Abstract
Background
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the gold standard surgical treatment for chronic ulcerative colitis. More recently, this procedure is being performed laparoscopically assisted. Postoperatively, small bowel obstruction (SBO) is one of the more common associated complications. However, it is unknown whether the addition of a laparoscopic approach has changed this risk. This study aims to assess and compare the incidence of SBOs after both open and laparoscopic restorative proctocolectomy.
Methods
All subjects who underwent restorative proctocolectomy from 1998–2008 were identified from a prospective Colorectal Surgery Database. Medical records were reviewed for all cases of SBO, confirmed by a combination of clinical symptoms and radiologic evidence. Comparisons were made between laparoscopic and open approaches. The incidence of SBO was also subdivided into pre-ileostomy takedown, early post-ileostomy takedown (30 d post), and late post-ileostomy takedown (30 d to 1 y post). Several potential risk factors were also evaluated. Statistical analysis was performed utilizing Fisher’s exact (for incidence) or t-tests (for means). Significance was defined as P < 0.05
Results
A total of 290 open cases and 100 laparoscopic cases were identified during this time period. The overall incidence of SBO at 1 y post-ileostomy takedown was 14% (n = 42) in the open group and 16% (n = 16) laparoscopic (P = NS). In the pre-ileostomy takedown period the incidence of SBO was 7% (n = 21) open and 13% (n = 13) laparoscopic (P = NS). While in the post-takedown period, the early incidence was 4% (n = 12) open and 1% (n = 1) laparoscopic and late incidence was 3% (n = 9) open and 2% (n = 2) laparoscopic (P = NS). Factors associated with an increased risk of SBO include coronary artery disease, prior appendectomy and W and J pouch configurations.
Conclusions
The burden of postoperative small bowel obstruction after restorative proctocolectomy is not changed with a laparoscopic approach. Most cases occur in the early postoperative period, especially prior to ileostomy reversal.
Keywords: proctocolectomy, IPAA, ileal pouch, small bowel obstruction
INTRODUCTION
Ulcerative colitis is a chronic inflammatory disease affecting the colon and rectum. Surgery is necessary when chronic ulcerative colitis is not effectively controlled with medication or under conditions of massive bleeding, dysplasia, or toxic colitis [1]. While there are a few options for surgery, the most widely accepted treatment is total proctocolectomy with ileal pouchanal anastomosis (IPAA). In most cases, a two-staged approach is utilized along with a temporary diverting loop ileostomy [2, 3]. However, in cases of toxic colitis or poor patient health status, a three-staged approach may be indicated. In any event, both approaches eventually lead to ileostomy reversal upon successful ileal pouch construction.
One of the most common postoperative complications after restorative proctocolectomy is small bowel obstruction (SBO) [1]. Various studies have determined that the incidence of SBO following restorative proctocolectomy ranges from 13% to 35% [3–6]. However, most of these have been evaluated after an open surgical approach and it is unclear what effect a laparoscopic technique may have on the incidence of SBO. A recent case-matched study from the Cleveland Clinic suggests that the incidence of SBO may be similar between open and laparoscopic approaches, both short- and long-term, though few others have made similar comparisons [7]. Similarly, Fraser et al. suggested that the incidence of SBO has not been changed by the introduction of a laparoscopic approach [8].
Though total proctocolectomy with IPAA has historically been approached in an open fashion, a number of more recent publications have demonstrated the efficacy of approaching this procedure with a laparoscopic assisted technique [9–11]. Many of these authors demonstrate short-term advantages of the laparoscopic approach including enhanced recovery and cosmetic appeal [9–13]. Recent evidence also suggests that a laparoscopic procedure may reduce the incidence of abdominal and pelvic adhesions, which are responsible for more than 75% of the small bowel obstructions following this procedure [14, 15]. It would seem that by allowing less adhesion formation via a laparoscopic technique, a lower incidence of SBO might result.
Therefore, the aim of this study is to determine whether the incidence of small bowel obstruction following a laparoscopic approach is different than that for the open approach. This project also aims to identify pertinent risk factors related to small bowel obstruction following both open and laparoscopic approaches.
