Abstract
Introduction
The effect size for exercise therapy in the treatment of chronic non-specific low back pain (cLBP) is only modest. This review aims to analyse the specificity of the effect by examining the relationship between the changes in clinical outcome (pain, disability) and the changes in the targeted aspects of physical function (muscle strength, mobility, muscular endurance) after exercise therapy.
Methods
We searched for exercise therapy trials for cLBP published up to 15 April 2010 in Medline, Embase, Cochrane Library, Cinahl, and PEDro. Two independent reviewers selected studies according to the inclusion criteria. Data extraction: one author extracted the data of the articles.
Results
Data synthesis: 16 studies with a total of 1,476 participants met the inclusion criteria. There was little evidence supporting a relationship between the changes in pain or physical function and the changes in performance for the following measures: mobility (no correlation in 9 studies, weak correlation in 1 study), trunk extension strength (7 and 2, respectively), trunk flexion strength (4 and 1, respectively) and back muscle endurance (7 and 0, respectively). Changes in disability showed no correlation with changes in mobility in three studies and a weak correlation in two; for strength, the numbers were four (no correlation) and two (weak correlation), respectively.
Conclusions
The findings do not support the notion that the treatment effects of exercise therapy in cLBP are directly attributable to changes in the musculoskeletal system. Future research aimed at increasing the effectiveness of exercise therapy in cLBP should explore the coincidental factors influencing symptom improvement.
Keywords: Chronic non-specific low back pain, Correlation, Clinical outcome, Physical performance, Exercise therapy
Introduction
Studies examining the effects of exercise therapy in the treatment of chronic non-specific low back pain (cLBP) show in general only moderate effectiveness [1–3]. This is often explained by the contradiction between the heterogeneity of cLBP patients and the uniformity of the exercise therapy approach [4]. In line with this approach lies the recommendation to sub-group patients and to develop relevant exercise programs for each group. However, there is little evidence that individually tailored or specific exercise programs show better success, which tends to question this approach [4]. Most exercise therapy trials report the changes in key outcome variables such as patient-rated pain, disability and global improvement, but they rarely examine these in relation to improvements in the targeted aspect of performance, e.g. strength or mobility. Hence, it cannot be assumed that the observed positive clinical outcome is a direct result of improvements in the specific functional deficit targeted by the treatment.
Recently, alternative theories have been proposed that aim to explain the lack of specificity of exercise therapy in cLBP. One suggests that the treatment effects of many cLBP therapies may be attributable to changes within the brain of cLBP patients rather than specific changes in the musculoskeletal system [4, 5]. Evidence supporting the involvement of cortical reorganisation in cLBP [6] comes from the finding of central nervous system changes [7–11] proportional to the severity and duration of the cLBP [4, 11, 12] and alterations (grey matter density loss) [13] in the brain of cLBP patients [4, 12, 14]. It is conceivable that other changes elicited by exercise therapy, e.g. improvements in self-efficacy, coping strategies and fear-avoidance [14–20], modification of motor control patterns as a consequence of a re-weighting of sensory input [21], changes in cortical organisation [22–25] or simply a positive therapist–patient interaction/relationship [26] may be responsible for the improvements in self-reported pain and disability.
Current treatments for cLBP may be ineffective because they are based on the unsubstantiated assumption that the problem is located in the lower back itself and is the result of a specific functional deficit that might be remedied by a specific type of exercise. The treatments applied to target these dysfunctions can be expensive, requiring individual treatment, specially trained therapists, and/or specialised equipment; if there is no evidence that specific exercises are actually required, then they represent an unnecessary drain on our limited health-care resources. If the observed alterations in the periphery, such as increased movement asymmetry and variability [27–29], reduced movement speed [30], increased muscle co-contraction [31, 32], and decreased back muscle endurance [33–35], strength [33, 35] and mobility [36] are compensatory rather than causative, then future research could be directed towards alternative (and perhaps less costly) intervention models with new approaches, e.g. strategies for re-training the cortical function [14, 37–42], hopefully generating more effective results in the treatment of cLBP.
The European guidelines for the management of cLBP [43] briefly reported on the relationship between changes in physical performance and changes in clinical outcome, and found that the associations were at best tenuous. The aim of this study was to perform a systematic review of the studies that have examined this phenomenon. Specifically, we evaluate the reported correlations between changes in clinical outcome(s) (pain, disability) and changes in physical function (range of motion, strength, and muscular endurance) as a result of physical therapy and exercise interventions in patients with cLBP.
Methods
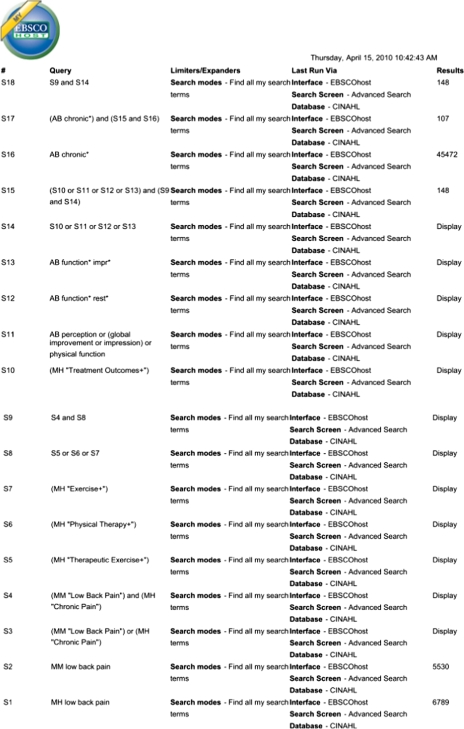
Individualised search strategies for Medline and Pre-Medline with Ovid, Cochrane library with Wiley, and Embase, Cinahl and PEDro databases (Appendix 1) were developed in collaboration with a librarian from the local university library. No limits were applied for the publication date of the articles. We used medical sub-headings as search terms, including low back pain, chronic disease, chronic low back pain, backache, treatment outcome, perception, pain measurement, pain, exercise therapy, physical therapy modalities, exercise movement techniques, and the free text words exercise therapy, physical therapy modalities, physiotherap*, exercise, global improvement, global impression, physical function, functional * restoration. We also reviewed the bibliographies of retrieved articles and relevant conference proceedings. The final search in all databases was performed on 15 April 2010.
Study selection
A study was considered eligible for inclusion in the review if it was a randomised controlled trial (RCT) or a non-randomised controlled trial (non-RCT) in English or German, examining the results of a physical activity intervention on patient reported outcome in cLBP. The studies had to investigate the effects of exercise and/or a physical therapy intervention of any type. Studies that evaluated the effectiveness of drugs, transcutaneous electrical stimulation and other non-exercise therapy modalities were excluded. The outcome measures of interest were: (1) outcomes related to physical function/performance (strength, mobility, muscular endurance) and (2) clinical outcomes (pain, disability). All participants with cLBP regardless of age were included. The definition of cLBP was the same as that given in the European guidelines for the management of cLBP [43].
Data collection and analysis
On the basis of the abstracts of the articles, studies were firstly eliminated if they did not focus on cLBP, exercise therapy or clinical and physical outcomes. Full text copies of the studies that were potentially suitable were then obtained and were independently assessed for inclusion by two of the authors (F.S. and E.D.B.) on the basis of the eligibility criteria. Studies were excluded if the individuals examined were not suffering from cLBP or if the studied patient groups were inhomogeneous due to the inclusion of a mixture of acute, subacute and chronic LBP patients. Further reasons for exclusion were (as per the European Guidelines [43]): a specific and uniform pathology (e.g. spondylolysis/spondylolisthesis, post-operative pain) and grouping of patients with mixed complaints (cLBP together with another complaint). In the event of disagreement between the raters, a third reviewer (B.W.) was available for consultation.
Data items
One author (F.S.) independently extracted the following information from each study selected for inclusion: (1) characteristics of the study participants; (2) type of intervention (including type, duration, frequency of training); (3) type of outcome measure (pain scores, disability scores, strength measurements, mobility scores, and muscular endurance measures); (4) statements concerning correlations and/or correlation coefficients for the relationship between clinical variables and performance outcomes. If a study reported both immediate post-intervention and follow-up data, we used the post-intervention data.
Risk of bias
The risk of bias and methodological quality of the RCT studies was assessed by the PEDro quality assessment tool, which is a ten-point checklist [44] that assesses randomisation, blinding of patients and therapists, follow-up, group baseline comparability and statistical analysis. All the identified RCTs had been already included in the PEDro database and we adopted their published rating (after double checking them ourselves and liaising with PEDro where discrepancies arose). The methodological quality of the non-RCT studies was assessed by means of the Downs and Black checklist [45]. Percentage agreement and Cohen’s kappa for the reviewers’ ratings were calculated with GRAPHPAD software (Version 2002–2005; GRAPHPAD Software Inc, San Diego, CA), and were interpreted in accordance with Landis and Koch’s [46] benchmarks for assessing the agreement between raters: poor (< 0), slight (0.0–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost perfect (0.81–1.0). The PRISMA-statement [47] was followed for reporting items of this systematic review and meta-analyses.
Data synthesis and analysis
The study results, i.e. correlation coefficients, were pooled using a random effects model. Appropriateness of pooling was checked through evaluating heterogeneity. Heterogeneity of the study findings was assessed with the I-squared statistic, where a value greater than 50% is considered to indicate substantial heterogeneity [48]. All other information was summarised and analysed qualitatively.
Results
Study selection
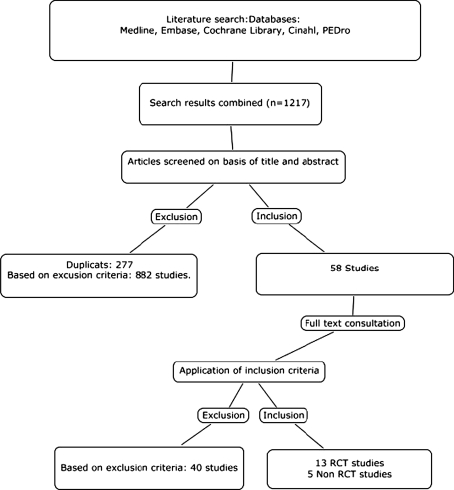
The database searches returned 1,217 articles of which 277 were duplicates. After reading the abstracts and applying the inclusion and exclusion criteria, 58 studies were considered potentially suitable and ordered for full text reading. After consulting the full texts, 16 studies, and 2 studies [16, 18] identified from a secondary analysis, with a total of 1,476 participants were identified as suitable for inclusion in the review (Fig. 1; Appendix 1).
