Abstract
Axonal injury is believed to be a major determinant of adverse outcomes following traumatic brain injury. However, it has been difficult to assess acutely the severity of axonal injury in human traumatic brain injury patients. We hypothesized that microdialysis-based measurements of the brain extracellular fluid levels of tau and neurofilament light chain, two low molecular weight axonal proteins, could be helpful in this regard. To test this hypothesis, 100 kDa cut-off microdialysis catheters were placed in 16 patients with severe traumatic brain injury at two neurological/neurosurgical intensive care units. Tau levels in the microdialysis samples were highest early and fell over time in all patients. Initial tau levels were >3-fold higher in patients with microdialysis catheters placed in pericontusional regions than in patients in whom catheters were placed in normal-appearing right frontal lobe tissue (P = 0.005). Tau levels and neurofilament light-chain levels were positively correlated (r = 0.6, P = 0.013). Neurofilament light-chain levels were also higher in patients with pericontusional catheters (P = 0.04). Interestingly, initial tau levels were inversely correlated with initial amyloid-β levels measured in the same samples (r = −0.87, P = 0.000023). This could be due to reduced synaptic activity in areas with substantial axonal injury, as amyloid-β release is closely coupled with synaptic activity. Importantly, high initial tau levels correlated with worse clinical outcomes, as assessed using the Glasgow Outcome Scale 6 months after injury (r = −0.6, P = 0.018). Taken together, our data add support for the hypothesis that axonal injury may be related to long-term impairments following traumatic brain injury. Microdialysis-based measurement of tau levels in the brain extracellular space may be a useful way to assess the severity of axonal injury acutely in the intensive care unit. Further studies with larger numbers of patients will be required to assess the reproducibility of these findings and to determine whether this approach provides added value when combined with clinical and radiological information.
Keywords: traumatic brain injury, microdialysis, amyloid-β, tau, neurofilament
Introduction
Axonal injury has been hypothesized to be a primary determinant of adverse outcomes following traumatic brain injury (Smith et al., 2003b). In autopsy studies, this pathology has been found to be highly prevalent in both severe and milder cases (Strich, 1956, 1961; Adams et al., 1982, 1989; Blumbergs et al., 1989, 1994, 1995; Christman et al., 1994; Bennett et al., 1995; Gorrie et al., 2002; Adams et al., 2011). In experimental studies, the extent of axonal injury after rotational acceleration injury in non-human primates was directly proportional to the depth of coma in the absence of other significant pathology (Gennarelli et al., 1982). Similar findings were observed in a pig model (Smith et al., 2000). Advanced MRI indicators of axonal injury have been found to be correlated with a variety of adverse clinical outcomes (Huisman et al., 2004; Wilde et al., 2006; Kraus et al., 2007; Levin et al., 2008; Niogi et al., 2008a, b; Wang et al., 2008; Kumar et al., 2009; Lipton et al., 2009; Lo et al., 2009; Perlbarg et al., 2009; Chang et al., 2010; Kondo et al., 2010; Marquez de la Plata et al., 2010; Warner et al., 2010; Kinnunen et al., 2011). However, there has been comparatively little study of axonal injury in patients with severe traumatic brain injury during the acute phase (Petzold et al., 2011), and new approaches are needed to assess the severity of axonal injury in the living human brain.
Tau is an intracellular, microtubule-associated protein that is highly enriched in axons. Its release into the CSF has been interpreted as indicative of axonal injury (Zemlan et al., 1999; Emmerling et al., 2000; Franz et al., 2003; Ost et al., 2006; Zetterberg et al., 2006). Likewise, neurofilament-light chain (NF-L) is an integral part of the axonal cytoskeleton and NF-L elevation in the CSF may serve as a complementary marker of axonal injury (Norgren et al., 2003; Van Geel et al., 2005; Zetterberg et al., 2006).
While CSF-based studies have provided significant insights, tau and NF-L release into the brain extracellular space as detected by microdialysis could be an even more direct measure of axonal injury. Microdialysis sampling can be used to assess local intracranial processes (Hillered et al., 2005), whereas CSF sampling likely reflects more global events (Fishman, 1992).Importantly, brain extracellular interstitial fluid is not in full equilibrium with the CSF (Fishman, 1992; Brody et al., 2008). Likewise, many patients with severe traumatic brain injury do not have external ventricular drains placed so serial CSF samples are not always available. While invasive, microdialysis catheters are relatively safe and readily placed at the bedside in conjunction with other cerebral monitoring devices.
Previously, we demonstrated that microdialysis could be used to serially measure amyloid-beta peptide (Aβ) levels in the brain interstitial fluid of severely injured patients undergoing invasive intracranial neurosurgical procedures for other clinical indications (Brody et al., 2008). We found that brain interstitial fluid Aβ dynamics correlated with neurological status, a result that fits nicely with a body of experimental evidence indicating that synaptic activity is directly linked to Aβ production and release into the extracellular space (Kamenetz et al., 2003; Cirrito et al., 2005, 2008; Kang et al., 2009; Bero et al., 2011).These interesting Aβ dynamics were not apparent in concomitantly sampled ventricular CSF (Brody et al., 2008).
However, we are aware of only one previous study of tau levels in the human brain interstitial fluid. Marklund and colleagues (2009) found that patients with microdialysis catheters placed near areas of focal injury apparent on CT scans had higher brain interstitial fluid tau levels than patients with presumed diffuse axonal injury. There was a negative correlation at later time points between tau levels and Aβ1–42 levels, but the sample size (n = 8 patients) and low sensitivity of the Aβ detection methods used limited the conclusions that could be drawn. NF-L has not previously been measured by microdialysis to our knowledge. Recently, proteolytic cleavage products of neurofilament heavy chain have been measured using high-molecular weight cut-off microdialysis catheters and found to be predictive of mortality following severe traumatic brain injury (Petzold et al., 2011).
We hypothesized that microdialysis measurements of tau and NF-L in the extracellular space of the injured human brain would represent a useful approach to assess the severity of traumatic axonal injury. Furthermore, we were interested in the relationship between axonal injury markers and Aβ based on our previous studies of Aβ dynamics. With these aims in mind, we developed sensitive methods to allow assessment of tau and NF-L levels with high time resolution in the same microdialysis samples used for measurements of Aβ. We used these methods in a total of 16 patients with severe traumatic brain injury, and found that tau levels were highest in pericontusional regions, inversely correlated with Aβ levels, concordant with NF-L levels and most importantly predictive of 6 month adverse clinical outcomes.
Materials and methods
Patients
All research protocols were approved by the human research protection offices at the Ospedale Maggiore Policlinico in Milan and Washington University in St Louis. Next of kin or legally authorized representatives provided written informed consent for every patient. A total of 19 patients admitted to intensive care for severe closed-head traumatic brain injury between 2006 and 2010 met inclusion criteria and were approached for this study. These inclusion criteria were: (i) clinical indication for placement of invasive intracranial pressure monitoring; (ii) age ≥16 years at Ospedale Maggiore Policlinico, age ≥18 years at Washington University; (iii) no severe coagulopathy defined as clinical evidence of excessive bleeding, platelet counts <100 000, International Normalized Ratio >1.4, or partial thromboplastin time >50; (iv) no clinical indication for future anticoagulation, e.g. life-threatening deep vein thrombi/pulmonary embolisms; (v) not a member of a vulnerable population, e.g. prisoners; (vi) not pregnant; and (vii) family or next-of-kin available to provide written informed consent. Of these, family members of two patients did not consent, and useful microdialysis samples were obtained in all but one patient. In this patient, the microdialysis catheter was placed in the subarachnoid space, rather than in the brain parenchyma. This did not result in any adverse clinical events but the samples were uninterpretable and the catheter was promptly removed. This yielded a total sample size of 16 patients. Aβ levels from 10 of these patients have previously been reported (Brody et al., 2008).
Microdialysis
CMA71 catheters (CMA Microdialysis AB) with a nominal molecular weight cut-off of 100 kDa were inserted by trained neurosurgeons at either the Ospedale Maggiore Policlinico or Washington University. All catheters were inserted in conjunction with another clinically indicated intracranial procedure. In 10 patients, this was the insertion of an intracranial pressure monitoring device. In six patients, this was evacuation of an intracranial or extracranial haematoma with or without decompressive craniotomy. Microdialysis catheters were placed a mean of 21.5 h (25–75th percentile: 15–28 h) after injury (Supplementary Table 1). Sample acquisition was started 1–2 h after catheter insertion. CT scans were used to confirm the placement of the microdialysis catheters. CNS perfusion fluid (CMA Microdialysis AB) +1.5% sterile human albumin was perfused at a rate of 0.3 µl/min, as described previously (Brody et al., 2008). Samples were collected every 1 to 2 h for at least 72 h. Samples were immediately placed on ice and frozen at −80°C within 12 h of collection.
