Abstract
Problem
Thoracic disc disease with radicular pain and myelopathic symptoms can have serious neurological sequelae. The authors present a relevant treatment option.
Methods
Data of patients with single level symptomatic thoracic disc herniation treated with thoracoscopic microdiscectomy were prospectively collected over a period of 10 years. Data collection included the preoperative status and the follow-up status was 6, 12 and 24 months after surgery for every patient.
Results
A total of 167 single level thorascoscopic discectomies without previous surgery on the level of the procedure were included in this study. The average preoperative duration of pain symptoms was 14.3 months, myelopathic symptoms were present for an average of 16.7 months before surgery. After the procedure pain scores measured with visual analog scale (VAS) decreased by 4.4 points and the muscle strength improved by a mean of 4.6 points (American Spinal Injury Association ASIA motor score). After 2 years, 79% of the patients reported a excellent or good outcome for pain and 80% of the patients reported a excellent or good outcome for motor function. The overall complication rate was 15.6%.
Conclusions
Thoracoscopic microdiscectomy for single level symptomatic disc herniation is a highly effective and reliable technique, it can be performed safely with low complication rate.
Keywords: Thoracic disc herniation, Thoracoscopic spine surgery, Thoracoscopy, Thoracic spine, Microsurgical endoscopy
Introduction
Over the past decades the treatment of thoracic disc herniation has changed profoundly. Since the introduction of thoracoscopy for the treatment of thoracic spine diseases in the early 1990’s thoracoscopic microdiscectomy has been evaluated in multiple studies [2, 9, 10, 13, 15, 17, 19, 21]. Despite the advantages documented for this technique [5, 17, 19], thoracoscopic microdiscectomy is still considered controversial, a steep learning curve and the possibility for life threatening complications are considered to be the major concerns [16–18].
The majority of the reports describing thoracoscopic discectomy are either retrospective, include patients with inhomogeneous pathologies or to small for statistically significant conclusions.
In order to address these short comings, we designed a prospective followed cohort study of patients with symptomatic single level thoracic disc herniation undergoing thoracoscopic microdiscectomy.
The goal of this study was to evaluate the effectivity of thoracoscopic discectomy without fusion, the clinical outcome and the complications in symptomatic patients with radicular or medullar compression.
Patients and methods
Between January 1995 to December 2004, 255 patients underwent 310 thoracoscopic excisions of herniated thoracic discs. 178 patients met the inclusion criteria for the study and 11 patients were lost to follow-up. The remaining 167 patients are the ones subject for analysis in this report. The average age was 46.8 years (range 20–81 years), 64 were males and 103 females. The mean follow-up was 24 months (range).
Study design
The inclusion and exclusion criteria for our study are listed in Table 1. In order to observe a homogeneous group of patients only symptomatic (due to radicular or medullary compression) single level thoracoscopic discectomies without fusion and without previous surgery on the same level were included. All the cases operated had neurological symptoms, multiple level patients were excluded. Data were collected preoperative and at the outpatient clinic at 6, 12 and 24 months after surgery. A postoperative CT scan was performed in all the cases. The surgical technique remained unchanged during the whole duration of the study.
Table 1.
Inclusion and exclusion criteria of the study
| Inclusion criteria | Exclusion criteria |
|---|---|
| Symptomatic thoracic disc herniation between Th2 and L1 due to medular or radicular compression | Previous surgery on the same spinal level |
| Multilevel surgery | |
| Thoracic instability without neural compression | |
| Fusion associated to the discectomy | |
| Spinal fracture | |
| Scoliotic deformity | |
| Tumor | |
| Infection |
Outcome evaluation
All the patients were examined by independent observer. The degree of pain was rated according to the visual analog score (VAS) (pain free = 0 up to agonizing pain = 10). Patients were also asked to classify their pain type as either localized dorsalgia, radicular pain (with uni or bilateral irradiation) or a combination of both.
Sensory disturbances were classified using a 0–3 point scale for each limb, outcome was graded according to the parameters listed in Table 2.
Table 2.
Sensory score
| Sensibility | Score points (for each limb) |
|---|---|
| Normal | 3 normal |
| Reduced sensibility for vibration | 2 moderate |
| Reduced sensibility for all qualities | 1 severe |
| Anesthesia | 0 complete lost |
The outcome for sensory disturbances was defined as excellent with 6 points, good with improvement of at least 2 points, regular with improvement of 1 point and poor with no improvement or postoperative worsening of the score value
Motor evaluation was documented using the 0–5 points scale of the American Spinal Injury Association (ASIA) score, measuring muscle strength in 5 different muscle groups of the lower limb (thus each side had a maximum of 25 points available). Outcome was considered excellent when normal muscle strength was achieved, good if there was a improvement of at least 3 points, regular for improvement of 1–2 points and poor for no improvement or postoperatively worsening (Table 3).