Fig. 1.
Flow diagram showing study selection
Methodological quality
The results of the methodological quality assessment are presented in Tables 1 (non-RCTs) and 2 (RCTs). For all the RCTs, PEDro scores were available in the PEDro database and were therefore not analysed in Graphpad. For the non-RCTs, the reviewers agreed on 114 of 130 methodological ratings (87.7%) (item 27 in the Downs and Black checklist was not rated, because this item was not clearly explained). The remaining disagreements were resolved after discussion between the reviewers. The inter-reviewer κ statistic was 0.752 (95% CI 0.638–0.866). The median criteria score on the PEDro list (range 1–10) was 5.0 (Table 2).
Table 1.
Methodology assessment score of the non-RCTs with Downs and Black quality assessment
| Item | Criteria | Handa et al. [59] | Taimela et al. [51] | Keller et al. [18] | Demoulin et al. [57] | Mellin et al. [64] |
|---|---|---|---|---|---|---|
| 1 | Is the hypothesis/aim/objective of the study clearly described? | 1 | 1 | 1 | 1 | 1 |
| 2 | Are the main outcomes to be measured clearly described in the Introduction or Methods section? | 1 | 1 | 1 | 1 | 1 |
| 3 | Are the characteristics of the patients included in the study clearly described? | 1 | 1 | 1 | 1 | 1 |
| 4 | Are the interventions of interest clearly described? | 1 | 1 | 1 | 1 | 1 |
| 5 | Are the distributions of principal confounders in each group of subjects to be compared clearly described? | 0 | 0 | 0 | 0 | 0 |
| 6 | Are the main findings of the study clearly described? | 1 | 1 | 1 | 1 | 1 |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | 1 | 1 | 1 | 1 | 1 |
| 8 | Have all important adverse events that may be a consequence of the intervention been reported? | 0 | 0 | 0 | 0 | 0 |
| 9 | Have the characteristics of patients lost to follow-up been described? | 0 | 0 | 0 | 1 | 0 |
| 10 | Have actual probability values been reported (e.g. 0.035 rather than <0.05) for the main outcomes except where the probability value is less than 0.001? | 0 | 1 | 1 | 1 | 0 |
| 11 | Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | 0 | 0 | 0 | 0 | 0 |
| 12 | Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | 0 | 0 | 0 | 0 | 0 |
| 13 | Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? | 1 | 1 | 1 | 1 | 1 |
| 14 | Was an attempt made to blind study subjects to the intervention they have received? | 0 | 0 | 0 | 0 | 0 |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | 0 | 0 | 0 | 0 | 0 |
| 16 | If any of the results of the study were based on data dredging, was this made clear? | 1 | 1 | 1 | 1 | 1 |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or in case–control studies, is the time period between the intervention and outcome the same for cases and controls? | 1 | 1 | 1 | 1 | 0 |
| 18 | Were the statistical tests used to assess the main outcomes appropriate? | 1 | 1 | 1 | 1 | 1 |
| 19 | Was compliance with the intervention/s reliable? | 1 | 1 | 1 | 1 | 1 |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | 1 | 1 | 1 | 1 | 1 |
| 21 | Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited from the same population? | 0 | 0 | 0 | 0 | 0 |
| 22 | Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited over the same period of time? | 0 | 1 | 0 | 0 | 0 |
| 23 | Were study subjects randomised to intervention groups? | 0 | 0 | 0 | 0 | 0 |
| 24 | Was the randomised intervention assignment concealed from both patients and health care stay until recruitment was complete and irrevocable? | 0 | 0 | 0 | 0 | 0 |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main endings were drawn? | 0 | 0 | 0 | 0 | 0 |
| 26 | Were losses of patients to follow-up taken into account? | 0 | 0 | 0 | 1 | 1 |
| 27 | Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%? | – | – | – | – | – |
| Total | 12 | 14 | 13 | 15 | 12 |
Table 2.
Methodology assessment score of the RCTs with PEDro
| Item | Criteria | Elnaggar et al. [49] | Ferreira et al. [50] | Frih et al. [56] | Johannsen et al. [53] | Kankaanpää et al. [62] | Keller et al. [65] | Khalil et al. [55] | Kofotolis et al. [54] | Mannion et al. [58] | Mannion et al. [16] | Reilly et al. [52] | Rittweger et al. [17] | Roche et al. [63] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Eligibility criteria | 0a | 1a | 1a | 1a | 1a | 1a | 1a | 0a | 1a | 1a | 0a | 1a | 1a |
| 2 | Random allocation | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 3 | Concealed allocation | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 4 | Baseline comparability | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| 5 | Blind subjects | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6 | Blind therapists | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 7 | Blind assessors | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| 8 | Adequate follow-up | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9 | Intention-to-treat analysis | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 10 | Between-group comparisons | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 11 | Point estimates and variability | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| PEDro score | 6 | 8 | 4 | 4 | 5 | 5 | 4 | 4 | 6 | 6 | 4 | 4 | 4 |
aEligibility criteria is not used to calculate the PEDro score
All 16 studies explicitly stated the eligibility criteria employed, 12 studies reported using an appropriate method to generate the random allocation sequence, reported group similarity at baseline for the most important prognostic indicators, were successful in obtaining at least 85% of the data for the primary outcome(s), performed an intention-to-treat analysis, provided between-group comparisons and provided point estimates and measures of variability for the primary outcome(s). 2 of 16 studies reported using an appropriate method for concealment of treatment allocation. The outcome assessors were blinded in 12 of 16 studies.
Content of the studies
Characteristics of the patients, duration of exercises, interventions and main findings for each study are summarised in Table 3.
Table 3.
Study characteristics
| Study | Title | RCT or non-RCT | Subjects and age | Duration and study design | Outcome measures | Results | |
|---|---|---|---|---|---|---|---|
| 1 | Ben Salah Frih et al. [56] | Efficacy and treatment compliance of a home-based rehabilitation programme for chronic low back pain: a randomised, controlled study | RCT | 107 patients (82♀/25♂), 35.7 ± 0.8 years of age, with a mean (SD) duration of cLBP of 64.5 (8.7) months for group A and 67.7 (10.7) months for group B | Group A: 54 patients, two with history of spinal surgery Group B: 53 patients, seven with history of spinal surgery Exercise for a month: Group A: home-based exercises (9 exercises for strength, flexibility and self-positioning) daily 30 min Group B: Standard rehabilitation programme (analgesic electrotherapy, flexibility training, pain management, stretching and proprioception exercises and muscle strengthening exercises.) 90 min a day, three times a week |
Mobility: Schöber test, FTF Pain: VAS Disability: Quebec Questionnaire Strength: Shirado test Muscular endurance: Sorensen |
The home-based rehabilitation group showed a significant reduction in pain and disability at 1 year of follow-up. In contrast, the standard rehabilitation programme group improved in the physical parameters (mobility, strength and back muscle endurance) and showed a reduction in disability, but not pain (no correlation analyses conducted) |
| 2 | Demoulin et al. [57] | Benefits of a physical training programme after back school for chronic low back pain patients | Non-RCT | 40 patients (21♀/19♂), 25–65 years of age, with a mean duration of cLBP of 10 years | All 40 patients followed an educational back school programme. After that, 17 patients started physical training sessions twice a week for 6 weeks and were named Education-Physical Group (EPG). The other 23 constituted the control group | Mobility: modified Schöber test Pain: VAS Disability: Dallas Pain Questionnaire Strength: dynamic strength of abdominal muscles and isokinetic concentric tests for knee flexors and extensors on a Cybex Norm dynamometer Muscular endurance: static endurance of trunk extensor muscles |
In the EPG group, the improvement in knee extensor strength was significantly correlated with changes in disability (Dallas score) [r = −0.45, p = 0.05]. No correlation was found between the change in clinical outcomes (pain and disability) and other outcomes of physical function (abdominal dynamic strength, trunk muscle endurance) (correlation analyses conducted, but no correlation coefficients presented) |
| 3 | Elnaggar et al. [49] | Effects of spinal flexion and extension exercises on low back pain and spinal mobility in chronic mechanical low-back pain patients | RCT | 56 patients (28♀/28♂), 20–50 years of age Flexion group FG: 28 patients; duration of cLBP of 72.2 (61.2) months Extension group EG: 28 patients; duration of cLBP of 88.8 (80.0) months |
FG: trunk flexion exercises for a period of 2 weeks. Every week, seven sessions were given for each patient: 3 supervised by a physical therapist and the other 4 were home treatments done by each patient. Each exercise was done 10 times in two to three sets per session Each exercise was done 10 times in two to three sets per session EG: Spinal extension exercises for a period of 2 weeks, following the same previously mentioned outline for a total number of treatments of 14 sessions in 2 weeks time Total exercise time for both groups was 30 min per day |
Mobility: ROM Pain: McGill Q |
The authors reported a weak negative correlation between the changes in LBP severity and the changes in thoracolumbar spinal mobility (flexion group: r = −0.17, p = 0.4; extension group: r = −0.41, p = 0.03; flexion and extension group: r = −0.24, p = 0.07) |
| 4 | Ferreira et al. [50] | Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomised trial | RCT | 240 patients out (♀/♂not reported) of which 49 dropped out, between 18 and 80 years old, with at least 3 months of cLBP (no exact duration reported) Patients were randomly assigned to one of the following three groups: |
12 sessions in 8 weeks | Mobility: assessment of spinal stiffness by two raters Pain: VAS Disability: Roland Morris Q |
The authors reported no significant correlation between changes in spinal stiffness and changes in pain (MCE group: r = 0.06, p = 0.64; SMT group: r = 0.23, p = 0.53; GE group: r = −0.04, p = 0.77; all subjects: r = 0.11, p = 0.15), disability (MCE group: r = −0.02, p = 0.86; SMT group: r = 0.00, p = 0.98; GE group: r = 0.17, p = 0.19; all subjects: r = 0.06, p = 0.4) and function (MCE group: r = −0.16, p = 0.2; SMT group: r = −0.14, p = 0.3; GE group: r = −0.18, p = 0.2; all subjects: r = −0.18, p = 0.02) |
| General Exercise Group: subjects were taught the individual non-specific stretching and strengthening exercises | |||||||
| Motor Control Exercise Group: exercises aimed at improving function of specific muscles of the low back region (Richardson et al. 1999) to recruit the deep muscles of the spine and gradually reduce unwanted over-activity of the global muscles | |||||||
| General Exercise Group: 60 patients | |||||||
| Motor Control Exercise: 60 patients | |||||||
| Spinal Manipulative Treatment: 71 patients | Spinal Manipulative Treatment Group: joint mobilisation or manipulation techniques were applied on the subject’s spine or pelvis | ||||||
