Abstract
Background:
Surgical repair of massive rotator cuff tears is associated with less favorable clinical results and a higher retear rate than repair of smaller tears, which is attributed to irreversible degenerative changes of the musculotendinous unit.
Materials and Methods:
During the study period, 25 consecutive patients with a massive rotator cuff tear were enrolled in the study and the tears were repaired with an open suture anchor repair technique. Preoperative and postoperative clinical assessments were performed with the Constant score, the simple shoulder test (SST) and a pain visual analog scale (VAS). At the final follow-up, rotator cuff strength measurement was evaluated and assessment of tendon integrity, fatty degeneration and muscle atrophy was done using a standardized magnetic resonance imaging protocol.
Results:
The mean follow-up period was 70 months. The mean constant score improved significantly from 42.3 to 73.1 points at the final follow-up. Both the SST and the pain VAS improved significantly from 5.3 to 10.2 points and from 6.3 to 2.1, respectively. The overall retear rate was 44% after 6 years. Patients with an intact repair had better shoulder scores and rotator cuff strength than those with a failed repair, and also the retear group showed a significant clinical improvement (each P<0.05). Rotator cuff strength in all testing positions was significantly reduced for the operated compared to the contralateral shoulder. Muscle atrophy and fatty infiltration of the rotator cuff muscles did not recover in intact repairs, whereas both parameters progressed in retorn cuffs.
Conclusions:
Open repair of massive rotator tears achieved high patient satisfaction and a good clinical outcome at the long-term follow-up despite a high retear rate. Also, shoulders with retorn cuffs were significantly improved by the procedure. Muscle atrophy and fatty muscle degeneration could not be reversed after repair and rotator cuff strength still did not equal that of the contralateral shoulder after 6 years.
Level of evidence:
Level IV
Keywords: Magnetic resonance imaging, massive rotator cuff tear, open rotator cuff repair, rotator cuff strength, subscapularis function
INTRODUCTION
Large tears are frequently associated with pain, weakness and persistent functional disability and are incompatible with heavy manual work in middle-aged patients.[1–3] Most massive rotator cuff tears show an unfavorable outcome after conservative treatment.[2–5] Non-reconstructive procedures are a reliable therapeutic option for the treatment of massive tears in elderly patients,[4–7] whereas surgical repair is recommended for the younger and active population, as tear size increases over time leading to cuff tear arthropathy.[5,8–10] In the literature, there is no randomized controlled trial comparing nonoperative with operative treatment or directly comparing surgical options and complete repair of massive tears showing the highest grade of recommendation in a recent review.[5] Surgical repair is technically challenging and associated with a higher retear rate than repair of smaller tears,[9,11–14] and also the overall outcome of massive tears is less satisfactory.[9,12–16] This finding is attributed to the fact that chronic massive tears are more commonly associated with advanced fatty degeneration and muscle atrophy.[1,4,9,14,16] It was found that intact repairs show a superior outcome compared to shoulders with a retear,[3,5,9,11,13] but structural failure in most cases is not generally associated with clinical failure,[3,9,11,12,16] as the majority of these cases show a clinical improvement.
The objectives of this study were to report on the clinical results and the cuff integrity after repair of massive rotator cuff tears, and to determine if fatty muscle degeneration recovers after repair.
Our hypothesis was that clinical results would be improved regardless of the presence of a retear or a lacking reversibility of fatty muscle degeneration and that rotator cuff strength is reduced in retorn cuffs.
MATERIALS AND METHODS
Twenty-five consecutive patients who underwent a repair of a massive rotator cuff tear between 2003 and 2005 were prospectively included in the study. All patients were available for final follow-up.
The local institutional review board approved the study and all patients gave written informed consent.
Patients were included in the study if they had a massive tear confirmed during surgery. Using the Cofield tear classification,[17] a tear was defined as a massive rotator cuff tear if the anterior-posterior dimension exceeded 5 cm. Patients who met the following criteria were excluded: previous operation, fracture or infection on the affected shoulder, or moderate to severe glenohumeral osteoarthritis. The indication for surgery was in all cases a painful shoulder with ongoing functional impairment after an unsuccessful period of physical therapy of at least 3 months.
