Abstract
Childhood maltreatment (CM) has been associated with diminished executive functioning in children and adults; however, there is a relative paucity of study of executive function in adolescents exposed to CM. Yet, executive dysfunction in adolescence may have important adverse consequences including increased vulnerability to risky behaviors and impaired school functioning. This study investigates the relationship between self-reported CM and an executive function, cognitive flexibility, in adolescents without identified psychiatric disorders. Effects of physical and emotional, abuse and neglect, maltreatment subtypes were explored. Thirty adolescents ages 12–17 years, 50% females, completed the retrospective self-report Childhood Trauma Questionnaire (CTQ) and were administered the Wisconsin Card Sorting Test (WCST). Correlational analyses assessed the relationship between WCST perseverative error scores norm-referenced for age and education with CTQ total scores. The relationship with non-perseverative errors, as well as with physical and emotional abuse and neglect CM subscores, were explored. Total CTQ scores showed significant associations with perseverative errors on the WCST, but not with non-perseverative errors. Significant associations with perseverative errors were seen for physical abuse and physical neglect among the CTQ subscales. The results suggest both physical abuse and physical neglect are associated with diminished cognitive flexibility in adolescents. These effects were detected in adolescents without identified psychiatric diagnoses suggesting the importance of considering executive dysfunction in adolescents exposed to CM who may not meet diagnostic criteria for an Axis I disorder and that tests of perseverative errors, such as those of the WCST, may be sensitive indicators of this dysfunction.
Introduction
Children and adult victims of abuse and neglect show disruptions in executive functions (Perez & Widom, 1994; Minzenberg, Poole, & Vinogradov, 2008). The relationship between childhood abuse and neglect with disturbances in executive functions in adolescents has received relatively little study. Yet, adolescence is a period during which a range of executive function abilities mature and reliance on frontal executive functions becomes increasingly necessary. Hence, compromised executive functioning in adolescents can have important adverse consequences.
Prepubertal children have demonstrated decreases in executive function performance on neuropsychological tests, including measures of attention, adaptive response inhibition and cognitive flexibility, in association with physical abuse and neglect (Beers & De Bellis, 2002; Pears & Fisher, 2005; Prasad, Kramer, & Ewing-Cobbs, 2005; Nolin & Ethier, 2007; De Bellis, Hooper, Spratt, & Woolley, 2009; Deprince, Weinzierl, & Combs, 2009). This suggests that physical abuse and neglect may adversely affect maturation of executive functions. Alterations in the developmental trajectory of executive function could lead to enduring developmental effects in adolescence and adulthood.
Associations between trauma and executive function have been demonstrated consistently in adults (Gil, Calev, Greenberg, Kugelmass, & Lerer, 1990; Diamond, Muller, Rondeau, & Rich, 2001; Stein, Kennedy, & Twamley, 2002; Brandes et al., 2002). The studies focused largely on adults with psychiatric disorders, predominantly with post-traumatic stress disorder (PTSD), and often did not assess effects of childhood abuse and neglect specifically. Studies of adults with a history of childhood maltreatment (CM) and without a psychiatric condition support the presence of adverse effects on aspects of executive functioning in the absence of psychopathology, including cognitive flexibility (Navalta, Polcari, Webster, Boghossian, & Teicher, 2006; Stein et al., 2002; Brandes et al., 2002).
The findings in children and adults exposed to CM implicate abnormalities in executive functioning in adolescents exposed to CM; however, there are limited prior studies of executive functioning in adolescents exposed to CM, and specifically of cognitive flexibility. In one study, female adolescents with PTSD who had been sexually abused demonstrated increased cognitive interference on a color-word Stroop task (Freeman & Beck, 2000). A study of adolescent boys in a therapeutic school who had a history of childhood physical abuse demonstrated difficulties in learning to avoid maladaptive responses on a passive avoidance learning task, as compared to boys in the therapeutic school who had not been abused and boys in local public schools (Mezzacappa, Kindlon, & Earls, 2001). These studies support the presence of vulnerability to executive function problems in adolescents exposed to CM. and suggest difficulties in the development of adaptive cognitive flexibility in adolescents exposed to CM, although this function was not tested specifically.