In vitro recovery of tau, NF-L and Aβ were measured for microdialysis catheters that were functioning normally at the time of removal and did not appear damaged. Catheters were inserted into vials of human CSF from patients with either traumatic brain injury or another neurological condition expected to cause elevated CSF tau and NF-L levels. Perfusion at the same flow rate with the same perfusion fluid was performed for 2–6 h. Aliquots of the CSF were placed into CMA collection tubes before and after the in vitro microdialysis. In vitro recovery was defined as the average concentration of each analyte in the microdialysis samples divided by the average concentration of each analyte in the CSF aliquots taken before and after in vitro microdialysis.
Analytical methods
Aβ1−x levels were measured by enzyme-linked immunosorbent assay (ELISA), as previously reported (Brody et al., 2008). The capture antibody was m266 recognizing Aβ13–26 and the detection antibody was biotinylated 3D6 recognizing Aβ1–5 with a free N-terminus. Standard curves were made using synthetic Aβ1–40 and ranged from 1.6 to 1200 pg/ml. The sensitivity of this ELISA was typically 4.9 pg/ml (Supplementary Table 2).
Total tau levels were measured by ELISA using a commercial kit (#KHB0042, Invitrogen). Recombinant human tau standards provided by the manufacturer were run with each set of assays to generate standard curves. The sensitivity of this ELISA was 32 pg/ml (Supplementary Table 2).
NF-L levels were measured by ELISA, as previously reported (Zanier et al., 2010). The capture antibody was the rabbit polyclonal AHP 286 (Serotec) and the detection antibodies were DA2 (Zymed) and 8A1 (Leinco). AHP 286 was raised using purified primate neurofilaments and recognizes NF-L with low levels of phosphorylation. DA2 is a mouse monoclonal antibody raised against dephosphorylated porcine NF-L that recognizes a phosphorylation-independent epitope (Shaw and Chau, 1988). 8A1 is a mouse monoclonal antibody raised against bovine NF-L (Guillemot and Cepko, 1992). All three cross react with human NF-L. Standard curves were made using purified bovine spinal cord NF-L (MP Biomedical). Two protocol modifications were made: biotinylated rabbit anti-mouse immunoglobulin-g (DAKO E0354) was used at 0.1 ng/ml and incubated for 1 h at room temperature. Poly-HRP 40-strep was used at 1:16 000 and incubated for 30 min at room temperature. The protocol was otherwise the same as previously published. The sensitivity of this ELISA was 12 pg/ml (Supplementary Table 2).
Lactate, pyruvate, glucose and glutamate measurements were made with a commercial bedside kinetic enzymatic analyser (CMA600) immediately after collection with standardization per the manufacturer's instructions before freezing. Urea was measured using the QuantiChrom (BioAssay Systems) colorimetric urea assay kit. A standard curve was run with each set of assays using urea standards provided by the manufacturer.
Sequential enzyme-linked immunosorbent assay
Due to the limited volume of samples available from human microdialysates (18 μl/h), the sequential ELISA method was used to measure multiple analytes in each sample (Osuchowski and Remick, 2006). The principle of the sequential ELISA strategy is that, in general, only one or a few specific analytes bind to the antibody coated wells of the ELISA plate; the rest remain in the solution phase. Instead of discarding the unbound analytes when the plate is washed after incubation, a portion of the solution phase can be transferred to another ELISA plate coated with a different capture antibody. This transfer step can be repeated several times.
Most samples were analysed as follows: original thawed samples were diluted between 1:10 and 1:30 and loaded onto a plate coated with m266 for measurements of Aβ1−x; after overnight incubation, 90 μl from each well was transferred to a plate coated with AHP286 for measurement of NF-L; after incubation, 50 μl from each well was mixed 1:1 with sample buffer from the Invitrogen human total tau kit and loaded into wells pre-coated with anti-tau antibody from the Invitrogen kit and; an additional 10–20 μl was diluted to 100 μl and assayed for urea. We used low protein binding polypropylene tubes (Axygen), and low protein binding plates and tips throughout. This process required a total of 4 days. Quantitative values have been reported after correction for all dilutions. All primary results reported are based on samples frozen and thawed once.
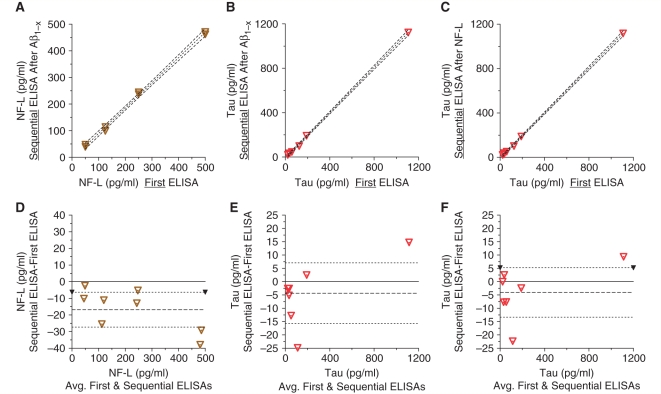
We verified that the sequential ELISA methods used to assess multiple analytes in the same samples resulted in accurate quantitation of the later analytes in the series. We performed sequential ELISAs on mock samples containing known quantities of Aβ, NF-L, tau and urea, and compared the results with the measurements obtained using standard (non-sequential) ELISA measurements on the same samples. For measurements of NF-L after Aβ1−x, tau after NF-L and tau after Aβ1−x, the results agreed very well [Fig. 1A–C, r2 = 0.99, 95% confidence interval (95% CI) of the slope of the best fit line close to 1 and 95% CI of the intercept always containing the origin]. Bland-Altman plots (Bland and Altman, 1999) demonstrated that there did not appear to be systematic errors due to the sequential ELISA procedure (Fig. 1D–F). We also tested the accuracy of the sequential ELISA measurements in five sets of pooled human microdialysis samples. This revealed that the sequential ELISA approach overestimated the true tau concentration by 3–9% compared with tau measurements made on naïve samples. The sequential ELISA approach underestimated the true NF-L concentration by 1–17%. We have not corrected for these errors, as none of the fundamental conclusions of the study would be altered as a result.
Figure 1.
Verification of the accuracy of sequential ELISA methods using mock microdialysis samples. Symbols indicate measured sample points. Dashed lines indicate linear best fits and 95% CIs. (A) NF-L sequential ELISA after Aβ1-x ELISA versus NF-L as the first ELISA: r2 = 0.99, slope 95% CI 0.90–0.99, y-intercept 95% CI −17.6 to 8.1. (B) Tau sequential ELISA after Aβ1-x ELISA versus tau as the first ELISA. r2 = 0.99, slope 95% CI 0.99–1.05, y-intercept 95% CI −20.5 to 2.3. (C) Tau sequential ELISA after NF-L ELISA versus tau as the first ELISA. r2 = 0.99, slope 95% CI 0.99–1.03, y-intercept 95% CI −17.7 to 3.4. (D–F) Bland-Altman plots for the data presented in panels (A–C).
Clinical outcome assessments
Telephone or in-person assessments of overall clinical outcome were performed using the Glasgow Outcome Scale-Extended (Teasdale et al., 1998; Wilson et al., 1998; Pettigrew et al., 2003). These assessments were performed at least 6 months after injury, and typically based on information obtained from both the patient and a reliable collateral source.
Statistical methods
All data were analysed using GraphPad Prism version 5 (GraphPad Software). Data were typically not normally distributed, so Mann–Whitney U-tests were used for unpaired group comparisons, Wilcoxon paired rank tests were used for comparisons across time and Spearman's rank order correlations were used for analyses of the relationships between variables. Two sided tests were used and were reported as significant for P < 0.05. P-values have not been corrected for multiple comparisons. Error bars and ranges represent 25–75th percentile confidence intervals.
To assess tau and Aβ dynamics in a homogenous fashion across all patients, time bins of 1–12 h and 61–72 h after the initiation of microdialysis were used. This made maximal use of the available samples, since microdialysis duration was variable (Supplementary Table 1). Parametric methods such as exponential curve fitting were not used, as there was a great deal of variability in the quality of such fits, and no a priori reason to presume a specific form (e.g. monoexponential) for the changes in analytes over time. Per cent changes in tau and Aβ were used as well as absolute changes because of the wide variation in initial levels of both markers.
