Abstract
Introduction
Surgical treatment is mandatory for spinal pseudarthrosis in advanced ankylosing spondylitis (AS) patients with painful sagittal deformity and/or neurological deficits. However, the most effective and safe surgical procedure for AS-related symptomatic thoracolumbar pseudarthrosis is still controversial. The purpose of this study is to explore the outcomes of pedicle subtraction osteotomy (PSO) at the level of pseudarthrotic lesion combined with supplemental anterior fusion for patients suffering from kyphotic pseudarthrosis in AS.
Materials and methods
Seven AS patients with thoracolumbar pseudarthrosis and kyphotic deformity were reviewed. There were 6 males and 1 female with a mean age of 41.7 years. All patients had back pain. Imaging findings demonstrated 3-column extensive discovertebral destruction in all patients. The preoperative global kyphosis averaged 75° (range, 37°–114°) with the apex at the level of pseudarthrosis. Three patients had incomplete neurological deficits (Frankel D) preoperatively. All patients underwent PSO at the level of pseudarthrosis in the first stage followed by supplemental anterior fusion in the second stage. Radiographic and clinical outcomes were assessed with an average follow-up of 38 months (range, 24–59 months). The visual analogue scale (VAS) was compared before surgery and at the final follow-up.
Results
All patients showed significant pain relief postoperatively and were satisfied with the kyphosis correction as well. Solid bony fusion was shown at the final follow-up. Three patients with neurological deficits had complete recovery of neurological function. The global kyphosis was corrected from 75º to 30º, with a mean correction of 45º. The VAS showed significant improvement. No surgical complication was observed.
Conclusion
PSO can be safely performed through the site of pseudarthrotic lesion in AS patients with pseudarthrosis and kyphotic deformity. After PSO, supplemental anterior fusion is sometimes necessary to support the anterior and middle column in a second stage if there is a bone defect in the osteotomy site.
Keywords: Ankylosing spondylitis, Pseudarthrosis, Osteotomy
Introduction
Ankylosing spondylitis (AS) is a systemic inflammatory disease predominantly affecting the sacroiliac joints and spine [10, 12]. The chronic inflammation causes progressive ossification of the spinal ligaments and facet joints, which eventually results in a fixed and rigid spine [7, 8, 15]. In addition, AS is also associated with vertebral osteoporosis [18]. Therefore, AS patients in advanced stage are more susceptible to fracture due to the rigidity of the ossified spine and osteoporosis [18, 19, 22]. A stress fracture is most likely to occur in thoracolumbar junction, a region with tremendous stress forces concentrated [4]. Persistent and abnormal motion at the stress fracture site makes spontaneous healing difficult, which leads to the formation of pseudarthrosis [20]. Pseudarthrosis may complicate with a progressive kyphotic deformity causing sagittal imbalance and considerable disturbances of posture [16, 23]. Additionally, it may associate with severe back pain, progressive myelopathy, and neurologic sequelae [1, 4, 14].
Surgical treatment is mandatory for patients with AS-related thoracolumbar pseudarthrosis, who present with painful thoracolumbar kyphosis, neurological deficits, and sagittal imbalance [16, 23]. The goals of surgical treatment are to restore sagittal alignment, to correct the kyphotic deformity and to achieve solid fusion of pseudarthrosis [23]. However, there is controversy regarding the optimal surgical procedure. Some authors believe that anterior fusion allows direct access to the anterior lesion [11, 16], whereas others consider that pseudarthrosis can be treated effectively by posterior, transpedicular wedge resection osteotomy at the level of pseudarthrosis and fixation without supplemental anterior fusion [4, 23]. Most surgeons recommend combined anterior and posterior approach for the treatment of pseudarthrosis and kyphotic deformity [6, 16].
In several previous surgical series, authors were most concerned about the pathogenesis, histopathological correlation of clinical, radiographic, and surgical findings of pseudarthrosis [11, 16, 25]. To the best of our knowledge, few have studied the outcomes of pedicle subtraction osteotomy (PSO) at the level of pseudarthrosis in advanced AS patients associated with thoracolumbar kyphosis. The purpose of this study is to evaluate the effectiveness of PSO through pseudarthrosis in the correction of the concomitant thoracolumbar kyphotic deformity complicating AS. Special attention is given to answer the following questions: (1) whether osteotomy at the pseudarthrosis segment can achieve the optimal restoration of the sagittal balance; (2) whether supplementary anterior interbody fusion is needed after PSO; (3) and whether such procedure may increase the risks of neurological complications.
