Abstract
Introduction
Pelvic tilt is an established measure of position which has been tied to sagittal plane spinal deformity. Increased tilt is noted in the setting of the aging spine and sagittal malalignment syndromes such as flatback (compensatory mechanism). However, the femoral heads are often poorly visualized on sagittal films of scoliosis series in adults, limiting the ability to determine pelvic incidence and tilt. There is a need to establish a coronal plane (better visualization) pelvic parameter which correlates closely with pelvic tilt.
Methods
This is a retrospective review of 71 adult patients (47 females and 24 males) with full-length standing spine radiographs. Visualization of all spinal and pelvic landmarks was available coronally and sagittally (including pelvis and acetabuli). Pelvic tilt was calculated through validated digital analysis software (SpineView®). A new parameter, the sacro-femoral-pubic angle (midpoint of S1 endplate to centroid of acetabuli to superior border of the pubic symphysis) was analyzed for correlation (and predictive ability) with sagittal pelvic tilt.
Results
The sacro-femoral-pubic angle (SFP angle) was highly correlated to PT, and according to this analysis, pelvic tilt could be estimated by the formula: PT = 75 − (SFP angle). A Pearson’s correlation coefficient of 0.74 (p < 0.005) and predictive ability of 76% accuracy was obtained (±7.5°). The correlation and predictive ability was greater for males compared to females (male: r = 0.87 and predictive model = 93%; female: r = 0.67 and predictive model = 67%).
Conclusion
The pelvic tilt is an essential measure in the context of radiographic evaluation of spinal deformity and malalignment. Given the routinely excellent visibility of coronal films this study established the SFP as a coronal parameter which can reliably estimate pelvic tilt. The high correlation and predictive ability of the SFP angle should prompt further study and clinical application when lateral radiographs do not permit assessment of pelvic parameters.
Keywords: Sagittal alignment, Pelvic tilt, Spine, Coronal, Radiographic evaluation
Introduction
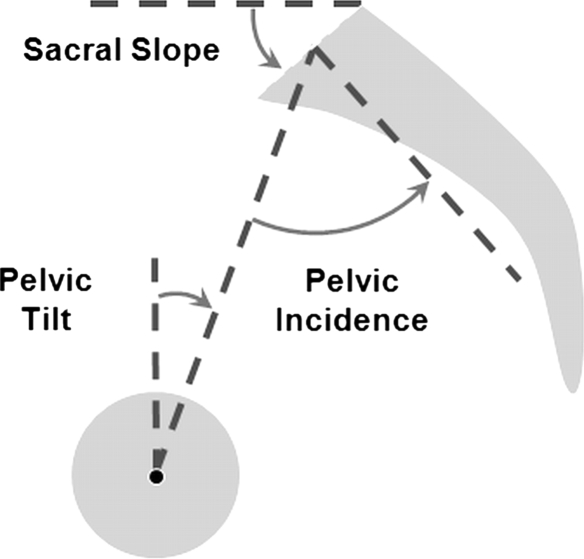
The evaluation of spine sagittal alignment is increasingly pursued in clinical practice as several parameters correlating with clinical outcomes have been described [1–8]. These measurements include various spinal angles and plumb lines, but it is increasingly evident that assessment of spinal deformity must include pelvic parameters [2]. Duval-Beaupere et al. [9, 10] initially described three pelvic angles (Fig. 1): pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS), which are interrelated by the equation PI = PT + SS. PI is a morphological parameter that is predictive of the theoretical lumbar lordosis. PT and SS are positional parameters, related to the orientation of the pelvis and the spinal alignment.
Fig. 1.
Pelvic parameters, PI defined as the angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral heads axis; SS defined as the angle between the horizontal and the sacral plate and PT defined by the angle between the vertical and the line through the midpoint of the sacral plate to femoral heads axis. “PI = PT + SS”
According to current knowledge of sagittal alignment, PT (defined by the angle between the vertical and the line from the midpoint of the sacral plate to the femoral head axis) is an established measure of pelvic version (position) which has been tied to sagittal plane spinal deformity and more recently to health-related quality of life scores in adults with spinal deformities (in association with sagittal vertical axis and T1 sagittal tilt) [2]. Increased pelvic tilt can be observed in the setting of the aging spine and sagittal malalignment. This pelvic retroversion reflects accommodation to global alignment and is related to a compensatory mechanism in order to maintain upright position [3]. In daily practice, clinical measurements of PT and pelvic parameters are simple and reliable on lateral X-rays including spine, pelvis and at least the femoral heads.