The current study investigates the relationship between self-reported history of CM on the Childhood Trauma Questionnaire (CTQ) and cognitive flexibility as assessed by perseverative errors measured on the Wisconsin Card Sorting Test (WCST), the WCST measure most sensitive to disturbances in frontal executive function (Greve, Stickle, Love, Bianchini, & Stanford, 2005; Heaton, Chelune, Talley, Kay, & Curtis, 1993). The adolescents were without psychiatric diagnoses, diminishing potential confounds of psychiatric symptoms. It was hypothesized that higher CTQ scores would be associated with more perseverative errors on the WCST.
Methods
Participants consisted of 15 male and 15 female adolescents, ages 12–17 years, with a mean age of 14.8yrs (SD=1.6) from the greater New Haven community. The adolescents were all enrolled in school and had a mean 9th grade level of education. Ethnic distribution was Caucasian (40%), Black (37%), Latino (10%), and Multiracial (13%). Mean socioeconomic status (SES), estimated using the Hollingshead Social Status Scale (Hollingshead, 1975), was 39.5 (SD=13.6), which falls in approximately the middle range of SES scores. Participants did not meet criteria for a major Axis I disorder as confirmed by administration of the revised Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version 2.0 [K-SADS-PL; (Kaufman, Birmaher, Brent, Rau, & Ryan, 1996)] to the participants and a parent or guardian. There was no history of psychiatric disorder in a first-degree relative as assessed by the Family History Screen for Epidemiologic Studies (Lish, Weissman, Adams, Hoven, & Bird, 1995). No participant had a history of major medical disorder or neurological disorder, loss of consciousness for five or more minutes or intelligence quotient below 70.
After a complete description of the research, written informed consent was obtained from parents/guardians. Written informed assent was obtained from minors. This research was approved by the institutional review board of the Yale School of Medicine.
All subjects completed the CTQ (Bernstein et al., 1994, 2003; Bernstein & Fink, 1998), a 28-item retrospective self-report questionnaire. In the CTQ, the CM domains of physical abuse, sexual abuse, emotional abuse, physical neglect and emotional neglect are each assessed by five items which participants rate on a five-point scale ranging from “never true” to “very often true” according to the frequency with which each event occurred. Physical abuse is defined as bodily assaults on a child by an older person that poses a risk for or results in injury, sexual abuse as sexual contact or conduct between a child and an older person, emotional abuse as verbal assaults on a child’s sense of worth or well-being, or any humiliating, demeaning, or threatening behavior directed toward a child by an older person, physical neglect as failure of caregivers to provide a child’s basic physical needs and emotional neglect as the failure of caretakers to provide basic psychological and emotional needs (Bernstein et al., 1994). Scores across the five CM domains are summed for a Total CTQ score; the five subscales scores permit assessments for effects each of the five abuse and neglect domains. Internal consistency has ranged from .76 to .92 (Bernstein et al., 1994, 1997, 2003; Bernstein & Fink, 1998; Wolfe, Scott,Wekerle, & Pittman, 2001; Messman-Moore & Brown, 2004).
Each subject was also administered the Wisconsin Card Sorting Test [WCST; (Heaton et al., 1993)]. The perseverative error subscore of the WCST has been shown to be highly sensitive to frontal lobe dysfunction (Sutker, Moan, & Allain, 1983; Heaton et al., 1993; Greve et al., 2005) and was utilized for this study. Non-perseverative errors were also explored. Perseverative and non-perseverative norm-referenced scores, which adjust for age and level of education, served as the dependent measures in analyses.
Correlation analyses and t-tests were performed to assess for potential effects of age and gender on CTQ and WCST scores. Pearson Correlation analyses assessed the relationships between CTQ total scores and WCST perseverative and non-perseverative errors. Findings were considered significant for p<0.025, adjusted for the two WCST performance measures. For the WCST measure(s) showing significant associations with Total CTQ, associations were explored for CTQ physical abuse, physical neglect, emotional abuse and emotional neglect subscores. As only three subjects reported a history of sexual abuse, effects of these were not tested in analyses. All significant findings are reported below. Analyses were conducted using SAS, version 9.1 (SAS, 2004).
Results and Discussion
The current study provides evidence supportive of associations between self-reported CM and diminished cognitive flexibility in adolescents. Specifically, higher Total CTQ scores were associated with increased perseverative errors (lower norm-referenced scores), r=−0.42, p=0.02 (Figure 1), but did not show significant associations with non-perseverative errors. Correlations between norm-referenced scores for perseverative errors and CTQ subscores were significant for physical abuse r=−0.43, p=0.019, physical neglect r=−0.46, p=0.011. There were no significant associations between age and CTQ Total or subscores, or between gender and either WCST or CTQ scores. There were also no significant associations between emotional abuse and neglect, and perseverative error scores. These results suggest that both childhood physical abuse and neglect may negatively impact the development of cognitive flexibility leading to dysfunction in the adolescent epoch.