Materials and methods
Seven consecutive AS patients with pseudarthrosis at the thoracolumbar kyphotic apex were reviewed. There were 6 males and 1 female with a mean age of 41.7 years (range 29–52 years).
Suddenly increased low back pain developed in 3 patients without preceding trauma. The symptoms were aggravated when standing or walking but relieved by lying down. The other 4 patients presented with localized pain around the pseudarthrotic lesion after a minor trauma, with poor response to the analgesics; these 4 patients also complained of progressive thoracolumbar kyphosis.
Of these 7 patients, 3 had neurological deficits as graded as Frankel D. On examination, 2 patients (Patient 4 and 7, Table 1) had significant decreases in muscle power (4/5), pinprick sensation and tendon reflex in the bilateral lower extremities. Another patient (Patient 6, Table 1) had motor loss (4/5) of the left leg with normal sensation and reflex.
Table 1.
Clinical data in AS patients with thoracolumbar pseudarthrosis
| Patient | Age/gender | Level of pseudarthrosis | History of injury | Neurologic function Initial/final follow-up |
Surgery | Outcome (VAS) Initial/final follow-up |
|---|---|---|---|---|---|---|
| 1 | 50/M | T11-T12 | Fall | Intact | PSO + AF | 6/0 |
| 2 | 41/F | T12-L1 | None | Intact | PSO + AF | 7/0 |
| 3 | 52/M | T12-L1 | Fall | Intact | PSO + AF | 7/0 |
| 4 | 29/M | T12-L1 | Fall | Frankel D/Frankel E | PSO + AF | 10/0 |
| 5 | 52/M | T12-L1 | Fall | Intact | PSO + AF | 7/0 |
| 6 | 32/M | T11-T12 | None | Frankel D/Frankel E | PSO + AF | 8/0 |
| 7 | 36/M | T11-T12 | None | Frankel D/Frankel E | PSO + AF | 5/0 |
PSO pedicle subtraction osteotomy, AF anterior fusion, VAS visual analogue scale
Radiologic assessment
All patients were referred for radiographic, CT and MRI examinations (Fig. 1) and the Charcot spinal lesions were ruled out according to these image studies. All patients had 3-column involved pseudarthrosis located from T11 to L1 levels (T11-T12 in 3 patients, T12-L1 in 4 patients) (Table 1).
Fig. 1.
A 41-year-old woman with severe disabling thoracolumbar kyphosis. She had a global kyphosis of 46° at the age of 39 years (a). Two years later, she presented with severe back pain and progressive thoracolumbar kyphotic deformity. Radiograph showed a global kyphosis of 114° with pseudarthrosis at the T12-L1 level (arrow) (b). CT sagittal reconstruction image demonstrated disc-space widening (arrowhead) and adjacent bony sclerosis, with the fracture of the facet joint (arrow) (c). T1 (d) and T2-weighted (e) sagittal MR images both revealed hypointense signal intensity of the pseudarthrosis and the adjacent soft tissue (arrowhead), as well as spinal canal stenosis (arrow). Radiograph after PSO showed a bone defect (arrow) (f). Radiograph after supplementary anterior fusion (g). Radiograph at 3 years follow-up showed the solid fusion at the T12-L1 level (h). Clinical appearance before surgery (i, j) and the final follow-up of 3 years (k, l)
Radiologic measurements in standing lateral radiographs before and after surgery included the global kyphosis of the whole spine, the local kyphosis at the level of pseudarthrosis, the sagittal vertical axis (SVA), thoracic kyphosis, and lumbar lordosis. Global kyphosis was measured between the maximally tilted upper and lower end vertebrae; using the standard Cobb’s method. The local kyphosis was measured as the angle between the upper endplate of the vertebra one cephalad to the pseudarthrosis and the lower endplate of the vertebra one caudal to the pseudarthrosis. SVA was defined as the distance between the vertical line through the center of C7 vertebral body and the posterosuperior corner of S1. Thoracic kyphosis was defined as the angle between the superior endplate of T5 and the inferior endplate of T12. Lumbar lordosis was measured between the superior endplate of T12 and S1.