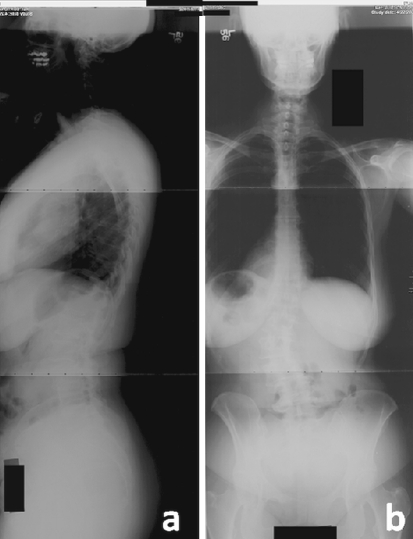
However, even if the full spine is clearly visible on plain X-rays (usually to the upper endplate of the sacrum), complete view of the pelvis (acetabuli and femoral heads) is often not obtained on sagittal films of scoliosis series in adults due to under penetration (Fig. 2) while it is clearly visible on most full spine coronal X-rays. Thus, there is an interest in establishing a coronal plane pelvic parameter which correlates closely with pelvic tilt in order to provide an alternative solution for evaluation of pelvic version when measurement of PT is impossible on lateral standing X-rays.
Fig. 2.
Example of clinical X-rays where evaluation of femoral heads is impossible on the lateral view (a), but visible on the AP radiographic acquisition (b)
The aim of this study is to describe a new coronal pelvic parameter named the sacro-femoral-pubic angle (SFP) and to evaluate its correlation with sagittal pelvic tilt.
Materials and methods
Study design
This study was based on a retrospective review of 71 adult patients (47 females and 24 males) who underwent full-length antero-posterior (AP) and lateral spine radiographs (LAT) for clinical or research purposes, in a single institution. Patients with normal sagittal alignment and those with spinal disorders were both included. The presence of a pelvic osseous abnormality or previous total hip replacement was an exclusion criteria for the study.
Radiographic measurements
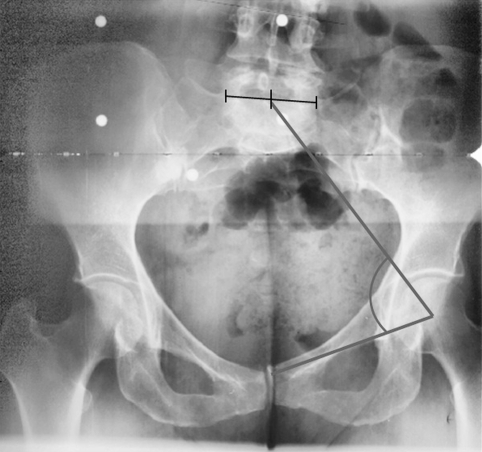
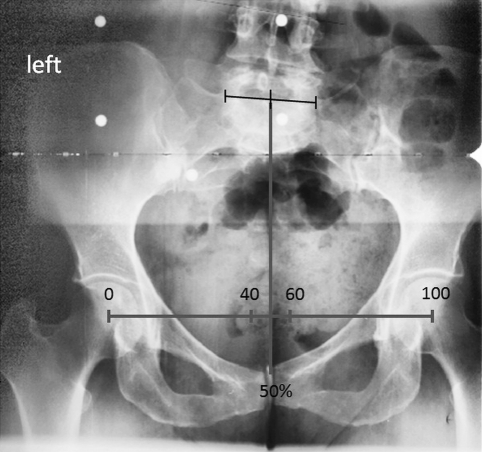
For each patient, a complete visualization of all spinal and pelvic landmarks was available on coronal and sagittal X-rays (pelvis and femoral heads included). A standardized measurement of pelvic tilt was obtained based on lateral view, using validated digital analysis software (SpineView®, Surgiview, Paris, France). On the coronal view, the SFP angle was calculated as the angle between the midpoint of the upper sacral endplate (by drawing the midpoint between lateral borders of L5–S1 facet joints), the centroid of one acetabulum and the upper midpoint of the pubic symphysis (Fig. 3). In order to evaluate the potential impact of pelvic asymmetry (intrinsic or due to pelvic rotation), measurements of the SFP angle were done on the right and left sides of the pelvis; pelvic asymmetry and axial rotation were estimated based on the projection of the center of S1 on the segment formed by the two centroids of the acetabuli (Fig. 4).