Results
Brain extracellular tau and amyloid-β: diffuse injury versus contusion
We studied a total of 16 patients with severe traumatic brain injury from the Neurosurgical Intensive Care Unit at the Ospedale Maggiore Policlinico in Milan and the Neurological/Neurosurgical Intensive Care Unit at Barnes Jewish Hospital in St Louis. Clinical characteristics of the patients and position of microdialysis catheters are summarized in Table 1. No catheter placement-related intracranial haemorrhages were detected. There were no other adverse events related to microdialysis procedures.
Table 1.
Clinical characteristics of patients
| Case number | Age (years) M/F | Initial GCS | GOS-E at 6 months | Marshall CT classification | Type of surgery | Microdialysis catheter position |
|---|---|---|---|---|---|---|
| 1 | 32 F | 5 | 6 | Evacuated mass lesion | EDH, ICH, Dec Crani | L Frontal |
| 2 | 49 F | 5 | 7 | Evacuated mass lesion | SDH, ICH, Dec Crani | R Frontal |
| 3 | 50 F | 7 | 3 | Evacuated mass lesion | EDH, ICH, Dec Crani | R Frontal |
| 4 | 21 F | 7 | 5 | Evacuated mass lesion | EDH, SDH, ICH, Dec Crani | Pericontusional |
| 5 | 24 M | 7 | 3 | Diffuse injury II | None | Pericontusional |
| 6 | 31 F | 4 | 3 | Diffuse injury II | None | Pericontusional |
| 7 | 16 F | 4 | 4 | Diffuse injury III | None | R Frontal |
| 8 | 40 M | 6 | 3 | Diffuse injury II | None | R Frontal |
| 9 | 41 M | 5 | 4 | Diffuse injury II | None | R Frontal |
| 10 | 32 F | 13 | 3 | Evacuated mass lesion | SDH, Dec Crani | Pericontusional |
| 11 | 35 M | 11 | 6 | Evacuated mass lesion | ICH, Dec Crani | Pericontusional |
| 12 | 41 F | 6 | 3 | Diffuse injury II | None | R Frontal |
| 13 | 29 M | 5 | 3 | Diffuse injury II | None | R Frontal |
| 14 | 30 M | 5 | 7 | Diffuse injury II | None | R Frontal |
| 15 | 63 M | 5 | 1a | Non-evacuated Mass lesion | None | Pericontusional |
| 16 | 39 M | 3 | 3 | Evacuated mass lesion | SDH | Pericontusional |
Dec Crani = decompressive craniectomy; Diffuse injury II = cisterns present, midline shift <5 mm, and/or small <25 cc high or mixed density lesions; Diffuse injury III = compressed or absent cisterns but midline shift <5 mm and/or small <25 cc high or mixed density lesions (Marshall et al., 1992); EDH = evacuation of epidural haematoma; GCS = initial post-stabilization total Glasgow Coma Score (Teasdale and Jennett, 1974); GOS-E = Glasgow Outcome Scale-Extended at 6 months (Wilson et al., 1998); ICH = evacuation of intracerebral haematoma; SDH = evacuation of subdural haematoma.
a This patient died of causes unrelated to traumatic brain injury ∼2 months after injury.
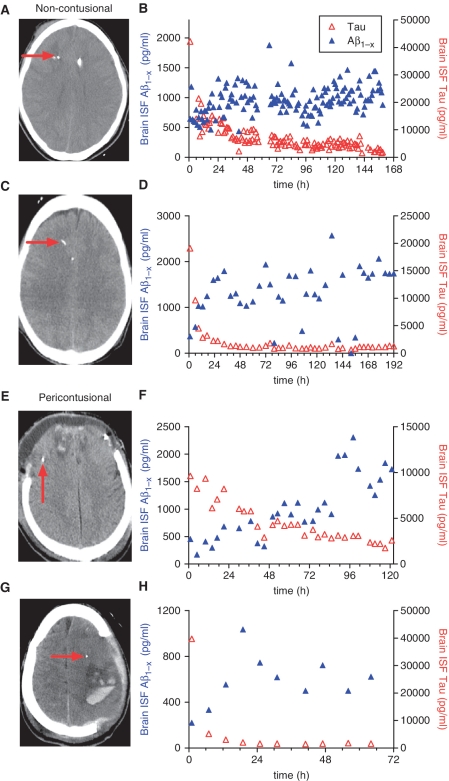
In nine patients, there were no apparent focal lesions on CT scans in the frontal lobes that could be targeted for microdialysis. In eight of these patients, the microdialysis catheters and intracranial pressure monitors were placed in the right frontal subcortical white matter (e.g. Fig. 2A and C). In one patient (Case 1), the catheter was placed in the left frontal subcortical white matter. These patients were all comatose (initial Glasgow coma scores 3–8) and such patients are often presumed to have diffuse axonal injury. These patients will be referred to as the ‘non-contusional’ group. In seven patients, there were frontal haemorrhagic contusions apparent on CT scans (e.g. Fig. 2E and G). In six of these patients, the microdialysis catheters were placed in pericontusional regions on either the right or left frontal lobe. In one patient (Case 6), the catheter was placed in the parietal lobe. These patients with apparent contusions near the microdialysis catheters will be referred to as the ‘pericontusional’ group.
Figure 2.
Examples of microdialysis-based measurements of tau and Aβ dynamics in the injured human brain. (A) CT scan of the brain from a patient in the non-contusional group. Microdialysis catheters tip (red arrow) apparent in normal-appearing right frontal subcortical white matter.(B) Brain interstitial fluid Aβ (left y-axis) and tau (right y-axis) levels as a function of time (h) since placement of the microdialysis catheter. (C and D) CT scan plus brain interstitial fluid Aβ and tau levels from another non-contusional patient. (E–H) CT scans plus brain interstitial fluid Aβ and tau levels from two patients with traumatic frontal contusions. Microdialysis catheter tips (red arrows) apparent near the frontal lobe contusions.
In all patients, tau levels could be measured in single microdialysis samples collected every 1 to 2 h. In initial patients (e.g. Fig. 2B), all hourly samples were analysed and a high time resolution time course was obtained. In the majority of the patients (e.g. Fig. 2D, F and H), samples were analysed every 4–6 h. Absolute tau levels varied considerably from patient to patient, but they were typically highest at the start of microdialysis and generally fell monotonically over time (Fig. 2). Interestingly, tau levels remained quite elevated even 72–120 h after the start of microdialysis (e.g. Fig. 2B and F). Aβ levels measured in the same samples rose over time (Fig. 2), as has been previously reported for a subset of these patients (Brody et al., 2008). Urea levels were measured as a control for microdialysis catheter function and were found to be stable, as previously shown (Brody et al., 2008).
In vitro recovery of tau ranged between 1% and 2%. In vitro recovery of Aβ was 30%, as reported previously (Brody et al., 2008). Despite several attempts, we have not been able to recover NF-L by microdialysis in vitro. These attempts have used human CSF with ∼1300 pg/ml of native NF-L (Zanier et al., 2010) and purified bovine NF-L spiked into artificial CSF at concentrations up to 500 ng/ml. Data presented here has not been corrected for fractional recovery.
Patients with contusions near the microdialysis catheters had higher tau levels than patients with catheters placed into non-contusional regions. Median tau levels over the first 24 h of microdialysis sampling in the pericontusional group were 15 950 pg/ml (11 390–27 240 pg/ml) versus 3469 pg/ml (1684–8691 pg/ml) in the non-contusional group (Fig. 3A, P = 0.005, Mann–Whitney U-test).
Figure 3.
Tau and Aβ measurements in non-contusional versus pericontusional groups. (A) Mean tau levels during the initial 24 h of microdialysis sampling were higher in patients with catheters placed in pericontusional regions: Error bars represent median and 25–75th percentiles (**P = 0.005, Mann–Whitney U-test). (B) Mean Aβ levels during the initial 24 h of microdialysis sampling were lower in pericontusional group (**P = 0.0012). (C) Tau levels decreased with time in all patients (*P = 0.0078 for non-contusional group, P = 0.016 for pericontusional group, Wilcoxon paired rank tests). (D) Aβ levels rose over time in all but one non-contusional patient (P = 0.29) and all but one pericontusional patient (*P = 0.031). NS = not significant.
In contrast, patients in the pericontusional group had lower Aβ levels than patients in the non-contusional group. Median Aβ levels over the first 24 h of microdialysis sampling in the pericontusional group were 270 pg/ml (83–417) versus 1023 pg/ml (778–1968) in the non-contusional group (Fig. 3B, P = 0.0012).
Tau dynamics were similar in the pericontusional and non-contusional groups. Tau levels fell from 1–12 h to 61–72 h in all patients in both groups (Fig. 3C, P = 0.016 for pericontusional group, P = 0.0078 for non-contusional group, Wilcoxon signed rank tests). The extent of the decrease between the pericontusional group (median decrease: 57%, range: 52–89%) and the non-contusional group (median decrease: 79%, range: 36–95%) was not significantly different (P = 0.72, Mann–Whitney U-test).
