Abstract
Background
Congenital heart disease consumes significant health care resources; however, there are limited data regarding factors impacting resource utilization. The purpose of this study was to evaluate variation between centers in total hospital costs for four congenital heart operations of varying complexity, and associated factors.
Methods and Results
The Premier Database was used to evaluate total cost in children undergoing isolated atrial septal defect (ASD) repair, ventricular septal defect (VSD) repair, tetralogy of Fallot (TOF) repair, or arterial switch operation (ASO) from 2001-2007. Mixed models were used to evaluate the impact of center on total hospital costs adjusting for patient and center characteristics and length of stay (LOS).
A total of 2,124 patients were included: 719 ASD (19 centers), 792 VSD (20 centers), 420 TOF (17 centers), and 193 ASO (13 centers). Total cost increased with complexity of operation from median $12,761 (ASD repair) to $55,430 (ASO). In multivariable analysis, models which accounted for center effects vs. those which did not performed significantly better for all four surgeries (all p ≤ 0.01). The proportion of total cost variation explained by center was 19% (ASD repair), 11% (VSD repair), 6% (TOF repair), and 3% (ASO). Higher volume centers had significantly lower hospital costs for ASD and VSD repair, but not for TOF repair and ASO.
Conclusions
Total hospital costs varied significantly by center for all congenital heart surgeries evaluated, even after adjustment for patient and center characteristics and LOS. Differences among centers were most prominent for lower complexity procedures.
Keywords: heart defects, congenital, cost
Introduction
Congenital heart disease causes an enormous health burden impacting nearly 1% of live births, and accounting for significant resource utilization with an estimated 6 billion dollars annually in acute care costs alone (1). It has been reported that of all birth defects, congenital heart defects are associated with the highest average hospital charges, length of stay, and mortality (2). In spite of this, few studies have evaluated factors impacting resource utilization in patients undergoing congenital heart surgery (3-7).
Analyses to date have been limited by the use of hospital charge data (which reflect the amount the hospital billed for services rather than actual cost), and analyzing surgeries of varying levels of complexity together (3-7). This makes it difficult to discern patient and center factors associated with higher hospital costs as the driving factor in most cases is the complexity of the procedure being performed. In addition, many studies to date have focused on patients undergoing congenital heart surgery from a single center, so that there are limited data regarding differences in resource utilization between centers (5,6). If differences in resource utilization between centers do exist, this would support further evaluation of factors mediating these differences to facilitate development of initiatives aimed at cost reduction, which is of particular importance in this era of rising health care costs. Thus, the purpose of this study was to evaluate variation between centers in total hospital costs for four congenital heart operations of varying levels of complexity, and to identify factors associated with increased hospital costs for each surgery.
Methods
Data Source
The Premier Database (Premier, Inc., Charlotte, North Carolina) is an inpatient administrative database including more than 500 US hospitals with on average more than 5 million hospital discharges per year. The database includes a wide range of hospitals with diverse characteristics in regard to geographic region, number of beds, population served, and teaching status. Both pediatric and adult data are collected. Data from both freestanding and non-freestanding children’s hospitals are included in the pediatric data. Data collected include diagnoses and procedures [using International Classification of Diseases, Ninth Revision, (ICD-9) coding], demographic information, resource utilization (including total hospital costs), length of hospital stay, and in-hospital mortality. Hospital characteristics are also collected. All data received from hospitals are validated against Premier standards, and any deviations are corrected by the participating hospitals. The Premier Database has been widely used in previous health outcomes and health economics studies (8,9).
Study Population
Patients 0–18 years of age undergoing congenital heart surgery from 2001-2007 at a Premier center were eligible for inclusion. As previously described, Risk Adjustment in Congenital Heart Surgery, version 1 (RACHS-1) methodology was used to identify patients undergoing four surgeries of varying levels of complexity: secundum atrial septal defect repair, ventricular septal defect repair, tetralogy of Fallot repair (excludes tetralogy of Fallot with pulmonary atresia), and the arterial switch operation for transposition of the great arteries (3,10). Only patients undergoing these procedures in isolation were included and those undergoing other concurrent cardiac surgical procedures were excluded. The complexity of the four included procedures as assessed by the Aristotle Basic Complexity Score ranged from 3 for atrial septal defect repair, 6 for ventricular septal defect repair, 8 for tetralogy of Fallot repair, to 10 for the arterial switch operation (11). Centers with less than five cases during the study period for a specific procedure were excluded from analysis of that procedure. Only survivors to hospital discharge were included in the analysis. This study was approved by the Duke Institutional Review Board with a waiver of informed consent.