| 5 | Handa et al. [59] | The effect of trunk muscle exercises in patients over 40 years of age with chronic low back pain | Non-RCT | 52 patients (36♀ with 8.9 (SD 8.2) years of cLBP and 16♂ with 3.9 (SD 3.6) years of cLBP), aged 40 years or older | Patients were categorised into one of the following three groups: Group A: 28 patients without appreciable abnormalities on diagnostic imaging Group B: 12 patients with lumbar disherniation Group C: 12 patients who abandoned the exercise regimen early in the study period. The control group consisted of 60 healthy volunteers (40♀/20♂) All patients were with LBP were individually instructed to perform the following four exercises: supine trunk-raising exercise; prone trunk extension exercise; pelvic tilting exercises; double knee–chest exercises. Each exercise was performed for 5–10 s and repeated 5–10 times. The four exercises formed one course, and three courses of exercise were done daily |
Pain: VAS Disability: Japanese Orthopaedic Association score Strength: Myoret RZ-450 isokinetic/isometric trunk testing machine |
There was a positive correlation between the improvement in the Japanese Orthopaedic Association score (for the evaluation of the therapeutic outcome in LBP) and changes in isokinetic extension strength (r = 0.40; p < 0.05) and a positive correlation between the reduction in pain and changes in isometric extension strength (r = 0.56; p < 0.05). There was, however, no significant correlation between the changes in flexion strength and improvement in clinical symptoms |
| 6 | Johannsen et al. [53] | Exercises for chronic low back pain | RCT | Patients were randomly assigned to endurance training (trunk muscle endurance) or coordination training (emphasis on coordination, balance and stability) for a 12-week intervention of 24 × 1 h sessions 40 patients (13♀/14♂) of which 13 dropped out, aged 18–65, with at least 3 months’ cLBP (no exact duration reported) |
ETG: 10 min warming up on a bicycle. Dynamic exercises emphasising muscle endurance for the low back muscles, abdominal muscles and hip abductors, adductors, and knee extensors. Movements strictly controlled. Patients were encouraged to do the greatest possible extension disregarding pain. Each patient did as many repetitions as possible up to 100, with 30-s pauses per 10 repetitions 1-h weekly during a 3-month period. Afterwards the patients were encouraged to continue exercises at home |
Mobility: mobility score Pain: 5-point scale Disability: by asking 0–12 points Strength: isokinetic test |
The authors sought to identify individual factors that were responsible for the improvement in symptoms (pain) and disability. They compared clinical outcome measures (pain score, disability score) with various aspects of physical function (mobility, isokinetic back extension strength) and X-ray abnormalities, but no correlations were found (correlation analyses conducted, but no correlation coefficients presented) |
| CTG: 10 min warming up on the floor, including jogging. Exercises emphasising coordination, balance, and stability were performed. Up to 40 repetitions of each exercise | |||||||
| Both groups: after each session 10 min of stretching with static stretching of 30 s | |||||||
| 7 | Kankaanpää et al. [62] | The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability | RCT | 54 patients (22♀/37♂), 30–50 years of age, with cLBP duration of 10.9/5.8 (8.5)/(6.8) years for group A and 6.8/7.4 (6.1)/(6.7) years for group B | Patients were randomly assigned to one of the following two groups: Active Rehabilitation Group (30 patients): 24 exercise sessions during 12 weeks at each 1.5 h: active rehabilitation included physical exercises with specific equipment, together with stretching and relaxation exercises. Behavioural support was provided by the physiotherapist. Four specially designed training units (lumbar flexion, lumbar extension, lateral flexion, and rotation) were used specifically to train trunk muscle function and coordination | Pain: VAS Disability: Pain and Disability Index PDI Endurance: isoinertial back extension test Electromyography |
The authors found that most of the subjects in the active rehabilitation group who improved in lumbar muscle endurance also decreased in back pain intensity. They conceded that it was not possible to ascertain whether the subjects improved in lumbar endurance because of pain reduction due to the therapy or whether the endurance improvement due to training led to a decrease in back pain (no correlation coefficients presented). No specific correlation data provided or multivariable analyses carried out to examine other potential explanations for the concordance between performance and pain changes |
| Control treatment group (24 patients): treatment method was selected so that the efficacy was assumed to be minor | |||||||
| 8 | Keller et al. [18, 65] | Trunk muscle strength, cross-sectional area, and density in patients with chronic low back pain | RCT | 112 patients (68♀/56♂), 25–60 years, with a duration of cLBP of 9 years | Patients were randomly assigned to either: | Pain: VAS Disability: ODI Strength: isokinetic test Muscular endurance: Sorensen |
Patients in CEG improved significantly in muscle strength compared with patients who underwent lumbar fusion. Both groups showed a decrease in disability to the same extent (no correlation coefficient presented). The analysis conducted in 2008 reported correlation coefficients (for both groups) for changes in muscle strength and changes in disability (ODI) (r = 0.57) as well as between changes in muscle strength and changes in pain (r = 0.55) |
| Lumbar fusion group LFG (60 patients): lumbar instrumented fusion was performed with transpedicular screws of either the L4–L5 and/or L5–S1 segment. As a standard procedure, physical therapies gave advice about physical activity during the first 3 months after surgery. Follow-up after 3 and 6 months | |||||||
| Randomised to lumbar fusion or cognitive intervention and exercises | |||||||
| Cognitive intervention and exercise group CEG (52 patients): the duration of the supervised treatment period was at first 1 week followed by 2 weeks at home and another treatment period of 2 weeks | |||||||
| 9 | Khalli et al. [55] | Stretching in the rehabilitation of low-back pain patients | RCT | 28 subjects (13♀/15♂), aged 48.45 years ± 18.71, with cLBP duration of 6.4 (11.1) years for group A and 5.7 (9.4) years for group B | Patients were randomly assigned to one of the following two groups: | Mobility: ROM Pain: VAS Strength: static test |
The authors reported that changes in lumbar paraspinal muscle activity (measured by electromyography EMG) and functional measures (static back extension strength and mobility) did not correlate directly with the changes in pain (correlation analyses conducted, but no correlation coefficients presented). They concluded that functional improvements can occur without a corresponding reduction in pain |
| Group A: non-specific stretching group (Control group) | |||||||
| Group B: stretching group | |||||||
| Both groups underwent a multimodal 2-week rehabilitation programme (number of sessions not reported) and the stretching group performed additional stretching sessions 2 times a week | |||||||
| 10 | Kofotolis et al. [54] | Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain | RCT | 108 women (108♀) of which 10 dropped out, 40 ± 12 years of age, the duration of cLBP was 30.1 (6.2) weeks for group A, 32.7 (8.3) weeks for group B and 34.9 (8.4) weeks for group C | Patients were randomly assigned to one of the following three groups: | Mobility: sagittal mobility Pain: Borg Disability: ODI Muscular endurance: flexion and extension test | The authors measured improvements in lumbar mobility, static and dynamic back extension endurance, functional ability, pain and disability. The back pain intensity scores showed similar improvements in both the training groups and the control group. The authors concluded that improvements in physical measures do not necessarily lead to pain reduction in subjects with cLBP (no correlation analyses conducted) |
| Group A: rhythmic stabilisation training group (isometric trunk flexion/extension strength training) | |||||||
| Group B: combination of isotonic exercises group (alternating concentric and excentric contractions) | |||||||
| Group C: control group (no exercise) for a 4-week intervention of 20 sessions 4-week programs. Training frequencies for both groups A and B was 5 times per week. Training volume per session included 3 sets of 15 repetitions. Total duration of 30–45 min | |||||||
| 11 | Mannion et al. [16, 58] | Active therapy for chronic low back pain part 1–3 | RCT | 148 patients (approx. 58%♀/42%♂) with a duration of cLBP of 10.0 (9.5) years, 30-60 years of age, 132 completed the therapy | Patients were randomly assigned to one of the following three groups for a 3-month intervention (24 sessions): | Pain: VAS Disability: Roland Morris disability Mobility: ROM Strength: Maximum test Muscular endurance: Sorensen and isometric test |
The authors found that, in multivariate models, changes in physical performance (lumbar range of motion, strength) were not significantly related to changes in disability (as measured by the Roland and Morris disability scale). In univariate analyses there was a weak correlation between reduced disability and increased range of lumbar flexion (r = 0.18; p = 0.04). There was also a non-significant tendency for improvements in trunk extension strength to correlate with pain reduction (r = 0.20, p = 0.06) |
| Physiotherapy group: half-hour individual sessions focusing on improving the functional capacity | |||||||
| Muscle reconditioning group: 1 h sessions in patient groups of two or three. Submaximal isoinertial loading to the lumbar spine | |||||||
| Aerobics/stretching classes: 1 h sessions in small groups comprising aerobics and stretching | |||||||
| 12 | Mellin et al. [64] | Outcome of a multimodal treatment including intensive physical training of patients with chronic low back pain | Non-RCT | 194 patients (46%♀/54%♂), 42.8 mean years of age, with a mean of at least 3 months of cLBP (no exact duration reported) | The treatment consisted of a 3-day pre-programme, 5-week home training period, 4-week intensive inpatient treatment programme with physical exercises, cognitive behavioural group therapy, back school education, relaxation training, and socioeconomic and vocational counselling | Mobility: forward flexion and extension measured with inclinometers at sacrum and L1 Strength: Isometrically by a dynamometer method and isokinetic lifting strength Disability: Roland Morris Disability Questionnaire |
The authors reported a significant correlation between the changes in spinal mobility and changes in disability (based on the Roland Morris Disability Questionnaire), but only in women |
| 13 | Reilly et al. [52] | Differences between a supervised and independent strength and conditioning programme with chronic low back syndromes | RCT | 40 subjects (20♀/20♂) with at least 3 months of cLBP (no exact duration reported), age unclear | 6-month intervention of 96 sessions: Exercise group EG: subjects in the EG were given a predesigned exercise programme, but were also assigned a certified strength and conditioning specialist who would monitor and work with each subject individually for 6 months 4 times per week Control group CG: subjects were given predesigned exercise programs, comprising flexibility, strength, and aerobic exercises. 4 times per week for 6 months, for a total of 96 sessions |