Table 3.
Motor evaluation
| Grade | Symptoms |
|---|---|
| Excellent | 50 points |
| Good | Improvement of at least 3 points |
| Regular | Improvement of 1–2 points |
| Poor | No improvement or worsening of symptoms |
Postoperative CT scans were analyzed by an independent observer to determine the degree of decompression achieved. Findings were classified as: complete decompression, disc remnant without compression and disc remnant resulting in compression on the spinal cord and/or spinal root. Patient satisfaction was evaluated with a self explaining questionnaire 12 and 24 months after surgery.
Statistical evaluation
The paired Students test was used to evaluate preoperative and postoperative data. A p value of ≤0.05 between the preoperative and postoperative evaluation after 6, 12 and 24 month was considered statistically significant.
Surgical indication and preoperative planning
Surgical indications were either myelopathic symptoms (with or without pain) or radicular pain resistant to treatment; medullar or radicular compression linked to symptoms was present in all the cases. Diagnostics included motor evoked potentials (MEP) and somato sensory evoked potentials (SSEP) to determine the degree of medullar dysfunction. All the patients had a magnetic resonance imaging (MRI) and a computed tomography after myelography (CT myelography) before surgery.
The surgical technique used in this patient cohort followed the steps described in previous reports [17, 18].
Summary of the operative technique
All surgeries performed used a three to four portal endoscopic techniques under general anesthesia and the patients were intubated with a double-lumen tube to allow the collapse of the lung on the side of surgery. Patients were placed in lateral decubitus and the spine target level was marked with an intrapleural needle placed paravertebral above the rib at the level of surgery under fluoroscopic vision. The surgical approach was from the side of the herniation or from the right side in patients with medial herniation.
In this study a right-sided approach to the spine was performed in 127 patients (76%), in 40 patients (24%) the approach was performed from the left side.
The first portal was usually placed at the intersection of the anterior auxiliary line and the intrapleural needle placed at the target level. A thoracoscopic exploration of the lung cavity was performed using a 30° angled endoscope. After the feasibility of the procedure was confirmed, two additional trocars were placed and the camera switched to a trocar permitting a perpendicular view of the target level while the first placed trocar served as the main working channel allowing a perpendicular access to the intervertebral space. The second working trocar served as a drainage devise. In case of incomplete pleural collapse or impaired visualization of the target level by the diaphragm a forth trocar was placed to allow separation of the lung or diaphragm. A resection of the head of the rib to allow access to the foramen was performed when the surgical level was above Th 10/11. The two lowest thoracic level Th 11/12 and Th 12/L 1 can be approached without resection of the head of the rib since the head inserts the vertebral body below the foramen at these levels.
Additionally a resection of the superior portion of the pedicle and the dorsolateral edge of the adjacent vertebral bodies was performed with the oscillating saw. The herniated portion of the disc is identified and removed through the osseous defect.
Medullar decompression is confirmed by observing the exposed Dura and using a Penfield probe for palpation. After confirmation of an adequate decompression the intervertebral defect was covered with microfibrillar collagen and the previously resected rib and bone fragments. A chest tube was inserted before lung expansion and the wounds were closed. After closure of the skin the chest tube drainage was assessed and in case of minor air trapping the chest tube removed otherwise it was left in place and removed on the first postoperative day. An intercostal block was performed to reduce postoperative pain and patients were mobilized on the first day after surgery.
Results
From the 167 patients that were included in this analysis, 19 (11%) reported a sudden or trauma related onset of symptoms and 148 patients (89%) described an insidious beginning of the illness. The distribution of the operated disc levels is shown in Table 4. The average hospitalization time was 4.06 days (range 2–18 days).
Table 4.
Distribution of operated spinal levels and number of affected segments
| Disc level | Number |
|---|---|
| T2/T3 | 5 |
| T3/T4 | 7 |
| T4/T5 | 2 |
| T5/T6 | 8 |
| T6/T7 | 29 |
| T7/T8 | 40 |
| T8/T9 | 19 |
| T9/T10 | 22 |
| T10/T11 | 14 |
| T11/T12 | 16 |
| T12/L1 | 5 |
| Total | 167 |
The histological results revealed that 70 patients (42%) had a calcified and 97 patients (58%) a soft disc herniation. Three of the calcified disc herniations had intradural extension of the lesion (1.8%), 127 patients were operated from the right and 40 from the left side.
The average hospitalization time was 4.06 days (range 2–18 days).