Radiographs demonstrated that these patients had extensive discovertebral erosive lesions, a widened disc space with irregular sclerositic margins and disassociation of the affected levels caused by extensive resorption and sclerosis of the discovertebral junction of the two neighboring bodies. All of the above findings were similar to the characteristics of nonunion of long bone fracture. One patient with flexion contracture of hips had a bilateral total hip replacement 36 months prior to spinal osteotomy. None of the other patients had any ankylosis or flexion deformity of the hips. CT scans demonstrated irregular discovertebral osteolysis with reactive sclerosis in 7 patients, vacuum phenomenon in 4 patients (Fig. 2), and lamina fracture in 1 patient. CT scans also identified marked osteophyte formation around the facet joint at the level of pseudarthrosis, leading to focal spinal canal stenosis in 4 patients. Sagittal CT reconstruction images revealed a lytic gap in the center of vertebral body in 4 cases; simultaneously, these 4 cases were associated with the fracture of facet joint. Sagittal MR images revealed that all patients had irregular low signal band extended into posterior elements on both T1 and T2-weighted images. Five patients had decreased signal intensity on T1-weighted images and increased signal intensity on T2-weighted images; 2 patients had low signals on both T1 and T2-weighted images. Encroachment of the pseudarthrotic lesion into the spinal canal, with the compression of the dural sac, was observed in 4 cases.
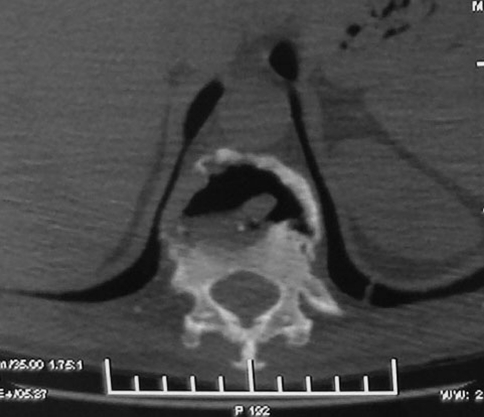
Fig. 2.
CT scan of pseudarthrosis at T11-12 segment demonstrates extensive osteolysis of the vertebral body and vacuum phenomenon
Surgical procedure
Neuromonitoring was performed throughout the surgical procedures. Under the general anesthesia, the patient was positioned prone on a special frame with four folders to accommodate the kyphotic spine. The spine was exposed through a posterior midline approach with dissection laterally to the transverse process. Pedicle screws were inserted in several segments cephalad and caudal to the level of pseudarthrosis. Initially, laminectomy was performed at the site of pseudarthrosis. During the procedure of laminectomy, the dura was meticulously dissected because there was no epidural fat between the dura and the bony structure, and the dura was directly adhered to the lamina. PSO was performed from the lateral vertebral wall to the midline. During osteotomy, the fibrous tissue, fibrocartilage, and necrotic bone around the spinal canal were excised. The pseudarthrotic cavity with fibrous tissue was removed with rongeurs and curettes, and the sclerotic bone around the lesion was resected with a high-speed burr. Finally, the closure of osteotomy was achieved by slowly extending the reduction frame in combination with compressive pressure on the pedicle screws above and below the osteotomy. A wake-up test was performed immediately after the correction of the deformity.
All patients had obvious anterior column defects after PSO, and a second-stage supplemental anterior fusion was performed two weeks after posterior procedure. After the pseudarthrotic lesion was radically debrided, the iliac tricortical bone graft was tightly introduced between the healthy vertebral bodies forming a press-fit.
Two weeks after combined posterior and anterior surgery, the patients were allowed to mobilize in a well-molded thoracolumbosacral brace for three months.
Outcome assessment
Clinical outcomes were assessed by visual analogue scale (VAS; rated on a scale from 0 to 10) preoperatively and at the final follow-up.