Fig. 3.
The sacro-femoro-pubic angle is defined as the angle between the midpoint of the upper sacral endplate (by drawing the midpoint between lateral borders of L5–S1 facet joints), the centroid of one acetabulum and the upper midpoint of the pubic symphysis
Fig. 4.
Evaluation pelvis asymmetry and/or axial rotation based on the projection of the center of S1 on the segment formed by the two centroids of the acetabuli. Using the offset between the two acetabuli as reference (scale 0–100), a projection of S1 in the middle of the two acetabuli is denoted as 50% (neutral rotation), a projection toward the left acetabulum will be between 0 and 50, and towards the right acetabulum will be between 50 and 100
Statistical analysis
Differences between right and left measurements of the SFP angle were evaluated using a paired t test analysis. The relationship between SFP angle and pelvic tilt was evaluated using a Pearson coefficient of correlation and a multi-linear regression analysis with a stepwise condition. Finally, a subgroup analysis by sex was conducted to evaluate the influence of gender on these parameters. Prediction accuracy of the PT estimation formulas was evaluated by calculating the positive and negative predictive values using a cut-off value of 20° for PT in reference to threshold established in order to obtain a satisfactory alignment [11]. The statistical analysis was conducted using SPSS Software (SPSS, Chicago, IL) with a level of significance was set at 0.05.
Results
Patient demographics
Seventy-one patients were included in this study with a mean age of 50.4 years (18–91 years); 66% of the subjects were females and 34% were males. The mean age was 50.2 ± 17.4 for males and 50.5 ± 19.4 years for females. No statistical difference in terms of age was observed between males and females (t test p = 0.95).
Global radiographic results
Based on the SpineView analysis, mean pelvic tilt (PT) on the whole series was 18.9° (SD = 11.5) and mean SFP angle was 59.2° (SD = 8.9), without any statistical difference between gender (t test p > 0.05). Comparison between left and right SFP values did not show significant differences (p = 0.219) (Table 1).
Table 1.
Summary of baseline data and distribution of pelvic tilt and SFP angle among groups
| Number of patients | PT | SFP | |||
|---|---|---|---|---|---|
| Mean (°) | SD (°) | Mean (°) | SD (°) | ||
| Females | 47 (66%) | 18.3 | 11 | 59.7 | 8.5 |
| Males | 24 (34%) | 20 | 12.5 | 58.1 | 9.9 |
| Entire group | 71 | 18.9 | 11.5 | 59.2 | 8.9 |
No statistical differences (paired t test p > 0.05) were observed between measurements
On the analysis of pelvic axial rotation (coronal X-ray was considered as neutral, i.e., without significant axial rotation when the ration was equal to 50%), results from all the X-rays showed a pelvic axial rotation included in a range of ±10% (i.e., between 40 on the left and 60 on the right). The difference between left and right SFP angle was significantly correlated with the evaluation of pelvic axial rotation (r = 0.738, p < 0.001).
Correlation analysis and linear models (Table 2)
Table 2.