Outcome related to pain control
Average duration of symptoms was 14.3 months, 80 patients (52.3%) complained about radicular pain, 57 patients (37.3%) reported a mixed type and 16 patients had local thoracic pain (10.4%). At 2-year follow-up, the clinical examination regarding pain showed 48 patients (31%) graded as excellent, 73 (48%) as good, 26 patients (17%) regular and 6 patients (4%) showed a poor result. The evolution of the three different pain types is resumed in Table 5.
Table 5.
Outcome related to the type of pain, follow-up at 1 or 2 years and number of patients
| Excellent | Good | Regular | Poor | |
|---|---|---|---|---|
| Radicular | 38 | 35 | 7 | |
| Mixed | 8 | 26 | 19 | 4 |
| Local | 4 | 8 | 1 | 3 |
| At 1 year | 50 (33%) | 69 (44%) | 27 (18%) | 7 (5%) |
| At 2 years | 48 (31%) | 73 (48%) | 26 (17%) | 6 (4%) |
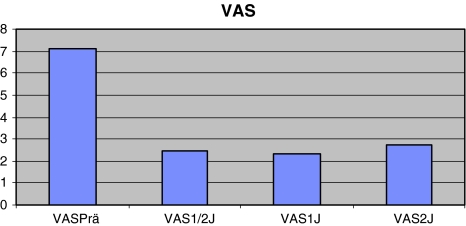
Pain together with motor and/or sensory disturbances was reported preoperatively by 153 patients. The mean preoperative VAS score was 7.14, improving to 2.45 points at 6 months, 2.33 at 1 year, increasing to 2.70 at the 2 years control (Fig. 1).
Fig. 1.
Evolution of pain symptoms measured by the visual analog score
The statistical analysis of the results obtained, showed a significant improvement of pain at 6 months (p ≤ 0.05) when compared to the preoperative status. This remained unchanged until the 24 months follow-up assessment. There was no significant difference among the 12- and 24-month results (p ≤ 0.05).
Outcome related to sensory disturbances
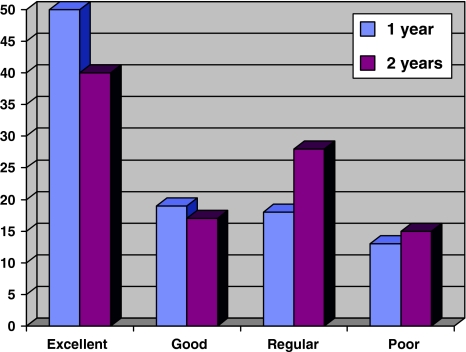
Some degree of sensory disturbance reported 99 patients (59%). The average duration of symptoms was 17.3 months. The mean average preoperative value was 3.3 points, improving up to 5.04 points at 6 months, 5.2 at 1 year and 4.9 after 2 years.
Statistical analysis (paired Students test) showed a significant improvement after 6 months (p ≤ 0.05). There was no significant difference among the postoperative assessment groups (p ≤ 0.05) when compared to the preoperative status. The final grading according to the outcome classification for the first and second postoperative year is depicted on Fig. 2.
Fig. 2.
Patients sensory outcome after 1 and 2 years
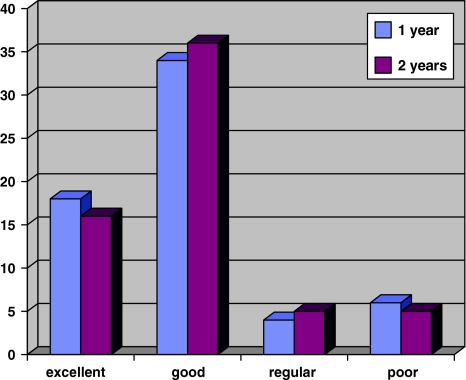
Outcome related to motor function
Myelopathic symptoms with motor weakness were present in 62 patients (37%). The average duration of symptoms was 16.75 months (1–120 months) with a mean motor score of 42.4 points improving to 45.5 at 6 months, 47.1 at 1 year and 47 points after 2 years.
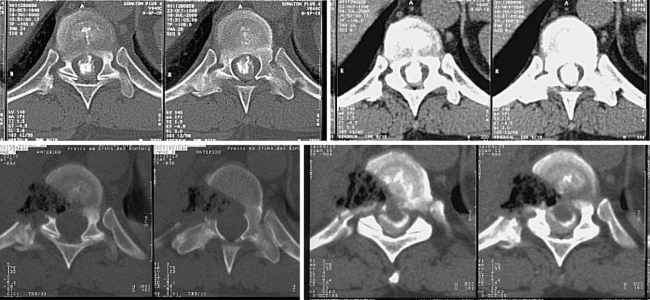
Two patients worsened postoperatively. Both had big calcified disc herniations filling 80 and 90% of the spinal canal cross sectional area. The motor score dropped from 50 to 42 and 45 to 40 points, respectively. In Fig. 4, Image 1 shows the preoperative and Image 2 the postoperative axial CT scan of one of these cases.