Results
Radiologic findings
The average follow-up was 38 months (range, 24–59 months). Before surgery, all patients presented with thoracolumbar kyphosis with the apex at the level of pseudarthrosis (Fig. 1). The average global kyphosis was corrected from 75° (range, 37°–114°) preoperatively to 30° (range, 13°–44°) postoperatively, with a mean correction of 45°. The local kyphosis was corrected from 45° (range, 37°–69°) preoperatively to 8.8° (range, 0°–24.3°) postoperatively, with a mean correction of 36.2°. The mean SVA improved from 103.5 mm (range, 62.6–132 mm) before surgery to 10.4 mm (range, 0–23.5 mm) after surgery, and an average correction of 93.1 mm was achieved. Thoracic kyphosis changed from 56.1° (range, 23.1°–82.6°) preoperatively to 48.1° (range, 24.2°–58.9°) postoperatively. Lumbar lordosis significantly improved from −10.1° (range, −47.6°−32.6°) to −42.2° (range, −2.8° to −54.1°), with an average correction of 32.1°.
Radiologic union was achieved in all patients after an average of 4 months (range, 3–6 months); and no patient had radiographic evidence of loss of correction, progressive kyphotic deformity or recurrent pseudarthrosis at the final follow-up.
Clinical results
All patients showed significant improvement of back pain after surgery. The VAS improved significantly from 7.1 preoperatively to 0 at the final follow-up (Table 1) and all patients were satisfied with the surgical results with an average follow-up of 38 months. Three patients with a neurological deficit (Frankel D) preoperatively had improvement to Frankel E at the final follow-up.
Surgical results
The average operative time was 250 min (range, 180–360 min) for PSO and 210 min (range, 180–240 min) for anterior fusion. The mean blood loss in PSO procedure was 2,200 ml (range, 1,200–4,000 ml) and 470 ml (range, 200–1,000 ml) in anterior fusion.
Microscopy of the excised specimen showed that fibro-ligament tissue with proliferation of fibrous tissue and hyaloid degeneration. In the area of cartilage lesion, irregular calcium salt sediment and endochondral ossification were observed.
Complications
There were no complications of dura tear, spinal cord, or nerve root injury in the posterior surgery. There were also no complications of aortic injury, cerebrospinal fluid leak, and pleural effusion in the anterior procedure. No infections occurred and no hardware failures were observed until the final follow-up. No evidence of delayed union or nonunion at the level of pseudarthrosis was observed at the final follow-up.
Discussion
Spine involvement in AS is characterized by the loss of spinal mobility and vertebral osteoporosis [3, 9]. Additionally, a fixed and rigid thoracolumbar kyphotic deformity often develops in patients with a long history of AS [7, 8]. In the advanced AS patients with complete ankylosed spine, with increased stresses in the thoracolumbar junction, a stress fracture can occur with minor trauma or even without any trauma [19, 21, 24]. As the stress fracture level is always the last mobile joint between two ankylosed spinal segments, the continued movement at the fracture site eventually contributes to the development of pseudarthrosis [2, 20]. In the current series, all patients had 3-column involved pseudarthrosis through the disc space at the thoracolumbar junction, located from T11 to L1 (Table 1). The findings of our study supported the theory that mechanical factors play an important role in the formation of pseudarthrosis [16]. As the thoracolumbar region in advanced AS patients with kyphotic spine acts as a fulcrum between the ossified thoracic and lumbar spine, a stress fracture tends to occur at such a site of high stress forces [4] and more commonly through the intervertebral disc space, as the ankylosed disc presents less resistance than the vertebral body [11]. In addition, persistent motion at the fracture site between the long lever arms makes spontaneous union difficult [4], resulting in the formation of pseudarthrosis.
The three-column involved pseudarthrotic lesion is extremely unstable, and may result in progressive thoracolumbar kyphotic deformity, sagittal imbalance, intractable pain, and neurological deficit [4, 14, 16, 23]. Its surgical indication has been well documented in literature [2, 4, 16, 23]. Most authors have reached a consensus that the goal of the surgical treatment is to achieve a successful arthrodesis of pseudarthrosis, and to restore spinal stability and sagittal balance [16, 23]. However, the optimal surgical procedure is still in debate.