The study group consisted of 20 men and 5 women, who had an average age of 60.7 years (range 51-64 years). The dominant shoulder was involved in 18 (72%) patients. The preoperative symptomatic interval averaged 18 months (range 3-50 months). Patients were followed up with clinical examination and magnetic resonance imaging (MRI) at an average of 70 months after the operation (range 58-84 months).
Clinical evaluation
All patients underwent a standard physical examination before and after the operation and their history was taken. The final follow-up evaluation was performed by an independent examiner who was not a member of the surgical team. Patients were evaluated with the scoring system of Constant and Murley[18] using the absolute Constant score and the age-adjusted Constant score,[19] the Simple Shoulder Test (SST)[19] and a pain visual analog scale (VAS) with 10 points representing the maximal imaginable pain. Clinical testing included assessment of active pain-free range of motion and testing of all specific rotator cuff tests and lag signs[20] for all rotator cuff components. Abduction strength for the Constant score was tested with a dynamometer (Isobex® dynamometer, Cursor SA, Bern, Switzerland).
Quantitative rotator cuff strength evaluation
For quantitative strength measurement of all rotator cuff components, we used a testing apparatus that had been used in a previous study.[21] With this electronic force measurement plate (FMP), the strength of all rotator cuff components could be tested in their specific position:[22] belly-press and lift-off position (subscapularis), Jobe-test position (supraspinatus) and external rotation position with the arm at 0° of abduction (infraspinatus and teres minor) [Figures 1–4].
Figure 1.

Internal rotation position (belly-press position)
Figure 4.

External rotation position
Figure 2.

Internal rotation position (lift-off position)
Figure 3.

Abduction position (Jobe-test position)
With the use of a sling and variable adjustment, the plate could be placed at the correct position for all patients. The testing positions and the mode and duration of action were explained in detail to all patients before testing. Strength testing was performed each three times on the operated and on the contralateral shoulder.
Force values in all testing positions were measured in Newton (N) and were compared to the contralateral arm. The FMP was also used for strength testing in a healthy control group of 100 patients. In this group, significant differences were present as men scored higher force values than women (P<0.05) in all testing positions, but the differences were not age related in both genders (P>0.05). Hand dominance showed significantly higher force values in the dominant arm versus the non-dominant arm in both gender groups only in the Jobe-test position (P<0.05), but not in the three other testing positions. The device was especially developed to quantify internal and external rotation strength, as both are underrepresented in the commonly used scoring systems.
Radiographic evaluation
All patients underwent preoperative routine radiographs including a true anteroposterior radiograph in neutral rotationand a y-view-radiograph. On the true anteroposterior radiograph, the acromiohumeral distance was measured in millimeters. Glenohumeral osteoarthritis was classified according to the criteria of Samilson and Prieto.[23]
A preoperative MRI scan was performed in all patients for grading of fatty muscle degeneration and muscle atrophy. The fatty infiltration grade (FIG) of each rotator cuff muscle was determined according to the MRI grading system described by Fuchs et al., based on the Goutallier CT-score.[24,25] Muscle atrophy was graded according to the classification of Thomazeau, using parasagittal images (Y-shaped view).[13]
Postoperatively, all the patients underwent a standardized MRI using a 1.5-T MRI scanner (Magnetom Espree, Siemens® Medical Solutions, Erlangen, Germany) with a dedicated shoulder coil. MR examination included the following sequences: paracoronal T1-weighted spin echo (TR 510 ms, TE 15 ms) and fat-suppressed intermediate weighted turbo spin-echoClinical evaluation (TSE; TR 2800 ms, TE 45 ms); axial fat-suppressed intermediate weighted TSE (TR 2800 ms, TE 45 ms) and parasagittal T2-weighted TSE (TR 4200 ms, TE 90 ms).
Tendon integrity was graded on axial and paracoronal T2-weighted, proton density weighted, as well as short inversion recovery (STIR) sequences according to the established MRI criteria.[26,27] On axial and paracoronal sequences, the status of the musculotendinous unit was graded as intact with normal thickness (grade I) or intact and thinned (grade II). The diagnosis of a rerupture was made if a tendon gap was filled with fluid-equivalent signal or a non-visualization of the tendon with tendon retraction was present on one or more sections (grade III).[27] On the Y-shaped view in the parasagittal plane, muscle atrophy was evaluated by measuring each rotator cuff muscle′s cross-sectional area (CSA) in square millimetres. On the Y-shaped view, the muscle borders were traced with use of PACS software in a modified technique as described by Juul-Kristense.[28] MR images were assessed by two experienced musculoskeletal radiologists who were blinded to the clinical findings.