Data Collection
Data collection included patient age (captured in years), sex, race/ethnicity, prematurity/low birth weight (neonates only), presence of genetic syndrome or major non-cardiac abnormality, and payor (private, government, other) as previously described (10,12). Center characteristics included center region, location (urban vs. rural), teaching hospital status, and children’s hospital status (freestanding vs. non-freestanding). Center average annual volume over the study period for the procedure of interest was also calculated.
Outcome
The primary outcome was total hospital cost. The Premier Database collects data directly from the cost accounting systems at participating hospitals. In the Premier Database, total hospital costs include direct or variable costs (including direct costs for in-hospital services such as procedures, room and board, professional fees for services performed by hospital staff, and pharmacy costs) and overhead or fixed costs for in-hospital services during the stay. Premier also maps individual costs to a standardized list of cost elements (e.g. room and board, pharmacy, laboratory, etc) for each participating center. Physician professional fees are not captured by the Premier Database. Given that the study period included several years of data (2001-2007), all cost figures were discounted to 2001 dollars.
Analysis
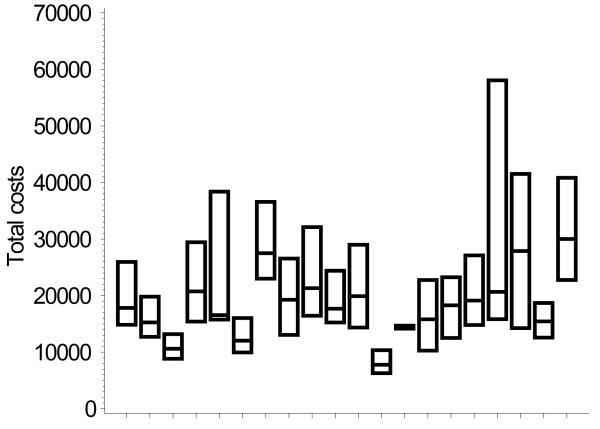
Patient and center characteristics, and total hospital costs for each of the four surgeries were summarized as median and interquartile range for continuous variables and frequencies and percentages for categorical variables. Total hospital costs for each center included in the analysis were also graphed by box and whisker plot for each of the four procedures.
To evaluate the impact of individual center on total hospital costs and the contribution of various patient and center factors, mixed models were used. Total cost was log transformed for analysis, due to the skewed distribution of cost data. Six random effect models were developed for each operation and compared to assess model performance with the inclusion of various patient and center factors. Model 1 included center as the only random effect and was not adjusted for other factors. Models 2-5 all included center as a random effect, and adjusted for various other factors as fixed effects. Model 2 included patient factors as fixed effects (age, gender, race, genetic syndrome, major non-cardiac abnormality, low birth weight, and insurance status); Model 3 included patient factors (as noted above) and length of stay as fixed effects; Model 4 included center factors only (children’s hospital status, urban vs. rural location, teaching status, region of country, and center volume for procedure of interest) as fixed effects; and Model 5 included all factors as fixed effects (patient factors, center factors, and length of stay). The sixth and final model included all patient factors, center factors and length of stay as fixed effects, but removed the random effect of center. This was done to evaluate the impact of center, accounting for all other patient and center factors. Models were compared using likelihood ratio testing and Akaike’s information criterion (AIC), with smaller AIC representing a better model (13). The proportion of total cost variation explained by the random center effect was also calculated for each model. Parameter estimates and standard errors are reported for center factors from Model 5 (which adjusts for patient factors and length of stay), to assess the independent association of various center factors with total costs. Estimates from this model of log cost were transformed back to actual cost, using the smearing estimate,
Finally, the cost savings per patient if all centers were to perform as well as the lowest cost quartile were estimated from the mixed models (Model 5) for each surgery. The estimated cost for each patient was calculated by transforming log cost to cost using the smearing estimate. Then, while the fixed effects were kept constant, the hospital effect was replaced with the average hospital effect of the lowest cost quartile, and estimated cost per patient recalculated. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC). A p-value < 0.05 was considered statistically significant.
