Abstract
Aim
To determine the frequency of different patterns of centralization and their association with outcomes and MRI findings in patients experiencing sciatica.
Methods
A prospective longitudinal cohort study of 176 patients with radicular pain below the knee, who all had an MDT clinical assessment. Based on their pain response, patients were divided into five groups: abolition centralization, reduction centralization, unstable centralization, peripheralization, and “no effect”. Patients had an MRI.
Results
Overall, 84.8% of patients reported experiencing centralization, 7.3% peripheralized and 7.9% reported “no effect”. The median reduction in RMQ scores across all the three centralization groups was 9.5 points at 3 months, and 12.0 points at 12 months. The peripheralization group improved similarly. The ‘no effect’ group improved significantly lower (p < 0.001), by 3.0 at both time points. Patients who centralized, and peripheralized had a significantly reduction in leg pain, the “no effect” group demonstrated a less favorable outcome (p < 0.02). There was no association between pain responses and the type of disc lesion.
Conclusion
In patients with sciatica, centralization was common and associated with improvement in activity limitation and leg pain. Centralization was very common in ruptured disc therefore the study does not support the theory, that centralization only occurs if the intra-discal hydrostatic mechanism is functional.
Keywords: Centralization, MDT, Lumbar disc herniation, Sciatica, Predictive value
Introduction
Low back pain (LBP) can be disabling, with significant direct and indirect costs to individuals as well as society [1, 2]. The cumulative life time incidence of LBP is approximately 80% [3–5] in western societies, and there is an urgent need that progress is made in the management of patients with LBP patients [2]. Sciatica is a subgroup of LBP, which involves nerve root compression, and this condition has a lifetime prevalence of 4–5% [4, 6]. The most common cause of nerve root compression is a herniated lumbar disc, especially when pain radiates below the knee. Even though patients with an acute lumbar disc herniation only account for 2% of the LBP population, they account for a disproportionately large amount (30%) of the U.S. National yearly cost of treatment for LBP [7].
Centralization describes a phenomenon where pain originating from the spine and referred distally, moves or retreats back towards the midline of the spine in response to repeated movements or guided positioning. The pain often diminishes or is eliminated entirely. To determine if this occurs in individual patients, a standardized physical assessment is performed using repeated lumbar end-range test movements or positions in various directions, most often in the sagittal or frontal planes, while monitoring the individual’s pattern of pain response. This phenomenon was described initially as a part of the diagnostic and treatment methods of McKenzie [8], who first observed it in 1956. Since then, these methods have evolved and have undergone considerable development. In general, a patient’s symptoms are said to be centralizing if “in response to the application of loading strategies, distal symptoms are decreasing or being abolished. This change can occur instantly, over days or may take one to two weeks” [8]. Several variations in the definition of centralization have been described in the literature [9–16].
‘The disc model’ was developed by McKenzie and is the theoretical background for the hypothesis of how and why centralisation occurs. A central part of this theory is that the repeated movements and/or positioning are able to move the nucleus material inside the disc. A prerogative for this movement of nucleus material is that the intra-discal pressure is present, and therefore in ‘the disc model’ if the annulus is broken and the interdiscal pressure is lost, centralization cannot occur.
The reported prevalence of centralization in patients with back pain ranges from 30.8% [15] to 87% [9] with a mean of 58% [17]. In a meta-analysis of 1,056 patients [17], centralization occurred in 64.5% (681 patients). The prevalence of centralization appears to be dependent on several factors: the more acute the pain, the more proximal the pain, the younger the patient, the higher the prevalence. The definition of centralization also affects the prevalence.
In general, patients who centralize [17] have a good to excellent outcome with respect to return to work (p < 0.03–0.04), with less pain and better function (p < 0.001). Donelson examined patients with referred leg pain and reported good or excellent outcomes in 98% of acute, and 77% of chronic patients. The absence of centralization predicted an unsatisfactory outcome (p < 0.001) [9].