Operative technique
Patients were treated with a standardized transdeltoid open surgical repair by a single surgeon. The open surgical repair was performed with the patient in the beach chair position. An arthroscopy was performed in all patients to check the tear location and to check if the tear could be addressed with a single transdeltoid open approach. After bursectomy, an arthroscopic subacromial decompression was performed; in case of a tender acromioclavicular joint (AC joint), an arthroscopic AC joint resection was performed. Using an open technique, tear size was measured with a ruler. Tear margins of the crescent and U-shaped tears were identified, and tears were classified using the Cofield classification as two-tendon tears involving the supraspinatus and infraspinatus and three-tendon tears involving the supraspinatus, infraspinatus and the subscapularis. Subscapularis involvement was graded using the Fox and Romeo classification.[29] Bursal, capsular and interval releases were performed with scissors to achieve adequate tendon mobilization for a repair with no or minimal tension. Tendons were reinserted at their original area of insertion. Tendon fixation was performed with suture anchors (Titancorkscrew® 5 mm or Biocorkscrew® 5 mm; Arthrex, Naples, FL, USA), double-loaded with number 2 braided non-absorbable sutures (Fiberwire® , Arthrex), in a single row technique using a modified Mason-Allen stitch technique.[19] Depending on the patient′s functional demand, the long head of the biceps tendon (LHB) was treated either with a biceps tenodesis or by tenotomy.
Rehabilitation
Postoperatively, the shoulder was protected using an abduction brace for 6 weeks. Passive mobilization of the shoulder was started 2 weeks after the operation. Gradual return to full active motion was started at 6 weeks and progressed to resistive strengthening. Heavy lifting was not allowed for a duration of 6 months.
Statistical methods
Standard statistical software (SPSS, Version 18, Chicago, IL, USA) was used to analyze the data. For descriptive analysis, the parameters were evaluated by calculating the mean, range and SD values. Wilcoxon test was used for analysis of paired data (e.g. pre- and postoperative Constant score, rotator cuff strength FMP values) and Mann-Whitney test was used for unpaired groups. Spearman correlation coefficient was used to test quantitative relationships between variables. The level of significance was set at a P value of <0.05.
RESULTS
In 13 cases the tear involved the supraspinatus and the infraspinatus (two-tendon tear). In 12 cases the tear involved the supraspinatus, the infraspinatus and the subscapularis tendon (three-tendon tear). According to the Fox and Romeo classification, in eight shoulders the tear involved the upper 25% of the tendon (type II) and in four shoulders the tears involved 25-50% of the upper subscapularis (type III).
An average of 3.8 suture anchors (range 3-5 anchors) was used for the repair. In 20 cases a biceps tenodesis was performed, and in two cases a biceps tenotomy was performed.
As complications, we observed one case of postoperative stiffness that was treated with an arthroscopic capsular release 12 months after the repair. There were no complications like hematoma, deep or superficial infection, deltoid dehiscence or nerve injury. No anchor loosening was detected on postoperative radiographs and MR images.
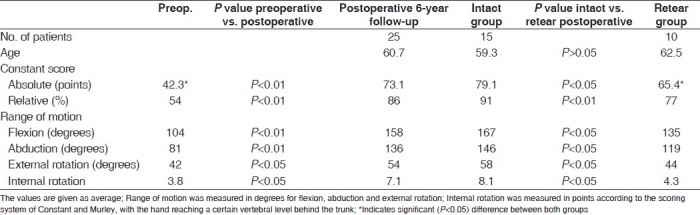
Clinical outcome
At the final follow-up, 70 months (range 58-84 months) after the operation, 80% of the patients rated their result as excellent or good and 20% rated their result as fair or poor. The mean Constant score improved significantly from 42.3 points (range 31-59 points) preoperatively to 73.1 points (range 51-87 points) postoperatively, with a significant gain in all subcategories. The relative Constant score averaged 86%. Pain-free flexion improved from an average of 104° to 158°, and abduction improved from an average of 81° to an average of 136° (each P<0.05). Overall active external rotation with the arm at the side (from a preoperative average of 42° to a postoperative average of 54°; P<0.05) improved significantly. Internal rotation behind the trunk (preoperative average level: iliosacral joint to postoperative average level: L1; P<0.05) was significantly improved by surgery [Table 1].