Summary of statistical results, showing correlation and predictive ability between SFP angle and PT
| Pearson coefficient | Linear predictive model | Predicted PT with simplified formula (°) | |
|---|---|---|---|
| Entire group | 0.74 (p < 0.005) | 76% (±7.5°) | 16.1 |
| Female | 0.67 (p < 0.005) | 67% (±7.5°) | 15.3 |
| Male | 0.87 (p < 0.005) | 93% (±5.8°) | 16.9 |
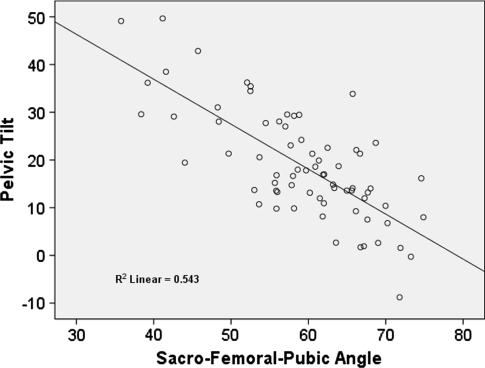
Statistical analysis between SFP and PT demonstrated a Pearson’s correlation coefficient of 0.74 (p < 0.005). The impact of SFP angle as a predictor parameter of PT was verified by the linear regression analysis (Fig. 5) where PT could be calculated by the following equation PT = 74.6 − 0.942 × (SFP angle) which in turn could be simplified as follows: PT = 75 − (SFP angle). Analysis by gender showed that correlation and predictive ability were greater for male patients than female patients but establishing a predictive model by gender did not increase the predictability of these formulas.
Fig. 5.
Linear regression model showing correlation between PT and SFP angles
Ability to detect pelvic retroversion
Comparison of the two established formulas demonstrated that the simplified one had the better positive and negative predictive values (PPV and NPV). The calculated PPV of the simplified formula was 0.75 which means that if the formula predicts a PT <20°, there is a 75% chance that the result will be in accordance with the real PT. The calculated NPV was 0.83 which means that if the formula predicts a PT >20°, there is an 83% chance that the result will be in accordance with the real PT. Of the 15 patients for whom the formula was not able to predict a correct PT, 13 were women, with a mean error of 11°.
Discussion
Sagittal spinal alignment has been reported as the main driver of disability and is correlated with postoperative outcomes in adults with spinal deformities [2, 8, 12, 13]. Various parameters have been investigated so far, describing regional (lumbar lordosis and thoracic kyphosis) and global alignment (SVA, T1 sagittal tilt). Recent studies have also reported the crucial impact of pelvic parameters (PI, PT and SS) and among them pelvic tilt have been widely studied in recent years and related to clinical outcomes. Lafage et al. [2] reported in a previous study that self-reported disability increases with anterior sagittal malalignment and pelvic retroversion. Conclusions of the study underlined the fact that analysis of the sagittal plane must integrate not only spinal parameters, but also pelvic measurements. One of the challenges in daily clinical practice relates to the loss of data available from standing full-length lateral X-rays due to insufficient exposure of the pelvis or the impossibility of a technician to determine the precise position of the femoral heads. It is therefore important to have an alternative approach to quantify pelvic parameters based solely on the coronal X-rays where femoral heads are commonly clearly visible.
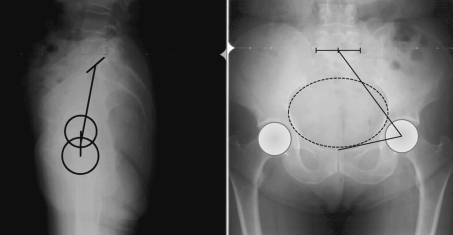
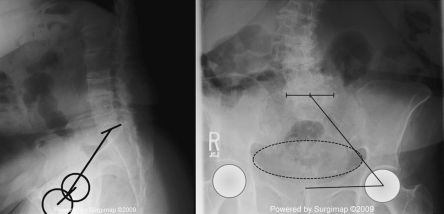
The purpose of the study was to evaluate the feasibility of using a coronal parameter to estimate the pelvic tilt when regular measurement of PT is impossible. Statistical analysis found significant correlation between the newly proposed SFP angle and the PT with satisfactory predictive ability, especially in male patients. Correlation between PT and SFP angle can be clinically explained by a simple analysis of the relative location of anatomical landmarks during sagittal pelvic rotation. It is common to describe the pelvis as a ring with an inner part, the pelvic inlet, formed anteriorly by the pubic symphysis, laterally by the pectineal and arcuate lines and posteriorly by the sacral promontory. In the absence of pelvic retroversion (i.e., pelvic tilt within normative range of value pelvic anteversion), the coronal projection of the pelvic inlet could be approximated by a circle or a slightly elliptical shape (Fig. 6). On the other hand, in case of pelvic retroversion, the projection of the pelvic inlet is vertically flattened (Fig. 7). Because the SFP angle is based on landmarks located, respectively, posterior, lateral and anterior to the pelvic inlet, the SFP angle will be affected in the same manner that the coronal projection of the pelvic inlet by the pelvic retroversion.