Pain: VAS Strength: isodynamic measurements Muscular endurance: amount of repetition of the 60% one repetition maximum |
The authors performed a regression analysis to determine the factors that contributed to the reduction in pain in the supervised exercise group. Three factors emerged: the numbers of training sessions completed, percent body fat reduction and treadmill endurance. The coefficient of determination indicated that 82% of the variance in pain reduction was accounted for by these three factors. A strong correlation (correlation analyses conducted, but no correlation coefficients presented) was observed between the number of training sessions completed and the decrease in pain and reported relapses. The most crucial element of exercise success was compliance (no correlation coefficient presented) |
| 14 | Rittweger et al. [17] | Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomised controlled trial | RCT | 60 patients (24♀/26♂), of which 10 dropped out, aged 40–60 years, cLBP duration of 11.6 (10.0) years for group A and 14.5 (10.2) years for group B | Patients were randomly assigned to one of the following groups: Group A: isodynamic lumbar extension exercise (LEX) Group B: whole-body vibration exercise group VbX Both groups performed 18 exercises within 12 weeks: 2 units per week during the first 6 weeks and 1 unit per week thereafter |
Mobility: ROM Pain: VAS Strength: isometric test |
The authors found no significant correlation of improvement in pain and gain in torque within groups (correlation analyses conducted, but no correlation coefficients presented) |
| 15 | Roche et al. [63] | Comparison of a functional restoration programme with active individual physical therapy for patients with chronic low back pain: a randomised controlled trial | RCT | 132 patients (46♀/86♂), aged 18 to 50 years, with at least 3 months’ cLBP (no exact duration of pain reported) | Patients were randomly assigned to one of the following two groups: functional restoration programme FRP (68 patients): 5 weeks, treatment 6 h/day, 5 days/week: Supervised by a physiotherapist who adjusted the exercise intensity to each participant every week. Included warm-up, stretching techniques, muscular strengthening exercises and endurance exercises. Strengthening exercises were performed exclusively with isotonic techniques Active individual exercise AIT (64 patients): 5 weeks, 1 h 3 days/week and individual exercises to be performed at home 50 min twice a week: flexibility training and pain management, stretching, and proprioception exercises. Home exercises (stretching, jogging, and swimming). All exercises were isotonic and no specific equipment was required |
Mobility: ROM Pain: VAS Disability: Dallas Q Muscular endurance: Sorensen |
There were significant improvements in both groups in all parameters (trunk flexibility, pain intensity, Dallas Pain Questionnaire scores, daily activities, anxiety depression, social interest, work and leisure activities, and self-reported improvement) apart from endurance in group B (no correlation analyses conducted) |
| 16 | Taimela et al. [51] | Strength, mobility, their changes, and pain reduction in active functional restoration for chronic low back disorders | Non-RCT | 143 patients (88♀ with 9.3 ± 7.4 years and 55♂ with 9.2 ± 7.6 years of cLBP), with a mean age of 44 years | 12-week treatment period with 24 treatment visits. The treatment included mobility and muscle exercises with specific equipment together with stretching and relaxation exercises and functional muscle and coordination exercises | Mobility: measured with specially designed units Pain: pain reduction scale: decrease = 1; no change or increase = 0 Strength: flexion–extension of the lumbar spine assessed with specially designed measuring units |
The authors reported the correlations between pain reduction and lumbar flexion torque (r = 0.01), lumbar extension torque (r = −0.04), sagittal total mobility (r = −0.08), mean lumbar rotational torque (r = −0.03), rotational total mobility (r = −0.22, p < 0.01), mean lumbar lateral flexion torque −0.06 and total mobility in lateral flexion (r = −0.12). They concluded that the correlations between pain reduction and improvement in musculoskeletal function were low in patients with cLBP |
ROM range of mobility, VAS visual analogue scale, ODI Owestry Disability Index, FTF Fingertip-to-Floor test
Correlation between changes in physical function/performance and changes in pain
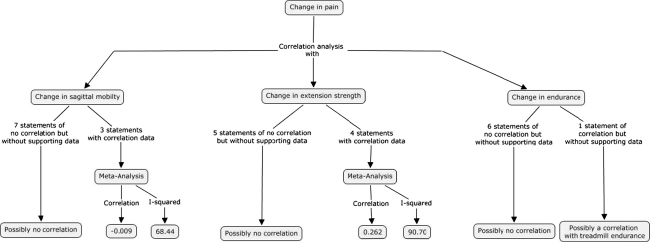
Figure 2 provides a summary of the study results describing the correlations between changes in physical function and changes in pain.
Fig. 2.
Summary of studies describing the relationship between changes in performance measures and changes in pain
Correlation between changes in pain and changes in sagittal mobility
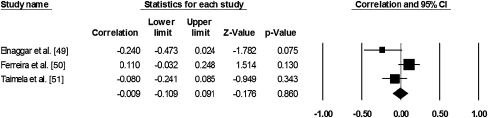
Ten studies were found (of which 3 gave the actual correlation coefficient data [49–51] and 7 did not [52–58]) that focused on the correlation between changes in pain and changes in sagittal mobility (flexion or flexion and extension). Nine studies reported that there was no correlation while one reported a low, but significant correlation [49]. We performed a meta-analysis using the data from the three studies reporting their correlation coefficients. The total correlation was very low (−0.009). However, the I-squared factor was high (68.4%) indicating high heterogeneity (Fig. 3).
Fig. 3.
Meta-analysis of the results of studies examining the relationship between the change in pain and change in spinal mobility in the sagittal plane
Correlation between changes in pain and changes in rotational and lateral mobility
Two studies examined the relationship between changes in pain and changes in rotational and lateral mobility. One study [49] found weak significant negative correlations between changes in pain and in rotational and lateral mobility (r = −0.35 and r = −0.35, respectively). The second study [51] found a weak significant correlation between pain and rotational total mobility (r = −0.22) and pain and total mobility in lateral flexion (r = −0.12).
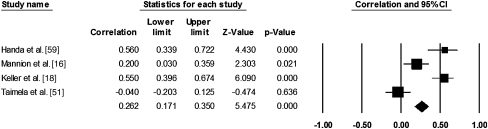
Correlation between changes in pain and changes in extension strength
Nine studies performed regression analyses to determine the relationship between changes in pain and changes in extension strength, of which four gave the actual correlation coefficient data [16, 18, 51, 59] and five did not [52–54, 56, 60]. Seven studies reported that there was no correlation between these attributes but five of these had provided no actual correlation coefficients. Among the four studies that reported the actual coefficients, two found no significant correlation [16, 51] (r = −0.4 and r = 0.2) and two [18, 59] reported a significant correlation (r = 0.56 and r = 0.55). The meta-analysis resulted in a total correlation of 0.262. Again, the I-squared factor was high (90.70%), indicating high heterogeneity (Fig. 4).
Fig. 4.
Meta-analysis of the results of studies examining the relationship between the change in pain and change in trunk strength
Correlation between changes in pain with changes in flexion strength
Five studies addressed the relationship between changes in pain and changes in trunk flexion strength. Four [52, 55, 57, 59] reported that there was no correlation (but did not give the actual correlation coefficients). The only study [51] that reported correlation coefficients showed a weak non-significant correlation (r = 0.01).
Correlation between changes in pain and changes in muscular endurance
Seven studies [52, 54, 56, 57, 61–63] examined the relationship between changes in pain and changes in muscular endurance, but none of them reported any specific correlation coefficients to substantiate their statements that there was no significant correlation between the variables.
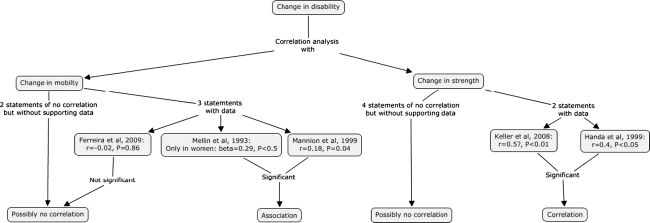
Correlation between changes in physical function/performance and changes in disability
Figure 5 provides a summary of the study results describing the correlations between changes in physical function and changes in disability.
Fig. 5.
Summary of studies describing the relationship between changes in performance measures and changes in disability
Correlation between changes in disability and changes in spinal mobility
Five studies (three providing the actual correlation coefficients and two without such data) focused on the relationship between changes in disability and changes in spinal mobility. Three of the five studies [36, 53, 57] reported that they found no correlation (one reporting r = −0.02, p = 0.86 [36]). Of the other two, one [64] found a significant correlation, but only in women (beta coefficient in multiple regression = 0.29, p < 0.05), while the second study [58] found a weak, but significant correlation (r = 0.18, p = 0.04). Due to the limited number of studies and the heterogeneity of the reported data, we refrained from performing a meta-analysis.
Correlation between changes in disability and changes in strength
Six studies (two providing the actual correlation coefficients and four without such data) investigated the relationship between changes in disability and changes in strength. Four reported that there was no correlation [53, 58, 60, 65] while two studies reported significant correlations (r = 0.57 [18], r = 0.40 [59]).
Correlation between changes in disability and changes in muscular endurance
No studies were found reporting the correlation between changes in disability and changes in muscular endurance.
Synthesis of results
The data analysis was mainly done qualitatively. Examination of just two relationships (pain and spinal mobility in the sagittal plane; pain and trunk extensor strength) resulted in sufficient studies reporting correlation coefficients to allow a meta-analysis to be carried out. These analyses resulted in high I-square values indicating large heterogeneity of the pooled data due to differences in intervention, control groups, duration of follow-up, outcome measures and study population.
Discussion
The aim of this systematic review was to study the relationship between changes in clinical outcome (pain, disability) and changes in physical function (range of motion, strength, muscular endurance) as a result of physical therapy and exercise interventions in cLBP. The majority of the 16 studies reviewed indicated that no such relationship exists. Changes in pain showed predominantly no significant correlation with changes in mobility (9 studies reported no significant correlation and just 1 reported a correlation), or trunk extensor strength (7 and 2 studies, respectively) or trunk flexor strength (4 studies and 1 study, respectively), and no correlation with changes in back muscle endurance (7 and 0 studies, respectively). The meta-analysis for the associations between changes in pain and mobility also supported this conclusion, although the I-squared coefficient of greater than 60% reduced the explanatory power of the pooled data. Overall, we conclude that there is not convincing evidence that changes in pain are strongly associated with changes in physical function/performance.