Table 1.
Comparison of clinical parameters at the preoperative and the follow-up evaluation
The SST increased from a preoperative average of 5.3 points (range 3-9 points) to a postoperative average of 10.2 points (range 6-12 points) (P<0.01). The pain VAS improved from a preoperative average of 6.3±2.8 points to a postoperative average of 2.1±2.0 points (P<0.001).
In the two-tendon tear group, there was no positive preoperative subscapularis test. In the three-tendon tear group, there were 10 positive belly-press tests (84%) and 8 positive lift-off tests (67%) preoperatively.
Postoperatively, we detected five (20%) residual positive belly-press tests. The lift-off test was positive in 2 out of 25 cases (8%) and could not be performed in 2 cases due to restricted internal rotation.
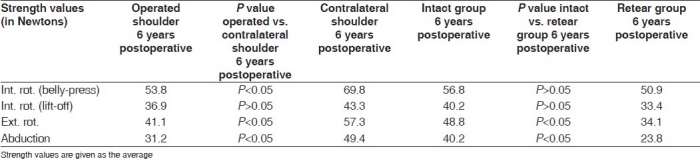
Rotator cuff strength evaluation
In the operated shoulder, subscapularis strength in the belly-press position averaged 53.8 N (range 26-94 N) compared to 69.8 N (range 36-119 N) on the contralateral side (P<0.05). In the lift-off position, the operated shoulder generated an average of 36.9 N (range 19-71 N) compared to 43.3 N (range 27-94 N) on the contralateral side (P>0.05) [Table 2]. Abduction strength in the Jobe-test position in the operated shoulder averaged 31.2 N (range 5-64 N) compared to 49.4 N (range 29-115 N) on the contralateral side (P<0.05). Using the dynamometer for the Constant score measurement, the average measured abduction strength on the operated shoulder was 3.3 kg (range 0.8-6.3 kg). External rotation strength on the operated side averaged 41.1 N (range 19-74 N) compared to 57.3 N (range 29-95 N) on the contralateral side (P<0.05). With the use of the FMP, we could show that there was a significant strength deficit on the operated shoulder in all specific positions compared to the contralateral side, except for the lift-off test.
Table 2.
Force measurement plate strength values of the operated shoulder (entire series, intact group, retear group) and the contralateral shoulder
Constant score results correlated well with FMP strength values for abduction in the Jobe position (P<0.001; r=0.736) and external rotation (P<0.01; r=0.548), but not for internal rotation strength in the belly-press position (P>0.05; r=0.363).
Comparison of postoperative intact repairs and retorn cuffs
Age was not a prognostic outcome factor associated with a higher retear rate at the follow-up (P>0.05). Patients with an intact repair had significantly better absolute and relative Constant scores and strength values than those with a failed repair. In all 11 patients with a retear, the Constant score showed a significant gain when compared to the preoperative status (P<0.05)[Table 1].
External rotation and abduction strength revealed significantly higher strength values for the intact group compared to the retear group (P<0.05) and the hypothesis could be confirmed [Table 2]. Strength values in both the groups correlated positively with Constant score results.
In intact repairs, subscapularis strength in the belly-press and the lift-off test positions did not gain significantly higher values compared to the retear group (P>0.05) [Table 2].
Comparison of initial two- and three-tendon tears
Constant score results of shoulders with an initial two-tendon tear were not significantly higher compared to shoulders with an initial three-tendon tear (75.2 vs. 72.4 points; P>0.05). At the final follow-up, subscapularis strength in initial three-tendon tears was not significantly reduced, compared to the group with initial two-tendon tears (50.1 N vs. 56.3 N; P>0.05). Abduction and external rotation strength at the final follow-up did not differ significantly in bothtear pattern groups (P>0.05).