Fig. 4.
Case example: 49-year-old female patient presented with calcified disc herniation without motor deficit and after complete resection of the herniation motor score dropped from 50 to 42 points. Image 1 shows preoperative CT scan with a calcified disc herniation of 90% canal occupation. Image 2 shows postoperative CT scan with and without contrast
Although clinically significant, there was no significant improvement of the motor function after 6-month follow-up (p = 0.06) (see Fig. 3).
Fig. 3.
Motor outcome at 1 and 2 years. 18 patients (29%) were graded as excellent, 34 patients (55%) as good, 4 patients (6.5%) had a regular and 6 patients (9.5%) as poor outcome. Two years postoperatively 16 patients (31%) were reported as excellent, 36 (49%) as good, 5 (10%) as regular and 5 as poor outcome (10%)
Outcomes related to patients degree of satisfaction
When asked if they were satisfied with treatment received, 130 patients (78%) answered positively, 21 (12.5%) felt uncertain and 16 patients (9.5%) were unsatisfied with the outcome.
Outcomes based on radiological follow-up postoperative CT control
Postoperative CT scan was reviewed and classified by a independent neuroradiologist. According to CT imaging, a complete resection and decompression was achieved in 144 cases (86%), 20 patients (12%) had minimal disc remnants without compressive effect either on the spinal cord or the nerve root. In 3 patients (1.8%) a disc remnant compressing the spinal cord was still present, all of them were reoperated achieving complete decompression (see Fig. 4).
Complications
The overall complication rate in this study was 15.6%. Two patients had more than one complication: the first had transitory intercostal neuralgia and pleuritis, the second patient had a pneumothorax and later developed clinical signs of segmental instability (Table 6).
Table 6.
Complications, percentage from 167 patients and number of reoperated cases
| Complication type | No. of patients | Percentage | Reoperated cases |
|---|---|---|---|
| ICN persisting up to 6 weeks | 9 | 5.4 | 0 |
| Pulmonary | 6 | 3.6 | 1 |
| Incomplete decompression | 3 | 1.8 | 3 |
| Instability | 3 | 1.8 | 3 |
| Motor deficit | 2 | 1.2 | 0 |
| Sensory deficit | 1 | 0.6 | 0 |
| Dural tear | 1 | 0.6 | 1 |
| Dural leakage after intradural herniation | 1 | 0.6 | 1 |
| Total number of patients | 24 | 15.6 | 9 |
The most common complication seen in this series was the postoperative onset of transitory intercostal neuralgia lasting up to 6 weeks in 9 patients (5.4%). Symptoms resolved after combined treatment with intercostal blocs, oral gabapentin and cortisone in all the cases.
Only 6 patients (3.6%) developed respiratory complications. The first case had a pleuritis that resolved with antibiotic and antiinflammatory drugs. A second case developed atelectasis resolving with physiotherapy. Two patients developed pneumothorax and were successfully treated with pleural drain for 3 days. The last two patients developed pleural effusions needing pleural drainage in one case, the second case had a multiseptated pleuritis requiring a revision thoracoscopy and drainage for 4 days.
Dural leaks and tears were registered in two patients (1.2%). One was caused by a partially intradural big calcified disc herniation with a 4 mm dural defect. The second case was a young female who 3 months after surgery started to complain about intermittent head aches. The control MRI revealed a paravertebral fluid collection, intraoperatively a small epithelialised cyst filled with cerebrospinal fluid (CSF) was drained and sealed. The leak was certainly caused during the surgery but so small that it could have been identified intraoperatively. Both patients were successfully reoperated (case 2, 24 months after the first operation). Severe pain due to segmental instability developed in 3 patients (1.8%). There were no lethal outcomes in this study.
Discussion
The combination of medullar compression at the narrowest section of the spinal canal in addition to the complex vascular anatomy of the spinal cord may explain why the thoracic level is one of the most sensible areas of the spinal cord. Despite the lack of scientific evidence it is our believe that unknown compensatory mechanisms must play an important role in preserving and protecting the spinal cord against external aggressors, since in most of our patients the mean time elapsed between appearance of the first symptoms and surgical treatment was 18 months.