Similarly, for disability, a predominance of studies showed no significant correlation with changes in mobility (3 reported no significant correlation and 2 a significant correlation) and changes in trunk extensor strength (4 and 2 studies, respectively), although these findings were less consistent than for pain.
In general, these findings concur with those of other systematic reviews and individual studies [43, 66–69]. As highlighted before [16], if specific types of exercise therapy are to be advocated—especially those that aim to target specific functional deficits—it is important to be able to establish that improvements in the clinical complaint after therapy are in some way associated with the specific changes in function elicited. It is often not clear whether changes in performance are responsible for improvements in pain/disability or whether these two simply occur coincidentally and are actually mediated by a common third factor. If a correlation between the changes in two variables (e.g., muscle strength and disability) is established, this does not necessarily prove the existence of a causal relationship; the converse, however, i.e. a reduction in disability/pain in the absence of any significant change in the performance dimension under investigation or vice versa (i.e., no correlation), would certainly imply that the two were unrelated. The latter appears to be emerging as the overarching conclusion of the studies conducted on this theme to date, and might also explain why no particular type of exercise therapy is presently considered to be superior to any other [1, 70], i.e., because the exercise therapy is not actually eliciting its effects by improving specific aspects of (dys)function. The assumption that the reversal of deficits in physical function—believed to either predispose to LBP or to arise due to physical deconditioning subsequent to cLBP—results in a decrease in pain/disability was hence not substantiated by this review. Instead, our findings appear more congruent with reports showing that patients with cLBP do not necessarily show marked deficits in function [71, 72]. Recently, the popular intervention of core-strengthening exercises (focusing on strengthening the rectus abdominus, internal and external obliques, and erector spinae muscles) was questioned in a study that sought to compare this type of exercise with a general non-specific strengthening programme [73]. The outcomes were similar in the two treatment groups, and the authors concluded that focusing specifically on core exercises might be a potential mistake in the rehabilitation of cLBP [73]. Furthermore, it was shown in other studies that even stretching exercises appeared to improve strength [55], which is difficult to explain on any physiological basis. A noteworthy feature of the trials included in this review was the large variability in exercise interventions. The diversity in the activities prescribed (e.g. strength and endurance training, interventions, with or without counselling) reflects the absence of consensus on the optimal activity programme for cLBP. Guidelines report that exercises may include aerobic activity, movement instruction, muscle strengthening, posture control and stretching, but at the same time provide no information about the required intensity, frequency, loading, progression, etc. for the chosen training programme. However, it is conceivable that these same factors—that undoubtedly influence the prescription of exercise in relation to medical conditions such as hypertension or obesity—are of less relevance when prescribing exercise for cLBP. Indeed, if the main aim of exercise therapy in cLBP is to get patients moving again and be able to confront their fears and anxieties about physical activity and movement, then the method used to do this may be immaterial. And if this were indeed the case, it may have the fortuitous side-effect that it would open up the array of potential options for the type of exercise to be carried out, allowing consideration of the all-important issues of cost, access to facilities and patient-preferences.
The biological mechanisms explaining the effects of exercise therapy are not yet clear [74], but the findings of the present review suggest that the improvements in clinical outcome do not result from local (muscle, joint, etc.) changes. Other possible explanations are that they derive from more central effects [14–20], perhaps as a correction of a distorted “body schema” [4, 14] or altered cortical representation of the back [22–25], from modification of motor control patterns as a consequence of a reweighting of sensory input [21], or simply from a positive therapist–patient interaction/relationship [26]. Several studies have reported a correlation between psychological status and low back pain or pain tolerance [15, 58, 75–78]. The efficacy of treatments that solely focus on psychological targets has, however, been shown to be small [4]. These psychological phenomena, similar to the peripheral physical deficits, may also be responses to an altered body schema in the sense of sensory–motor incongruence that causes fear [4]. Exercise therapy seems to positively influence psychological variables such as fear-avoidance beliefs, catastrophising and self-efficacy regarding pain-control [79], in addition to providing physical benefits. Possibly by experiencing no harm in completing exercises, patients gain trust in the function of their back and thereby adjust their irrational cognitions and appraisals [79], whilst simultaneously improving their physical function.
Based on the findings of our review and on similar information from other systematic reviews and studies [43, 66–69], we suggest that changes in physical function are largely unable to explain changes in the clinical condition in cLBP patients, and that the important “side effects” of exercise therapy (including, amongst other things, changes in psychological variables such as fear-avoidance beliefs, catastrophising and self-efficacy regarding pain-control) should be more specifically emphasised and investigated in future rehabilitation programs.
Limitations
We used a structured study protocol to guide our search strategy, study selection, extraction of data and statistical analysis. However, a number of possible limitations of this review should be noted. First, the search strategy was limited to published studies identified through the selected search engines. Second, as noted, a publication bias may have been present, as well as a language bias, given that we restricted our search to English and German language publications. Third, as there were only 12 randomised trials, we also included several observational studies, the results of which may be affected by confounding bias due to the absence of random assignment. However, as the focus of our analysis was not the relative efficacy of different treatments, this was expected to be of little consequence. The literature search for this review revealed 58 studies that potentially could have been included, but more than half of them had not conducted any correlation analyses. We tried to obtain the original data by contacting the authors of the studies that had failed to report actual correlation data, either by email, telephone or both. Unfortunately, the few who responded either no longer had access to the data or were not interested in providing their data. This undoubtedly resulted in a loss of potential information. A further problem was that most studies that did conduct correlation analyses, did not report any corresponding data (correlation coefficients) substantiating their reported non-significant correlations that would otherwise have allowed for quantitative data analysis with meta-analyses. Finally, the interventions were heterogeneous in their design and of variable quality.
Future thoughts
Intervention strategies that focus solely on the symptom area in the lower back should be extended to apply a more global treatment approach. Both psychological and psychosocial interventions in addition to conventional exercise therapy may have a more positive effect on treatment outcome [80–90]. The targeted effect of such an approach would be the development of a sense of control over pain and the elimination of pain-avoidance mechanisms, whilst simultaneously improving overall physical fitness/function. Emphasis would shift from the “reversal of specific performance deficits” to the “adoption of enjoyable health-promoting physical activity” and this would potentially be associated with a wider choice and reduced cost. The availability of and access to such treatments might also be broadened by offering, e.g. group treatment sessions in community-based (rather than medical) settings. The exercise programs might include the training of proprioception, sensorimotor control and postural balance [91], in addition to the more conventional aspects of performance (strength, mobility, etc.). Lastly, the beneficial psychological effects of exercise should be investigated in greater detail. A better knowledge of the psychological changes induced by physical activity and training, and any accompanying “placebo” effects or educational effects due to the therapist–patient interaction, has the potential for enhancing the efficacy of exercise as a treatment for cLBP.
Conclusions
We conclude that the available literature does not appear to support a convincing association between changes in clinical outcome and changes in physical function after exercise therapy for cLBP. We hypothesise that the beneficial effects of exercise are more “central” than local, perhaps involving psychological, cognitive or neurophysiological (cortical organisation) adaptations. Thus, instead of trying to subdivide cLBP patients into further subgroups on the basis of specific functional deficits, future therapy approaches might better focus on influencing these central factors in cLBP patients.
Acknowledgments
We acknowledge the financial support of the Institute of Human Movement Sciences and Sport, Swiss Federal Institute of Technology, Zürich, Switzerland. We would like to thank the librarians of the Swiss Federal Institute of Technology Library, Zürich, for their assistance with the literature search.
Conflict of interest
None.