Figure 1.
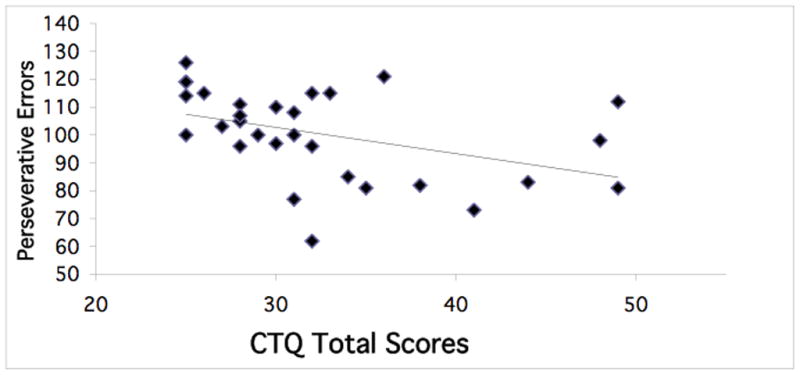
The Association Between Childhood Trauma Questionnaire Scores and WCST Performance.
The graph shows Wisconsin Card Sorting perseverative error scores norm-referenced to adjust for age and education as a function of total scores on the Childhood Trauma Questionnaire (CTQ Total Scores). The negative associations were significant indicating reports of higher childhood maltreatment were associated with lower performance, ie. more perseverative errors.
The findings are consistent with reports of executive dysfunction in prepubertal children in association with physical abuse and neglect. This suggests that this dysfunction may persist during the adolescent period and/or may influence the trajectory of executive development into adolescence. Determining whether executive dysfunction progresses from the prepubertal to adolescent epoch will require longitudinal studies that cross these developmental stages.
The finding in the adolescents in association with physical neglect is relatively novel. Prior reports of effects of early physical abuse on executive functioning in adults, as discussed above, suggest that these alterations may extend beyond childhood. Enduring effects of childhood physical neglect in adulthood have received little study. The current results suggest that physical neglect in childhood may also adversely affect the development of specific executive function capacities and the dysfunction persists at least into adolescence. This highlights the necessity for further studies of adolescents and adults exposed to physical neglect, as well as physical abuse, in childhood.
The neurobiological mechanisms that may mediate the effects of CM on executive function development cannot be determined from this study. Late childhood and adolescence are critical periods in the development of prefrontal cortical regions that subserve the maturation of executive functions, such as cognitive flexibility (Welsh, Pennington, & Groisser, 1991; Bourgeois, Goldman-Rakic, & Rakic, 1994; Lewis, 1997; Erickson, Akil, Levey, & Lewis, 1998; Klingberg, Vaidya, Gabrieli, Moseley, & Hedehus, 1999; Paus, 2004; Anderson, Anderson, Northam, Jacobs, & Catroppa, 2001; Luciana, Conklin, Hooper, & Yarger, 2005). Structural MRI studies show reduced brain frontal lobe volume in children exposed to CM (Weiss, Longhurst, & Mazure, 1999; De Bellis, 2005; Cicchetti & Toth, 2005; Minzenberg et al., 2008). Mechanisms theorized to mediate these effects include those related hypothalamic-pituitary-adrenal (HPA) axis (Weiss et al., 1999; Maciejewski & Mazure, 2006). Together, these data suggest adverse effects of CM on frontal development may underlie the effects reported herein. Physical neglect has received less study than physical abuse. However, it has the potential to have potent effects on frontal developmental as effects could derive both from emotional aspects of the neglect, effects on HPA functioning, as well as from deprivation of basic physical needs, such as nutrition and activity, critical for healthy neurodevelopment. Future studies of mechanisms that mediate effects of physical abuse and neglect on frontal maturation and associated executive functions are needed.