A multifactorial etiology may explain why until now and since the report of Arseni and Nash [4] thoracic disc herniation is (wrongly) considered a “low incidence” disease. In 1971 Carson [8] presented a report of 18 cases with thoracic disc herniation. Based on the barely available literature at that time and due to the lack of sensitive diagnostic procedures the incidence of symptomatic thoracic disc disease was estimated to be one case in a million [3, 8]. Despite the fact that better and highly sensitive diagnostic instruments and minimally invasive treatment options have been developed since Carson’s first report, thoracic disc herniation is still considered a “low incidence” disease.
Based upon review of the current literature and the fund of knowledge acquired during the last 40 years, it appears that the dorsal area is the largest section of the spine, and because of that it should have a higher incidence of disc disease as previously reported. The majority of the series published after the introduction of CT or MRI report an incidence of thoracic disc herniation between 11 and 37% [3, 10, 23]. An autopsy study published by Abbott et al. [1] in the 1950’s reported an incidence of thoracic disc herniation between 7 and 15%. Modern literature, that relays on state of the art diagnostics, reports an incidence of this disease much higher as commonly assumed. In fact all papers published after the introduction of CT or MRI report an incidence between 11 and 37% for symptomatic or asymptomatic disc herniation [22]. Whereas prevalence measures how much disease is present in a population at a particular point in time, incidence is calculated as the number of new cases of a disease in a specified time period divided by the size of the population under consideration who are initially disease free.
The most common preoperative symptoms reported in this series was pain, affecting 153 of the patients (92%), reduced sensibility in 99 patients (59%) and motor deficit in 62 patients (37%).When analyzing the results of pain control in this patient population, the radicular pain group showed the best results with over 90% of the patients reporting an excellent or good outcome. The complication registered in this group were two cases of transitory intercostal neuralgia (ICN) and one patient developing severe axial pain, needing a spondylodesis 6 months later.
Anand [2] reported a negative average of improvement in a small group of five patients with radicular pain. These contrasts with results reported by Oskunian [1] in 75% in the Oswestry disability index (ODI) scale. Our previous publication [18] reported similar results in a smaller group of 19 patients (included in this study). Similar to what occurs at the cervical and lumbar spine, once the nerve root is decompressed, pain reduction is quick and almost complete. Thus, it is not surprising that 73 patients (91%) rated the procedure as satisfactory since almost the majority felt immediate pain relief, had low postoperative discomfort and short hospitalization time fulfilling almost all their expectations.
Mixed pain was the second biggest group in this study with 57 (37%) patients reporting severe dorsalgia and radicular compromise. These patients had commonly pain localized either at the upper, mid or lower back, depending on the location of the disc hernia at the thoracic spine. Many of these cases were diagnosed when an MRI scout view of the cervical or lumbar spine depicted circumstantially the cervicothoracic or thoracolumbar area. In our experience disc hernias located in the upper thoracic spine (T5 upwards) spread out at the cervical area, in contrast those placed in the lower thoracic spine (T10 downwards) irradiate to the lumbar area (mimicking lumbalgia) and ventrally to the lower abdominal or inguinal region [6]. In this patient population, 12 patients (21%) were diagnosed by means of a routine CT scan and not because of their clinical symptoms. Although this cohort included the majority of patients with long-lasting therapy resistant pain for the longest period of time and 61% of the calcified discs herniations, nevertheless 34 patients (60%) had a excellent or good outcome. The group with poor outcome included two cases that were unchanged and two that worsened after surgery, these two cases underwent thoracoscopic fusion months later, one of them improving and the second reported only a slight improvement so that he was rated as unchanged. At 2 years there was a slight improvement in the group with good outcome, the remaining categories stayed almost unchanged, suggesting that results after 1 year may be conclusive.
Fusion after thoracic discectomy remains matter of controversial. Despite the fact that these patients had axial and radicular pain, only three of them needed fusion months later. Few studies in the literature address this issue. Anand [2] reported 40 fusions in a group of 100 thoracoscopically treated cases. In his study he described no difference in outcome between fused and non-fused cases at 2-year follow-up. Broc [7] published in 1997 the first study analyzing segmental stability after single level discectomy. He concluded that although there were minimal changes in the instantaneous axis of rotation, it did not affect stability significantly. In the present study only 3 patients (2%) needed a spondylodesis because of axial pain symptoms, months after the decompressive surgery was done. As far as bone and disc resection was kept between given limits no additional fusion was required. The last and smallest group was the one complaining about isolated local back pain (dorsalgia). In this group 12 (75%) of the 16 patients included had an excellent or good result, achieving levels almost as good as the group with radicular pain. Why the decompression of the spinal cord leads to improvement in back pain is still a matter that needs to be studied in detail.