Several authors advised anterior fusion for pseudarthrosis as the optimal surgical procedure, given that it had the advantages of direct access to the anterior lesion, complete curettage, and ideal biomechanical characteristics for repairing the lesion [11, 16]. However, this procedure did not help to correct the global kyphotic deformity [4]. In contrast, a previous study has reported good results from PSO alone for AS-related pseudarthrosis. Chang et al. [4] reported that 30 patients underwent opening-wedge osteotomy at the level of pseudarthrosis achieved a mean of 38° correction for the local kyphosis. In addition, fusion was observed at the anterior gaps created by opening-wedge osteotomy at the final follow-up.
Most surgeons advocated combined anterior and posterior approach for the treatment of pseudarthrosis with kyphotic deformity in advanced AS patients [6, 16]. Chen et al. [6] adopted anterior debridement and fusion with autograft for the pseudarthrosis in the first stage, followed by posterior fusion and instrumentation in the second stage; additionally, Smith-Petersen osteotomy was performed in patients with kyphosis greater than 45°.
The real question is whether the additional anterior fusion after posterior osteotomy through pseudarthrosis is actually needed. Chang et al. [4] pointed out that posterior correction and fixation without anterior fusion is an effective method for the treatment of pseudarthrosis with kyphosis complicating AS. They believed that the superior fusion capacity of AS, the rigid fixation and the improved biomechanical environment with decreased shearing and distraction forces, together contributed to achieve solid fusion. In contrast to the findings of Chang et al. [4], Kim et al. [16] reported the surgical results in a series of 12 patients with a kyphotic pseudarthrosis complicating AS. Smith-Petersen osteotomy was performed at the level of pseudarthrosis for the correction of sagittal plane deformity and anterior interbody fusion for pseudarthrosis repair in the first stage. In a subset of patients, PSO was performed at the lumbar spine for the correction of lumbar hypolordosis in the second stage. In Kim’s [16] repot, radiologic union of pseudarthrosis was achieved in 4.2 months. The authors concluded that anterior interbody fusion for repairing the pseudarthrosis could achieve successful fusion and good clinical results.
To our best knowledge, the current study is the first series, which investigated the outcomes of PSO at the site of thoracolumbar pseudarthrosis, followed by second-stage anterior autograft fusion. In this series, pseudarthrotic lesion was located from T11 to L1 levels associated with spinal canal stenosis in four cases. We concerned more about the risks of neurological complications and the results of kyphotic deformity correction following PSO through pseudarthrosis above L1. In the current study, the correction of global kyphosis, local kyphosis, and SVA following PSO was 45°, 36.2° and 93.1 mm, respectively, without neurological complications. In Van Royen’s report [23], two patients with AS-related pseudarthrosis were treated with PSO at the level of pseudarthrosis (one in L1, one in L1-2), and the achieved correction of kyphosis were 24° and 31°. However, one patient was complicated with insufficient correction of SVA and incomplete neurological deficit. In another article describing the use of PSO through pseudarthrosis, Chang et al. [4] gained an average 38° correction of the local kyphosis in 30 patients with pseudarthrosis complicating AS. Comparing with the outcomes of these studies [4, 16, 23] (Table 2), the results of our series suggest that PSO at the site of pseudarthrosis in the distal thoracic and high lumbar spine (above L1) is safe and can achieve the best sagittal balance. Importantly, there were no dural tears, spinal cord injury during the posterior procedure. The satisfied correction rate (Table 2) was ascribed to using the closing-opening wedge osteotomy technique. Given the anterior column at the site of the pseudarthrosis being opened during the osteotomy, a closing wedge of the posterior column at the level of the pseudarthrosis was feasible to accomplish. In this procedure, the correction of the kyphotic deformity was achieved by closing the shortened middle and posterior columns and opening the anterior column with the center of correction located posterior to the spinal cord, helping to prevent spinal cord injury.
Table 2.