Small sample size is an important limitation of this study. Another limitation is the risk of potential recall bias as CM history was based on retrospective self-report. Although the CTQ has shown excellent reliability and validity in adolescent and adult community and psychiatric samples (Bernstein & Fink, 1998; Bernstein et al., 2003; Scher, Stein, Asmundson, McCreary, & Forde, 2001; Paivio & Cramer, 2004), multiple informant data or assessment of the specific ages of the CM were not available. Future studies that investigate specific ages at which the abuse and neglect occurred would be important in understanding the critical periods during which abuse and neglect influence adolescent dysfunction and the developmental mechanisms that mediate the effects. A further limitation is our focus on cognitive flexibility. Future studies that include both more comprehensive executive function testing, as well as that parse specific functions that may contribute to perseverative responses, could permit examination of the scope of executive dysfunction and more specifically define the abilities most affected. Identification of skills more likely to be preserved could aid researchers in constructing intervention strategies for CM exposure that draw on intact cognitive capacities that could potentially compensate for and minimize dysfunction.
The current study begins to fill the gap in the CM literature by providing evidence that adolescents exposed to childhood physical abuse and neglect may not express symptoms that meet full DSM-IV criteria for an Axis I disorder, but may have alterations in the development of executive functions, including the focus of this study, cognitive flexibility. This is important as executive dysfunction may present challenges to adolescents, such as difficulty with school performance, and diminished ability to adaptively inhibit behavior that in turn could contribute to increased engagement in risk-taking behaviors as well as elevated risk for psychiatric disorders (Weiss et al., 1999; Widom, 1999; Maciejewski & Mazure, 2006; Batten, Aslan, Maciejewski, & Mazure, 2004). Findings on the perseverative responses measure of the WCST suggest that such tests may provide sensitive indicators of difficulties that may otherwise elude detection during more standard clinical examinations.
Acknowledgments
This work was supported by the National Institute of Health (NIH) Roadmap for Medical Research Common Fund grant UL1-DE19586 (RS) and the NIH Roadmap for Medical Research/Common Fund (RS), National Institute of Drug Abuse RL1DA024856 (HPB, JHK, LCM), K05DA020091 (LCM) and PL1-DA24859 (RS), the National Institute of Mental Health R01MH69747 (HPB), T32MH14276 (JHK), Women’s Health Research at Yale (HPB, CMM), the National Alliance for Research in Schizophrenia and Depression (HPB, JHK), the Attias Family Foundation (HPB), Marcia Simon Kaplan (JHK) and the Klingenstein Foundation (JHK). We thank Susan Quatrano, Philip Markovich, Kathryn Armstrong, Sarah Nicholls, Matthew Freiburger, and Matthew Hirschtritt for their efforts with the research subjects and the research subjects for their participation.
References
- Anderson VA, Anderson P, Northam E, Jacobs R, Catroppa C. Development of executive functions through late childhood and adolescence in an australian sample. Developmental Neuropsychology. 2001;20(1):385–406. doi: 10.1207/S15326942DN2001_5. [DOI] [PubMed] [Google Scholar]
- Barlow KM, Thomson E, Johnson D, Minns RA. Late neurologic and cognitive sequelae of inflicted traumatic brain injury in infancy. Pediatrics. 2005;116:e174–e185. doi: 10.1542/peds.2004-2739. [DOI] [PubMed] [Google Scholar]
- Batten SV, Aslan M, Maciejewski PK, Mazure CM. Childhood maltreatment as a risk factor for adult cardiovascular disease and depression. Journal of Clinical Psychiatry. 2004;65(2):249–254. doi: 10.4088/jcp.v65n0217. [DOI] [PubMed] [Google Scholar]
- Beers SR, De Bellis MD. Neuropsychological function in children with maltreatment-related posttraumatic stress disorder. American Journal of Psychiatry. 2002;159(3):483–485. doi: 10.1176/appi.ajp.159.3.483. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. American Journal of Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood trauma Questionnaire in an adolescent psychiatric population. Journal of Child and Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T. Development and validation of a brief screening version of the Childhood Trauma Questionaire. Child Abuse & Neglect. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bourgeois J, Goldman-Rakic PS, Rakic P. Synaptogenesis in the prefrontal cortex of rhesus monkeys. Cerebral Cortex. 1994;4:78–96. doi: 10.1093/cercor/4.1.78. [DOI] [PubMed] [Google Scholar]