MATERIALS AND METHODS
This study was designed as a retrospective analysis and was approved by the University of Wisconsin-Madison Health Sciences Institutional Review Board. All subjects with a diagnosis of ulcerative colitis who underwent total colectomy with IPAA at the University of Wisconsin from 1998 to 2008 were identified from a prospective Colorectal Surgery Database. Both the laparoscopic and open approaches were performed by four surgeons. The laparoscopic assisted approach to this procedure was introduced in 2003. This entailed a pure laparoscopic (without the use of a hand port) approach to colectomy with a small suprapubic incision utilized for proctectomy and ileal-pouch construction. Medical records (electronic or paper) were reviewed to track all cases of SBO and to identify potential associated risk factors. Follow-up time or date of last contact was also recorded.
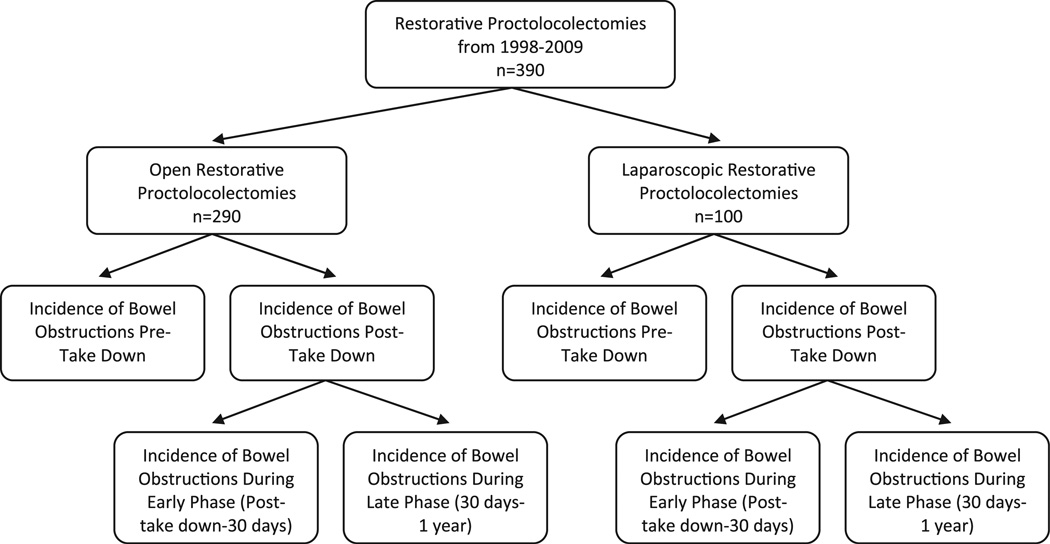
The primary end point of this study was the incidence of small bowel obstruction. This was defined as the combination of both clinical symptoms (failure to pass flatus or stool, bloating, nausea, emesis) and radiologic evidence (abdominal X-ray or abdomen/pelvis CT scan). The small bowel obstructions were then sub-categorized into pre-ileostomy takedown, early post-ileostomy takedown (30 d post) and late post-ileostomy takedown (30 d to 1 y post takedown) (Fig. 1). The severity of the SBO was further classified based on whether it was operative or nonoperative and whether the patient had developed multiple SBOs. For those SBOs that required operation, the reason for the SBO was also recorded.
FIG. 1.
Flow chart representing time periods and sample groups studied.
A number of patient demographic variables were analyzed, including age at initial surgery, gender, BMI, ASA score at time of initial surgery, past medical history factors, including COPD/asthma, diabetes, hypertension (HTN), coronary artery disease (CAD), prior abdominal surgery [including prior colectomy (subtotal or total), appendectomy, cholecystectomy, or gynecologic surgery], and medication use at time of initial surgery (including anti-inflammatory medications or immunomodulators).
Similarly, a number of perioperative factors were also recorded including length of initial hospital stay, time to ileostomy takedown, preoperative hemoglobin level, operative time, estimated blood loss, transfusion requirements, ileal pouch configuration, and use of an adhesion prevention barrier (Seprafilm; Genzyme, Cambridge, MA) as stated in the operative record.
Statistical Analysis
Univariate analysis was performed to detect differences between groups and identify factors correlating with risks of small bowel obstruction. P values were calculated with t-tests, Chi-Square, or Fisher’s exact test where appropriate. Significance was defined as P ≤ 0.05. Multivariable logistic regression was used to further evaluate differences between laparoscopic and open groups after adjusting for other factors.