Results
A total of 2,124 survivors to hospital discharge were included: 719 patients undergoing atrial septal defect repair (n = 19 centers), 792 patients undergoing ventricular septal defect repair (n = 20 centers), 420 patients undergoing tetralogy of Fallot repair (n = 17 centers), and 193 patients undergoing the arterial switch operation (n = 13 centers). Patient and center characteristics for each of the four surgical groups are displayed in Table 1. Of note, there was a wider range of center annual volume for the lower complexity surgeries (atrial septal defect repair, and ventricular septal defect repair), compared with the higher complexity surgeries (tetralogy of Fallot repair, and arterial switch operation).
Table 1.
Patient and Center Characteristics
| Variable | ASD Repair (n= 719) |
VSD Repair (n= 792) |
TOF Repair (n= 420) |
ASO (n= 193) |
|---|---|---|---|---|
| Median age (IQR), years | 3.0 (1.0, 6.0) | -- | -- | -- |
| Sex, female n (%) | 450 (62.6%) | 389 (49.1%) | 188 (44.8%) | 52 (26.9%) |
| Race/ethnicity | ||||
| Non-hispanic white | 434 (60.4%) | 349 (44.1%) | 222 (52.9%) | 125 (64.8%) |
| Non-hispanic black | 88 (12.2%) | 145 (18.3%) | 87 (20.7%) | 21 (10.9%) |
| Hispanic | 55 (7.6%) | 97 (12.2%) | 26 (6.2%) | 15 (7.8%) |
| Other | 142 (19.8%) | 201 (25.4%) | 85 (20.2%) | 32 (16.6%) |
| Prematurity, n (%)* | 2 (0.3%) | 1 (0.1%) | 3 (0.7%) | 12 (6.2%) |
| Low birth weight, n (%)* | 0 (0%) | 1 (0.1%) | 2 (0.5%) | 1 (0.5%) |
| Genetic syndrome, n (%) | 65 (9.0%) | 153 (19.3%) | 33 (7.9%) | 2 (1.0%) |
| Major non-cardiac abnormality, n (%) | 17 (2.4%) | 30 (3.8%) | 28 (6.7%) | 16 (8.3%) |
| Payor | ||||
| Private | 368 (51.2%) | 354 (44.7%) | 205 (48.8%) | 85 (44.0%) |
| Government | 325 (45.2%) | 405 (51.1%) | 204 (48.5%) | 94 (48.7%) |
| Other | 26 (3.6%) | 33 (4.2%) | 11 (2.6%) | 14 (7.3%) |
| Median length of stay (IQR), days | 3 (3-4) | 5 (4-8) | 8 (6-14) | 17 (14-26) |
| Center Region, n (%) | ||||
| Northeast | 77 (10.7%) | 141 (17.8%) | 55 (13.1%) | 37 (19.2%) |
| Midwest | 113 (15.7%) | 105 (13.3%) | 66 (15.7%) | 30 (15.5%) |
| West | 78 (10.8%) | 140 (17.7%) | 37 (8.8%) | 3 (6.7%) |
| South | 451 (62.7%) | 406 (51.3%) | 262 (62.4%) | 113 (58.5%) |
| Center, n (%) | ||||
| Children’s hospital | 371 (51.6%) | 294 (37.1%) | 183 (43.6%) | 86 (44.6%) |
| Teaching hospital | 462 (64.3%) | 481 (60.7%) | 248 (59.0%) | 129 (66.8%) |
| Urban location | 577 (80.3%) | 721 (91.0%) | 386 (91.9%) | 169 (87.6%) |
| Center annual volume, median (range) | 11 (1-33) | 12 (1-29) | 8 (1-20) | 5 (1-10) |
ASD = atrial septal defect, VSD = ventricular septal defect, TOF = tetralogy of Fallot, ASO = arterial switch operation, IQR = interquartile range Dashes indicate all patients in that group less than 1 year of age
neonates only
Unadjusted total hospital costs for each of the four surgeries are displayed in Table 2. As expected, total hospital costs increased with increasing complexity of operation from a median of $12,761 for atrial septal defect repair to a median of $55,430 for the arterial switch operation. For each of the 4 surgeries, room and board accounted for the largest proportion of total costs (Table 2), and the upper cost quartile had longer median length of stay compared with the lower cost quartile (atrial septal defect repair 4 days vs. 3 days, ventricular septal defect repair 6 days vs. 4 days, tetralogy of Fallot repair 12 days vs. 7 days, and arterial switch operation 22 days vs. 15 days). Box and whisker plots displaying unadjusted total hospital costs by center for each of the four surgeries are displayed in Figure 1 A–D. Of note, although only survivors to hospital discharge were included in the analysis, we also examined the mortality rate (prior to excluding those who died) by center cost quartiles for each operation. Mortality tended to be higher in the upper vs. lower cost quartile for the higher complexity operations: tetralogy of Fallot repair (5% vs. 2%) and arterial switch operation (15% vs. 1%) and similar in the upper vs. lower cost quartile for the lower complexity operations: atrial septal defect repair (1% vs. 1%) and ventricular septal defect repair (0.5% vs. 1%).