- Brandes D, Ben-Schachar G, Gilboa A, Bonne O, Freedman S, Shalev AY. PTSD symptoms and cognitive performance in recent trauma survivors. Psychiatry Research. 2002;110:231–238. doi: 10.1016/s0165-1781(02)00125-7. [DOI] [PubMed] [Google Scholar]
- Cichetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2006;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- De Bellis MD. The psychobiology of neglect. Child Maltreatment. 2005;10:150–172. doi: 10.1177/1077559505275116. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Hooper SR, Spratt EG, Woolley DP. Neuropsychological findings in childhood neglect and their relationships to pediatric PTSD. Journal of the International Neuropsychological Society. 2009;15:868–878. doi: 10.1017/S1355617709990464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePrince AP, Weinzierl KM, Combs MD. Executive function performance and trauma exposure in a community sample of children. Child Abuse & Neglect. 2009;33:353–361. doi: 10.1016/j.chiabu.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Diamond T, Muller RT, Rondeau LA, Rich JG. The relationships among PTSD symptomatology and cognitive functioining in adult survivors of child maltreatment. In: Columbus Frank., editor. Advances in Psychology Research. V. New York: Nova Science Publishers; 2001. pp. 253–279. [Google Scholar]
- Erickson SL, Akil M, Levey AI, Lewis DA. Postnatal development of tryosine hydroxylase- and dopamine transporter-immunoreactive axons in monkey rostral entorhinal cortex. Cerebral Cortex. 1998;8:415–427. doi: 10.1093/cercor/8.5.415. [DOI] [PubMed] [Google Scholar]
- Freeman JB, Beck JG. Cognitive interference for trauma cues in sexually abused adolescent girls with posttraumatic stress disorder. Journal of Clinical Child Psychology. 2000;29(2):245–256. doi: 10.1207/S15374424jccp2902_10. [DOI] [PubMed] [Google Scholar]
- Gil T, Calev A, Greenberg D, Kugelmass S, Lerer B. Cognitive functioning in post-traumatic stress disorder. Journal of Traumatic Stress. 1990;3(1):29–45. [Google Scholar]
- Greve KW, Stickle TR, Love JM, Bianchini KJ, Stanford MS. Latent structure of the wisconsin card sorting test: a confirmatory factor analytic study. Archives of Clinical Neuropsychology. 2005;20:355–364. doi: 10.1016/j.acn.2004.09.004. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtis G. Wisconsin Card Sorting Test Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1993. [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. New Haven: Department of Sociology, Yale University; 1975. [Google Scholar]
- Kaufman J, Birmaher B, Brent DA, Rau U, Ryan N. The schedule for affective disorders and schizophrenia for school-age children. University of Pittsburgh; 1996. [DOI] [PubMed] [Google Scholar]
- Klingberg T, Vaidya CJ, Gabrieli JDE, Moseley ME, Hedehus M. Myelination and organization of the frontal white matter in children: A diffusion tensor MRI study. NeuroReport. 1999;10:2817–2821. doi: 10.1097/00001756-199909090-00022. [DOI] [PubMed] [Google Scholar]
- Lewis DA. Development of the prefrontal cortex during adolescence: Insights into vulnerable neural circuits in schizophrenia. Neuropsychopharmacology. 1997;16(6):385–398. doi: 10.1016/S0893-133X(96)00277-1. [DOI] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4. New York, NY: Oxford University Press; 2004. [Google Scholar]
- Lish JD, Weissman MM, Adams PB, Hoven CW, Bird H. Family psychiatric screening instrument for epidemiologic studies: Pilot testing and validation. Psychiatric Research. 1995;57:169–180. doi: 10.1016/0165-1781(95)02632-7. [DOI] [PubMed] [Google Scholar]
- Luciana M, Conklin HM, Hooper CJ, Yarger RS. The development of nonverbal working memory and executive control processes in adolescents. Child Development. 2005;76(3):697–712. doi: 10.1111/j.1467-8624.2005.00872.x. [DOI] [PubMed] [Google Scholar]
- Maciejewski PK, Mazure CM. Fear of critisicm and rejection mediates an association between childhood emotional abuse and adult onset of major depression. Cognitive Therapy and Research. 2006;30(1):105–122. [Google Scholar]
- Messman-Moore TL, Brown AL. Child maltreatment and perceived family environment as risk factors for adult rape: is child sexual abuse the most salient experience? Child Abuse & Neglect. 2004;28:1019–1034. doi: 10.1016/j.chiabu.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Mezzacappa E, Kindlon D, Earls F. Child abuse and performance task assessments of executive functions in boys. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2001;42:1041–1048. doi: 10.1111/1469-7610.00803. [DOI] [PubMed] [Google Scholar]