Aβ levels rose in most patients (Fig. 3D). This rise was significant in the pericontusional group (P = 0.031), though not significant for the non-contusional group in isolation (P = 0.29). The extent of the rise was greater in the pericontusional group (median increase: 170%, range: 88–220%) compared with the non-contusional group (median increase: 47%, range: 16–62%, P = 0.05).
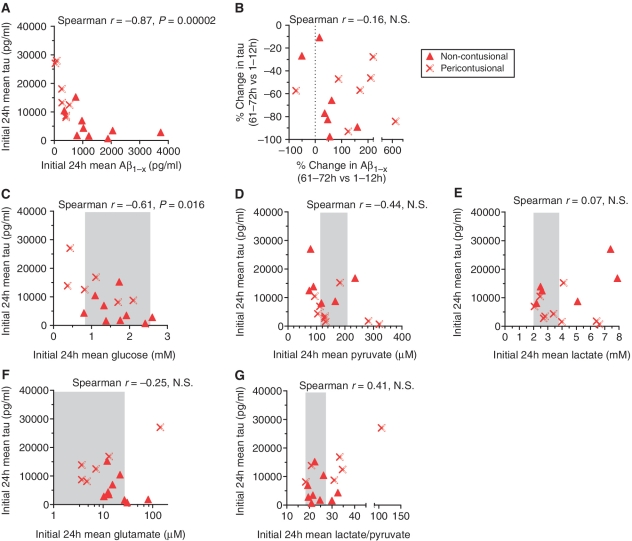
Correlations between tau and other microdialysis analytes
Patients with the highest tau levels typically had relatively low Aβ levels. This inverse correlation was highly statistically significant (Spearman r = −0.87, P = 0.000023) and present for both pericontusional and non-contusional patients (Fig. 4A).
Figure 4.
Correlations between tau and other microdialysis analytes. (A) Inverse correlation between initial Aβ levels and initial tau levels. (B) No correlation between the per cent change in Aβ levels and per cent change in tau levels. (C) Inverse correlation between initial brain interstitial fluid glucose levels and initial tau levels. (D) No significant correlation between initial brain interstitial fluid pyruvate levels and initial tau levels. (E) No correlation between initial brain interstitial fluid lactate levels and initial tau levels. (F) No correlation between initial brain interstitial fluid glutamate levels and initial tau levels. (G) No significant correlation between initial brain interstitial fluid lactate/pyruvate levels and initial tau levels. Shaded regions represent mean ± 1 standard deviation of estimated normal values (Reinstrup et al., 2000; Hillered et al., 2005). NS = not significant.
There was not a strong correlation between the dynamics of tau and Aβ. The extent of the reduction in tau from 1–12 h to 61–72 h after the initiation of microdialysis did not significantly correlate with the extent of the rise in Aβ during the same time period, as measured using per cent changes (Fig. 4B, r = −0.16) or absolute changes (data not shown).
The same microdialysis samples were assayed for commonly measured small molecule analytes (Hillered et al., 2005). There was a statistically significant negative correlation between tau levels and glucose levels (Fig. 4C, r = −0.61, P = 0.016); most glucose levels were within the normal range, but the two patients with abnormally low glucose levels also had high tau levels. There was a non-significant trend towards higher lactate/pyruvate ratios in patients with the highest tau levels (Fig. 4G, r = 0.41, P = 0.13) and no correlation between tau levels and glutamate levels (Fig. 4F). Microdialysis data for each individual subject are shown in Supplementary Table 1.
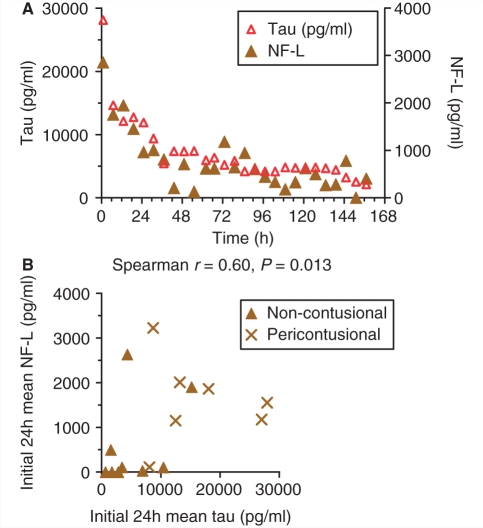
Tau as a marker of axonal injury: concordance with neurofilament light-chain levels
The dynamics of tau and NF-L levels were often very similar; both typically fell monotonically over time (e.g. Fig. 5A). There was a positive correlation between initial tau levels and initial NF-L levels (Fig. 5B, Spearman r = 0.60, P = 0.0013). NF-L levels were significantly higher in patients with microdialysis catheters placed near contusions (median: 1555 pg/ml, range: 1152–2012) than in patients with catheters placed in non-contusional regions (median 104 pg/ml, range: 0–1201, Fig. 5B, P = 0.04, Mann–Whitney U-test). This result was qualitatively similar to the findings for tau. NF-L levels were more variable than tau levels, and undetectable in some patients despite moderately high tau levels (Fig. 5B). Some of this may be due to instability of NF-L (Pant, 1988; Koel-Simmelink et al., 2011). We found that freezing and thawing microdialysis samples resulted in a 29 ± 12% (mean ± SD) loss of NF-L, but negligible loss of other analytes. This may account for the increased variability of NF-L measurements relative to other microdialysis markers.
Figure 5.
Close correspondence between microdialysis measurements of tau and NF-L. (A) Example of microdialysis-based measurements of brain interstitial fluid tau (left y-axis) and NF-L (right y-axis) dynamics in a non-contusional patient. (B) Positive correlation between initial tau and NF-L levels in 16 patients.
Microdialysis-based predictors of clinical outcome
We assessed the univariate relationship between early interstitial fluid tau levels and clinical outcomes in these patients and found a significant relationship in the expected direction: higher initial tau levels were associated with lower (worse) Glasgow Outcome Scale-Extended scores at 6 months after injury (Fig. 6A). This inverse correlation was statistically significant (r = −0.60, P = 0.018). The same fundamental relationship appeared to extend to both pericontusional patients and non-contusional patients. One patient died ∼2 months after injury of causes that were unrelated to traumatic brain injury. Therefore, this subject was not included in outcome analyses. No patients were in a persistent vegetative state (Glasgow Outcome Scale-Extended score of 2). Setting a cut-off value of 10 000 pg/ml (Fig. 6A, dashed horizontal line) allowed a 70% sensitivity and 80% specificity for predicting poor clinical outcome, defined as Glasgow Outcome Scale-Extended <5 (Fig. 6A, dashed vertical line). A cut-off value above 14 000 pg/ml allowed 60% sensitivity but 100% specificity for predicting poor clinical outcome. The area under the receiver operating characteristic curve was 0.76.
Figure 6.
Tau levels, but not levels of other microdialysis analytes, predicted overall clinical outcomes 6 months after injury. (A) Significant correlation between tau levels in the first 12 h after catheter placement and overall clinical outcomes. Better outcomes indicated by higher Glasgow Outcome Score-Extended scores. (B) Non-significant correlation between initial Aβ levels and clinical outcomes. (C) No correlation between initial brain interstitial fluid glucose levels and clinical outcomes. (D) Non-significant correlation between initial brain interstitial fluid lactate/pyruvate levels and clinical outcomes. (E) Non-significant correlation between initial brain interstitial fluid glutamate levels and clinical outcomes. NS = not significant.
There was not a strong relationship between Aβ levels and clinical outcomes in these patients. Lower initial Aβ levels were weakly associated with worse outcomes (Fig. 6B), but this was not statistically significant. Neither the dynamics of tau nor Aβ correlated with clinical outcomes (data not shown). Likewise, neither initial glucose levels (Fig. 6C), lactate/pyruvate ratios (Fig. 6D), nor glutamate levels (Fig. 6E) were significantly correlated with outcome in these patients.
Discussion
In summary, we have found that the axonal proteins tau and NF-L can be quantitatively assessed with 1–2 h time resolution by microdialysis in the injured human brain. The levels of these two putative markers of axonal injury were highest when microdialysis catheters were placed in pericontusional regions, but still elevated when catheters were placed in normal-appearing regions of the brain. Initial tau levels were inversely correlated with initial Aβ levels, and dynamics were opposite; Aβ rose and tau fell over time concordantly with the dynamics in CSF following severe traumatic brain injury reported by others (Kay et al., 2003). Importantly, initial microdialysis tau levels directly correlated with poor clinical outcomes. Other microdialysis analytes including Aβ, glucose, lactate/pyruvate ratio and glutamate did not correlate with outcomes. However, glucose, lactate/pyruvate and glutamate were often within the normal range, making it difficult to directly compare our patients to those in other series (Zauner et al., 1997; Koura et al., 1998; Goodman et al., 1999; Marcoux et al., 2008; Timofeev et al., 2011). Overall, our findings complement and extend previous results on the topic of microdialysis measurements of tau (Marklund et al., 2009).