Fig. 6.
Example of a patient with a low PT on sagittal view (left) (pelvic anteversion). On the coronal view (right), SFP angle value is high and pelvic inlet projection can be approximate by a circle
Fig. 7.
Example of a patient with pelvic retroversion on the sagittal view (left) (high PT). On the coronal view (right), SFP angle value is lower and pelvic inlet projection is vertically flattened
In a previous study, Lucas et al. [14] found an estimation of transverse plane pelvic rotation using a posterior–anterior radiograph by identification of anatomical landmarks on pelvic sawbones. They described a left/right ratio of coronal plane distances between the sacro-iliac joint and the anterior superior iliac spine. This coronal parameter showed a nearly linear correlation with a transversal plane pelvic rotation up to 20°. Validation of Lucas’ ratio as well as the SFP angle described in the current study assumes the absence of important hemipelvic asymmetry. According to Badii [15] a pelvic height asymmetry is uncommon and was under 5 mm in less than 5.3% of the 323 pelvises studied. Berry et al. [16] did not find any significant differences between the left and right side of the pelvis based on a study of 129 specimens. On the other hand, Boulay et al. [17] have described the presence of pelvic asymmetry on a three dimensional study on 12 anatomical specimens. However, results from our study did not demonstrate differences using right or left acetabuli centroid and in an acceptable range of axial pelvic rotation. Furthermore, a clinical advantage of the SFP angle is its independence towards the potential coronal inclination of the pelvis, for example due to lower limb discrepancy.
The SFP angle demonstrated good correlation with PT as noted with a Pearson’s coefficient of 0.74 and a predictive ability of 76% on the whole series with a simplified prediction formula, but these results were less accurate for females than for male patients. Such differences may result from pelvic morphology variations between genders. Patriquin et al. [18] demonstrated that pubic bone and sciatic notch morphology differed between the genders enough to reliably predict gender based on pelvic shape alone. Schutz [19] recently discussed the role of parity on pelvic remodeling. In summary, both congenital and environmental factors may explain variations in correlation noted in this investigation.
Based on the results of this study, the SFP angle emerges as a valuable alternative for the evaluation of pelvic tilt when its measurement is impossible on a lateral X-ray. Furthermore, if the upper sacrum is visible on a lateral radiographic series then combining the SFP with a measured sacral slope (SS) can yield an approximation of the pelvic incidence (PI) according to the relationship PI = SS + PT. The SFP may also be of interest in other surgical fields such as total hip arthroplasty [20], where the evaluation of pelvic antero- or retro-version is associated with variable risks of dislocation [21], or for patients with hip-spine syndrome [22], in order to evaluate reciprocal effects of treatments.
The findings of this study should not imply that a single coronal radiograph is sufficient to quantify pelvic shape and position. However, while the SFP does not replace the important measure of pelvic tilt, it constitutes a pragmatic approach to permit enhanced analysis of sagittal spino-pelvic alignment when sagittal X-rays do not permit such measurement and repeated radiographs (in an attempt to provide further imaging) is not acceptable due to radiation dose or clinical management (e.g., lack of onsite imaging). Of note, this study was carried out using full-length cassettes and results are not intended to be used as a replacement tool for evaluation of the sagittal alignment using a single AP pelvic X-ray. Further studies will be helpful to determine the independent clinical relevance of the SFP through prospective health-related quality of life studies in patients suffering from spinal deformity.