Results of pedicle subtraction osteotomy for spinal pseudarthrosis complicating ankylosing spondylitis reported in the literature and in the current study
| Author (year) | No. cases operated | Surgical method | Clinical/radiological outcome | Complications |
|---|---|---|---|---|
| Chang [4] (2006) | 30 | Posterior opening-wedge osteotomy | A mean correction of 38° for local kyphosis | Postoperative pneumonia in 1 patient Superficial infection in 1 patient |
| Van Royen [23] (2006) | 2 | Transpedicular wedge resection osteotomy | The correction of kyphosis was 24° and 31°, respectively | Incomplete neurological deficit in 1 patient |
| Kim [16] (2007) | 12 | Smith-Petersen osteotomy or pedicle subtraction osteotomy with anterior interbody fusion in one-stage or two-stage | The mean correction was 20.9° with Smith-Petersen osteotomy and 26.3° with pedicle subtraction osteotomy | Dural tears in 3 cases Leg pain with paresthesia in 2 patients Early deep wound infection in 1 patient |
| Current study | 7 | Pedicle subtraction osteotomy through pseudarthrosis combined with anterior interbody fusion | The kyphosis was corrected from 75º to 30º, with a mean correction of 45º. Solid bony fusion achieved at the final follow-up | No perioperative complications |
We performed anterior interbody fusion after PSO at the level of pseudarthrosis for several reasons. First, the pseudarthrosis in this study is the extensive discovertebral lesion with 3-column involved. After the pseudarthrosis being radically excised in the procedure of PSO, it is hard to accomplish closure of the osteotomy site using the anterior cortex as the hinge. In the authors’ opinion, the procedure is more similar to the spinal shortening. However, in the spinal shortening procedure, the correction at one level will not exceed 40° [13, 17]. In this series, the average kyphotic deformity is 75°. If we try to accomplish bone-on-bone fusion after PSO, excessive dural buckling, curving, or even kinking may occur at the apex of the deformity, which is probably dangerous. In this situation, the closing-opening osteotomy technique can be adopted to achieve larger correction for severe kyphotic deformity, and to avoid potential spinal cord curving, or kinking. In the current study, an average 45° correction of global kyphosis was achieved without neurological complications, indicating the effectiveness and safety of the closing-opening osteotomy technique in severe thoracolumbar kyphosis secondary to AS pseudarthrosis. Second, we deem that for these patients—with evident bony defect in the anterior and middle column after PSO at the site of pseudarthrosis—solid fusion cannot be achieved without anterior support, even if there is a normal or superior bone-healing capacity in AS patients [4]. Third, the anterior and middle column at the segment of the bony defect will be functionally unstable; an iliac graft packed between the vertebral bodies can support the anterior and middle column structurally to restore the stability, and can achieve bony surfaces contact contributing to a rapid healing. Fourth, the presence of a gap in the anterior column may place excessive loads on the posterior instrumentation and compromise stability of the construct, which increases the incidence of late complications such as loss of correction or instrumentation failure [5, 15]. In this situation, an anterior strut graft can effectively reduce the stresses that act on the posterior instrumentation to prevent the above-mentioned complications. As reported by Chen et al. [5], one patient of L3-4 spondylodiscitis in AS underwent PSO at L3 suffered from back pain, recurrence of kyphotic deformity and implant failure at 2 years follow-up. They deemed that the implant failure was attributable to the unhealed spondylodiscitis and the defect of the anterior column. Fortunately, the back pain was alleviated and the deformity progression was arrested after an additional anterior fusion for stabilizing the spondylodiscitis. Investigating PSO without anterior fusion for the treatment of pseudarthrosis with kyphosis complicating AS, Chang et al. [4] observed an average 2° (range, 1°–6°) loss of local kyphosis during the follow-up period. Comparatively, the loss of correction did not occur in our series and solid consolidation was achieved in all patients at the final follow-up; this might be ascribed to the full anterior support and rigid posterior fixation. The clinical and radiographic results in this study were similar to Kim et al. [16], who reported the results of SPO and anterior interbody fusion at the level of pseudarthrosis for the treatment of 12 patients with kyphotic pseudarthrosis complicating AS. They found that successful fusion and good clinical results were achieved in all patients.