We interpret these results as adding support for the hypothesis that axonal injury may be related to long-term impairments following traumatic brain injury. It is not surprising that the levels of tau and NF-L were higher in pericontusional regions; we expect that there is more neuronal loss and likely more extensive axonal injury in these regions than in regions that appear normal on CT. However, even the patients in whom catheters were placed into brain regions without CT lesions were in coma on admission to the hospital. Such patients are often presumed to have widespread or diffuse axonal injury. However, this diagnosis is rarely verified in the intensive care unit. The most likely interpretation of our findings is that there is substantial axonal injury also in normal-appearing regions of the brain following severe traumatic brain injury. Elevated brain interstitial fluid tau and NF-L levels detected by microdialysis support the diagnosis of diffuse axonal injury in these patients. This interpretation fits well with other lines of evidence that suggests that axonal injury is a primary determinant of many adverse outcomes following traumatic brain injury (Gennarelli et al., 1982; Smith et al., 2000, 2003b; Huisman et al., 2004; Wilde et al., 2006; Kraus et al., 2007; Levin et al., 2008; Niogi et al., 2008a, b; Wang et al., 2008; Kumar et al., 2009; Lipton et al., 2009; Lo et al., 2009; Perlbarg et al., 2009; Chang et al., 2010; Kondo et al., 2010; Marquez de la Plata et al., 2010; Warner et al., 2010; Kinnunen et al., 2011; Petzold et al., 2011).
An alternative explanation is that trauma to the brain due to insertion of the microdialysis catheter itself is responsible for the elevated tau levels in patients without apparent CT abnormalities. We cannot fully rule out a contribution of iatrogenic trauma, but argue that this is not likely to explain the majority of the tau and NF-L elevations. First, the levels and time courses of these proteins were quite variable, which is more consistent with variable initial injury severities and ongoing axonal degeneration, and less consistent with the relatively stereotyped catheter insertion procedure. Second, elevated levels of tau were associated with poor clinical outcomes. These poor outcomes are more likely to be related to injury severity and very unlikely to result from insertion trauma. Ultimately, experimental animal models including microdialysis data from uninjured control groups (Alessandri et al., 2003; Timaru-Kast et al., 2008; Schwetye et al., 2010) will be required to definitively resolve this issue. Along these lines, recent tau microdialysis experiments in uninjured mice indicate that insertional trauma has little effect on tau levels (K. Yamada and D.M. Holtzman, unpublished results).
There are several limitations of this study that should be kept in mind. Most importantly, we have not directly verified the relationship between brain interstitial fluid tau levels and the severity of traumatic axonal injury. This would likely require an experimental animal model in which microdialysis measurements are correlated with histopathological assessments of axonal injury in each animal in the region surrounding the microdialysis catheter location. Pig models could be appropriate for this approach, as the same catheters used in human patients can be placed into pig brain subcortical white matter as is typically done in human patients (Alessandri et al., 2003; Timaru-Kast et al., 2008). Advanced imaging methods sensitive to traumatic axonal injury such as Diffusion Tensor Imaging (Mac Donald et al., 2007a, b; Perlbarg et al., 2009; Niogi and Mukherjee, 2010) in the same subjects studied by microdialysis would also be of great interest. This is a critical area for future investigation. While predominantly axonal tau has also been detected in other non-neuronal cell types after traumatic brain injury (Smith et al., 2003), and a dendritic role for tau has been reported (Ittner et al., 2010). Nonetheless, the concordance of tau and NF-L levels makes it likely that both of these markers fundamentally reflect the same axonal injury processes.
Second, we have not measured the levels of tau and NF-L normally present in the extracellular space of the human brain. One would expect the normal extracellular levels to be quite low as they are both intracellular cytoskeletal proteins. CSF studies, while not directly comparable to microdialysis, have demonstrated considerably lower levels of these proteins in normal controls than in patients with traumatic brain injury (Zemlan et al., 1999; Franz et al., 2003; Norgren et al., 2003; Van Geel et al., 2005; Ost et al., 2006; Zetterberg et al., 2006).
Third, the relatively modest sample size precluded meaningful multivariate analyses of the predictors of outcomes (Timofeev et al., 2011). This will be an important avenue for future investigation. For example, it would be of great interest to assess whether the use of microdialysis-based measurements of initial tau levels improves upon the predictions of outcome made by the IMPACT model, which incorporates early clinical factors and Marshall CT scan classification (Murray et al., 2007).
Fourth, the relative recovery of tau was poor, and potentially variable between subjects. This potential variability between patients could have influenced our findings, but is not likely to have caused the correlation between tau levels and 6 month clinical outcomes. The use of even higher molecular weight cut-off catheters or additional carrier proteins in the perfusion fluid could be used to improve recovery in future investigations. We have not been able to determine the relative recovery of NF-L, despite several in vitro attempts, including catheter immersion in a large volume of human CSF (Afinowi et al., 2009). This suggests one of the two interpretations: either that the recovery is <0.1%, or the characteristics of NF-L in vitro (i.e. oligomerization, binding to other proteins, degradation, phosphorylation, glycosylation etc.) are different from those in vivo (Petzold, 2005). We have not assessed the molecular weight, isoelectric point, phosphorylation status or hydrophobicity of the tau and NF-L recovered by microdialysis from the injured human brain. These are important areas for future investigation, but beyond the scope of the current manuscript.
An intriguing observation arising from this study is the wide variation in the rate at which tau and NF-L decreased over time. It does not appear that changes due to dilution (e.g. from oedema) or systematic declines in microdialysis recovery are responsible; Aβ levels rose over time and urea levels remained stable. These variable decreases are likely to be due at least in part to heterogeneity in factors influencing diffusion and clearance, but could also in principle reflect variable ongoing release of these proteins into the interstitial fluid. In this study design, we cannot distinguish between these two possibilities. Local brain blood flow measurements could be helpful in future investigations. This is a critical question, as delayed axonal degeneration could be an important target for therapeutic interventions, whereas if all of the axonal injury occurs at the time of injury, efforts to improve prevention or restorative therapy would be more appropriate. Again, a valid experimental model will be required to fully address this issue.
As stated above, we have not assessed the phosphorylation state of tau in the interstitial fluid following traumatic brain injury. Hyperphosphorylated tau aggregations in the form of perisomatic and proximal dendritic tangles or neuropil threads are pathological features of sports-related chronic traumatic encephalopathy and a subset of severe cases of traumatic brain injury (Geddes et al., 1999; Ikonomovic et al., 2004; Jellinger, 2004; Uryu et al., 2007; McKee et al., 2009). These pathologies are similar to those seen in several age-related neurodegenerative disorders (Lee et al., 2001). The relationship between elevated extracellular tau levels detected by microdialysis and these aggregations of intracellular tau detected by immunohistochemistry following traumatic brain injury is unknown. We speculate that injury to both axonal membranes and cytoskeletal structures could release tau protein into the extracellular space. Less severe axonal injury could release some tau into the extracellular space, but result in additional tau protein being dissociated from disrupted microtubules yet retained intracellularly. This tau could aggregate in situ or be transported back to the cell bodies. Alternatively, different pools of tau could be involved: axonal tau could be released into the interstitial fluid, and newly synthesized tau could aggregate proximally in part because it is not properly transported into axons.
Hyperphosphorylation of tau dramatically reduces its solubility. Therefore, the fractional recovery of these hyperphosphorylated tau species by microdialysis would be expected to be very low, at least for the 100 kDa molecular weight cut-off microdialysis catheters employed in this study. Catheters with a very high molecular weight cut-off (Winter et al., 2002, 2004) could be considered for future investigations along these lines.
The findings that interstitial fluid Aβ levels were lowest when tau levels were highest may seem surprising, but should be interpreted in the context of the established effects of synaptic activity on soluble extracellular Aβ release. Aggregation and elevated levels of Aβ have been reported in association with traumatic axonal injury in both human patients with traumatic brain injury and experimental animals (Smith et al., 1999, 2003a; Ikonomovic et al., 2004; Uryu et al., 2007). However, these aggregations were detected immunohistochemically and were likely to represent primarily insoluble Aβ. Microdialysis instead samples the soluble extracellular Aβ pool (Hillered et al., 2005; Schwetye et al., 2010). Aβ dynamics in this soluble extracellular pool have been shown to be tightly linked to synaptic activity in animals (Cirrito et al., 2005, 2008) and positively correlated with neurological status in humans (Brody et al., 2008). Thus, we interpret the low interstitial fluid Aβ levels in the patients with high tau levels as an indication that more severe axonal injury causes more profound synaptic and neurological impairment in these patients. It is unlikely that the arrow of causality is in the opposite direction, i.e. higher Aβ levels somehow prevent release of tau into the interstitial fluid or enhance its clearance.