RESULTS
Overall, there were 290 patients that underwent open restorative proctocolectomy and 100 patients that had laparoscopic assisted restorative proctocolectomy during the specified time period. A comparison of patient demographics between laparoscopic and open groups can be seen in Table 1. In addition, a comparison of perioperative variables between laparoscopic and open groups can be seen in Table 2. Mean follow-up time after takedown was 44 mo (range 0–145 mo) for the open group and 26 mo (range 1–76 mo) for the laparoscopic group.
TABLE 1.
Demographic Data
| Open restorative proctocolectomy (n = 290) |
Laparoscopic restorative proctocolectomy (n = 100) |
P value | |
|---|---|---|---|
| Age (y, mean ± SD) | 38.7 ± 13.6 | 37.5 ± 13.7 | NS |
| Female (%)/male (%) | 119 (41%)/171 (59%) | 54 (54%)/46 (46%) | 0.03 |
| BMI (kg/m2, mean ± SD) | 26.3 ± 5.1 | 24.2 ± 4.4 | <0.001 |
| Operative data | |||
| ASA score* | 0.01* | ||
| 1 (%) | 20 (7%) | 2 (2%) | |
| 2 (%) | 233 (83%) | 91 (95%) | |
| 3 (%) | 26 (10%) | 3 (3%) | |
| Hgb (g/dL, mean ± SD) | 12.8 ± 2.1 | 12.7 ± 2.1 | NS |
| Past medical history | |||
| COPD/asthma (%) | 16 (6%) | 4 (4%) | NS |
| Diabetes (%) | 16 (6%) | 7 (7%) | NS |
| HTN (%) | 27 (9%) | 9 (9%) | NS |
| CAD (%) | 9 (3%) | 1 (1%) | NS |
| Surgical history | |||
| Any prior abdominal surgery | 104 (36%) | 24 (24%) | 0.04 |
| Prior colectomy (total or subtotal) (%) | 34 (12%) | 2 (2%) | 0.002 |
| Prior appendectomy (%) | 8 (3%) | 6 (6%) | NS |
| Prior cholecystectomy (%) | 8 (3%) | 6 (6%) | NS |
| Any prior gynecological surgery (%) | 34 (12%) | 9 (9%) | NS |
| Prior C-section (%) | 20 (7%) | 7 (7%) | NS |
| Perioperative medication use | |||
| Steroids (%) | 180 (62%) | 60 (60%) | NS |
| 5-ASA meds (%) | 182 (63%) | 58 (58%) | NS |
| Other immunomodulators (%) | 29 (10%) | 10 (10%) | NS |
TABLE 2.
Perioperative Variables
| Open restorative proctocolectomy (n = 290) |
Laparoscopic restorative proctocolectomy (n = 100) |
P value | |
|---|---|---|---|
| Operation time (min, mean ± SD) | 346 ± 73 | 434 ± 73 | <0.001 |
| Estimated blood loss (mL, mean ± SD) | 310 ± 194 | 285 ± 202 | NS |
| Transfusion* | NS* | ||
| None | 265 (91%) | 94 (94%) | |
| 1 unit (%) | 22 (8%) | 6 (6%) | |
| 2 units (%) | 3 (1%) | 0 (0%) | |
| Pouch configuration* | <0.001* | ||
| S (%) | 255 (88%) | 92 (92%) | |
| W (%) | 30 (10%) | 0 (0%) | |
| J (%) | 5 (2%) | 8 (8%) | |
| Seprafilm use (%) | 229 (79%) | 64 (64%) | 0.005 |
| Elective (%)/urgent (%) | 280 (97%)/10 (3%) | 98 (98%)/2 (2%) | NS |
| Postoperative stay (d, mean ± SD) | 7.4 ± 3.5 | 6.4 ± 3.3 | 0.007 |
| Time to takedown (d, mean ± SD) | 108 ± 71 | 89 ± 44 | 0.002 |
These three P values were calculated at the same time using a 2 × 3 table and Fisher’s exact test.
The overall incidence of SBO with the above mean follow-up times were 22% (n = 64) and 21% (n = 21) in the open and laparoscopic groups respectively (P = NS). The incidence at 1 y post-ileostomy takedown was 14% (n = 42) in the open group and 16% (n = 16) laparoscopic (P = NS). In the pre-ileostomy takedown period the incidence of SBO was 7% (n = 21) open and 13% (n = 13) laparoscopic (P = NS). While in the post-takedown period, the early incidence was 4% (n = 12) open and 1% (n = 1) laparoscopic, and late incidence was 3% (n = 9) open and 2% (n = 2) laparoscopic (P = NS).