The reliability of any clinical test is a prerequisite to justifying its use. For classifying centralization, Fritz et al. reported an average agreement of 88% (Kappa 0.79) by 40 practicing and student physical therapists, who did not have any formal qualifications in the McKenzie system. They observed videotapes of a standardized examination of 12 patients and classified each patient according to his/her pain response to movement [16]. Kilpikoski et al. reported that two highly experienced physical therapists with credentials in mechanical diagnosis and therapy (MDT) examined 39 chronic LBP patients. Their agreement in identifying the patients who centralized was 95% (Kappa 0.7) [18]. In a literature review by Aina et al. [17], the authors concluded that agreement in identifying centralization ranged between 88% and 100% (Kappa 0.51 to 0.96, mean 0.75).
The aims of the study were: To identify the prevalence of types of pain response to repeated movement and guided positioning in patients with sciatica? To examine the possible association between baseline pain responses; and the treatment outcome and baseline type of disc lesion.
Methods
This study is a secondary analysis of data from a prospective randomized controlled trial (RCT) investigating conservative treatment in patients suffering from sciatica. All patients were referred from private practitioners, rheumatologists or chiropractors to a specialist spine center for evaluation and treatment.
Inclusion and exclusion criteria
Patients were included if they were 18–65 years of age and had radicular pain of dermatomal distribution to the knee or below in one or both legs, leg pain ≥3 on a 1–10 point scale at first visit to the clinic, and a duration of sciatica between two weeks and one year. Patients were excluded if they had: Cauda Equina Syndrome, pending worker’s litigation, previous back surgery, spinal tumors, pregnancy, a first language other than Danish, or an inability to follow the rehabilitation protocol due to concomitant disease such as depression or heart failure.
The details of the original study have been published elsewhere [19] and are only briefly restated here. Patients were randomized to one of the two treatment programs; either ‘symptom-guided exercises’ or ‘sham exercises’ (for details http://www.sygehuslillebaelt.dk/wm335360 click exercise program or sham exercise). Both the treatment programs contained identical information and advice but differed in the type of exercise program that was included. The treatment lasted for 8 weeks with a minimum of four and a maximum of eight treatments. The findings from the initial examination, performed before randomization, including the pain response classification, were concealed from the treatment providers and therefore had no influence on the treatment administered.
Centralization procedures
The examiner at baseline was a physiotherapist with 10 years of clinical experience but no formal McKenzie Institute education. Another physiotherapist, whose training included a ‘Diploma in MDT’ from the McKenzie Institute, provided training in centralization and the use of standardized examination procedures to the baseline examiner and the treating therapists. One of the four treating therapists also had formal McKenzie Institute education. The examiner who performed the baseline assessment was blinded to the patient’s treatment allocation and MRI findings.
The definition of centralization used in this study was “the phenomenon by which distal limb pain emanating from the spine is immediately or eventually abolished in response to the deliberate application of loading strategies. Such loading causes reduction, then abolition of peripheral pain that appears to progressively retreat in a proximal direction” [8].
Operationalization
The examination was used to classify individual patients’ pain as displaying centralization, peripheralization or no effect. For those displaying centralization, sub-categories were determined. The assessment procedure was:
A thorough pain history was taken to determine if any positions and direction of movements increased or decreased symptoms. This could reveal the most likely spinal movement that would centralize the pain and give direction for the first movement tested.
At the onset of testing, the patient stood at a bench with the spine erect. Using a standardized text of instructions, the examiner instructed the patient to record on a pain drawing a) the exact location of the present pain and b) the pain intensity (0–10) for each region (lumbar, gluteal, thigh, crus and foot region).
The movement direction and position (lying, standing) in which pain was most likely to centralize was taken to its available end-range and performed repeatedly. The symptom response was continuously monitored. The test movement was continued until the pain was abolished or as long as the most distal pain continued to decrease.
If distal symptoms worsened, that specific movement or positioning was immediately discontinued.