Appendix 1: Search strategies used in Ovid, Cochrane, Embase, Cinahl and PEDro databases
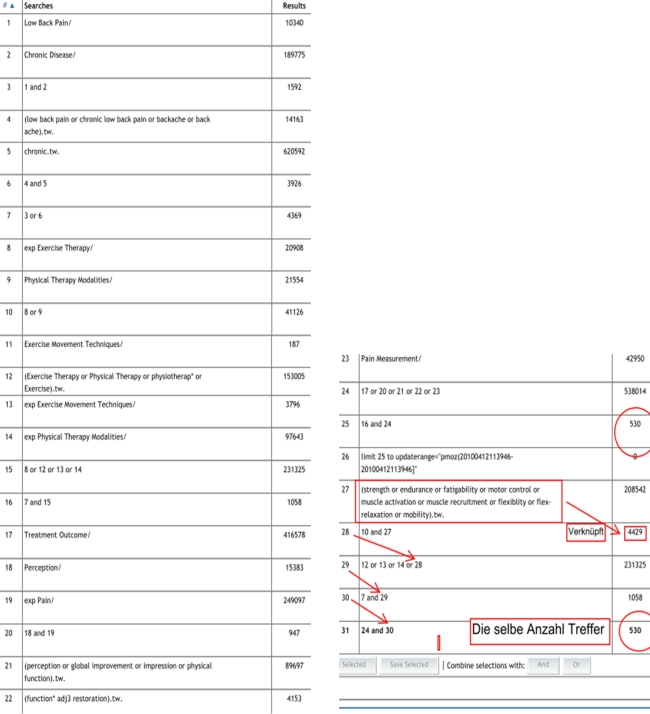
Ovid Medline Database search
Cochrane search with Wiley InterScience
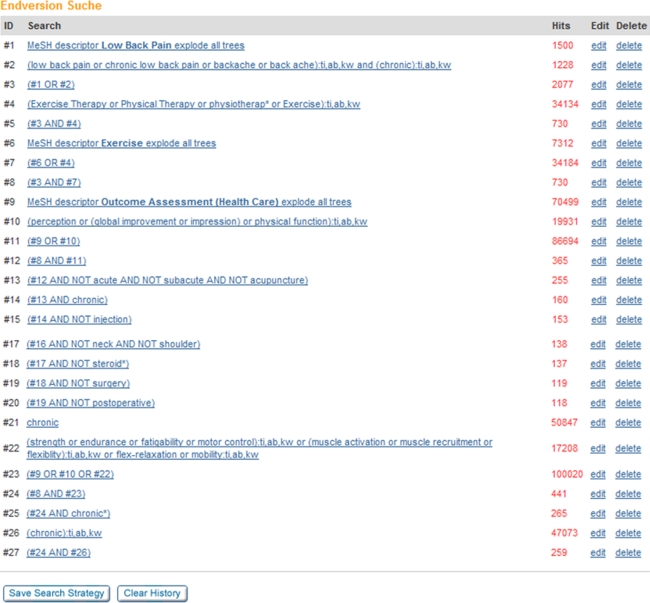
Embase search
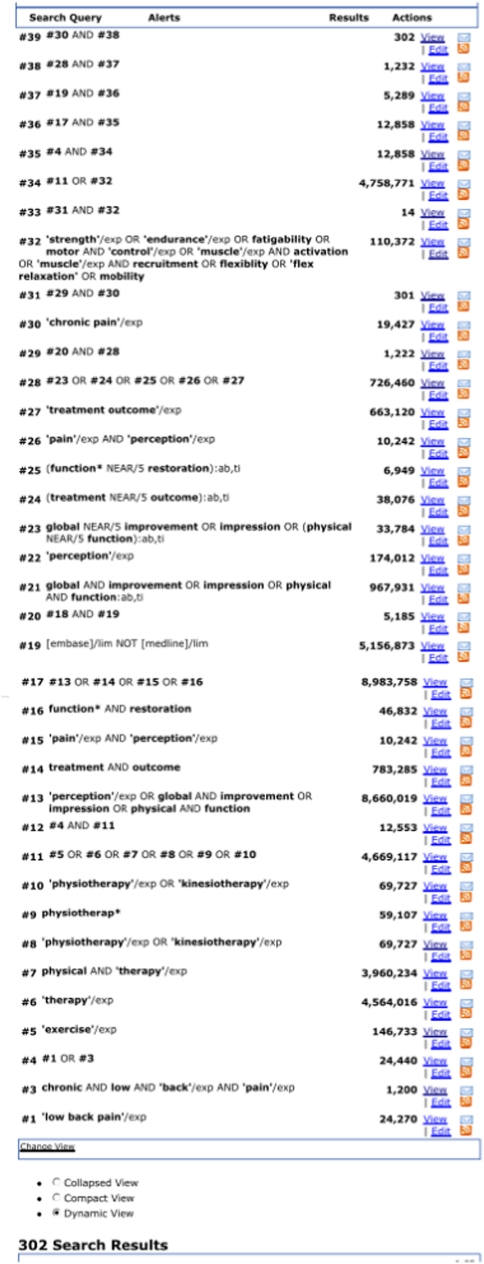
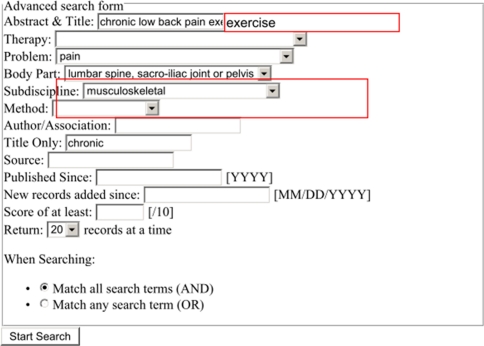
Cinahl search
PEDro search
Appendix 2
See Table 4:
Table 4.
Excluded studies after full text consultation
| Author/year | Title | Exclusion criteria | |
|---|---|---|---|
| 1 | Akbari (2008) | The effect of motor control exercise versus general exercise on lumbar local stabilising muscles thickness: randomised controlled trial of patients with chronic low back pain | Muscle thickness is not one of the specific targeted aspects of training |
| 2 | Andrade (2008) | [Back school for patients with non-specific chronic low back pain: benefits from the association of an exercise program with patient’s education] | Language (Portuguese) |
| 3 | Bayramoglu (2001) | Isokinetic measurement of trunk muscle strength in women with chronic low back pain | No correlation information |
| 4 | Bertocco (2002) | Controlled study on the efficacy of two different treatments in obese patients affected by chronic low back pain, assessed by an isokinetic device. (Analysis of muscle strength and spinal mobility) | No correlation information |
| 5 | Callaghan (1994) | Evaluation of a back rehabilitation group for chronic low back pain in an out-patient setting | No correlation information |
| 6 | Chan (2008) | The correlations among pain, disability, lumbar muscle endurance and fear-avoidance behaviour in patients with chronic low back pain | No correlation information |
| 7 | Demoulin (2010) | Effectiveness of a semi-intensive multidisciplinary outpatient rehabilitation program in chronic low back pain | No correlation information |
| 8 | Dundar (2008) | Clinical effectiveness of aquatic exercise to treat chronic low back pain: a randomised controlled trial | No correlation information |
| 9 | Estlander (1991) | Effects and follow-up of a multimodal treatment program including intensive physical training for low back pain patients | No correlation information |
| 10 | Fransoo (2006) | Comparison of three types of treatment for lower back pain (French) | Language, not chronic LBP |
| 11 | Friedrich (2005) | Long-term effect of a combined exercise and motivational program on the level of disability of patients with chronic low back pain | No reports on targeted aspects of training! |
| 12 | Friedrich (1997) | Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomised controlled trial | No correlation information |
| 13 | Gagnon (2005) | Efficacy of Pilates Exercises as Therapeutic Intervention in Treating Patients with LBP | Mixed subacute and chronic |
| 14 | Gladwell (2006) | Does a Program of Pilates Improve Chronic Non-Specific c Low Back Pain? | No correlation information |
| 15 | Harts (2008) | A high-intensity lumbar extensor strengthening program is little better than a low-intensity program or a waiting list control group for chronic low back pain: a randomised clinical trial | No correlation information |
| 16 | Helmhout (2004) | Comparison of a high-intensity and a low-intensity lumbar extensor training program as minimal intervention treatment in low back pain: a randomised trial | No correlation information |
| 17 | Hildebrandt (1996) | [Multidisciplinary treatment program for chronic low back pain, part 1. Overview] | No correlation information |
| 18 | Holmes (1996) | Comparison of female geriatric lumbar extension strength: asymptotic versus chronic low back pain patients and their response to active rehabilitation | No correlation information |
| 19 | Kell (2009) | A comparison of two forms of periodised exercise rehabilitation programs in the management of chronic non-specific low back pain | No correlation information |
| 20 | Kuukkanen (1996) | Muscular performance after a 3 month progressive physical exercise program and 9 month follow-up in subjects with low back pain. A controlled study | Mixed population |
| 21 | Kuukkanen (2000) | Effects of a three-month therapeutic exercise programme on flexibility in subjects with low back pain | Mixed population |
| 22 | Limke (2008) | Randomised trial comparing the effects of one set vs. two sets of resistance exercises for outpatients with chronic low back pain and leg pain | No correlation information |
| 23 | Marshall (2006) | Evaluation of functional and neuromuscular changes after exercise rehabilitation for low back pain using a Swiss ball: a pilot study | No correlation information |
| 24 | Martin (1985) | Physiotherapy exercises for low back pain: process and clinical outcome | Mixed population |
| 25 | Maul (2005) | Long-term effects of supervised physical training in secondary prevention of low back pain | Not chronic LBP |
| 26 | McIIveen (1998) | A randomised controlled study of the outcome of hydrotherapy for subjects with low back or back and leg pain | No correlation information |
| 27 | Miller (2005) | A comparison of the Mckenzie approach to a specific spine stabilisation program for chronic low back pain | Not chronic LBP according to the definition used here |
| 28 | Miltner (2001) | [Strengthening lumbar extensors-therapy of chronic back pain—an overview and meta-analysis] | Systematic review |
| 29 | Mirovsky (2006) | The effect of ambulatory lumbar traction combined with treadmill on patients with chronic low back pain | No correlation information |
| 30 | Olivier (2008) | [Does exercise therapy for chronic lower back pain require daily isokinetic reinforcement of the trunk muscles?] | Language (French) |
| 31 | Risch (1993) | Lumbar strengthening in chronic low back pain patients. Physiologic and psychological benefits | No correlation information |
| 32 | Saur (1996) | [Multidisciplinary treatment program for chronic low back pain, part 2. Somatic aspects] | No correlation information |
| 33 | Sertpoyraz (2009) | Comparison of isokinetic exercise versus standard exercise training in patients with chronic low back pain: a randomised controlled study | No correlation information |
| 34 | Sjogren (1997) | Group hydrotherapy versus group land-based treatment for chronic low back pain | No correlation information |
| 35 | Sokunbi (2008) | A randomised controlled trial (RCT) on the effects of frequency of application of spinal stabilisation exercises on multifidus cross-sectional area (MFCSA) in participants with chronic low back pain | No reports on physical function |
| 36 | Storheim (2000) | The effect of intensive group exercise in patients with chronic low back pain | No correlation information |
| 37 | Tekur (2008) | Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: a randomised control study | No correlation information |
| 38 | Udermann (1999) | Back pain: The effect of physiological and educational treatment modalities on various outcome measures | Full text not available |
| 39 | Winter (2002) | Effects of aquatic lumbar stabilisation and strengthening exercise protocol on chronic low back pain patients | No correlation information |
| 40 | Yeung (2003) | The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low back pain | No correlation information |
References
- 1.Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res: Clin Rheumatol. 2010;24(2):193–204. doi: 10.1016/j.berh.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Howard PD, Hudicka K, Keating C, Neidig N, Quiros S. The effect of trunk strengthening on chronic low back pain: a systematic review of the literature. Orthop Phys Ther Pract. 2010;22(1):19–22. [Google Scholar]
- 3.Keller A, Hayden J, Bombardier C, Tulder M. Effect sizes of non-surgical treatments of non-specific low-back pain. Eur Spine J. 2007;16(11):1776–1788. doi: 10.1007/s00586-007-0379-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wand BM, O’Connell NE. Chronic non-specific low back pain—sub-groups or a single mechanism? BMC Musculoskelet Disord. 2008;9:11. doi: 10.1186/1471-2474-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flor H, Knost B, Birbaumer N. Processing of pain- and body-related verbal material in chronic pain patients: central and peripheral correlates. Pain. 1997;73(3):413–421. doi: 10.1016/S0304-3959(97)00137-1. [DOI] [PubMed] [Google Scholar]
- 6.Flor H, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci Lett. 1997;224(1):5–8. doi: 10.1016/S0304-3940(97)13441-3. [DOI] [PubMed] [Google Scholar]
- 7.Grachev ID, Fredrickson BE, Apkarian AV. Abnormal brain chemistry in chronic back pain: an in vivo proton magnetic resonance spectroscopy study. Pain. 2000;89(1):7–18. doi: 10.1016/S0304-3959(00)00340-7. [DOI] [PubMed] [Google Scholar]
- 8.Siddall PJ, Stanwell P, Woodhouse A, Somorjai RL, Dolenko B, Nikulin A, Bourne R, Himmelreich U, Lean C, Cousins MJ, Mountford CE. Magnetic resonance spectroscopy detects biochemical changes in the brain associated with chronic low back pain: a preliminary report. Anesth Analg. 2006;102(4):1164–1168. doi: 10.1213/01.ane.0000198333.22687.a6. [DOI] [PubMed] [Google Scholar]