Radiographic results
The MRI appearance of the tendons was never normal, with increased tendon signal intensity in all the repaired tendons [Figure 5]. In 13 of the 14 intact rotator cuffs (93%), the tendons were graded as thinned with increased signal intensity (grade II). The overall retear rate was 44% (11 out of 25). Five (38%) of the 13 shoulders with an initial posterosuperior two-tendon tear and 6 (50%) of the 12 patients with an initial three-tendon tear had a retear. When compared with the preoperative MRI, no retear was larger than the initial tear, with four retears having a similar tear size as the original tear and seven retears being distinctly smaller, as measured on sagittal MRI planes. The retear always involved the supraspinatus tendon. In six cases, the retear was limited to the supraspinatus tendon; in four cases, the tear involved the supraspinatus tendon and the upper infraspinatus tendon; and in one case of an initial three-tendon tear, the retear involved the supraspinatus, infraspinatus and the upper part of the subscapularis tendon.
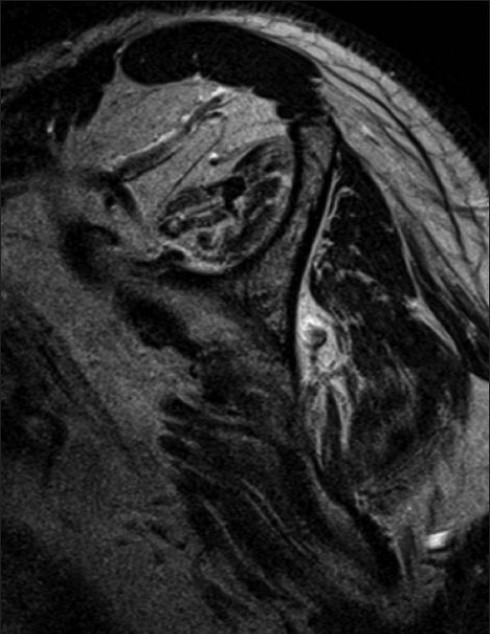
Figure 5.
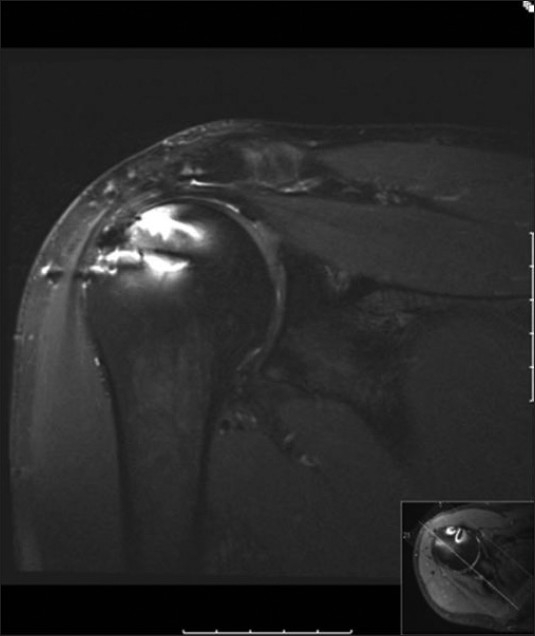
Intact repair showing a thinned supraspinatus tendon with increased tendon signal intensity
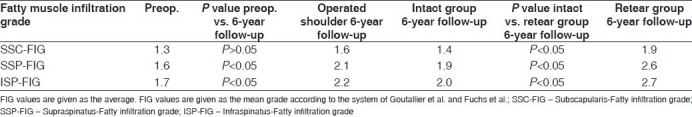
Overall, the preoperative muscular atrophy and the fatty infiltration of the rotator cuff muscles were not reversed by the surgical repair [Figures 6 and 7]. However, the cross-sectional areas of all rotator cuff muscles were significantly greater when the repair was intact (P<0.05), compared to retorn cuffs [Table 3]. Fatty degeneration progressed in the supraspinatus and in the infraspinatus, but not in the subscapularis. In the retear group the FIG showed a significantly higher FIG value (P<0.05) compared to the intact group [Table 4].
Figure 6.