All directions of repeated movements were tested with a maximum of 10 repetitions, until either centralization was reported or all movements in the standardized instructions were exhausted. Movement was always the first option, unless symptoms worsened, in which case positioning was used thereafter. At the conclusion, the impact of the most effective movement or positioning on the subject’s distal pain response was recorded.
After centralization had occurred or all possible movement or positioning tests had been performed, the patient walked freely around the room for approximately 1 min.
- After this testing procedure, the patient filled out a second pain drawing, blind to the first drawing. The two pain drawings were then compared by the examiner and an assessment regarding whether centralization had taken place was made according to the following criteria:
- Abolition centralization: the most distal pain was abolished and pain was recorded more proximally on the second drawing than on the first.
- Reduction centralization: the pain was located at the same distal location but with reduced intensity.
- Unstable centralization: the pain was reduced or abolished during the repeated movement testing or positioning but after resuming a weight-bearing position for one minute, the pain intensity level returned to the pre-testing intensity.
- Peripheralization: the most distal pain increased in intensity or area in all test movement directions or positions.
- No change: throughout testing, there was no change in the location and intensity of the distal symptoms.
Groups (a) + (b) + (c) were classified as centralizers and groups (d) + (e) as non-centralizers.
MRI
Lumbar MRI was performed immediately after the baseline examination, in an open low field 0.2 T, MRI unit with a body spine surface coil. The patients were placed in the supine position with extended hips and knees, producing a slight lumbar lordosis. Five sequences of localized images were taken, two coronal and three sagittal. The MRI scans were evaluated by the consultant radiologist, and classified into one of the five distinct groups of disc contour changes. The following classification terms were used: normal, bulging, focal protrusion, broad-based protrusion, extrusion and sequestration [20–22]. The intra- and inter-tester reliability for this classification system is high, with kappa values of 0.78 and 0.68, respectively [23]. The study group have earlier shown that there was no difference between the treatment groups in relation to the development of disc contour or nerve root compromise [24].
Association of types of pain response with MRI findings
It is believed that in normal discs and in discs with a bulge, it is unlikely that the annulus is ruptured and therefore the intra-discal pressure is intact. On the contrary, discs where the nucleus material is sequestrated or extruded, annular rupture has definitely occurred and intra-discal pressure is likely to be lost. In discs with focal or broad-based protrusions, both ruptures of the annulus and no ruptures are believed to occur. Therefore a comparison was made between patients with certain intact annulus and an intact inter-discal pressure and patients with a certain ruptured annulus and no inter-discal pressure. The first group was expected to have high ability to centralize. According to ‘the disc model’, all patients with a ruptured annulus would not be expected to centralize.
Data analysis
Categorical variables were tabulated and descriptive statistics used to report characteristics of the participants. To test for differences in outcome between the three centralization groups, ANCOVA was performed twice with improvement in activity limitation and improvement in leg pain as the outcome variables, while controlling for baseline gender, age and treatment allocation. The analysis was performed using Stata 8 (StataCorp, Texas, USA). A significance level of 5% (two-sided) was chosen for all tests.
The study was approved by the local Ethical Committee reference no. VP20010134.
Results
Consecutive patients were invited to participate in the original study and 181 agreed. Five were excluded at baseline as analgesic use just prior to the examination resulted in their having no pain at the time of examination, this meant that the capacity to perform a clinical examination that tested natural pain response was absent. Follow-up data were available for 165 patients hence 11 patients dropped out during the treatment period.
Demographic data
The mean age of the participants was 45 (37–52), with 48% being women. Sum score of positive straight leg raise (SLR), sensory and motor deficits and asymmetric reflexes in lower extremities (LE) was: 0 = 1%, 1 = 4%, 2 = 30%, 3 = 43%, 4 = 22%. The mean Roland Morris Disability Questionnaire score was 15.5 (11–18).