A potential weakness of our study is that the impact of PSO on sagittal spinopelvic alignment could not be fully quantified. In the current study, the spinal parameters (GK, SVA, TK, and LL) were adopted to evaluate the effect of PSO through pseudarthrosis in advanced AS on the sagittal alignment of the spine. However, comparison between preoperative and postoperative sagittal alignment of the pelvis was not carried out using pelvic parameters (pelvic incidence, pelvic tilt, and sacral slope).
In conclusion, the current study reports the outcomes of PSO at the level of pseudarthrosis followed by supplemental anterior fusion for the treatment of thoracolumbar pseudarthrosis in advanced AS patients. A satisfied kyphotic correction, successful fusion, and good clinical outcomes were achieved without additional neurological complications. Results of this study suggest that PSO at the site of pseudarthrosis is a safe and effective method for the treatment of AS patients with thoracolumbar pseudarthrosis and kyphotic deformity. Based on the results of this study, we deem that the necessity of supplemental anterior fusion for pseudarthrosis following PSO should be decided according to the extent of osteotomy closure. After PSO with pseudarthrosis is completely cleared, if the osteotomy site can be completely closed, there is no need to perform anterior interbody fusion. However, if the postoperative radiograph demonstrates an anterior column defect with wide opening at the level of pseudarthrosis following PSO, strong consideration should be given to perform a supplemental anterior fusion. In the current series, all patients had a bone defect in the osteotomy site after PSO, anterior strut fusion was performed to support the anterior column and to prevent the loss of correction and implant failure.
Acknowledgments
One of the authors (Bang-ping Qian) has received funding from Development of Medical Technology Key Project, Nanjing, China (ZKX10008) and Medical Technology Development Project, Nanjing, China (YKK09100).
Conflict of interest
None.
References
- 1.Arun R, Dabke HV, Mehdian H (2011) Comparison of three types of lumbar osteotomy for ankylosing spondylitis: a case series and evolution of a safe technique for instrumented reduction. Eur Spine J Jul 29, 2011 [epub ahead of print] [DOI] [PMC free article] [PubMed]
- 2.Bron JL, Vries MK, Snieders MN, Horst-Bruinsma IE, Royen BJ. Discovertebral (Andersson) lesions of the spine in ankylosing spondylitis revisited. Clin Rheumatol. 2009;28:883–892. doi: 10.1007/s10067-009-1151-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bronson WD, Walker SE, Hillman LS, Keisler D, Hoyt T, Allen SH. Bone mineral density and biochemical markers of bone metabolism in ankylosing spondylitis. J Rheumatol. 1998;25:929–935. [PubMed] [Google Scholar]
- 4.Chang KW, Tu MY, Huang HH, Chen HC, Chen YY, Lin CC. Posterior correction and fixation without anterior fusion for pseudoarthrosis with kyphotic deformity in ankylosing spondylitis. Spine. 2006;31:E408–E413. doi: 10.1097/01.brs.0000219870.31561.c2. [DOI] [PubMed] [Google Scholar]
- 5.Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine. 2001;26:E354–E360. doi: 10.1097/00007632-200108150-00010. [DOI] [PubMed] [Google Scholar]
- 6.Chen LH, Kao FC, Niu CC, Lai PL, Fu TS, Chen WJ. Sugical treatment of spinal pseudoarthrosis in ankylosing spondylitis. Chang Gung Med J. 2005;28:621–628. [PubMed] [Google Scholar]
- 7.Debarge R, Demey G, Roussouly P. Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle substraction osteotomy. Eur Spine J. 2010;19:65–70. doi: 10.1007/s00586-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Debarge R, Demey G, Roussouly P. Sagittal balance analysis after pedicle substraction osteotomy in ankylosing spondylitis. Eur Spine J. 2011;20(Suppl 5):619–625. doi: 10.1007/s00586-011-1929-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El Maghraoui A, Borderie D, Cherruau B, Edouard R, Dougados M, Roux C. Osteoporosis, body composition, and bone turnover in ankylosing spondylitis. J Rheumatol. 1999;26:2205–2209. [PubMed] [Google Scholar]