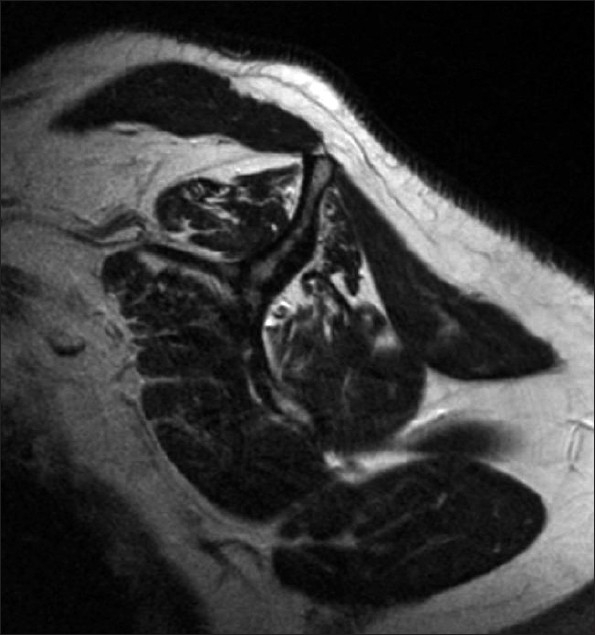
Persistent mild atrophy of the subscapularis (SSC), supraspinatus (SSP) and infraspinatus (ISP) muscles, with moderate fatty muscle infiltration following a successful repair
Figure 7.
Advanced atrophy and fatty degeneration of rotator cuff muscles in a three-tendon retear
Table 3.
Muscle cross-sectional area (in mm2) of the study population, the intact group and the retear group
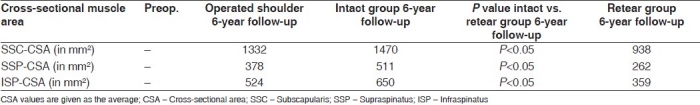
Table 4.
Fatty infiltration grade of the muscles at the preoperative and the follow-up evaluation
An FIG higher than stage 2 of the infraspinatus muscle correlated inversely with the postoperative Constant score (P<0.05; r=-0.412).
Analysis of conventional radiographs showed that the mean acromiohumeral distance decreased significantly (P<0.01) from 9.5 mm (range 6-13 mm) preoperatively to 7.6 mm (range 3-12 mm) at the 6-year follow-up.
The average degree of present osteoarthritis increased significantly (P<0.05) from stage 1.1 preoperatively to stage 1.5 postoperatively.
DISCUSSION
Open repair of massive rotator cuff tears achieved good patient satisfaction and significant clinical improvement at the 5-year follow-up in an active patient population with an average age of 61 years. Overall clinical outcomes improved regardless of tendon integrity, but were significantly more pronounced in intact cuffs. MRI revealed a retear rate of 44% and demonstrated that fatty muscle degeneration and muscle atrophy were not reversible at the 5-year follow-up, which concurs with the findings of previous studies.[3,9,16]
The new strength testing device was implemented to additionally quantify internal and external rotation strength that reflects the function of the transversal force couple,[15,21] which is especially important in the presence of a retear.[1,5,9,30,31,32] We found a significant strength deficit for abduction and external rotation in retorn cuffs compared to intact cuffs, but not for internal rotation strength. We believe that this is due to the fact that the subscapularis retear rate with 10% (1 out of 10) was very low and that all initial three-tendon tears only involved the upper subscapularis portion. With a mainly restored subscapularis function, the remaining external rotation function became the most important factor for a sufficiently working transversal force couple balancing the humeral head in case of a retear.[1,5,9,30] Partial subscapularis insufficiency was present in 16% of the cases in the postoperative course and occurred only in the group of initial three-tendon tears with preoperative subscapularis involvement. The presence of an initial subscapularis tendon tear did not correlate with a less favorable outcome or lower postoperative scores.[9]
Postoperative strength in all tested positions still did not equal that of the contralateral shoulder after 6 years, except for the lift-off test.[21,33]
Our long-term results with a clinical improvement after repair of massive tears regardless of tendon integrity are consistent with the results of Gerber and Zumstein,[3,9] who also showed a significant clinical improvement after open repair of 27 massive tears at the 3- and 10-year follow-up despite a retear rate of 37% and 57%, respectively. These authors found a slight improvement of clinical scores at the 10-year follow-up compared to the 3-year follow-up, despite an increasing retear rate. At both follow-ups, the authors found no reversibility of fatty muscle infiltration and muscle atrophy. We could confirm these findings and found a mild progression of both parameters in postoperative intact cuffs, but a significant progression in retorn cuffs.