Prevalence of types of pain response to repeated movement and positioning
In this sample, 84.8% of people (95% CI, 79.6–90.5%) had one of the three types of centralization: 25.5% had abolition centralization, 43.6% reduction centralization, and 15.8% an unstable centralization. In contrast, 15.2% (95% CI, 9.4–20.3%) of people were non-centralizers, 7.3% were peripheralizers and 7.9% showed a response of no effect. Despite severe sciatica, no patient worsened or developed further neurological deficit or Cauda Equina Syndrome as a result of the assessment procedure.
The prevalence of types of disc lesions in the participants, as identified by MRI was: sequestrated discs 6%, extruded discs 31%, broad-based disc protrusion 9%, focal disc protrusion 38%, disc bulge 18% and normal discs 8%.
The duration of leg symptoms before the examination at baseline appeared to be evenly distributed between the different types of pain response.
Association of types of pain response with MRI findings
In this study, 83.7% (95% CI, 69–93%) of the people with normal discs or discs with a bulge and an intact inter-discal pressure were able to centralize. The patients with extruded and sequestered discs with certain lack of intra-discal presure had the highest centralization level of all, 93.5% (95% CI, 82–98%), despite the disc model predicting that none would be able to centralize (Table 1).
Table 1.
The prevalence of various disc lesions amongst the different pain response groups
| Normal | Bulge | Focal protrusion | Broad based protrusion | Extrusion | Sequestration | |
|---|---|---|---|---|---|---|
| Abolition centralization | 3 (22%) | 8 (28%) | 17 (27%) | 4 (33%) | 8 (22%) | 2 (22%) |
| Reduction centralization | 8 (57%) | 8 (28%) | 29 (46%) | 2 (16.5%) | 22 (59%) | 3 (33.5%) |
| Unstable centralization | 2 (14%) | 7 (24%) | 6 (9.5%) | 3 (25%) | 5 (13%) | 3 (33.5%) |
| Peripheralization | 0 (0%) | 3 (10%) | 5 (8%) | 1 (9%) | 1 (3%) | 1 (11%) |
| No change | 1 (7%) | 3 (10%) | 6 (9.5%) | 2 (16.5%) | 1 (3%) | 0 (0%) |
| Total | 14 (100%) | 29 (100%) | 63 (100%) | 12 (100%) | 37 (100%) | 9 (100%) |
Association of types of pain response with outcomes
The median improvement in activity limitation (RMQ scores) across all three centralization groups was 9.5 points at 8 weeks and 12.0 points at 12 months follow-up. A similar improvement was observed in the peripheralization group (7.0 points at 8 weeks and 14.0 points at 12 months). The ‘no effect’ group improved by 3.0 points at both follow-up time periods. There were no differences at any time period between the improvements in activity limitation experienced by people who centralized and those who peripheralized. The improvement in activity limitation in the ‘no effect’ group was less than those in the other groups at both time periods (p < 0.001) (Fig. 1). The improvement in the three different centralization groups was similar, the mean reduction in RMQ at the 8 weeks follow-up were: abolition centralization 8.1, reduction centralization 7.1 and unstable centralization 9.7.
Fig. 1.
Activity limitations measured as the median Roland Morris Disability Questionnaire sum score (0–23 scale) at baseline, 8 weeks and 1 year follow-up after treatment in the three groups with different response to repetitive movement and/or positioning
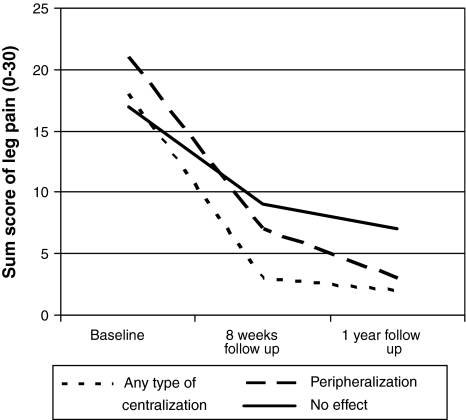
Overall, there were improvements in leg pain intensity (the sum of present, worst, mean leg pain in the last 2 weeks on a 0–30 scale) at both follow-up time periods. The median improvement in leg pain intensity across all the three centralization groups was 15 points at 8 weeks and 16 points at 12 months follow-up. A similar improvement was observed in the peripheralization group (14 points at 8 weeks and 18 points at 12 months). The ‘no effect’ group improved by 8 points at 8 weeks and 10 points at 12 months follow-up. The improvements in leg pain experienced in the ‘no effect’ group was less than those in the other groups at both time periods (p < 0.05) (Fig. 2).