Table 2.
Unadjusted total hospital costs per patient
| Proportion of Total Hospital Costs Explained by: | ||||||
|---|---|---|---|---|---|---|
| Operation | Total Hospital Cost, median (IQR) | Room/Board | OR | Pharmacy | Supply Lab | |
| ASD repair | $ 12,761 (10,863 – 14,828) | 33% | 24% | 17% | 6% | 6% |
| VSD repair | $ 18,834 (14,155 – 27,181) | 38% | 17% | 14% | 8% | 8% |
| TOF repair | $ 28,223 (20,224 – 42,517) | 38% | 17% | 12% | 8% | 8% |
| ASO | $ 55,430 (41,874 – 81,660) | 40% | 11% | 11% | 9% | 8% |
The top 5 cost categories for each operation are listed.
ASD = atrial septal defect, VSD = ventricular septal defect, TOF = tetralogy of Fallot, ASO = arterial switch operation, IQR = interquartile range, OR = operating room
Figure 1.
Box plots displaying center variation in unadjusted total hospital costs A. ASD repair, B. VSD repair, C. TOF repair, D. ASO
Each box represents one center, middle bar represents the median, and ends of box the interquartile range.
ASD=atrial septal defect, VSD=ventricular septal defect, TOF=tetralogy of Fallot, ASO=arterial switch operation
Results from mixed models are displayed in Table 3. For all four surgeries, the proportion of total cost variation explained by center decreased as patient and center factors and length of stay were added into the models (comparing Model 1 through Model 5). Adjusting for patient and center factors and length of stay, models which accounted for center effects (Model 5) vs. those which did not (Model 6) performed significantly better for all 4 surgeries indicating that center is a significant factor impacting total hospital costs (p-value from likelihood ratio testing comparing Model 5 vs. Model 6: atrial septal defect repair p<0.0001, ventricular septal defect repair p<0.0001, tetralogy of Fallot repair p<0.0001, and arterial switch operation p=0.01). For all surgeries, AIC was also smaller for Model 5 (which included center effects) vs. Model 6, indicating better model performance. Accounting for all patient and center factors and length of stay (Model 5), the proportion of total cost variation explained by center decreased as the complexity of surgery increased: 19% for atrial septal defect repair, 11% for ventricular septal defect repair, 6% for tetralogy of Fallot repair, and 3% for arterial switch operation.
Table 3.
Model characteristics
| ASD Repair | VSD Repair | TOF Repair | ASO | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | Proportion of total cost variation explained by center |
Proportion of total cost variation explained by center |
Proportion of total cost variation explained by center |
Proportion of total cost variation explained by center |
|||||
| Random Effect |
Fixed Effects |
AIC | AIC | AIC | AIC | ||||
| (1) center | -- (unadjusted) |
913 | 0.33 | 1398 | 0.22 | 740 | 0.13 | 306 | 0.28 |
| (2) center | patient factors |
842 | 0.31 | 1267 | 0.18 | 691 | 0.12 | 307 | 0.24 |
| (3) center | patient factors + LOS |
391 | 0.25 | 884 | 0.16 | 278 | 0.10 | 102 | 0.14 |
| (4) center | center factors |
916 | 0.25 | 1403 | 0.15 | 750 | 0.08 | 310 | 0.11 |
| (5) center | patient & center factors + LOS |
388 | 0.19 | 887 | 0.11 | 286 | 0.06 | 101 | 0.03 |
| (6) -- | patient & center factors + LOS |
570 | 980 | 306 | 104 | ||||
Characteristics of 6 models evaluating total hospital cost adjusting for patient factors, center factors, length of stay, and/or center.