Several studies showed that good clinical outcomes can be achieved despite a high retear rate, which was detected with ultrasound[11,12] and MRI,[3,9,16] suggesting that small retears can be compensated clinically and that patients do benefit from a repair attempt. Mellado et al.[16] showed that open repair of massive cuff tears in 28 patients resulted in significant clinical improvement and patient satisfaction despite a retear rate of 86%. Correlation of postoperative clinical and MRI results showed that a retear of 3.4 cm or less in the coronal plane and a postoperative fatty infiltration of the infraspinatus less than or equal to 2 were positive predictors for a good clinical outcome.
We found that fatty degeneration of the infraspinatus, higher than stage 2, and reduced external rotation strength may predict inferior clinical outcomes.
With use of the electronic FMP, we could perform a quantitative measurement of abduction strength, internal rotation strength and external rotation strength, which allows to quantify the functional status of the residual force couple in case of a retear and represents an useful addition to the widely used clinical scores, in which internal and external rotation strengths are underrepresented. FMP abduction strength values showed a good correlation with the values obtained with the widely used Isobex dynamometer. Consistent with the findings of Rokito et al.,[33] we could show that strength of the operated shoulder still did not equal that of the contralateral shoulder at the 6-year follow-up. Burkhart et al.,[14] as the first study group, described significant clinical improvement following arthroscopic repair of 22 massive rotator cuff tears, even with stage 3 and 4 fatty degeneration of rotator cuff muscles, and the authors attribute their good outcomes to a minimal invasive arthroscopic reconstruction technique. In that study, no postoperative MRI was applied.
Further comparative studies will have to prove the possible positive effect of a minimal invasive arthroscopic approach and partial repair techniques with strain reduction for the repair of massive cuff tears.[14,30] Most radiographic controlled[9,11,12,16] studies and the present study demonstrate that clinical outcomes improve regardless of tendon integrity and that a repair attempt is justified, especially in an active population at the age of 60 years.
This study has several limitations. It was a retrospective study and we included no control group. Strength measurement with the FMP was only available at the final follow-up examination. As arthroscopic debridement or reversed tuberculoplasty is only an option for the treatment of massive tears in an elderly low-demand population,[6] these techniques are of limited benefit for a younger and active patient group like in our series.[1,8] As tear size and degeneration of the musculotendinous unit increase over time,[8,9] massive tears with mild to moderate fatty muscle infiltration benefit from a repair in order to restore the force couple that is necessary for normal glenohumeral joint function and to avoid the early occurrence of cuff tear arthropathy.[5,9]
CONCLUSION
We could achieve high patient satisfaction and good clinical outcomes at the long-term follow-up after repair of massive rotator cuff tears despite a retear rate of 44%. Also, shoulders with retorn cuffs were significantly improved by the procedure, and good shoulder function in case of a retear was based on a functioning subscapularis/infraspinatus musculotendinous unit. Muscle atrophy and fatty muscle degeneration could not be reversed in intact repairs and progressed in retorn cuff muscles. Rotator cuff strength could be measured with the FMP in all planes and still was reduced compared to the contralateral shoulder after 6 years.
ACKNOWLEDGMENT
The study was funded by a grant of the German Arthrosis Society (Grant P171).
Footnotes
Source of Support: German Arthrosis Society (Grant P171)
Conflict of Interest: None declared.