Fig. 2.
The sum score of the present, mean and worst leg pain intensity at baseline, 8 weeks and 1 year follow-up
Discussion
In this study of 176 patients with sciatica, the prevalence of centralization, of any type, was high. Centralization and peripherilization predicted good outcomes at follow-up. There was no association between the type of disc lesions as identified by MRI and the pain response to repeated movement or positioning at baseline. The prevalence of centralization was similar in patients with an intact annulus to that in patients with confirmed annular rupture.
Prognosis
The improvement in activity limitation and leg pain in people whose pain centralized confirms previous findings that centralization is a predictor of a good outcome. The similar outcomes achieved by people who peripheralized is surprising. This positive prognosis for peripheralizers might be due to natural history or some form of treatment response. Werneke et al. [25] followed patients over time to monitor any change in their pain response to repeated movement, and found that some patients who were not initially centralizers later became centralizers.
The patients with the worst prognosis were in the “no change” group. The dynamic disc model proposed by [11], and supported by their data, suggests that patients whose pain is not affected by directional loading tests are unlikely to have symptoms of discal origin. The lack of improvement in the “no change” group appears to support this concept.
Centralization and intact annulus
It is has been proposed that centralization only occurs if the annulus is intact and the intra-discal hydrostatic mechanism is functioning normally [8]. Therefore patients with sequestrated or extruded discs should not be able centralize, in fact, 93.5% did centralize, which was 10% more than the group with a normal intact annulus. All types of pain responses were observed in all the various types of disc lesions, except peripheralization in normal discs. If the “dynamic disc model” is the sole explanation of centralization, our results are a contradiction of this widespread theory. There is clearly more to be investigated regarding the pathoanatomical explanations responsible for referred or radicular pain that changes location. The positive response after repeated movement could be due to a positive effect on the blood flow by decompressing the vasa nervorum, or a positive mechanical effect on the extruded disc material even when the annulus is ruptured.
Operationalization
To document when patients centralize, Donelson described the use of a pain drawing, upon which a grid is superimposed dividing the low back and legs into six regions. To be graded as centralization the most distal pain had to move from one region to another [10]. It is our belief however, that there is a lack of sensitivity in such a requirement for large changes in pain location. For example, that distal pain moving proximally from above the ankle to below the knee would not be recorded as centralization, even though the pain may have moved approximately 40 cm more centrally. Despite recommendations by Aina et al. [17] and Werneke and Hart [26], it was chosen in this study to define the centralization phenomenon to occur if a reduction of the most distal pain took place or the most distal pain moved centrally, regardless of the distance and independent of artificial borders. This method was assumed to be more sensitive in measuring centralization.
Prevalence
The patients in this study had considerable current leg pain at baseline examination, mean 4.5 (scale 0–10) after optional intake of analgesics, and 65% had 3 or 4 (of 4) positive root compression signs. These patients are typically not assessed using this examination procedure due to the clinicians fears of aggravating the symptoms. It is certainly noteworthy that 84.8% of patients with such severe pain and severe disc pathology were still able to centralize their pain. This is consistent with the literature as reviewed by [27] but contrary to Sufka et al. [14] found that the more distal the pain, the less likely that the patients would centralize. Kopp et al. [28] however, found that 52% of patients with neurological deficits were able to reduce their pain and recover their full ROM in comfort within 3–5 days of starting extension exercises.