LOS = length of stay, AIC = Akaike’s information criterion, with smaller AIC representing a better model. ASD = atrial septal defect, VSD = ventricular septal defect, TOF = tetralogy of fallot, ASO = arterial switch operation
Adjusting for patient and center factors and LOS, the models with and without center (model 5 vs. model 6) were compared and model 5 performs significantly better than model 6 for all surgeries via likelihood ratio testing (ASD repair p<0.0001, VSD repair p<0.0001, TOF repair p<0.0001, arterial switch operation p=0.01) indicating that center is an important factor impacting total hospital cost. See text for detailed summary of table results.
The association of various center factors with adjusted total hospital costs for each of the 4 surgeries from Model 5 (which accounts for patient characteristics, length of stay, and center effects) is displayed in Table 4. Higher center volume was associated with significantly lower hospital costs. This effect was only present for lower complexity surgeries (atrial septal defect and ventricular septal defect repair). The estimated average difference in adjusted total hospital costs between the upper and lower center volume quartiles for atrial septal defect repair was $1782, and for ventricular septal defect repair $1196.
Table 4.
Center factors associated with increased adjusted total hospital cost in multivariable analysis
| ASD Repair | VSD Repair | TOF Repair | ASO | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |||
| Children’s hospital | |||||||||||||||
| Yes | 0.07 | 0.16 | 0.67 | 0.13 | 0.15 | 0.37 | 0.12 | 0.12 | 0.30 | −0.11 | 0.11 | 0.35 | |||
| No | (reference) | ||||||||||||||
| Hospital location | |||||||||||||||
| Urban | 0.20 | 0.24 | 0.39 | 0.34 | 0.21 | 0.10 | 0.10 | 0.20 | 0.62 | 0.07 | 0.14 | 0.64 | |||
| Rural | (reference) | ||||||||||||||
| Teaching hospital | |||||||||||||||
| Yes | 0.23 | 0.13 | 0.07 | 0.25 | 0.12 | 0.03 | 0.16 | 0.09 | 0.10 | 0.10 | 0.10 | 0.30 | |||
| No | (reference) | ||||||||||||||
| Center region | |||||||||||||||
| Northeast | −0.24 | 0.21 | 0.25 | −0.007 | 0.17 | 0.97 | 0.15 | 0.18 | 0.41 | −0.08 | 0.12 | 0.51 | |||
| Midwest | −0.17 | 0.17 | 0.32 | −0.10 | 0.17 | 0.55 | −0.01 | 0.14 | 0.93 | 0.43 | 0.12 | 0.001 | |||
| West | −0.01 | 0.20 | 0.95 | 0.17 | 0.18 | 0.33 | 0.05 | 0.14 | 0.75 | −0.15 | 0.16 | 0.35 | |||
| South | (reference) | ||||||||||||||
| Center volume | −0.01 | 0.002 | 0.001 | −0.008 | 0.004 | 0.03 | 0.002 | 0.006 | 0.70 | −0.01 | 0.01 | 0.24 | |||
Estimates represent adjusted log cost in dollars. See text for differences in adjusted estimates of actual cost associated with center volume in ASD and VSD repair groups.
ASD = atrial septal defect, VSD = ventricular septal defect, TOF = tetralogy of Fallot, ASO = arterial switch operation, CV = cardiovascular
Finally, the average adjusted cost savings per patient if all centers were to perform as well as the lowest cost quartile were estimated from the models for each surgery: atrial septal defect repair $3741, ventricular septal defect repair $6323, tetralogy of Fallot repair $5789, and arterial switch operation $12,846.
Discussion
In this multi-center analysis, we found that total hospital costs varied significantly by center for all four congenital heart operations evaluated. These differences persisted even after adjustment for patient characteristics and length of stay, and were most prominent for lower complexity operations.
Congenital heart defects, while relatively rare, consume a large share of health care resources (1,2). Children with congenital heart disease often require numerous hospitalizations which may include advanced surgical or interventional therapies, care by a multidisciplinary team of specialists, frequent imaging and other diagnostic testing, drug and device therapy, and life-long outpatient follow-up. Over the past several decades, survival following congenital heart surgery has improved significantly, such that evaluation of other outcomes including resource utilization, quality of life, complications, and neurodevelopmental function has now received greater attention (14). Previous studies have suggested that inpatient costs account for the majority of resource utilization in terms of direct medical costs for patients undergoing congenital heart surgery, as opposed to outpatient services (15). Similar to others, we also found that the vast majority of inpatient costs were related to room and board charges and that higher costs were associated with longer length of stay (7). Differences in length of stay are likely related to both patient pre-operative, operative, and post-operative factors as well as center-related factors.