From a clinical perspective, microdialysis-based monitoring of tau and NF-L to assess axonal injury could potentially be used together with other methods to add information about the status of brain white matter following severe brain injury. Further studies will be required to determine whether this or any other microdialysis-based monitoring improves outcomes or assists in prognosis. Rapid improvements in the speed and sensitivity of protein biomarker measurements may allow bedside assessments in the near future (Arruda et al., 2009). If fully validated, these microdialysis-based assessments of tau and NF-L could be useful for early phase clinical pharmacodynamic testing of candidate therapeutics targeting traumatic axonal injury.
Funding
Burroughs Wellcome Career Award in the Biomedical Sciences (to D.L.B.); National Institutes of Health (grant numbers K08 NS049237 and R01 NS065069 to D.L.B.); Fondazione IRCCS Cà Granda-Ospedale Maggiore Policlinico, departmental funds.
Supplementary material
Supplementary material is available at Brain online.
Acknowledgements
We are grateful to the patients and their families for participation in this study. We would like to thank the ICU nurses and students at both Washington University and Ospedale Maggiore Policlinico including Giovanna Brandi, Anna Sigurtà, Ilaria Belloni and Kate Schwetye for assistance in collecting samples and data. We thank the Radiology Department of the Fondazione IRCCS Cà Granda-Ospedale Maggiore Policlinico for providing the CT images. We thank Dr Michael Diringer for serving as the external safety monitor at Washington University.
Glossary
Abbreviations
- Aβ
amyloid-β peptide
- ELISA
enzyme-linked immunosorbent assay
- NF-L
neurofilament-light chain
References
- Adams JH, Doyle D, Ford I, Gennarelli TA, Graham DI, McLellan DR. Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology. 1989;15:49–59. doi: 10.1111/j.1365-2559.1989.tb03040.x. [DOI] [PubMed] [Google Scholar]
- Adams JH, Graham DI, Murray LS, Scott G. Diffuse axonal injury due to nonmissile head injury in humans: an analysis of 45 cases. Ann Neurol. 1982;12:557–63. doi: 10.1002/ana.410120610. [DOI] [PubMed] [Google Scholar]
- Adams JH, Jennett B, Murray LS, Teasdale GM, Gennarelli TA, Graham DI. Neuropathological findings in disabled survivors of a head injury. J Neurotrauma. 2011;28:701–9. doi: 10.1089/neu.2010.1733. [DOI] [PubMed] [Google Scholar]
- Afinowi R, Tisdall M, Keir G, Smith M, Kitchen N, Petzold A. Improving the recovery of S100B protein in cerebral microdialysis: implications for multimodal monitoring in neurocritical care. J Neurosci Methods. 2009;181:95–9. doi: 10.1016/j.jneumeth.2009.02.021. [DOI] [PubMed] [Google Scholar]
- Alessandri B, Heimann A, Filippi R, Kopacz L, Kempski O. Moderate controlled cortical contusion in pigs: effects on multi-parametric neuromonitoring and clinical relevance. J Neurotrauma. 2003;20:1293–305. doi: 10.1089/089771503322686094. [DOI] [PubMed] [Google Scholar]
- Arruda DL, Wilson WC, Nguyen C, Yao QW, Caiazzo RJ, Talpasanu I, et al. Microelectrical sensors as emerging platforms for protein biomarker detection in point-of-care diagnostics. Expert review of molecular diagnostics. 2009;9:749–55. doi: 10.1586/erm.09.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett M, O'Brien DP, Phillips JP, Farrell MA. Clinicopathological observations in 100 consecutive patients with fatal head injury admitted to a neurosurgical unit. Irish Med J. 1995;88:60–2. [PubMed] [Google Scholar]
- Bero AW, Yan P, Roh JH, Cirrito JR, Stewart FR, Raichle ME, et al. Neuronal activity regulates the regional vulnerability to amyloid-beta deposition. Nat Neurosci. 2011;14:750–6. doi: 10.1038/nn.2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- Blumbergs PC, Jones NR, North JB. Diffuse axonal injury in head trauma. J Neurol Neurosurg Psychiatry. 1989;52:838–41. doi: 10.1136/jnnp.52.7.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumbergs PC, Scott G, Manavis J, Wainwright H, Simpson DA, McLean AJ. Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet. 1994;344:1055–6. doi: 10.1016/s0140-6736(94)91712-4. [DOI] [PubMed] [Google Scholar]
- Blumbergs PC, Scott G, Manavis J, Wainwright H, Simpson DA, McLean AJ. Topography of axonal injury as defined by amyloid precursor protein and the sector scoring method in mild and severe closed head injury. J Neurotrauma. 1995;12:565–72. doi: 10.1089/neu.1995.12.565. [DOI] [PubMed] [Google Scholar]
- Brody DL, Magnoni S, Schwetye KE, Spinner ML, Esparza TJ, Stocchetti N, et al. Amyloid-beta dynamics correlate with neurological status in the injured human brain. Science. 2008;321:1221–4. doi: 10.1126/science.1161591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang MC, Kim SH, Kim OL, Bai DS, Jang SH. The relation between fornix injury and memory impairment in patients with diffuse axonal injury: a diffusion tensor imaging study. NeuroRehabilitation. 2010;26:347–53. doi: 10.3233/NRE-2010-0572. [DOI] [PubMed] [Google Scholar]
- Christman CW, Grady MS, Walker SA, Holloway KL, Povlishock JT. Ultrastructural studies of diffuse axonal injury in humans. J Neurotrauma. 1994;11:173–86. doi: 10.1089/neu.1994.11.173. [DOI] [PubMed] [Google Scholar]
- Cirrito JR, Kang JE, Lee J, Stewart FR, Verges DK, Silverio LM, et al. Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo. Neuron. 2008;58:42–51. doi: 10.1016/j.neuron.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirrito JR, Yamada KA, Finn MB, Sloviter RS, Bales KR, May PC, et al. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005;48:913–22. doi: 10.1016/j.neuron.2005.10.028. [DOI] [PubMed] [Google Scholar]
- Emmerling MR, Morganti-Kossmann MC, Kossmann T, Stahel PF, Watson MD, Evans LM, et al. Traumatic brain injury elevates the Alzheimer's amyloid peptide A beta 42 in human CSF. A possible role for nerve cell injury. Ann N Y Acad Sci. 2000;903:118–22. doi: 10.1111/j.1749-6632.2000.tb06357.x. [DOI] [PubMed] [Google Scholar]
- Fishman R. Cerebrospinal fluid in diseases of the nervous system. 2nd edn. Philadelphia: Elsevier; 1992. [Google Scholar]
- Franz G, Beer R, Kampfl A, Engelhardt K, Schmutzhard E, Ulmer H, et al. Amyloid beta 1-42 and tau in cerebrospinal fluid after severe traumatic brain injury. Neurology. 2003;60:1457–61. doi: 10.1212/01.wnl.0000063313.57292.00. [DOI] [PubMed] [Google Scholar]
- Geddes JF, Vowles GH, Nicoll JA, Revesz T. Neuronal cytoskeletal changes are an early consequence of repetitive head injury. Acta Neuropathol. 1999;98:171–8. doi: 10.1007/s004010051066. [DOI] [PubMed] [Google Scholar]
- Gennarelli TA, Thibault LE, Adams JH, Graham DI, Thompson CJ, Marcincin RP. Diffuse axonal injury and traumatic coma in the primate. Ann Neurol. 1982;12:564–74. doi: 10.1002/ana.410120611. [DOI] [PubMed] [Google Scholar]
- Goodman JC, Valadka AB, Gopinath SP, Uzura M, Robertson CS. Extracellular lactate and glucose alterations in the brain after head injury measured by microdialysis. Crit Care Med. 1999;27:1965–73. doi: 10.1097/00003246-199909000-00041. [DOI] [PubMed] [Google Scholar]
- Gorrie C, Oakes S, Duflou J, Blumbergs P, Waite PM. Axonal injury in children after motor vehicle crashes: extent, distribution, and size of axonal swellings using beta-APP immunohistochemistry. J Neurotrauma. 2002;19:1171–82. doi: 10.1089/08977150260337976. [DOI] [PubMed] [Google Scholar]
- Guillemot F, Cepko CL. Retinal fate and ganglion cell differentiation are potentiated by acidic FGF in an in vitro assay of early retinal development. Development. 1992;114:743–54. doi: 10.1242/dev.114.3.743. [DOI] [PubMed] [Google Scholar]