The incidence of SBO requiring operative intervention at one year was 7% (n = 19) in the open group and 6% (n = 6) in the laparoscopic group (P = NS) (Table 3). In the pre-ileostomy takedown period the incidence of operative SBO was 7% (n = 4) open and 5% (n = 5) laparoscopic (P = NS). While in the post-takedown period, the early operative incidence was 1% (n = 3) open and 1% (n = 1) laparoscopic, and late incidence was 2% (n = 6) open and 0% (n = 0) laparoscopic (P = NS). The incidence of recurrent SBOs was 2% (n = 6) in the open group and 5% (n = 5) in the laparoscopic group (P = NS).
TABLE 3.
Incidence and Timing of SBOs for Open and Laparoscopic Assisted Procedures
| No SBO (%) | SBO at 1 year post-takedown |
SBO pre- takedown |
SBO early post-takedown |
SBO late post-takedown |
Operative SBO |
Recurrent SBO |
|
|---|---|---|---|---|---|---|---|
| Open (n = 290) | 248 (86%) | 42 (14%) | 21 (7%) | 12 (4%) | 9 (3%) | 19 (7%) | 6 (2%) |
| Laparoscopic (n = 100) | 84 (84%) | 16 (16%) | 13 (13%) | 1 (1%) | 2 (2%) | 6 (6%) | 5 (5%) |
| P value | N/A | NS | 0.17* | 0.17* | 0.17* | NS | NS |
These three P values were calculated at the same time using a 2 × 3 table and Fisher’s exact test.
Upon further evaluation of SBOs requiring operative intervention, 74% (n = 14) of the open cases were directly attributed to adhesions compared with 33% (n = 2) of the laparoscopic cases (P = NS). In the pre-takedown period, the cause of operative SBO was less likely to be adhesions, causative in 50% (n = 5) for the open group and only 20% (n = 1) in the laparoscopic group (P = NS). In the post-takedown period, the only cause of SBO was adhesions in both the open (n = 9) and laparoscopic (n = 1) groups (P = NS). Other operative findings responsible for SBO included: kinking, herniation, and volvulus around the ileostomy as stated in the operative records.
Though a number of factors were recorded, only a history of CAD, prior appendectomy, and pouch configuration (with SBO more likely associated with W and J pouches versus S pouches), appeared to be significantly associated with the development of SBO when both open and laparoscopic approaches are combined for univariate analysis (Table 4). In our multivariate analysis, the assessed risk factors were similar; however, prior appendectomy was no longer found to be a significant risk factor (OR = 3.8 [1.0–14.8]; P = 0.06). Furthermore, multivariate analysis confirmed that surgical approach (laparoscopic and open) was not a predictor for SBO (OR = 1.0 [0.4–2.4]) (Table 5). When assessing both the laparoscopic and open groups separately and further analyzing these factors, pouch configuration is the only consistent factor in both groups, with SBO continuing to be more likely associated with W and J pouches. Meanwhile, a past medical history of CAD remains the only other statistically significant factor in the open group.
TABLE 4.