We are not aware of previous studies evaluating variation in hospital costs between centers caring for patients undergoing congenital heart surgery. In a large study evaluating in-hospital charges in more than 10,000 patients undergoing congenital heart surgery in 2000, Connor et al demonstrated significant variation in hospital charges between the 27 different US states included in the analysis (3). Variation between centers was not evaluated. Investigators also found that, as expected, higher complexity cases were associated with increased hospital charges (3).
In the present study, we chose to perform separate analyses of four common surgeries in order to evaluate variation between institutions, and important factors impacting resource utilization, across varying levels of surgical complexity. We also evaluated hospital costs rather than charges in order to assess the actual cost of the services. Interestingly, we found that while total hospital costs varied significantly by center for all operations evaluated, these differences were most prominent for the lower complexity procedures (atrial septal defect and ventricular septal defect repair). The reasons for this are unclear, however it may be possible that for the higher complexity cases, the complexity of the procedure or patient-specific factors outweigh any center-related factors impacting cost. In addition we found that for the lower complexity surgeries, higher center surgical volume was associated with lower total hospital costs, while this association was not seen for the higher complexity surgeries. In evaluating other center-level factors impacting hospital costs, we did not find that teaching or children’s hospitals were associated with reduced hospital costs, similar to other studies (3).
There may be several reasons for the association of center volume with lower hospital costs. It may be that patients at higher volume centers have fewer post-operative complications. While were not able to evaluate post-operative complications specific to congenital heart surgery in this study utilizing administrative data, it has previously been shown that complications following congenital heart surgery are associated with increased resource utilization (4). In addition, it may also be possible that larger, more experienced centers have greater resources and standardized protocols of care to facilitate post-operative recovery. The implementation of multidisciplinary standardized care protocols has been associated with decreased length of stay and reduced hospital charges for patients undergoing congenital heart surgery (16-18). Davis et al. showed that implementation of a standardized care plan for 65 consecutive children undergoing atrial septal defect repair at their institution was associated with significant reductions in intensive care unit and total hospital length of stay, as well as a reduction in total hospital charges (16). Fernandes et al. evaluated a more diverse population of 175 patients undergoing congenital heart surgery and also found that patients treated according to a standardized recovery protocol vs. conventional care had reduced length of stay and reduced hospital costs (17). Standardized management has also been shown to improve outcome in high risk cohorts as well, such as single ventricle patients undergoing the Norwood operation (19). Interestingly, we found that the association of center volume with cost was only significant for the lower complexity surgeries. This may be due to a wider range of center surgical volume for the lower complexity surgeries, compared with the higher complexity surgeries.
The results of this study have several implications in this era of rising health care costs. Our data, along with the previous Connor et al. analysis, suggest significant variation in resource utilization among different US states and different centers caring for patients undergoing congenital heart surgery (3). Further analysis of factors associated with outcome and cost in this population may elucidate best practices which can both improve outcome and reduce cost across different centers and regions. Our data suggest that while higher complexity operations account for greater relative cost, there is greater variation in cost from center to center for lower complexity operations. In addition, while our data indicate that the estimated cost savings per patient if all centers performed as well as the lower cost quartile is greater for the higher complexity procedures, the total cost savings across the board would likely be greater for the lower complexity surgeries such as atrial septal defect and ventricular septal defect repair which are over two times more common than tetralogy of Fallot repair and the arterial switch operation (20). Thus,, initial efforts to reduce costs may be best focused on these lower complexity, but common, congenital heart operations.