- Hillered L, Vespa PM, Hovda DA. Translational neurochemical research in acute human brain injury: the current status and potential future for cerebral microdialysis. J Neurotrauma. 2005;22:3–41. doi: 10.1089/neu.2005.22.3. [DOI] [PubMed] [Google Scholar]
- Huisman TA, Schwamm LH, Schaefer PW, Koroshetz WJ, Shetty-Alva N, Ozsunar Y, et al. Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. AJNR Am J Neuroradiol. 2004;25:370–6. [PMC free article] [PubMed] [Google Scholar]
- Ikonomovic MD, Uryu K, Abrahamson EE, Ciallella JR, Trojanowski JQ, Lee VM, et al. Alzheimer's pathology in human temporal cortex surgically excised after severe brain injury. Exp Neurol. 2004;190:192–203. doi: 10.1016/j.expneurol.2004.06.011. [DOI] [PubMed] [Google Scholar]
- Ittner LM, Ke YD, Delerue F, Bi M, Gladbach A, van Eersel J, et al. Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer's disease mouse models. Cell. 2010;142:387–97. doi: 10.1016/j.cell.2010.06.036. [DOI] [PubMed] [Google Scholar]
- Jellinger KA. Head injury and dementia. Curr Opin Neurol. 2004;17:719–23. doi: 10.1097/00019052-200412000-00012. [DOI] [PubMed] [Google Scholar]
- Kamenetz F, Tomita T, Hsieh H, Seabrook G, Borchelt D, Iwatsubo T, et al. APP processing and synaptic function. Neuron. 2003;37:925–37. doi: 10.1016/s0896-6273(03)00124-7. [DOI] [PubMed] [Google Scholar]
- Kang JE, Lim MM, Bateman RJ, Lee JJ, Smyth LP, Cirrito JR, et al. Amyloid-{beta} Dynamics are regulated by orexin and the sleep-wake cycle. Science. 2009;326:1005–7. doi: 10.1126/science.1180962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay AD, Petzold A, Kerr M, Keir G, Thompson E, Nicoll JA. Alterations in cerebrospinal fluid apolipoprotein E and amyloid beta-protein after traumatic brain injury. J Neurotrauma. 2003;20:943–52. doi: 10.1089/089771503770195795. [DOI] [PubMed] [Google Scholar]
- Kinnunen KM, Greenwood R, Powell JH, Leech R, Hawkins PC, Bonnelle V, et al. White matter damage and cognitive impairment after traumatic brain injury. Brain. 2011;134:449–63. doi: 10.1093/brain/awq347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koel-Simmelink MJ, Teunissen CE, Behradkia P, Blankenstein MA, Petzold A. The neurofilament light chain is not stable in vitro. Ann Neurol. 2011;69:1065–6. doi: 10.1002/ana.22438. [DOI] [PubMed] [Google Scholar]
- Kondo K, Maruishi M, Ueno H, Sawada K, Hashimoto Y, Ohshita T, et al. The pathophysiology of prospective memory failure after diffuse axonal injury–lesion-symptom analysis using diffusion tensor imaging. BMC Neurosci. 2010;11:147. doi: 10.1186/1471-2202-11-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koura SS, Doppenberg EM, Marmarou A, Choi S, Young HF, Bullock R. Relationship between excitatory amino acid release and outcome after severe human head injury. Acta Neurochirurgica. 1998;71:244–6. doi: 10.1007/978-3-7091-6475-4_70. [DOI] [PubMed] [Google Scholar]
- Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM. White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain. 2007;130:2508–19. doi: 10.1093/brain/awm216. [DOI] [PubMed] [Google Scholar]
- Kumar R, Husain M, Gupta RK, Hasan KM, Haris M, Agarwal AK, et al. Serial changes in the white matter diffusion tensor imaging metrics in moderate traumatic brain injury and correlation with neuro-cognitive function. J Neurotrauma. 2009;26:481–95. doi: 10.1089/neu.2008.0461. [DOI] [PubMed] [Google Scholar]
- Lee VM, Goedert M, Trojanowski JQ. Neurodegenerative tauopathies. Ann Rev Neurosci. 2001;24:1121–59. doi: 10.1146/annurev.neuro.24.1.1121. [DOI] [PubMed] [Google Scholar]
- Levin HS, Wilde EA, Chu Z, Yallampalli R, Hanten GR, Li X, et al. Diffusion tensor imaging in relation to cognitive and functional outcome of traumatic brain injury in children. J Head Trauma Rehabil. 2008;23:197–208. doi: 10.1097/01.HTR.0000327252.54128.7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton ML, Gulko E, Zimmerman ME, Friedman BW, Kim M, Gellella E, et al. Diffusion-tensor imaging implicates prefrontal axonal injury in executive function impairment following very mild traumatic brain injury. Radiology. 2009;252:816–24. doi: 10.1148/radiol.2523081584. [DOI] [PubMed] [Google Scholar]
- Lo C, Shifteh K, Gold T, Bello JA, Lipton ML. Diffusion tensor imaging abnormalities in patients with mild traumatic brain injury and neurocognitive impairment. J Comput Assist Tomogr. 2009;33:293–7. doi: 10.1097/RCT.0b013e31817579d1. [DOI] [PubMed] [Google Scholar]
- Mac Donald CL, Dikranian K, Bayly P, Holtzman D, Brody D. Diffusion tensor imaging reliably detects experimental traumatic axonal injury and indicates approximate time of injury. J Neurosci. 2007a;27:11869–76. doi: 10.1523/JNEUROSCI.3647-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mac Donald CL, Dikranian K, Song SK, Bayly PV, Holtzman DM, Brody DL. Detection of traumatic axonal injury with diffusion tensor imaging in a mouse model of traumatic brain injury. Exp Neurol. 2007b;205:116–31. doi: 10.1016/j.expneurol.2007.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcoux J, McArthur DA, Miller C, Glenn TC, Villablanca P, Martin NA, et al. Persistent metabolic crisis as measured by elevated cerebral microdialysis lactate-pyruvate ratio predicts chronic frontal lobe brain atrophy after traumatic brain injury. Crit Care Med. 2008;36:2871–7. doi: 10.1097/CCM.0b013e318186a4a0. [DOI] [PubMed] [Google Scholar]
- Marklund N, Blennow K, Zetterberg H, Ronne-Engström E, Enblad P, Hillered L. Monitoring of brain interstitial total tau and β amyloid proteins by microdialysis in patients with traumatic brain injury. J Neurosurg. 2009;110:1227–37. doi: 10.3171/2008.9.JNS08584. [DOI] [PubMed] [Google Scholar]
- Marquez de la Plata CD, Yang FG, Wang JY, Krishnan K, Bakhadirov K, Paliotta C, et al. Diffusion tensor imaging biomarkers for traumatic axonal injury: analysis of three analytic methods. J Int Neuropsychol Soc. 2010;17:24–35. doi: 10.1017/S1355617710001189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall LF, Marshall SB, Klauber MR, Van Berkum Clark M, Eisenberg H, Jane JA, et al. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9(Suppl 1):S287–92. [PubMed] [Google Scholar]
- McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709–35. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray GD, Butcher I, McHugh GS, Lu J, Mushkudiani NA, Maas AI, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:329–37. doi: 10.1089/neu.2006.0035. [DOI] [PubMed] [Google Scholar]
- Niogi SN, Mukherjee P, Ghajar J, Johnson CE, Kolster R, Lee H, et al. Structural dissociation of attentional control and memory in adults with and without mild traumatic brain injury. Brain. 2008b;131:3209–21. doi: 10.1093/brain/awn247. [DOI] [PubMed] [Google Scholar]
- Niogi SN, Mukherjee P. Diffusion tensor imaging of mild traumatic brain injury. J Head Trauma Rehabil. 2010;25:241–55. doi: 10.1097/HTR.0b013e3181e52c2a. [DOI] [PubMed] [Google Scholar]
- Niogi SN, Mukherjee P, Ghajar J, Johnson C, Kolster RA, Sarkar R, et al. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am J Neuroradiol. 2008a;29:967–73. doi: 10.3174/ajnr.A0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norgren N, Rosengren L, Stigbrand T. Elevated neurofilament levels in neurological diseases. Brain Res. 2003;987:25–31. doi: 10.1016/s0006-8993(03)03219-0. [DOI] [PubMed] [Google Scholar]
- Ost M, Nylen K, Csajbok L, Ohrfelt AO, Tullberg M, Wikkelso C, et al. Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology. 2006;67:1600–4. doi: 10.1212/01.wnl.0000242732.06714.0f. [DOI] [PubMed] [Google Scholar]