Univariate Evaluation of Potential Risk Fators for SBO After Combining Open and Laparoscopic Groups
| No SBO (n = 332) | SBO within 1 y post-takedown (n = 58) | P value | |
|---|---|---|---|
| Age (y, mean ± SD) | 38.7 ± 13.4 | 36.6 ± 14.8 | NS |
| Female (%)/male (%) | 143 (43%)/189 (57%) | 30 (52%)/28 (48%) | NS |
| BMI (kg/m2, mean ± SD) | 25.9 ± 4.8 | 25.1 ± 5.8 | NS |
| Operative data | |||
| ASA score | |||
| 1 (%) | 17 (5%) | 5 (9%) | NS* |
| 2 (%) | 279 (84%) | 45 (78%) | |
| 3(%) | 24 (7%) | 7 (12%) | |
| HgB (g/dL, mean ± SD) | 12.8 ± 2.1 | 12.8 ± 1.9 | NS |
| Past medical history | |||
| COPD/asthma (%) | 18 (5%) | 2 (3%) | NS |
| Diabetes (%) | 20 (6%) | 3 (5%) | NS |
| HTN (%) | 32 (10%) | 4 (7%) | NS |
| CAD (%) | 6 (2%) | 4 (7%) | 0.05 |
| Surgical history | |||
| Any prior abdominal surgery (%) | 107 (32%) | 21 (36%) | NS |
| Prior colectomy (total or subtotal) (%) | 31 (9%) | 5 (9%) | NS |
| Prior appendectomy (%) | 8 (2%) | 6 (10%) | 0.001 |
| Prior cholecystectomy (%) | 10 (3%) | 4 (7%) | NS |
| Any prior gynecologic surgery (%) | 36 (11%) | 7 (12%) | NS |
| Prior C-section (%) | 23 (7%) | 4 (7%) | NS |
| Perioperative medication use | |||
| Steroids (%) | 200 (60%) | 40 (69%) | NS |
| 5-ASA meds (%) | 202 (61%) | 38 (66%) | NS |
| Other immunomodulators (%) | 36 (11%) | 3 (5%) | NS |
| Operation time (min, mean ± SD) | 367 ± 83 | 363 ± 78 | NS |
| Estimated blood loss (mL, mean ± SD) | 305 ± 198 | 296 ± 185 | NS* |
| Transfusions* | |||
| None (%) | 305 (92%) | 54 (93%) | |
| 1 unit (%) | 24 (7%) | 4 (7%) | |
| 2 units (%)) | 3 (1%) | 0 (0%) | |
| Pouch type* | <0.001* | ||
| S (%) | 304 (92%) | 43 (74%) | |
| W (%) | 21 (6%) | 9 (16%) | |
| J (%) | 7 (2%) | 6 (10%) | |
| Seprafilm use (%) | 254 (77%) | 39 (67%) | NS |
| Elective (%)/urgent (%) | 323 (97%)/9 (3%) | 55 (95%)/3 (5%) | NS |
These three P values were calculated at the same time using a 2 × 3 table and Fisher’s exact test.
TABLE 5.
Multivariate Analysis of Potential Risk Factors for SBO
| Odds ratio (OR) | 95% Confidence limits | P value | |
|---|---|---|---|
| Surgical approach: | |||
| Open | Referent | Referent | Referent |
| Laparoscopic | 1.0 | 0.4–2.4 | NS |
| Gender: | |||
| Male | Referent | Referent | Referent |
| Female | 1.5 | 0.8–2.9 | NS |
| BMI | 1.0 | 0.9–1.0 | NS |
| ASA score | 1.0 | 0.4–2.3 | NS |
| Past medical history: | |||
| Any prior abdominal surgery | 1.5 | 0.6–3.6 | NS |
| Prior colectomy (total or subtotal) | 0.5 | 0.1–2.0 | NS |
| Prior appendectomy | 3.8 | 1.0–14.8 | 0.06 |
| CAD | 6.9 | 1.5–31.9 | 0.01 |
| Seprafilm use | 1.0 | 0.5–1.9 | NS |
| Pouch type: | |||
| J | Referent | Referent | Referent |
| S | 0.2 | 0.05–0.8 | 0.02 |
| W | 0.4 | 0.1–2.4 | NS |
| OR time | 1.0 | 1.0–1.0 | NS |
Immunosuppressive medications (including steroids) at the time of initial surgery did not influence the incidence of SBO (P = NS). In addition, the use of the adhesion prevention barrier, Seprafilm (Genzyme) did not seem to influence the likelihood of SBO though its use was confirmed in only 75% (n = 293) of cases as stated in the operative record (P = 0.14).
DISCUSSION
The results of this study confirm that SBO remains one of the more common postoperative complications associated with restorative proctocolectomy. The overall incidence at 1 y of 14% in the open and 16% in the laparoscopic groups remains high and is a significant burden worthy of discussion with patients undergoing this procedure. Despite the presumed advantage that a laparoscopic approach may decrease the inflammatory response and theoretically lead to less adhesion formation, we noted no statistically significant differences between the timing and severity of SBO between the open and laparoscopic groups. This may be due to the fact that in almost all of these laparoscopic cases, the pelvic portion of the procedure (proctectomy and IPAA) is still performed via a small suprapubic incision and thereby still inciting the usual inflammatory response. However, after breaking down our population into early and late presentations, as well as pre- and post-ileostomy reversal, there was a slight trend toward the majority of laparoscopic-related SBOs presenting in the pre-takedown period. Though the reason for this is unclear, it would seem that in this early period adhesion formation is less likely to be responsible for bowel obstruction and other causes are accountable (i.e., mechanical). Few other groups have similarly compared the incidence of SBO between laparoscopic and open approaches. However, one such group from the Cleveland Clinic revealed similar findings to the current study [7]. They noted a similar incidence of SBO between open and laparoscopic approaches at 30 d (open, 4% and laparoscopic, 6%), 1 y (open, 13% and laparoscopic, 20%), and 5 y (open, 16% and laparoscopic, 21%) (P = NS) [7].