Study limitations
In this study, patients were evaluated and classified in a single baseline session. Werneke, however, has shown that some centralizers are not identified until subsequent assessment sessions [26]. It is possible therefore, that some of our ‘non-centralizers’ would have been re-classified as centralizers with further assessment in subsequent sessions. But since 84.8% of the patients were classified as centralizers this number is likely to be very small. The opposite situation may also have occurred, where some of the patients classified in the Centralization groups (probably in the reduction or unstable group) might have become non-centralizers over time.
Conclusion
From a symptomatic point of view, it seems that no matter what type of disc lesion is found on MRI and despite the severity of the symptoms (leg pain) and neurological findings; it is possible for a majority of this subgroup of patients to positively affect their symptoms by centralization. It could be of great value for these patients to know how to gain relief while natural healing takes its course. This knowledge may be achieved by mechanical testing and the teaching of how to maintain control over symptoms.
Acknowledgments
We wish to thank Natalie DeMorton. B.App.Sc (Physio), Ph.D. for performing the ANCOVA analysis.
Conflict of interest
None.
Footnotes
The study was funded by The Regional Institute of Health Sciences Research.
References
- 1.Bigos L, et al. Acute low back problems in adults, clinical practice guidelines. Rockville: U.S. Department of Health and Human Services; 1994. pp. 1–160. [Google Scholar]
- 2.Manniche C et al (1999) Low back pain. Frequency, management and prevention from an HTA perspective. Danish Institute for Health Technology Assessment, Copenhagen, pp 1–107
- 3.Kelsey JL, White AA., III Epidemiology and impact of low-back pain. Spine. 1980;5:133–142. doi: 10.1097/00007632-198003000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Heliovaara M, Impivaara O, Sievers K, et al. Lumbar disc syndrome in Finland. J Epidemiol Community Health. 1987;41:251–258. doi: 10.1136/jech.41.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leboeuf-Yde C, Klougart N, Lauritzen T. How common is low back pain in the Nordic population? Data from a recent study on a middle-aged general Danish population and four surveys previously conducted in the Nordic countries. Spine. 1996;21:1518–1525. doi: 10.1097/00007632-199607010-00005. [DOI] [PubMed] [Google Scholar]
- 6.Manninen P, Riihimäki H, Heliövaara M. Incidence and risk factors of low-back pain in middle-aged farmers. Occup Med (Lond) 1995;45:141–146. doi: 10.1093/occmed/45.3.141. [DOI] [PubMed] [Google Scholar]
- 7.Shvartzman L, Weingarten E, Sherry H, et al. Cost-effectiveness analysis of extended conservative therapy versus surgical intervention in the management of herniated lumbar intervertebral disc. Spine. 1992;17:176–182. doi: 10.1097/00007632-199202000-00010. [DOI] [PubMed] [Google Scholar]
- 8.McKenzie R, May S. The lumbar spine. Mechanical diagnosis and therapy. 2. Waikanae, New Zealand: Spinal Publications New Zealand Ltd; 2003. [Google Scholar]
- 9.Donelson R, Silva G, Murphy K. Centralization phenomenon. Its usefulness in evaluating and treating referred pain. Spine. 1990;15:211–213. doi: 10.1097/00007632-199003000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Donelson R, Grant W, Kamps C, et al. Pain response to sagittal end-range spinal motion. A prospective, randomized, multicentered trial. Spine. 1991;16:206–212. doi: 10.1097/00007632-199106001-00006. [DOI] [PubMed] [Google Scholar]
