.
Few reports have addressed the use of TCTO in ASD. The majority of data that does exist on TCTO for ASD includes small case series from a single institution or reports that include thoracic procedures as part of a series of lumbar PSO (LPSO) procedures. O’Shaughnessy et al. [14] reported on 25 TPSOs performed in 15 ASD patients. Improvements were demonstrated in TK (75.7° to 54.3°, P < 0.005) and SVA (106.1 to 38.8 mm, P < 0.005) post-operatively. Mean sagittal correction at the osteotomy site was 16.3°. Correction was greater for more caudal TPSO levels (mean correction 10.7° for T2–T4 TPSO, 14.7° for T5–T8, and 23.9° for T9–T12). The authors noted that TPSOs in lower thoracic segments provide greater sagittal correction, due to the morphology and greater size of these vertebral bodies, and concluded that their current practice is to perform TPVCRs for corrections between T2 and T10 to achieve greater correction.
The present series offers multiple contrasts with that of O’Shaughnessy et al. [14]. The current study provides a substantially greater number of patients, is a multi-center investigation, and includes both TPSOs and TPVCR procedures. Although the mean number of osteotomies per patient was considerably lower in the present series (1.05) compared with that of O’Shaughnessy et al. (1.67), the degree of sagittal correction for cases with primarily sagittal or multi-planar deformity was comparable, 20.8° versus 16.3°, respectively. The present series does not provide support for the supposition of O’Shaughnessy et al., that TPVCR enables a more robust correction than TPSO, as we identified no significant differences in focal correction at the osteotomy site between the TPVCR and TPSO groups. Compared with patients treated with TPSO, those treated with TPVCR had a non-significant trend toward greater risk of poor post-operative SPA. The direction of this trend is unexpected, and it is possible that unappreciated differences in technique or patient selection may account for this finding. In addition, because the series of O’Shaughnessy et al. does not provide assessment or discussion of pelvic parameters, it is unclear whether residual sagittal malalignment may have been masked by increased pelvic retroversion (elevated PT).
Yang et al. reported a series of 35 adults with ASD treated with PSO (28 LSPO, 7 TPSO) [15]. They reported significant improvement in focal correction at the osteotomy site, TK, and SVA for patients treated with LPSO. However, they noted only significant improvement in focal correction at the osteotomy site, not TK or SVA, for patients treated with TPSO. They concluded that LPSO offers potential significant improvement of focal, regional, and global spinal alignment, whereas TPSO was only associated with improved alignment at the osteotomy site. These findings contrast with the present series, in which significant improvement in focal, regional, and global alignment were identified following TCTO. This contrast may reflect differences in technique or the relatively small number of patients treated with TPSO in the study by Yang et al. Alternatively, the significant degree of sagittal malalignment in the patient population treated with TPSO by Yang et al. (mean pre-operative SVA = 127 mm) may have been incompletely corrected with a single level TPSO. This latter explanation is consistent with the primary conclusion of the present study; additional or alternative correction procedures should be considered when planning TCTO for patients with substantial spino-pelvic malalignment. Other reports have documented TPSO and TPVCR as treatments for ASD [16, 18]. However, these cases have typically been included as only a small subset of a larger study of LPSO, and primarily included only distal thoracic (T11 or T12) osteotomies, substantially limiting the ability to provide meaningful comparisons to the present series.
The importance of achieving spinal alignment in ASD surgery has been well established [2–6, 9, 12, 13, 24]. Glassman et al. correlated radiographic findings with standardized HRQOL measures in 298 ASD patients, including 172 with and 126 without history of prior spine fusion [2]. Positive sagittal malalignment proved to be the most reliable predictor of clinical symptoms in both patient groups. The importance of the pelvis in regulating spinal alignment has also been established [9, 11–13, 25]. LaFage et al. prospectively correlated spino-pelvic radiographic parameters and HRQOL measures in 125 adults with spinal deformity. The strongest correlations with poor HRQOL measures were SVA, T1 spino-pelvic inclination, and PT [5].