- Osuchowski MF, Remick DG. The repetitive use of samples to measure multiple cytokines: the sequential ELISA. Methods. 2006;38:304–11. doi: 10.1016/j.ymeth.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Pant HC. Dephosphorylation of neurofilament proteins enhances their susceptibility to degradation by calpain. Biochem J. 1988;256:665–8. doi: 10.1042/bj2560665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlbarg V, Puybasset L, Tollard E, Lehericy S, Benali H, Galanaud D. Relation between brain lesion location and clinical outcome in patients with severe traumatic brain injury: a diffusion tensor imaging study using voxel-based approaches. Human Brain Mapping. 2009;30:3924–33. doi: 10.1002/hbm.20817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew LE, Wilson JT, Teasdale GM. Reliability of ratings on the Glasgow Outcome Scales from in-person and telephone structured interviews. J Head Trauma Rehabil. 2003;18:252–8. doi: 10.1097/00001199-200305000-00003. [DOI] [PubMed] [Google Scholar]
- Petzold A. Neurofilament phosphoforms: surrogate markers for axonal injury, degeneration and loss. J Neurol Sci. 2005;233:183–98. doi: 10.1016/j.jns.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Petzold A, Tisdall MM, Girbes AR, Martinian L, Thom M, Kitchen N, et al. vivo monitoring of neuronal loss in traumatic brain injury: a microdialysis study. Brain. 2011;134:464–83. doi: 10.1093/brain/awq360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinstrup P, Stahl N, Mellergard P, Uski T, Ungerstedt U, Nordstrom CH. Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery. 2000;47:701–9. doi: 10.1097/00006123-200009000-00035. discussion 9–10. [DOI] [PubMed] [Google Scholar]
- Schwetye KE, Cirrito JR, Esparza TJ, Mac Donald CL, Holtzman DM, Brody DL. Traumatic brain injury reduces soluble extracellular amyloid-beta in mice: a methodologically novel combined microdialysis-controlled cortical impact study. Neurobiol Dis. 2010;40:555–64. doi: 10.1016/j.nbd.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw G, Chau V. Ubiquitin and microtubule-associated protein tau immunoreactivity each define distinct structures with differing distributions and solubility properties in Alzheimer brain. Proc Natl Acad Sci USA. 1988;85:2854–8. doi: 10.1073/pnas.85.8.2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DH, Chen XH, Iwata A, Graham DI. Amyloid beta accumulation in axons after traumatic brain injury in humans. J Neurosurg. 2003a;98:1072–7. doi: 10.3171/jns.2003.98.5.1072. [DOI] [PubMed] [Google Scholar]
- Smith DH, Chen XH, Nonaka M, Trojanowski JQ, Lee VM, Saatman KE, et al. Accumulation of amyloid beta and tau and the formation of neurofilament inclusions following diffuse brain injury in the pig. J Neuropathol Exp Neurol. 1999;58:982–92. doi: 10.1097/00005072-199909000-00008. [DOI] [PubMed] [Google Scholar]
- Smith C, Graham DI, Murray LS, Nicoll JA. Tau immunohistochemistry in acute brain injury. Neuropathol Appl Neurobiol. 2003;29:496–502. doi: 10.1046/j.1365-2990.2003.00488.x. [DOI] [PubMed] [Google Scholar]
- Smith DH, Meaney DF, Shull WH. Diffuse axonal injury in head trauma. J Head Trauma Rehabil. 2003b;18:307–16. doi: 10.1097/00001199-200307000-00003. [DOI] [PubMed] [Google Scholar]
- Smith DH, Nonaka M, Miller R, Leoni M, Chen XH, Alsop D, et al. Immediate coma following inertial brain injury dependent on axonal damage in the brainstem. J Neurosurg. 2000;93:315–22. doi: 10.3171/jns.2000.93.2.0315. [DOI] [PubMed] [Google Scholar]
- Strich SJ. Diffuse Degeneration of the cerebral white matter in severe dementia following head injury. J Neurol, Neurosurg Psychiatry. 1956;19:163–85. doi: 10.1136/jnnp.19.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strich SJ. Shearing of nerve fibres as a cause of brain damage due to head injury. Lancet. 1961;2:443–8. [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Teasdale GM, Pettigrew LE, Wilson JT, Murray G, Jennett B. Analyzing outcome of treatment of severe head injury: a review and update on advancing the use of the Glasgow Outcome Scale. J Neurotrauma. 1998;15:587–97. doi: 10.1089/neu.1998.15.587. [DOI] [PubMed] [Google Scholar]
- Timaru-Kast R, Meissner A, Heimann A, Hoelper B, Kempski O, Alessandri B. Acute subdural hematoma in pigs: role of volume on multiparametric neuromonitoring and histology. J Neurotrauma. 2008;25:1107–19. doi: 10.1089/neu.2008.0517. [DOI] [PubMed] [Google Scholar]
- Timofeev I, Carpenter KL, Nortje J, Al-Rawi PG, O'Connell MT, Czosnyka M, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134:484–94. doi: 10.1093/brain/awq353. [DOI] [PubMed] [Google Scholar]
- Uryu K, Chen XH, Martinez D, Browne KD, Johnson VE, Graham DI, et al. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp Neurol. 2007;208:185–92. doi: 10.1016/j.expneurol.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Geel WJ, Rosengren LE, Verbeek MM. An enzyme immunoassay to quantify neurofilament light chain in cerebrospinal fluid. J Immunol Methods. 2005;296:179–85. doi: 10.1016/j.jim.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Wang JY, Bakhadirov K, Devous MD, Sr, Abdi H, McColl R, Moore C, et al. Diffusion tensor tractography of traumatic diffuse axonal injury. Arch Neurol. 2008;65:619–26. doi: 10.1001/archneur.65.5.619. [DOI] [PubMed] [Google Scholar]
- Warner MA, Marquez de la Plata C, Spence J, Wang JY, Harper C, Moore C, et al. Assessing spatial relationships between axonal integrity, regional brain volumes, and neuropsychological outcomes after traumatic axonal injury. J Neurotrauma. 2010;27:2121–30. doi: 10.1089/neu.2010.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilde EA, Chu Z, Bigler ED, Hunter JV, Fearing MA, Hanten G, et al. Diffusion tensor imaging in the corpus callosum in children after moderate to severe traumatic brain injury. J Neurotrauma. 2006;23:1412–26. doi: 10.1089/neu.2006.23.1412. [DOI] [PubMed] [Google Scholar]
- Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–85. doi: 10.1089/neu.1998.15.573. [DOI] [PubMed] [Google Scholar]
- Winter CD, Iannotti F, Pringle AK, Trikkas C, Clough GF, Church MK. A microdialysis method for the recovery of IL-1beta, IL-6 and nerve growth factor from human brain in vivo. J Neurosci Methods. 2002;119:45–50. doi: 10.1016/s0165-0270(02)00153-x. [DOI] [PubMed] [Google Scholar]
- Winter CD, Pringle AK, Clough GF, Church MK. Raised parenchymal interleukin-6 levels correlate with improved outcome after traumatic brain injury. Brain. 2004;127:315–20. doi: 10.1093/brain/awh039. [DOI] [PubMed] [Google Scholar]
- Zanier ER, Refai D, Zipfel GJ, Zoerle T, Longhi L, Esparza TJ, et al. Neurofilament light chain levels in ventricular cerebrospinal fluid after acute a neurysmal subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2010;82:157–9. doi: 10.1136/jnnp.2009.177667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zauner A, Doppenberg EM, Woodward JJ, Choi SC, Young HF, Bullock R. Continuous monitoring of cerebral substrate delivery and clearance: initial experience in 24 patients with severe acute brain injuries. Neurosurgery. 1997;41:1082–91. doi: 10.1097/00006123-199711000-00011. discussion 91–3. [DOI] [PubMed] [Google Scholar]
- Zemlan FP, Rosenberg WS, Luebbe PA, Campbell TA, Dean GE, Weiner NE, et al. Quantification of axonal damage in traumatic brain injury: affinity purification and characterization of cerebrospinal fluid tau proteins. J Neurochem. 1999;72:741–50. doi: 10.1046/j.1471-4159.1999.0720741.x. [DOI] [PubMed] [Google Scholar]
- Zetterberg H, Hietala MA, Jonsson M, Andreasen N, Styrud E, Karlsson I, et al. Neurochemical aftermath of amateur boxing. Arch Neurol. 2006;63:1277–80. doi: 10.1001/archneur.63.9.1277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.