Conflict of interest
None.
References
- 1.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 2.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 3.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–1578. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 4.Gangnet N, Dumas R, Pomero V, Mitulescu A, Skalli W, Vital JM. Three-dimensional spinal and pelvic alignment in an asymptomatic population. Spine (Phila Pa 1976) 2006;31:E507–E512. doi: 10.1097/01.brs.0000224533.19359.89. [DOI] [PubMed] [Google Scholar]
- 5.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 6.El Fegoun AB, Schwab F, Gamez L, Champain N, Skalli W, Farcy JP. Center of gravity and radiographic posture analysis: a preliminary review of adult volunteers and adult patients affected by scoliosis. Spine (Phila Pa 1976) 2005;30:1535–1540. doi: 10.1097/01.brs.0000167534.49069.e9. [DOI] [PubMed] [Google Scholar]
- 7.Schwab F, Lafage V, Farcy JP, Bridwell K, Glassman S, Ondra S, Lowe T, Shainline M. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine (Phila Pa 1976) 2007;32:2723–2730. doi: 10.1097/BRS.0b013e31815a58f2. [DOI] [PubMed] [Google Scholar]
- 8.Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976) 2008;33:2243–2247. doi: 10.1097/BRS.0b013e31817d1d4e. [DOI] [PubMed] [Google Scholar]
- 9.Duval-Beaupere G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 12.Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47:95–101. doi: 10.3340/jkns.2010.47.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 14.Lucas B, Asher M, McIff T, Lark R, Burton D. Estimation of transverse plane pelvic rotation using a posterior–anterior radiograph. Spine (Phila Pa 1976) 2005;30:E20–E27. doi: 10.1097/01.brs.0000175181.28730.ab. [DOI] [PubMed] [Google Scholar]
- 15.Badii M, Shin S, Torreggiani WC, Jankovic B, Gustafson P, Munk PL, Esdaile JM. Pelvic bone asymmetry in 323 study participants receiving abdominal CT scans. Spine (Phila Pa 1976) 2003;28:1335–1339. doi: 10.1097/01.BRS.0000065480.44620.C5. [DOI] [PubMed] [Google Scholar]
- 16.Berry JL, Stahurski T, Asher MA. Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine (Phila Pa 1976) 2001;26:E143–E148. doi: 10.1097/00007632-200104010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Boulay C, Tardieu C, Benaim C, Hecquet J, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupere G, Pelissier J. Three-dimensional study of pelvic asymmetry on anatomical specimens and its clinical perspectives. J Anat. 2006;208:21–33. doi: 10.1111/j.1469-7580.2006.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patriquin ML, Loth SR, Steyn M. Sexually dimorphic pelvic morphology in South African whites and blacks. Homo. 2003;53:255–262. doi: 10.1078/0018-442X-00049. [DOI] [PubMed] [Google Scholar]
- 19.Schutz H, Donovan ER, Hayes JP. Effects of parity on pelvic size and shape dimorphism in Mus. J Morphol. 2009;270:834–842. doi: 10.1002/jmor.10723. [DOI] [PubMed] [Google Scholar]
- 20.Philippot R, Wegrzyn J, Farizon F, Fessy MH. Pelvic balance in sagittal and Lewinnek reference planes in the standing, supine and sitting positions. Rev Chir Orthop Traumatol. 2009;95:70–76. doi: 10.1016/j.otsr.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Thomasson E, Guingand O, Terracher R, Mazel C. Role of sagittal spinal curvature in early dislocation after revision total hip arthroplasty: prospective analysis of 49 revision procedures. Rev Chir Orthop Reparatrice Appar Mot. 2004;90:226–231. doi: 10.1016/S0035-1040(04)70098-7. [DOI] [PubMed] [Google Scholar]
- 22.Lazennec JY, Riwan A, Gravez F, Rousseau MA, Mora N, Gorin M, Lasne A, Catonne Y, Saillant G. Hip spine relationships: application to total hip arthroplasty. Hip Int. 2007;17:91–104. [PubMed] [Google Scholar]