Another important endpoint in the analysis and discussion of our results is the sensory disturbances that developed earlier than motor disfunctions. The mean onset of symptoms in this group of 99 patients was 17.3 months previous to the diagnosis and treatment of the illness. The data obtained quantifying the compromise and further recovery of the sensory qualities show clearly a significant high percentage of sustainable success after 2 years (Fig. 2).
Since medullar compression is mainly anterior, pressure is probably affecting the posterior bundles by altering its vascular supply. Decompression probably reverts this process what may explain why patients with marked hypoesthesia recovered almost completely at the 2-year follow-up examination. Although motor deficit was present in only 37% of the patients, symptoms lasted for almost 1.5 years until surgical treatment was performed. Even with that long-lasting symptomatology, 80% of the patients were graded excellent or good after 2 years (Fig. 3). This result suggests that even compression over a longer period can be reverted by decompression in the vast majority of the cases. Similar to the sensory deficit results at 1 year seem to be definitive, after that time the capacity of recovery seems to reach its limit. Nevertheless, recovery of more than 5 score points is a more than encouraging fact when the decision for or against surgical treatment has to be taken.
The majority of our 130 patients (78%) that were satisfied with the procedure belonged to the groups with good and excellent overall results. The unsatisfied patients had 1 or more complications (9 patients) and 7 had a regular or poor outcome. Anand [2] reported 83.8% of satisfied patients after 2 years follow, slightly higher to the 78% achieved in this study. These data confirm that thoracoscopic microdiscectomy has a high degree of acceptance among the treated patients. Although quick recovery and low pain levels are important for patients, the fact that the operation can be done without “wide opening of the chest” and still achieve results comparable to “big surgery” seems to be the most convincing argument.
A particularly important advantage of CT over MRI from a surgical perspective is its superior ability to distinguish soft-tissue neural compression from bony compression. This is especially true for subtle lateral pathology where, on the basis of MRI, it may be difficult to distinguish nerve root compression due to a soft lateral disc extrusion from that due to a prominent bone spur [24].
Some authors sought to determine the association between radiologic and clinical diagnoses and to measure the impact of more magnetic resonance imaging (MRI) and computed tomography (CT) scans on clinical decision-making in patients referred to a surgical clinic for back pain. In their conclusion, the clinical diagnosis had a poor association with radiologic abnormalities. Despite an increase in the number of MRI and CT scans, the number of patients deemed surgical candidates has not changed [25].
Postoperative CT showed complete or nearly complete decompression in 98% of the patients, demonstrating the high effectivity that thoracoscopy achieves. Remnants compressing the spinal cord were found in three cases, patients were reintervened thoracoscopically to complete the decompression. All patients involved calcified discs (middle or big sized), the remnants were located cranially (2 cases) or caudally (1 case) from the disc space. Insufficient exposure (bone resection) rather than lack of visualization was the reason why these disc pieces were overseen. Contrary to Gille and Dickmanns reports [11, 21] we do not consider thoracotomy or partial disc removal as a alternative for thoracoscopic decompression. With adequate instruments and appropriate technique for dural repair and postoperative management full decompression can be achieved without exposing the patients to any additional risks.
The overall complication rate of 15.6% in this series compares favorably to others published by means of an open approach via thoracotomy. There was no lethal outcome and none of the complications was severe or life threatening. This result contrasts with our previous published data including our early results [19, 20] with an overall complication rate of 23%. The former included redo surgeries, multilevel and instrumented cases, requiring a higher level of surgical skills and experience but also bearing the risk of a higher complication rate, these data are similar to those published by Oskunian [14] 24% and Anand [2] 21%, both with a similar inhomogeneous patient population.
As in other reports transitory intercostal neuralgia (ICN) was the leading complication (5.4%) resolving in all the cases at maximum 6 weeks. Anand [2] reported 6% of transitory neuralgia while Oskunian’s incidence [14] reached 13% declining steeply after changing stiff for flexible trocars. Leverage between the narrow rib spaces and stiff trocars, as used in abdominal surgery, irritates the intercostal nerve leading to neuralgic pain.
The use of soft trocars from the beginning of the study, immediate postoperative infiltration of the wounds with local anesthetics and cortisone as well as early treatment with gabapentin may explain the low incidence of ICN in this group.
Pulmonary complications resolved all except one with physiotherapy and/or drainage. A patient with multiseptated pleural effusion needed thoracoscopic revision. In the last 5 years of the study due to intense postoperative physiotherapy immediately after the first postoperative day, only two cases of respiratory complications (pneumothorax, pleuritis) occurred. Contrasting with data published for thoracotomy, reporting an incidence of respiratory complications up to 33% [20, 21], thoracoscopy seems to reduce significantly the risk of postoperative pulmonary affections.