REFERENCES
- 1.Jost B, Zumstein MA, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–79. doi: 10.2106/JBJS.E.00003. [DOI] [PubMed] [Google Scholar]
- 2.Gartsman GM. Massive, irreparable tears of the rotator cuff.Results of operative debridement and subacromial decompression. J Bone Joint Surg Am. 1997;79:715–21. doi: 10.2106/00004623-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–15. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928–34. doi: 10.2106/JBJS.F.01073. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92:1894–908. doi: 10.2106/JBJS.I.01531. [DOI] [PubMed] [Google Scholar]
- 6.Liem D, Lengers N, Dedy N, Poetzl W, Steinbeck J, Marquardt B. Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24:743–8. doi: 10.1016/j.arthro.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Lehmann C, Cuomo F, Kummer FJ, Zuckerman JD. The incidence of full thickness rotator cuff tears in a large cadaveric population. Bull Hosp Jt Dis. 1995;54:30–1. [PubMed] [Google Scholar]
- 8.Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710–4. doi: 10.1177/0363546510393944. [DOI] [PubMed] [Google Scholar]
- 9.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–31. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
- 10.Turkel SJ, Panio MW, Marshall JL, Girgis FJ. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–17. [PubMed] [Google Scholar]
- 11.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff.Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–9. [PubMed] [Google Scholar]
- 12.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome of repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–24. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Ortho Relat Res. 1997:275–83. [PubMed] [Google Scholar]
- 14.Burkhart SS, Barth JR, Richards DP, Zlatkin MB, Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23:347–54. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears.Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991:45–56. [PubMed] [Google Scholar]
- 16.Mellado JM, Calmet J, Olona M, Esteve C, Camins A, Pérez Del Palomar L, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005;184:1456–63. doi: 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 17.Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67:974–9. [PubMed] [Google Scholar]
- 18.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–4. [PubMed] [Google Scholar]
- 19.Habermeyer P. Schulterchirurgie. Heidelberg: Urban-Schwarzenberg Verlag; 2009. [Google Scholar]
- 20.Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996;5:307–13. doi: 10.1016/s1058-2746(96)80058-9. [DOI] [PubMed] [Google Scholar]
- 21.Bartl C, Salzmann GM, Seppel G, Eichhorn S, Holzapfel K, Wörtler K, et al. Subscapularis function and structural integrity after arthroscopic repair of isolated subscapularis tears. Am J Sports Med. 2011:1255–62. doi: 10.1177/0363546510396317. [DOI] [PubMed] [Google Scholar]
- 22.Tokish JM, Decker MJ, Ellis HB, Torry MR, Hawkins RJ. The belly-press test for the physical examination of the subscapularis muscle: Electromyographic validation and comparison to the lift-off test. J Shoulder Elbow Surg. 2003;12:427–30. doi: 10.1016/s1058-2746(03)00047-8. [DOI] [PubMed] [Google Scholar]
- 23.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–60. [PubMed] [Google Scholar]
- 24.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599–605. doi: 10.1016/s1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 25.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures.Pre- and post-operative evaluation by CT-scan. Clin Orthop Relat Res. 1994:78–83. [PubMed] [Google Scholar]
- 26.Magee Th, Gaenslen ES, Seitz R, Hinson GA, Wetzel LH. MR imaging of the shoulder after surgery. AJR Am J Roentgenol. 1997;168:925–8. doi: 10.2214/ajr.168.4.9124141. [DOI] [PubMed] [Google Scholar]
- 27.Motamedi AR, Urrea LH, Hancock RE, Hawkins RJ, Ho C. Accuracy of magnetic resonance imaging in determining the presence and size of recurrent rotator cuff tears. J Shoulder Elbow Surg. 2002;11:6–10. doi: 10.1067/mse.2002.120139. [DOI] [PubMed] [Google Scholar]
- 28.Juul-Kristensen B, Bojsen-Moller F, Finsen L, Eriksson J, Johansson G, Stâhlberg F, et al. Muscle sizes and moment arms of rotator cuff muscles determined by magnetic resonance imaging. Cells Tissues Organs. 2000;167:214–22. doi: 10.1159/000016784. [DOI] [PubMed] [Google Scholar]
- 29.Fox JA, Noerdlinger MA, Romeo AA. Arthroscopic subscapularis repair. Tech Shoulder Elbow Surg. 2003;4:154–68. [Google Scholar]
- 30.Yoo JC, Ahn JH, Koh KH, Lim KS. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25:1093–100. doi: 10.1016/j.arthro.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 31.Reilly P, Amis AA, Wallace AL, Emery RJ. Supraspinatus tears: propagation and strain alteration. J Shoulder Elbow Surg. 2003;12:134–8. doi: 10.1067/mse.2003.7. [DOI] [PubMed] [Google Scholar]
- 32.Yao L, Metha U. Infraspinatus muscle atrophy: Implications? Radiology. 2003;226:161–4. doi: 10.1148/radiol.2261011818. [DOI] [PubMed] [Google Scholar]
- 33.Rokito AS, Cuomo F, Gallagher MA, Zuckerman JD. Long-term functional outcome of repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg Am. 1999;81:991–7. doi: 10.2106/00004623-199907000-00012. [DOI] [PubMed] [Google Scholar]