Although not the impetus of this study, comparisons of the laparoscopic and open groups again confirmed one of the benefits of the laparoscopic approach, namely, that the length of hospital stay is shortened. We and others have previously demonstrated this advantage of a laparoscopic over open approach for restorative proctocolectomy, though operative times are consistently longer [9, 10]. In addition, since laparoscopy has also been shown to have a beneficial effect on adhesion formation [14, 15], it would seem that by utilizing this approach for restorative proctocolectomy, a decrease in the incidence of SBO might be seen. However, this was not apparent in the current study. Despite these findings, we also noted that the time period from original surgery to ileostomy reversal was decreased in the laparoscopic group. Though this may be partially explained by a few instances where early required reoperation in this group resulted in earlier reversal, this finding likely represents the assumption of less adhesion formation after laparoscopy and, therefore, an offering of earlier ileostomy reversal.
In our review, we noted that adhesions were causative in cases of SBO requiring operative intervention in 74% of the open cases compared with only 33% laparoscopic. While this finding was not found statistically significant, it does parallel prior research, noting again that laparoscopy is associated with a reduction in adhesion formation [14, 15]. With this in mind, it might confirm that in the laparoscopic pre-ileostomy takedown period, the small bowel remains freely mobile as a result of fewer adhesions and is potentially more prone to mechanical kinking or twisting, especially at the ileostomy site. Unfortunately, we have been unable to identify any technical factors that may be responsible for these findings and it does not appear that ileostomy orientation plays a role. This contrasts with the open group, which demonstrates a more evenly distributed time course for SBO and more SBOs caused by adhesions. It, therefore, seems possible that over a longer time period, the laparoscopic group might reveal a lower incidence of SBO, since adhesions during that time would likely be responsible. While the incidence of SBO did increase over the course of patient follow-up in the open compared with the laparoscopic group, no significant differences were noted and, due to the short term follow-up in this study (especially in the laparoscopic group), this trend cannot be confirmed at present. Longer term evaluation is necessary to investigate this possibility further.
Although this is a large series of both open and laparoscopic cases, we recognize the limitations of a retrospective review and it may therefore be difficult to make reliable conclusions with the number of predictor variables examined. In addition, we recognize the possibility of losing some patients to follow-up, as they could potentially seek care for a SBO elsewhere. Examination of the demographic data does reveal some differences between the laparoscopic and open groups. We noted that the laparoscopic group demonstrated an increased female population, lower BMIs, lower ASA scores, and, as expected, significantly fewer patients with prior colectomy or any other prior abdominal surgery. These differences are likely attributed to careful patient selection in the laparoscopic group, especially in the earlier period of utilizing this approach. However, even when these findings are corrected for with logistic regression, laparoscopic patients failed to demonstrate significant differences in the incidence or severity of SBO.
The similar incidence of SBO between the laparoscopic and open groups led to an evaluation of multiple factors in an attempt to identify those contributing to an increased risk. Of these factors, only CAD, prior appendectomy, and pouch configuration were associated with an increased risk of SBO, though prior appendectomy was not significant when adjusting in a multivariate model. In our study, use of the S pouch configuration was by far the most common and demonstrated the lowest associated incidence of SBO, while the W and J pouches revealed an increased SBO risk. Since our study group was made up of only a small number of W and J pouch configurations, further study is necessary to determine if this finding holds true. Aside from this, evaluation also revealed that CAD was associated with an increased risk of SBO. A link between CAD and SBO seems unlikely and is difficult to explain, though again a small sample size may be responsible. Although it is possible that prior appendectomy (from the univariate analysis) could contribute an increased risk for the development of SBO, an evaluation of other prior abdominal surgeries failed to reveal similar results. In addition, we have shown that even in cases where a three-staged procedure with prior colectomy was utilized, there was no increase in the incidence of SBO. Finally, we also identified cases from the operative record, utilizing an adhesion prevention barrier. However, we found that no beneficial effect with respect to SBO was demonstrated. This is similar to an earlier prospective trial failing to show prevention in the rate of SBO with use of Seprafilm (Genzyme) [16].