Limitations
In this analysis we used a large administrative database to evaluate variation in hospital costs. Although administrative datasources contain valuable resource utilization information which makes these types of analyses possible, they may lack detailed clinical data in some cases. It is also possible that certain unmeasured confounders may be present, however we were able to adjust for important patient and center factors demonstrated to impact resource utilization in previous analyses using both administrative and clinical data. While the Premier database includes a diverse variety of hospitals in terms of region of the country, teaching status, and center volume, not all US children’s hospitals are represented, and thus, our results may not be generalizable across all centers. A strength of the present analysis was the use of cost data rather than charges, in order to better reflect the cost of the services being provided. However, these data are likely an underestimate of true total costs as they do not account for physician professional fees, and other costs relevant to the family and society such as transportation to the hospital, lodging, child care for other siblings, and loss of income and productivity if it is necessary to take time off from the workplace. We were also unable to account for the cost of previous or subsequent surgical procedures the patient may have had, such as tetralogy of Fallot patients who under went initial palliation with a Blalock-Taussig shunt prior to complete repair. In addition, the relatively small number of patients and procedures in certain groups, such as those undergoing the arterial switch operation may have limited our power to detect differences in this group. Finally, although we used widely recognized methodology to identify operations of interest in the database, it is possible that coding errors may exist in administrative datasources (10). The similarity of our cost data with that from other studies utilizing clinical datasources, and expected increase in total cost with increased complexity of operations in our analysis, support the validity of these data (5-7).
Conclusions
In this multicenter evaluation of hospital costs in patients undergoing congenital heart surgery, we found significant variation from center to center even after accounting for important patient factors and length of stay. These differences were most pronounced for lower complexity surgeries and hospital surgical volume seemed to play a role. Further evaluation of patient outcomes in conjunction with cost and associated factors may elucidate strategies to both improve outcome and reduce cost variation across centers. Our data would suggest that these efforts may be best focused first on lower complexity, common, operations, where cost variation across centers is most pronounced and the overall expected cost reduction would be greatest given the higher frequency of these types of surgeries. In addition, the recent linking of clinical registry data with administrative data in the congenital heart surgery population will enable analyses such as those evaluating costs (captured in the administrative database) associated with specific post-operative complications (captured in the registry), and thus, the cost-savings that may be expected from quality improvement initiatives to reduce post-operative morbidities and complications (21).
Acknowledgments
Funding Sources: Dr. Pasquali receives grant support from the National Heart, Lung, and Blood Institute (1K08HL103631-01), and from the American Heart Association Mid-Atlantic Affiliate Clinical Research Program.
This study was supported in part by cooperative agreement HS016957 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Conflict of Interest Disclosures: None
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gray DT, Pourmoghadam K, Weis J, Hsu A, Moore J, Jacobs J, Steiner C, Jacobs M. Nationwide trends in inpatient pediatric cardiac surgery and interventional catheterization procedures from 1997-2006: On-line estimates from the US Healthcare Cost and Utilization Project. Circ Cardiovasc Qual Outcomes. 2009;2:e23. [Google Scholar]
- 2.Robbins JM, Bird TM, Tilford JM, Cleves MA, Hobbs CA, Grosse SD, Correa A. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects-United States, 2003. MMWR. 2007;56:25–29. [PubMed] [Google Scholar]
- 3.Connor JA, Gauvreau K, Jenkins KJ. Factors associated with increased resource utilization for congenital heart disease. Pediatrics. 2005;116:689–695. doi: 10.1542/peds.2004-2071. [DOI] [PubMed] [Google Scholar]