- 9.Giesecke T, Gracely RH, Clauw DJ, Nachemson A, Duck MH, Sabatowski R, Gerbershagen HJ, Williams DA, Petzke F (2006) Central pain processing in chronic low back pain. Evidence for reduced pain inhibition. Schmerz 20(5):411–414, 416–417. doi:10.1007/s00482-006-0473-8 [DOI] [PubMed]
- 10.Small DM, Apkarian AV. Increased taste intensity perception exhibited by patients with chronic back pain. Pain. 2006;120(1–2):124–130. doi: 10.1016/j.pain.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Baliki MN, Chialvo DR, Geha PY, Levy RM, Harden RN, Parrish TB, Apkarian AV. Chronic pain and the emotional brain: specific brain activity associated with spontaneous fluctuations of intensity of chronic back pain. J Neurosci. 2006;26(47):12165–12173. doi: 10.1523/JNEUROSCI.3576-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, Gitelman DR. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. J Neurosci. 2004;24(46):10410–10415. doi: 10.1523/JNEUROSCI.2541-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt-Wilcke T, Leinisch E, Ganssbauer S, Draganski B, Bogdahn U, Altmeppen J, May A. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain. 2006;125(1–2):89–97. doi: 10.1016/j.pain.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Wand BM, Parkitny L, O’Connell NE, Luomajoki H, McAuley JH, Thacker M, Moseley GL. Cortical changes in chronic low back pain: current state of the art and implications for clinical practice. Man Ther. 2011;16(1):15–20. doi: 10.1016/j.math.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Mannion AF, Taimela S, Müntener M, Dvorak J. Active therapy for chronic low back pain part 1. Effects on back muscle activation, fatigability, and strength. Spine. 2001;26(8):897–908. doi: 10.1097/00007632-200104150-00013. [DOI] [PubMed] [Google Scholar]
- 16.Mannion AF, Dvorak J, Taimela S, Muntener M. Kraftzuwachs nach aktiver therapie bei patienten mit chronischen ruckenschmerzen (LBP): muskulare adaptationen und klinische relevanz (Increase in strength after active therapy in chronic low back pain (CLBP) patients: muscular adaptations and clinical relevance) [German] Der Schmerz. 2001;15(6):468–473. doi: 10.1007/s004820100034. [DOI] [PubMed] [Google Scholar]
- 17.Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine. 2002;27(17):1829–1834. doi: 10.1097/00007632-200209010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Keller A, Brox JI, Reikerås O (2008) Predictors of change in trunk muscle strength for patients with chronic low back pain randomized to lumbar fusion or cognitive intervention and exercises. Pain Med (Malden, Mass) (6):680–687 [DOI] [PubMed]
- 19.Hakkinen A, Hakkinen K, Hannonen P, Alen M. Strength training induced adaptations in neuromuscular function of premenopausal women with fibromyalgia: comparison with healthy women. Ann Rheum Dis. 2001;60(1):21–26. doi: 10.1136/ard.60.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smeets RJE, Wade D, Hidding A, Leeuwen PJC, Vlaeyen JWS, Knottnerus JA. The association of physical deconditioning and chronic low back pain: a hypothesis-oriented systematic review. Disabil Rehabil. 2006;28(11):673–693. doi: 10.1080/09638280500264782. [DOI] [PubMed] [Google Scholar]
- 21.Popa T, Bonifazi M, Della Volpe R, Rossi A, Mazzocchio R. Adaptive changes in postural strategy selection in chronic low back pain. Exp Brain Res. 2007;177(3):411–418. doi: 10.1007/s00221-006-0683-4. [DOI] [PubMed] [Google Scholar]
- 22.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 23.Crombez G, Eccleston C, Baeyens F, Houdenhove B, Broeck A. Attention to chronic pain is dependent upon pain-related fear. J Psychosom Res. 1999;47(5):403–410. doi: 10.1016/S0022-3999(99)00046-X. [DOI] [PubMed] [Google Scholar]
- 24.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1–2):329–339. doi: 10.1016/S0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 25.Woby SR, Roach NK, Urmston M, Watson PJ. Outcome following a physiotherapist-led intervention for chronic low back pain: the important role of cognitive processes. Physiotherapy. 2008;94(2):115–124. doi: 10.1016/j.physio.2007.08.008. [DOI] [Google Scholar]
- 26.Klaber Moffett JA, Richardson PH. The influence of the physiotherapist-patient relationship on pain and disability. Physiother Theory Pract. 1997;13(1):89–96. doi: 10.3109/09593989709036451. [DOI] [Google Scholar]
- 27.Keefe FJ, Hill RW. An objective approach to quantifying pain behavior and gait patterns in low back pain patients. Pain. 1985;21(2):153–161. doi: 10.1016/0304-3959(85)90285-4. [DOI] [PubMed] [Google Scholar]
- 28.Selles RW, Wagenaar RC, Smit TH, Wuisman PI. Disorders in trunk rotation during walking in patients with low back pain: a dynamical systems approach. Clin Biomech (Bristol, Avon) 2001;16(3):175–181. doi: 10.1016/S0268-0033(00)00080-2. [DOI] [PubMed] [Google Scholar]
- 29.Vogt L, Pfeifer K, Portscher M, Banzer W. Influences of nonspecific low back pain on three-dimensional lumbar spine kinematics in locomotion. Spine (Phila Pa 1976) 2001;26(17):1910–1919. doi: 10.1097/00007632-200109010-00019. [DOI] [PubMed] [Google Scholar]
- 30.Marras WS, Ferguson SA, Gupta P, Bose S, Parnianpour M, Kim JY, Crowell RR. The quantification of low back disorder using motion measures. Methodology and validation. Spine (Phila Pa 1976) 1999;24(20):2091–2100. doi: 10.1097/00007632-199910150-00005. [DOI] [PubMed] [Google Scholar]
- 31.Ferguson SA, Marras WS, Burr DL, Davis KG, Gupta P. Differences in motor recruitment and resulting kinematics between low back pain patients and asymptomatic participants during lifting exertions. Clin Biomech (Bristol, Avon) 2004;19(10):992–999. doi: 10.1016/j.clinbiomech.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Marras WS, Davis KG, Kirking BC, Granata KP. Spine loading and trunk kinematics during team lifting. Ergonomics. 1999;42(10):1258–1273. doi: 10.1080/001401399184938. [DOI] [PubMed] [Google Scholar]
- 33.Holmstrom E, Moritz U, Andersson M. Trunk muscle strength and back muscle endurance in construction workers with and without low back disorders. Scand J Rehabil Med. 1992;24(1):3–10. [PubMed] [Google Scholar]
- 34.Jorgensen K, Nicolaisen T. Trunk extensor endurance: determination and relation to low-back trouble. Ergonomics. 1987;30(2):259–267. doi: 10.1080/00140138708969704. [DOI] [PubMed] [Google Scholar]
- 35.Nicolaisen T, Jorgensen K. Trunk strength, back muscle endurance and low-back trouble. Scand J Rehabil Med. 1985;17(3):121–127. [PubMed] [Google Scholar]
- 36.Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Maher C, Refshauge K (2009) Relationship between spinal stiffness and outcome in patients with chronic low back pain. Man Ther (1):61–67 [DOI] [PubMed]
- 37.Moseley GL. Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 2006;67(12):2129–2134. doi: 10.1212/01.wnl.0000249112.56935.32. [DOI] [PubMed] [Google Scholar]
- 38.Moseley GL. Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain. 2005;114(1–2):54–61. doi: 10.1016/j.pain.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 39.Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain. 2004;108(1–2):192–198. doi: 10.1016/j.pain.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 40.McCabe CS, Haigh RC, Ring EF, Halligan PW, Wall PD, Blake DR. A controlled pilot study of the utility of mirror visual feedback in the treatment of complex regional pain syndrome (type 1) Rheumatology (Oxford) 2003;42(1):97–101. doi: 10.1093/rheumatology/keg041. [DOI] [PubMed] [Google Scholar]
- 41.Flor H, Denke C, Schaefer M, Grusser S. Effect of sensory discrimination training on cortical reorganisation and phantom limb pain. Lancet. 2001;357(9270):1763–1764. doi: 10.1016/S0140-6736(00)04890-X. [DOI] [PubMed] [Google Scholar]
- 42.Fregni F, Gimenes R, Valle AC, Ferreira MJ, Rocha RR, Natalle L, Bravo R, Rigonatti SP, Freedman SD, Nitsche MA, Pascual-Leone A, Boggio PS. A randomized, sham-controlled, proof of principle study of transcranial direct current stimulation for the treatment of pain in fibromyalgia. Arthritis Rheum. 2006;54(12):3988–3998. doi: 10.1002/art.22195. [DOI] [PubMed] [Google Scholar]
- 43.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G, Pain CBWGoGfCLB (2006) Chapter 4 European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 15 Suppl 2:S192–S300 [DOI] [PMC free article] [PubMed]
- 44.Verhagen AP, Vet HC, Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–1241. doi: 10.1016/S0895-4356(98)00131-0. [DOI] [PubMed] [Google Scholar]
- 45.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 47.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kahn SR, Shrier I, Kearon C. Physical activity in patients with deep venous thrombosis: a systematic review. Thromb Res. 2008;122(6):763–773. doi: 10.1016/j.thromres.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 49.Elnaggar IM, Nordin M, Sheikhzadeh A, Parnianpour M, Kahanovitz N (1991) Effects of spinal flexion and extension exercises on low-back pain and spinal mobility in chronic mechanical low-back pain patients. Spine (8):967–972 [DOI] [PubMed]
- 50.Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Hodges PW, Jennings MD, Maher CG, Refshauge KM (2007) Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain (1–2):31–37 [DOI] [PubMed]