- Minzenberg MJ, Poole JH, Vinogradov S. A neurocognitive model of borderline personality disorder: Effects of childhood sexual abuse and relationship to adult social attachment disturbance. Development and Psychopathology. 2008;20:341–368. doi: 10.1017/S0954579408000163. [DOI] [PubMed] [Google Scholar]
- Navalta CP, Polcari A, Webster DM, Boghossian A, Teicher MH. Effects of childhood sexual abuse on neuropsychological and cognitive function in college women. Journal of Neuropsychiatry and Clinical Neuroscience. 2006;18(1):45–53. doi: 10.1176/jnp.18.1.45. [DOI] [PubMed] [Google Scholar]
- Nolin P, Ethier L. Using neuropsychological profiles to classify neglected children with or without physical abuse. Child Abuse & Neglect. 2007;31:631–643. doi: 10.1016/j.chiabu.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Paus T. Mapping brain maturation and cognitive development during adolescence. TRENDS in Cognitive Science. 2004;9(2):60–68. doi: 10.1016/j.tics.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Pears K, Fisher PA. Developmental, cognitive, and neuropsychological functioning in preschool-aged foster children: Associations with prior maltreatment and placement history. Developmental and Behavioral Pediatrics. 2005;26(2):112–122. doi: 10.1097/00004703-200504000-00006. [DOI] [PubMed] [Google Scholar]
- Perez CM, Widom CS. Childhood victimization and long-term intellectual and academic outcomes. Child Abuse & Neglect. 1994;18(8):617–633. doi: 10.1016/0145-2134(94)90012-4. [DOI] [PubMed] [Google Scholar]
- Piavio SC, Cramer KM. Factor structure and reliability of the childhood trauma questionnaire in a canadian undergraduate student sample. Child Abuse & Neglect. 2004;28(8):889–904. doi: 10.1016/j.chiabu.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Pittenger C, Duman RS. Stress, depression, and neuroplasticity: A convergence of mechanisms. Neuropsychopharmacology. 2008;33:88–109. doi: 10.1038/sj.npp.1301574. [DOI] [PubMed] [Google Scholar]
- Porter C, Lawson JS, Bigler ED. Neurobehavioral sequelae of child sexual abuse. Child Neuropsychology. 2005;11:203–220. doi: 10.1080/092970490911379. [DOI] [PubMed] [Google Scholar]
- Prasad MR, Kramer LA, Ewing-Cobbs L. Cognitive and neuroimaging findings in physically abused preschoolers. Archive of Disease in Childhood. 2005;90:82–85. doi: 10.1136/adc.2003.045583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS. Version 9.1. Cary, NC: SAS Institute, Inc; 2004. [Google Scholar]
- Scher CD, Stein MB, Asmundson GJG, McCreary DR, Forde DR. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14(4):843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Schoeman R, Carey P, Seedat S. Trauma and posttraumatic stress disorder in South African adolescents: A case-control study of cognitive deficits. The Journal of Nervous and Mental Disease. 2009;197(4):244–250. doi: 10.1097/NMD.0b013e31819d9533. [DOI] [PubMed] [Google Scholar]
- Stein MB, Kennedy CM, Twamley EW. Biological Psychiatry. 2002;52:1079–1088. doi: 10.1016/s0006-3223(02)01414-2. [DOI] [PubMed] [Google Scholar]
- Sutker PB, Moan CE, Allain AN. Assessment of cognitive control in psychopathic and normal prisoners. Journal of Behavioral Assessment. 1983;5(4):275–286. [Google Scholar]
- Twamley EW, Hami S, Stein MB. Neuropsychological function in college students with and without posttraumatic stress disorder. Psychiatry Research. 2004;126:265–274. doi: 10.1016/j.psychres.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Weiss EL, Longhurst JG, Mazure CM. Childhood sexual abuse as a risk factor for depression in women: Psychosocial and neurobiological correlates. American Journal of Psychiatry. 1999;156(6):816–828. doi: 10.1176/ajp.156.6.816. [DOI] [PubMed] [Google Scholar]
- Welsh MC, Pennington BF, Groisser DB. A normative-developmental study of executive functions: A window on prefrontal function in children. Developmental Neuropsychology. 1991;7(2):131–149. [Google Scholar]
- Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. American Journal of Psychiatry. 1999;156(8):1223–1229. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Scott K, Wekerle C, Pittman A. Child maltreatment: Risk of adjustment problems and dating violence in adolescence. Journal of American Academy of Child and Adolescent Psychiatry. 2001;40(3):282–289. doi: 10.1097/00004583-200103000-00007. [DOI] [PubMed] [Google Scholar]