- 10.El-Sharkawi MM, Koptan WM, El-Miligui YH, Said GZ. Comparison between pedicle substraction osteotomy and anterior corpectomy and plating for correcting post-traumatic kyphosis: a multicenter study. Eur Spine J. 2011;20:1434–1440. doi: 10.1007/s00586-011-1720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fang D, Leong JC, Ho EK, Chan FL, Chow SP. Spinal pseudoarthrosis in ankylosing spondylitis. Clinicopathological correlation and the results of anterior spinal fusion. J Bone Joint Surg Br. 1988;70:443–447. doi: 10.1302/0301-620X.70B3.3372569. [DOI] [PubMed] [Google Scholar]
- 12.Feldtkeller E, Vosse D, Geusens P, Linden S. Prevalence and annual incidence of vertebral fractures in patients with ankylosing spondylitis. Rheumatol Int. 2006;26:234–239. doi: 10.1007/s00296-004-0556-8. [DOI] [PubMed] [Google Scholar]
- 13.Gertzbein SD, Harris MB. Wedge osteotomy for the correction of posttraumatic kyphosis. A new technique and a report of three cases. Spine. 1992;17:374–379. doi: 10.1097/00007632-199203000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Good AE, Keller TS, Weatherbee L, Braunstein EM. Spinal cord block with a destructive, lesion of the dorsal spine in ankylosing spondylitis. Arthritis Rheum. 1982;25:218–222. doi: 10.1002/art.1780250217. [DOI] [PubMed] [Google Scholar]
- 15.Kiaer T, Gehrchen M. Transpedicular closed wedge osteotomy in ankylosing spondylitis: results of surgical treatment and prospective outcome analysis. Eur Spine J. 2010;19:57–64. doi: 10.1007/s00586-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim KT, Lee SH, Suk KS, Lee JH, Im YJ. Spinal pseudarthrosis in advanced ankylosing spondylitis with sagittal plane deformity: clinical characteristics and outcome analysis. Spine. 2007;32:1641–1647. doi: 10.1097/BRS.0b013e318074c3ce. [DOI] [PubMed] [Google Scholar]
- 17.Lehmer SM, Keppler L, Biscup RS, Enker P, Miller SD, Steffee AD. Posterior transvertebral osteotomy for adult thoracolumbar kyphosis. Spine. 1994;19:2060–2067. doi: 10.1097/00007632-199409150-00009. [DOI] [PubMed] [Google Scholar]
- 18.Mitra D, Elvins DM, Speden DJ, Collins AJ. The prevalence of vertebral fractures in mild ankylosing spondylitis and their relationship to bone mineral density. Rheumatology (Oxford) 2000;39:85–89. doi: 10.1093/rheumatology/39.1.85. [DOI] [PubMed] [Google Scholar]
- 19.Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5:51–55. doi: 10.1007/BF00307827. [DOI] [PubMed] [Google Scholar]
- 20.Pettersson T, Laasonen L, Leirisalo-Repo M, Tervahartiala P. Spinal pseudoarthrosis complicating ankylosing spondylitis: a report of two patients. Br J Rheumatol. 1996;35:1319–1323. doi: 10.1093/rheumatology/35.12.1319. [DOI] [PubMed] [Google Scholar]
- 21.Taggard DA, Traynelis VC. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine. 2000;25:2035–2039. doi: 10.1097/00007632-200008150-00006. [DOI] [PubMed] [Google Scholar]
- 22.Trent G, Armstrong GW, O’Neil J. Thoracolumbar fractures in ankylosing spondylitis. High-risk injuries. Clin Orthop Relat Res. 1988;227:61–66. [PubMed] [Google Scholar]
- 23.Royen BJ, Kastelijns RC, Noske DP, Oner FC, Smit TH. Transpedicular wedge resection osteotomy for the treatment of a kyphotic Andersson lesion-complicating ankylosing spondylitis. Eur Spine J. 2006;15:246–252. doi: 10.1007/s00586-005-1008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vosse D, Feldtkeller E, Erlendsson J, Geusens P, Linden S. Clinical vertebral fractures in patients with ankylosing spondylitis. J Rheumatol. 2004;31:1981–1985. [PubMed] [Google Scholar]
- 25.Wu PC, Fang D, Ho EK, Leong JC. The pathogenesis of extensive discovertebral destruction in ankylosing spondylitis. Clin Orthop Relat Res. 1988;230:154–161. [PubMed] [Google Scholar]