- 11.Donelson R, Aprill C, Medcalf R, et al. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine. 1997;22:1115–1122. doi: 10.1097/00007632-199705150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Long AL. The centralization phenomenon. Its usefulness as a predictor or outcome in conservative treatment of chronic low back pain (a pilot study) Spine. 1995;20:2513–2520. doi: 10.1097/00007632-199512000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Karas R, McIntosh G, Hall H, et al. The relationship between nonorganic signs and centralization of symptoms in the prediction of return to work for patients with low back pain. Phys Ther. 1997;77:354–360. doi: 10.1093/ptj/77.4.354. [DOI] [PubMed] [Google Scholar]
- 14.Sufka A, Hauger B, Trenary M, et al. Centralization of low back pain and perceived functional outcome. J Orthop Sports Phys Ther. 1998;27:205–212. doi: 10.2519/jospt.1998.27.3.205. [DOI] [PubMed] [Google Scholar]
- 15.Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. A prospective analysis. Spine. 1999;24:676–683. doi: 10.1097/00007632-199904010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Fritz JM, Delitto A, Vignovic M, et al. Interrater reliability of judgments of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil. 2000;81:57–61. doi: 10.1016/s0003-9993(00)90222-3. [DOI] [PubMed] [Google Scholar]
- 17.Aina A, May S, Clare H. The centralisation phenomenon of spinal symptoms—a systematic review. Man Ther. 2004;9:134–143. doi: 10.1016/j.math.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Kilpikoski S, Airaksinen O, Kankaanpaa M, et al. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine. 2002;27:207–214. doi: 10.1097/00007632-200204150-00016. [DOI] [PubMed] [Google Scholar]
- 19.Albert HB. Manniche C (2011) The efficacy of systematic active conservative treatment for patients with severe sciatica. A single-blind randomized clinical controlled trial (In review) [DOI] [PubMed]
- 20.Milette PC. The proper terminology for reporting lumbar intervertebral disk disorders. Am J Neuroradiol. 1997;18:1859–1866. [PMC free article] [PubMed] [Google Scholar]
- 21.Brant-Zawadzki M, Jensen MC, Obuchowski N, et al. Interobserver and intraobserver variability in interpretation of lumbar disc abnormalities: a comparison of two nomenclatures. Spine. 1995;20:1257–1263. doi: 10.1097/00007632-199502000-00026. [DOI] [PubMed] [Google Scholar]
- 22.Masaryk TJ, Ross JS, Modic MT, et al. High-resolution MR imaging of sequestered lumbar intervertebral disks. Am J Roentgenol. 1988;150:1155–1162. doi: 10.2214/ajr.150.5.1155. [DOI] [PubMed] [Google Scholar]
- 23.Solgaard Sorensen J, Kjaer P, Jensen ST, et al. Low-field magnetic resonance imaging of the lumbar spine: reliability of qualitative evaluation of disc and muscle parameters. Acta Radiol. 2006;47:947–953. doi: 10.1080/02841850600965062. [DOI] [PubMed] [Google Scholar]
- 24.Jensen TS, Albert HB, Soerensen JS, Manniche C, Leboeuf-Yde C. Natural course of disc morphology in patients with sciatica: an MRI study using a standardized qualitative classification system. Spine. 2006;31:1605–1612. doi: 10.1097/01.brs.0000221992.77779.37. [DOI] [PubMed] [Google Scholar]
- 25.Werneke M, Hart D. Discriminant validity and relative precision for classifying patients with nonspecific neck and back pain by anatomic pain patterns. Spine. 2003;28:161–166. doi: 10.1097/00007632-200301150-00012. [DOI] [PubMed] [Google Scholar]
- 26.Werneke M, Hart DL, Resnik L, et al. Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther. 2008;38:116–125. doi: 10.2519/jospt.2008.2596. [DOI] [PubMed] [Google Scholar]
- 27.Wetzel FT, Donelson R. The role of repeated end-range/pain response assessment in the management of symptomatic lumbar discs. Spine. 2003;3:146–154. doi: 10.1016/s1529-9430(02)00565-x. [DOI] [PubMed] [Google Scholar]
- 28.Kopp JR, Alexander AH, Turocy RH, et al. The use of lumbar extension in the evaluation and treatment of patients with acute herniated nucleus pulposus. A preliminary report. Clin Orthop. 1986;202:211–218. [PubMed] [Google Scholar]