Strengths of the present study include the multicenter design and relatively large number of patients. The contribution of cases to the present series from multiple surgeons across the United States strengthens the generalizability of our findings and conclusions. The primary limitations of this study are the retrospective design and the lack of direct correlations with HRQOL measures. Since this study is based on radiographic review, the retrospective design should have limited impact. Correlations between sagittal spinal alignment and HRQOL measures have been reported in multiple prior studies and have been discussed in the present study for context. Efforts are currently underway to provide prospective clinical outcomes assessment following TCTO.
Conclusion
TCTO is an effective procedure to correct rigid thoracic spinal deformities. Planning for these procedures often focuses upon regional correction at the osteotomy site. Failure to consider global SPA may result in sub-optimal SPA. Poor final SPA in this study occurred in 22% patients, despite similar operative procedures and regional deformity correction as patients who achieved ideal post-operative SPA. High pre-operative PT and SVA predicted failed post-operative SPA. Additional or alternative correction procedures should be considered when planning TCTO for patients with significant spino-pelvic malalignment.
Acknowledgments
Study group support provided by Depuy Spine.
Conflict of interest
None.
References
- 1.Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85-A:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 3.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 4.Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976) 2007;32:2189–2197. doi: 10.1097/BRS.0b013e31814b8371. [DOI] [PubMed] [Google Scholar]
- 5.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 6.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–1578. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 7.Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959–E967. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 8.Smith JS, Fu KM, Urban P, Shaffrey CI. Neurological symptoms and deficits in adults with scoliosis who present to a surgical clinic: incidence and association with the choice of operative versus nonoperative management. J Neurosurg Spine. 2008;9:326–331. doi: 10.3171/SPI.2008.9.10.326. [DOI] [PubMed] [Google Scholar]
- 9.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupere G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg. 2005;71:213–220. [PubMed] [Google Scholar]
- 11.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupere G, Pelissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 13.Gottfried ON, Daubs MD, Patel AA, Dailey AT, Brodke DS. Spinopelvic parameters in postfusion flatback deformity patients. Spine J. 2009;9:639–647. doi: 10.1016/j.spinee.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 14.O’Shaughnessy BA, Kuklo TR, Hsieh PC, Yang BP, Koski TR, Ondra SL. Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976) 2009;34:2893–2899. doi: 10.1097/BRS.0b013e3181c40bf2. [DOI] [PubMed] [Google Scholar]
- 15.Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5:9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 16.Mummaneni PV, Dhall SS, Ondra SL, Mummaneni VP, Berven S. Pedicle subtraction osteotomy. Neurosurgery. 2008;63:171–176. doi: 10.1227/01.NEU.0000325680.32776.82. [DOI] [PubMed] [Google Scholar]
- 17.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31:S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 18.Loon PJ, Stralen G, Loon CJ, Susante JL. A pedicle subtraction osteotomy as an adjunctive tool in the surgical treatment of a rigid thoracolumbar hyperkyphosis; a preliminary report. Spine J. 2006;6:195–200. doi: 10.1016/j.spinee.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Ikenaga M, Shikata J, Takemoto M, Tanaka C. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine. 2007;6:330–336. doi: 10.3171/spi.2007.6.4.8. [DOI] [PubMed] [Google Scholar]
- 20.Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36” radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 21.Marks MC, Stanford CF, Mahar AT, Newton PO. Standing lateral radiographic positioning does not represent customary standing balance. Spine (Phila Pa 1976) 2003;28:1176–1182. doi: 10.1097/01.BRS.0000067271.00258.51. [DOI] [PubMed] [Google Scholar]
- 22.El Fegoun AB, Schwab F, Gamez L, Champain N, Skalli W, Farcy JP. Center of gravity and radiographic posture analysis: a preliminary review of adult volunteers and adult patients affected by scoliosis. Spine (Phila Pa 1976) 2005;30:1535–1540. doi: 10.1097/01.brs.0000167534.49069.e9. [DOI] [PubMed] [Google Scholar]
- 23.Rillardon L, Levassor N, Guigui P, Wodecki P, Cardinne L, Templier A, Skalli W. Validation of a tool to measure pelvic and spinal parameters of sagittal balance. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:218–227. [PubMed] [Google Scholar]
- 24.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 25.Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP (2011) Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976) 36(13):1037–1045 [DOI] [PubMed]