- 51.Taimela S, Harkapaa K. Strength, mobility, their changes, and pain reduction in active functional restoration for chronic low back disorders. J Spinal Disord. 1996;9(4):306–312. doi: 10.1097/00002517-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 52.Reilly K, Lovejoy B, Willams R, Roth H (1989) Differences between a supervised and independent strength and conditioning program with chronic low back syndromes. J Occup Med (6):547–550 [DOI] [PubMed]
- 53.Johannsen F, Remvig L, Kryger P, Beck P, Warming S, Lybeck K, Dreyer V, Larsen LH (1995) Exercises for chronic low back pain: a clinical trial. J Orthop Sports Phys Ther (2):52–59 [DOI] [PubMed]
- 54.Kofotolis N, Kellis E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility, and functional performance in women with chronic low back pain. Phys Ther. 2006;86(7):1001–1012. [PubMed] [Google Scholar]
- 55.Khalil TM, Asfour SS, Martinez LM, Waly SM, Rosomoff RS, Rosomoff HL (1992) Stretching in the rehabilitation of low-back pain patients. Spine (3):311–317 [DOI] [PubMed]
- 56.Ben Salah Frih Z, Fendri Y, Jellad A, Boudoukhane S, Rejeb N. Efficacy and treatment compliance of a home-based rehabilitation programme for chronic low back pain: a randomized, controlled study. Ann Phys Rehabil Med. 2009;52(6):485–496. doi: 10.1016/j.rehab.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 57.Demoulin C, Maquet D, Tomasella M, Croisier J, Crielaard J, Vanderthommen M. Benefits of a physical training program after back to school for chronic low back pain patients. J Musculoskelet Pain. 2006;14(2):21–31. doi: 10.1300/J094v14n02_04. [DOI] [Google Scholar]
- 58.Mannion AF, Müntener M, Taimela S, Dvorak J (1999) A randomized clinical trial of three active therapies for chronic low back pain. Spine (23):2435–2448 [DOI] [PubMed]
- 59.Handa N, Yamamoto H, Tani T, Kawakami T, Takemasa R. The effect of trunk muscle exercises in patients over 40 years of age with chronic low back pain. J Orthop Sci. 2000;5(3):210–216. doi: 10.1007/s007760050153. [DOI] [PubMed] [Google Scholar]
- 60.Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise. Spine. 2002;27(17):1829–1834. doi: 10.1097/00007632-200209010-00003. [DOI] [PubMed] [Google Scholar]
- 61.Mannion AF, Dvorak J, Taimela S, Müntener M (2001) [Increase in strength after active therapy in chronic low back pain (CLBP) patients: muscular adaptations and clinical relevance]. Schmerz (Berlin, Germany) (6):468–473 [DOI] [PubMed]
- 62.Kankaanpää M, Taimela S, Airaksinen O, Hänninen O (1999) The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self-experienced disability, and lumbar fatigability. Spine (10):1034–1042 [DOI] [PubMed]
- 63.Roche G, Ponthieux A, Parot-Shinkel E, Jousset N, Bontoux L, Dubus V, Penneau-Fontbonne D, Roquelaure Y, Legrand E, Colin D, Richard I, Fanello S (2007) Comparison of a functional restoration program with active individual physical therapy for patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil (10):1229–1235 [DOI] [PubMed]
- 64.Mellin G, Harkapaa K, Vanharanta H, Hupli M, Heinonen R, Jarvikoski A. Outcome of a multimodal treatment including intensive physical training of patients with chronic low back pain. Spine. 1993;18(7):825–829. doi: 10.1097/00007632-199306000-00003. [DOI] [PubMed] [Google Scholar]
- 65.Keller A, Brox JI, Gunderson R, Holm I, Friis A, Reikerås O (2004) Trunk muscle strength, cross-sectional area, and density in patients with chronic low back pain randomized to lumbar fusion or cognitive intervention and exercises. Spine (1):3–8 [DOI] [PubMed]
- 66.Mellin G. Physical therapy for chronic low back pain: correlations between spinal mobility and treatment outcome. Scand J Rehabil Med. 1985;17(4):163–166. [PubMed] [Google Scholar]
- 67.Yeung CKN, Leung MCP, Chow DHK. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. J Altern Complement Med. 2003;9(4):479–490. doi: 10.1089/107555303322284767. [DOI] [PubMed] [Google Scholar]
- 68.Hollmann W, Struder HK. Exercise, physical activity, nutrition, and the brain. Nutr Rev. 1996;54(4 Pt 2):S37–S43. doi: 10.1111/j.1753-4887.1996.tb03897.x. [DOI] [PubMed] [Google Scholar]
- 69.Renkawitz T, Boluki D, Grifka J. The association of low back pain, neuromuscular imbalance, and trunk extension strength in athletes. Spine J. 2006;6(6):673–683. doi: 10.1016/j.spinee.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 70.Lewis A, Morris M, Walsh C (2008) Are physiotherapy exercises effective in reducing chronic low back pain? Phys Ther Rev 13(1)
- 71.Verbunt JA, Smeets RJ, Wittink HM. Cause or effect? Deconditioning and chronic low back pain. Pain. 2010;149(3):428–430. doi: 10.1016/j.pain.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 72.Verbunt JA, Seelen HA, Vlaeyen JW, Heijden GJ, Heuts PH, Pons K, Knottnerus JA. Disuse and deconditioning in chronic low back pain: concepts and hypotheses on contributing mechanisms. Eur J Pain. 2003;7(1):9–21. doi: 10.1016/S1090-3801(02)00071-X. [DOI] [PubMed] [Google Scholar]
- 73.Kell RT, Asmundson GJG. A comparison of two forms of periodized exercise rehabilitation programs in the management of chronic nonspecific low-back pain. J Strength Cond Res. 2009;23(2):513–523. doi: 10.1519/JSC.0b013e3181918a6e. [DOI] [PubMed] [Google Scholar]
- 74.Manniche C, Ostergaard K, Jordan A. Training of back and neck in the year of 2002. Ugeskr Laeger. 2002;164(14):1910–1913. [PubMed] [Google Scholar]
- 75.Southwick SM, White AA. The use of psychological tests in the evaluation of low-back pain. J Bone Jt Surg Am. 1983;65(4):560–565. [PubMed] [Google Scholar]
- 76.Sertpoyraz F, Eyigor S, Karapolat H, Capaci K, Kirazli Y (2009) Comparison of isokinetic exercise versus standard exercise training in patients with chronic low back pain: a randomized controlled study. Clinical Rehabilitation (3):238–247 [DOI] [PubMed]
- 77.Biering-Sorensen F, Bendix AF. Working off low back pain. Lancet. 2000;355(9219):1929–1930. doi: 10.1016/S0140-6736(00)02321-7. [DOI] [PubMed] [Google Scholar]
- 78.Loeser JD, Melzack R. Pain: an overview. Lancet. 1999;353(9164):1607–1609. doi: 10.1016/S0140-6736(99)01311-2. [DOI] [PubMed] [Google Scholar]
- 79.Mannion AF, Junge A, Taimela S, Muntener M, Lorenzo K, Dvorak J (2001) Active therapy for chronic low back pain: part 3. Factors influencing self-rated disability and its change following therapy. Spine (8):920–929 [DOI] [PubMed]
- 80.Lindstrom I, Ohlund C, Eek C, Wallin L, Peterson LE, Fordyce WE, Nachemson AL. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant-conditioning behavioral approach. Phys Ther. 1992;72(4):279–290. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 81.Mayer TG, Gatchel RJ, Mayer H, Kishino ND, Keeley J, Mooney V. A prospective two-year study of functional restoration in industrial low back injury. An objective assessment procedure. JAMA. 1987;258(13):1763–1767. doi: 10.1001/jama.1987.03400130077037. [DOI] [PubMed] [Google Scholar]
- 82.Alaranta H, Rytokoski U, Rissanen A, Talo S, Ronnemaa T, Puukka P, Karppi SL, Videman T, Kallio V, Slatis P. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled clinical trial. Spine (Phila Pa 1976) 1994;19(12):1339–1349. doi: 10.1097/00007632-199406000-00007. [DOI] [PubMed] [Google Scholar]
- 83.Hazard RG, Fenwick JW, Kalisch SM, Redmond J, Reeves V, Reid S, Frymoyer JW. Functional restoration with behavioural support. A one-year prospective study of patients with chronic low-back pain. Spine (Phila Pa 1976) 1989;14(2):157–161. doi: 10.1097/00007632-198902000-00003. [DOI] [PubMed] [Google Scholar]
- 84.Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49(2):221–230. doi: 10.1016/0304-3959(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 85.Fordyce WE, Brena SF, Holcomb RJ, Lateur BJ, Loeser JD. Relationship of patient semantic pain descriptions to physician diagnostic judgments, activity level measures and MMPI. Pain. 1978;5(3):293–303. doi: 10.1016/0304-3959(78)90016-7. [DOI] [PubMed] [Google Scholar]
- 86.Rosomoff HL, Rosomoff RS. Comprehensive multidisciplinary pain center approach to the treatment of low back pain. Neurosurg Clin N Am. 1991;2(4):877–890. [PubMed] [Google Scholar]
- 87.Jensen MP, Turner JA, Romano JM, Karoly P. Coping with chronic pain: a critical review of the literature. Pain. 1991;47(3):249–283. doi: 10.1016/0304-3959(91)90216-K. [DOI] [PubMed] [Google Scholar]
- 88.Turk DC, Rudy TE. Toward an empirically derived taxonomy of chronic pain patients: integration of psychological assessment data. J Consult Clin Psychol. 1988;56(2):233–238. doi: 10.1037/0022-006X.56.2.233. [DOI] [PubMed] [Google Scholar]
- 89.Ryan CG, Gray HG, Newton M, Granat MH. Pain biology education and exercise classes compared to pain biology education alone for individuals with chronic low back pain: a pilot randomised controlled trial. Man Ther. 2010;15(4):382–387. doi: 10.1016/j.math.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 90.Schofferman J. Restoration of function: the missing link in pain medicine? Pain Med. 2006;7(Suppl 1):S159–S165. doi: 10.1111/j.1526-4637.2006.00131.x. [DOI] [Google Scholar]
- 91.Karimi N, Ebrahimi I, Ezzati K, Kahrizi S, Torkaman G, Arab AM. The effects of consecutive supervised stability training on postural balance in patients with chronic low back pain. Pakistan J Med Sci. 2009;25(2):177–181. [Google Scholar]