In summary, the burden of postoperative small bowel obstruction after restorative proctocolectomy is not changed with a laparoscopic approach. Most cases tend to occur in the early postoperative period, especially prior to ileostomy reversal.
ACKNOWLEDGMENT
The authors thank Glen Leverson, Ph.D. for his statistical assistance in this project.
REFERENCES
- 1.Bach S, Mortensen N. Ileal pouch surgery for ulcerative colitis. World J Gastroenterol. 2007;13:3288. doi: 10.3748/wjg.v13.i24.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ. 1978;2:85. doi: 10.1136/bmj.2.6130.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomosis complications and function in 1005 patients. Ann Surg. 1995;222:120. doi: 10.1097/00000658-199508000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacLean AR, Cohen Z, MacRee HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg. 2002;235:200. doi: 10.1097/00000658-200202000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Young CJ, Solomon MJ, Eyers AA, et al. Evolution of the pelvic pouch procedure at one institution: The first 100 cases. Aust NZ J Surg. 1999;69:438. doi: 10.1046/j.1440-1622.1999.01552.x. [DOI] [PubMed] [Google Scholar]
- 6.Marcello PW, Roberts PL, Schoetz DJ, Jr, et al. Obstruction after ileal pouch-anal anastomosis: A preventable complication? Dis Colon Rectum. 1993;36:1105. doi: 10.1007/BF02052257. [DOI] [PubMed] [Google Scholar]
- 7.El-Gazzaz G, Kiran R, Remzi F, et al. Outcomes for case-matched laparoscopically assisted versus open restorative proctocolectomy. British J of Surg. 2009;96:522. doi: 10.1002/bjs.6578. [DOI] [PubMed] [Google Scholar]
- 8.Fraser J, Garey C, Laituri C, et al. Outcomes of laparoscopic and open total colectomy in the pediatric population. J. Laproendosc Adv Surg Tech A. 2010;20:659. doi: 10.1089/lap.2010.0086. [DOI] [PubMed] [Google Scholar]
- 9.Larson D, Cima R, Dozois E, et al. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch–anal anastomosis: A single institutional case-matched experience. Ann Surg. 2006;243:670. doi: 10.1097/01.sla.0000216762.83407.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heise CP, Kenedy G, Foley EF, et al. Laparoscopic restorative proctocolectomy with ileal S-pouch. Dis Colon Rectum. 2008;51:1790. doi: 10.1007/s10350-008-9408-z. [DOI] [PubMed] [Google Scholar]
- 11.Fichera A, Silvestri MT, Hurst RD, et al. Laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis: A comparative observational study on long-term functional results. J Gastrointest Surg. 2009;13:526. doi: 10.1007/s11605-008-0755-9. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed AU, Keus F, Heikens JT, et al. Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis (Review) The Chochrane Library. 2009;1:1. doi: 10.1002/14651858.CD006267.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Ferrante M, Declerck S, De Hertogh G, et al. Outcome after proctolocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. Inflamm Bowel Dis. 2008;14:20. doi: 10.1002/ibd.20278. [DOI] [PubMed] [Google Scholar]
- 14.Indar AA, Efron JE, Young-Fadok TM. Laparoscopic ileal pouchanal anastomosis reduces abdominal and pelvic adhesions. Surg Endosc. 2009;23:174. doi: 10.1007/s00464-008-0139-y. [DOI] [PubMed] [Google Scholar]
- 15.Cox MR, Gunn IF, Eastman MC, et al. The operative etiology and types of adhesions causing small bowel obstruction. Aust N Z J Surg. 1993;63:848. doi: 10.1111/j.1445-2197.1993.tb00358.x. [DOI] [PubMed] [Google Scholar]
- 16.Fazio VW, Cohen Z, Fleshman JW, et al. Reduction in adhesive small-bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006;49:1. doi: 10.1007/s10350-005-0268-5. [DOI] [PubMed] [Google Scholar]