- 4.Benavidez OJ, Connor JA, Gauvreau K, Jenkins KJ. The contribution of complications to high resource utilization during congenital heart surgery admissions. Congenit Heart Dis. 2007;2:319–326. doi: 10.1111/j.1747-0803.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 5.Ungerleider RM, Kanter RJ, O’Laughlin M, Bengur AR, Anderson PA, Herlong JR, Li J, Armstrong BE, Tripp ME, Garson A, Meliones JN, Jaggers J, Sanders SP, Greeley WJ. Effect of repair strategy on hospital cost for infants with tetralogy of Fallot. Ann Surg. 1997;225:779–83. doi: 10.1097/00000658-199706000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ungerleider RM, Bengur AR, Kessenich AL, Liekweg RJ, Hart EM, Rice BA, Miller CE, Lockwood NW, Knauss SA, Jaggers J, Sanders SP, Greeley WJ. Risk factors for higher cost in congenital heart operations. Ann Thorac Surg. 1997;64:44–8. doi: 10.1016/s0003-4975(97)00503-1. [DOI] [PubMed] [Google Scholar]
- 7.Parrish MD, Pollock M, Gauthier N, Park J, Hobde B. Sources of variability in hospital costs of atrial septal defect repair. Am J Cardiol. 1998;82:252–4. doi: 10.1016/s0002-9149(98)00301-4. [DOI] [PubMed] [Google Scholar]
- 8.LaPointe NMA, Sun JL, Kaplan S, d’Almada P, Al-Khatib SM. Rhythm versus rate control in the contemporary management of atrial fibrillation in-hospital. Am J Cardiol. 2008;101:1134–1141. doi: 10.1016/j.amjcard.2007.11.067. [DOI] [PubMed] [Google Scholar]
- 9.Kim MH, Klingman D, Lin J, Pathak P, Battleman D. Cost of hospital admission for antiarrhythmic drug initiation in atrial fibrillation. Ann Pharmacother. 2009;43:840–848. doi: 10.1345/aph.1L698. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123:110–118. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 11.Al-Radi OO, Harrell FE, Caldarone CA, McCrindle BW, Jacobs JP, Williams MG, VanArsdell GS, Williams WG. Case complexity scores in congenital heart surgery: a comparative study of the Aristotle Basic Complexity score and the Risk Adjustment in Congenital Heart Surgery (RACHS-1) system. J Thorac Cardiovas Surg. 2007;133:865–875. doi: 10.1016/j.jtcvs.2006.05.071. [DOI] [PubMed] [Google Scholar]
- 12.Pasquali SK, Hall M, Slonim AD, Jenkins KJ, Marino BS, Cohen MS, Shah SS. Off-label use of cardiovascular medications in children hospitalized with congenital and acquired heart disease. Circ Cardiovasc Qual Outcomes. 2008;1:74–83. doi: 10.1161/CIRCOUTCOMES.108.787176. [DOI] [PubMed] [Google Scholar]
- 13.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- 14.Gillum RF. Epidemiology of congenital heart disease in the United States. Am Heart J. 1994;127:919–927. doi: 10.1016/0002-8703(94)90562-2. [DOI] [PubMed] [Google Scholar]
- 15.Williams DL, Gelijns AC, Moskowitz AJ, Weinberg AD, Ng JH, Crawford E, Hayes CJ, Quaegebeur JM. Hypoplastic left heart syndrome: valuing the survival. J Thorac Cardiovasc Surg. 2000;119:720–31. doi: 10.1016/S0022-5223(00)70007-9. [DOI] [PubMed] [Google Scholar]
- 16.Davis JT, Allen HD, Cohen DM. Fiscal impact of a practice pattern for secundum atrial septal defect repair in children. Am J Cardiol. 1994;74:512–514. doi: 10.1016/0002-9149(94)90919-9. [DOI] [PubMed] [Google Scholar]
- 17.Fernandes AM, Mansur AJ, Canêo LF, Lourenço DD, Piccioni MA, Franchi SM, Afiune CM, Gadioli JW, Sde A Oliveira, Ramires JA. The reduction in hospital stay and costs in the care of patients with congenital heart diseases undergoing fast-track cardiac surgery. Arq Bras Cardiol. 2004;83:27–34. 18–26. doi: 10.1590/s0066-782x2004001300003. [DOI] [PubMed] [Google Scholar]
- 18.Waldman JD, George L, Lamberti JJ, Lodge FA, Pappelbaum SJ, Turner SW, Mathewson JW, Kirkpatrick SE. Containing costs in the treatment of congenital heart disease. West J Med. 1984;141:123–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Srinivasan C, Sachdeva R, Morrow WR, Gossett J, Chipman CW, Imamura M, Jaquiss RDB. Standardized management improves outcomes after the Norwood procedure. Congenit Heart Dis. 2009;4:329–337. doi: 10.1111/j.1747-0803.2009.00323.x. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs JP, Jacobs ML, Mavroudis C, Lacour-Gayet FG, Tchervenkov CI. Executive Summary: The Society of Thoracic Surgeons Congenital Heart Surgery Database - Twelfth Harvest – (January 1, 2006 – December 31, 2009) The Society of Thoracic Surgeons and Duke Clinical Research Institute, Duke University Medical Center; Durham, North Carolina, United States: 2010. Spring. Harvest. [Google Scholar]
- 21.Pasquali SK, Jacobs JP, Shook GJ, O’Brien SM, Hall M, Jacobs ML, Welke KF, Gaynor JW, Peterson ED, Shah SS, Li JS. Linking clinical registry data with administrative data using indirect identifiers: Implementation and validation in the congenital heart surgery population. American Heart Journal. 2010;160:1099–1104. doi: 10.1016/j.ahj.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]