Symptomatic postoperative instability was observed in 3 patients (1.8%). The leading symptom was therapeutic resistant axial pain. All three cases had a thoracoscopic spondylodesis using a modification of the technique described years ago [16, 17]. Thoracic stability is determined by the interaction of the vertebrae, discs, the ribcage and the sternum [12]. Alterations in the integrity of these elements can lead to mechanical instability. Moreover, the resection of disc herniation causing neurological deficit or intractable pain can lead to postoperative column insufficiency. However, the thoracoscopic technique described in previous reports was biomechanically tested by Broc [7]. He concluded that although minimal biomechanical alterations of the operated segment occur, these do not lead to destabilization of the spinal segment. The low incidence reported here supports these results, suggesting that fusion after thoracic discectomy is unnecessary unless extensive bone resection (as in big calcified hernias) or multilevel discectomies are needed. The three instability cases were located at the levels Th 7/8, Th 10/11 and Th 11/12. According to this, fusion might be considered for levels situated near or at the thoraco lumbar region, probably because it is the transition area between the stiff thoracic and the more flexible lumbar spine.
The two cases of motor deficits and worsening occurred in two patients with giant calcified disc herniations. One of those having intradural expansion of the lesion. Both cases had a long-lasting anamnesis with progressive myelopathy. Although surgical steps were uneventful the degree of manipulation of a seriously compromised spinal cord can be the reason for neurological worsening.
The third patient complained about a loss of sensation in the groin 2 years after surgery without further neurological compromise. Similar to the result reported by Oskunian [14] the incidence of worsening was 1.8%. Compared with Stillermann’s and Fessler’s revision of the literature [10, 21], the percentage of worsening in these thoracoscopic series is the lowest reported in recent publications.
From the two cases of dural tear documented, only one needed immediate reoperation because of continuous leaking. Although suturing is a complicated task to be done endoscopically, the defect was closed using fascia and fibrin glue. In addition, a lumbar drain for 72 h helped sealing the leakage after 6 days.
Conclusions
This prospective followed cohort study shows that
For single level disc herniation, thoracoscopic microdiscectomy is a highly effective technique with the lowest incidence of complications reported in the literature.
According to the results thoracoscopic microdiscectomy is the first choice for treating radicular pain.
Calcified disc herniations bare a higher risk of developing complications.
Thoracic disc herniation may have a higher incidence than previously assumed.
The “optimal” surgical approach for this affection remains unclear but the majority of the published articles dealing with it agree that the best results are achieved using an anterior approach [17, 18, 21].
The outcome reported in this study suggests that for single level disease thoracoscopic removal of a herniated disc seems to be as safe and effective as thoracotomy achieving a marked reduction of the type and incidence of complications. While keeping this in mind, the learning curve does not seem to be steeper than for other techniques. Most surgeons acquainted with arthroscopy or neuroendoscopy must have acquired enough visual and motor skills allowing him to learn and apply this technique safely.
You must list what are the strengths and weaknesses of this study. The strength of this study is that it is to our knowledge the largest series of patients reported with a thoracic disc herniation that were treated by means of a thoracoscopic approach. We also acknowledge as weakness that this is a retrospective non-randomized review study and that in order to draw better conclusions a prospective randomized series should be conducted.
Conflict of interest
No funds were received in support of this study.
References
- 1.Abbott KH, Retter RH. Protrusions of thoracic intervertebral disks. Neurology. 1956;1:1–10. doi: 10.1212/wnl.6.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Anand N, Regan JJ. Video-assisted thoracoscopic surgery for thoracic disc disease. Spine. 2002;27(8):871–879. doi: 10.1097/00007632-200204150-00018. [DOI] [PubMed] [Google Scholar]
- 3.Arce CA, Dohrmann GJ. Thoracic disc herniation: Improved diagnosis with computed tomographic scanning and a review of the literature. Surg Neurol. 1985;23:356–361. doi: 10.1016/0090-3019(85)90206-X. [DOI] [PubMed] [Google Scholar]
- 4.Arseni C, Nash F. Thoracic intervertebral disc protrusion: a clinical study. J Neurosurg. 1995;17:418–430. doi: 10.3171/jns.1960.17.3.0418. [DOI] [PubMed] [Google Scholar]
- 5.Ayhan S, Nelson C, et al. Transthoracic surgical treatment for centrally located thoracic disc herniations presenting with myelopathy. A 5-year institutional experience. J Spinal Disord Tech. 2010;23(2):79–88. doi: 10.1097/BSD.0b013e318198cd4d. [DOI] [PubMed] [Google Scholar]
- 6.Balagué F, Fankhauser H. Unusual presentation of thoracic disc herniation. Clin Rheumatol. 1989;8(2):269–273. doi: 10.1007/BF02030085. [DOI] [PubMed] [Google Scholar]
- 7.Broc GG, Crawford NR, Sonntag VK, Dickman CA. Biomechanical effects of transthoracic microdiscectomy. Spine. 1997;22(6):605–612. doi: 10.1097/00007632-199703150-00005. [DOI] [PubMed] [Google Scholar]
- 8.Carson J, Gumpert J, Jefferson A. Diagnosis and treatment of thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1971;34:68–77. doi: 10.1136/jnnp.34.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eichholz KM, O’toole JE, Fessler RG. Thoracic microendoscopic discectomy. Neurosurg Clin N Am. 2006;17(4):441–446. doi: 10.1016/j.nec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Fessler RG, Sturgill M. Review: complications of surgery for thoracic disc disease. Surg Neurol. 1998;49(6):609–618. doi: 10.1016/S0090-3019(97)00434-5. [DOI] [PubMed] [Google Scholar]
- 11.Gille O, Soderlund C, Razafimahandri HJ, Mangione P, Vital JM. Analysis of hard thoracic herniated discs: review of 18 cases operated by thoracoscopy. Eur Spine J. 2006;15(5):537–542. doi: 10.1007/s00586-005-1014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horton WC, Kraiwattanapong C, et al. The role of the sternum, costosternal articulations, intervertebral discand facets in thoracic sagittal plane biomechanics. A comparison of three different sequences of surgical release. Spine. 2005;30(18):2014–2023. doi: 10.1097/01.brs.0000180478.96494.88. [DOI] [PubMed] [Google Scholar]
- 13.Longo UG, Papapietro N, Maffulli N, Denaro V. Thoracoscopy for minimally invasive thoracic spine surgery. Orthop Clin North Am. 2009;40(4):459–464. doi: 10.1016/j.ocl.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. J Neurosurg Spine. 2005;3(6):459–464. doi: 10.3171/spi.2005.3.6.0459. [DOI] [PubMed] [Google Scholar]
- 15.Regan JJ, Ben-Yishay A, Mack MJ. Video assisted thoracoscopic excision of herniated thoracic disc: description of technique and preliminary experience in the first 29 cases. J Spinal Disord. 1998;11:183–191. doi: 10.1097/00002517-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Rosenthal D, Rosenthal R, Simone A. Removal of a protruded thoracic disc using microsurgical endoscopy. A new technique. Spine. 1994;19(9):1087–1091. doi: 10.1097/00007632-199405000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal D, Dickman CA. Thoracoscopic microsurgical excision of herniated thoracic discs. J Neurosurg. 1998;89(2):224–235. doi: 10.3171/jns.1998.89.2.0224. [DOI] [PubMed] [Google Scholar]
- 18.Sheikh H, Samartzis D, Perez-Cruet MJ. Techniques for the operative management of thoracic disc herniation: minimally invasive thoracic microdiscectomy. Orthop Clin North Am. 2007;38:351–361. doi: 10.1016/j.ocl.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Stillerman CB, Chen TC, Couldwell WT, Zhang W, Weiss MH. Experience in the surgical management of 82 symptomatic herniated thoracic discs and review of the literature. J Neurosurg. 1998;88:623–633. doi: 10.3171/jns.1998.88.4.0623. [DOI] [PubMed] [Google Scholar]
- 20.Stillerman CB, Weiss MH. Management of thoracic disc disease. Clin Neurosurg. 1992;38:325–352. [PubMed] [Google Scholar]
- 21.Theodore N, Dickman CA. Current management of thoracic disc herniation. Contemp Neurosurg. 1996;18(19):1–7. [Google Scholar]
- 22.Williams MP, Cherryman GR, Husband JE. Significance of thoracic disc herniation demonstrated by MR imaging. J Comput Tomog. 1989;13:211–214. doi: 10.1097/00004728-198903000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Wood KB, Blair JM, Aepple DM. The natural history of asymptomatic thoracic disc herniations. Spine. 1997;22(5):525–530. doi: 10.1097/00007632-199703010-00011. [DOI] [PubMed] [Google Scholar]
- 24.Garfin SR, Vaccaro AR (1997) Orthopaedic knowledge update. In: North American Spine Society Spine (ed) Imaging studies of the spine, Rosemont, IL (ISBN 0-89203-169-7)
- 25.Li AL, Yen D. Effect of increased MRI and CT scan utilization on clinical decision-making in patients referred to a surgical clinic for back pain. Can J Surg. 2011;54(2):128–132. doi: 10.1503/cjs.001510. [DOI] [PMC free article] [PubMed] [Google Scholar]