Abstract
Background:
Adolescents experience rapid biological, psychological, and social transitions that can be associated with mental health problems. During the high school period there are also more academic stressors.
Objective:
(1) To study the prevalence of mental disorders in high school (grade 12) students. (2) To study some related sociodemographic data.
Materials and Methods:
A cross-sectional study, using GHQ-28, that included 354 students randomly selected from grade 12 in four high schools – two male and two female high schools – in the National Guard Housing (Iskan), in Kashmalaan (suburb of Riyadh).
Results:
The overall prevalence of mental disorders was found to be 48% (41% in males and 51% in females); more than 80% of these cases were mild to moderate. Females showed significantly more severe disorders than males (P = 0.017) and students with excellent performance degrees showed a significantly lower rate of mental disorders than others (P = 0.021). However, our study did not show a significant association between psychiatric disorders and other social variables (family size, birth order, and polygamous family) or smoking.
Conclusion:
The adolescent age groups in our community had high rates of mental disorders, which required more attention from the family, as well as the educational and health institutes in our country.
Keywords: Adolescents, GHQ-28, high school students, mental disorder, prevalence, Saudi Arabia
INTRODUCTION
Young people can have mental, emotional, and behavioral problems that are real, painful, and expensive. These disorders are a source of stress for adolescent as well as his family, school, community, and larger society in the short and long term.[1,2]
Mental health problems for adolescents refer to the range of all diagnosable emotional, behavioral, and mental disorders. They include depression, anxiety, adjustment, conduct, eating disorders, and others.[3–5]
This group (adolescent) is most vulnerable to psychological disturbances, and their risk of psychiatric ill health is higher than that of any other easily identified group in our society and studies have consistently shown a high incidence of emotional and behavioral problems at such an age.[1,2,4,6]
The period of life between 10 and 19 years of age — which is the definition of the adolescence period by the Worl Health Organization (WHO) — is one of rapid biological, psychological, and social developmental transitions, associated with a need for independence, autonomy, identity formation, and privacy expectations, also there is an increased concern of peer acceptance and relationship, loneliness and shyness, more attention to medical issues like menstrual disorders, short stature, acne, body image, and weight disorders. During this period there is an increased morbidity in mental health problems, and compared to childhood there is an increased rate of depression, with more suicides and para-suicides among young people.[1,2]
The reported prevalence of mental or psychiatric disorders among adolescents, vary from study to study and from place to place. In western countries, the prevalence of mental health problems among adolescents has been reported to be between 2 and 56%.[1,7–9] In Arab countries the studies in this age group are limited, one study done in United Arab Emirates estimate that 24% of the children and adolescents are suffering from emotional and behavioral problems.[10]
The aim of this study is to study the prevalence of mental disorders in high school students. Having this information for this particular age group is important to influence policy and planning for better mental health care development, service, and even prevention.
MATERIALS AND METHODS
This is a cross-sectional study, investigating the prevalence of mental disorders in third year level high school students (twelfth grade), in National Guard Housing (Iskan city), in Kashmalaan (a suburb of Riyadh). The study was done during the first week of January 2003.
The study population was made up of all the twelfth grade high school male and female students, their total number was 785 students distributed in four schools, two male schools (302 students) and two female schools (483 students).
The study population had several unique characteristics: The responsible person or the guardian in the family (father or others) was a soldier in the National Guard; all lived in the same catchment area, with similar houses and an almost similar family income, also all the families were relatively recently settled tribal families, with low parental educational level. The sample size calculated was: 365 students.
The subjects were selected from the four schools according to their proportion, then from each school, by systematic random sampling from the alphabetical students list in these schools.
The data was collected by using the General Health Questionnaire (GHQ), which was a self-administered screening instrument, designed to detect the current diagnosable psychiatric disorders. It was used in the surveys and clinical settings to identify the potential cases, leaving the task of diagnosing the actual disorders to a psychiatric interview.[4,11]
The GHQ-28 item version was introduced incorporating the four subscales of somatic, anxiety, social dysfunctions, and severe depressive symptoms.[4] See Table 1 for information about subscales.
Table 1.
Subscales of GHQ and some of their characteristics
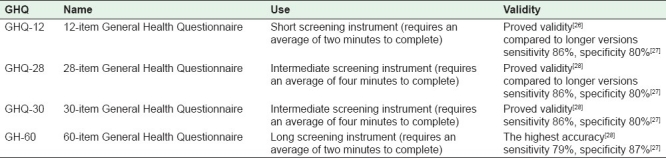
Compared to other versions of the GHQ-short versions; 12 and 30 — the 28 item version was found to be the best in sensitivity (100%), specificity (81.9%), and overall misclassification rate (17.5%), when used in the 4 / 5 caseness threshold score.[4]
The GHQ-28 was translated to Arabic and validated in the King Khaled University Hospital in Riyadh.[12]
Each questionnaire consisted of two sections: (1) Information about the sociodemographic characteristics and (2) the GHQ-28 described earlier.
RESULTS
The response rate was 97% of the sample size (354 students out of 365).
The numbers of females were more than males (61% females and 39% males) [Table 2].
Table 2.
Sample characteristics
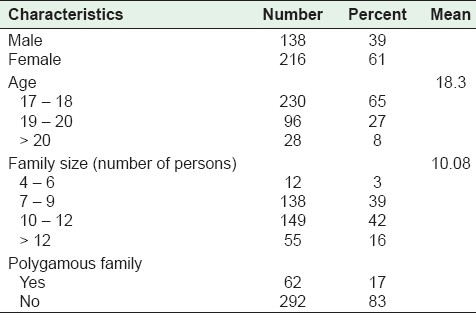
The age of the students ranged between 17 and 24 years, 65% of the sample was aged between 17 and 18 and 27.4% between 19 and 20 years – mean age was 18.3 (SD ± 1.07).
The family size (number of family members including father, mother, and siblings living in the same house) of the participants was high; 10 to 12 persons 42.1% and seven to nine persons 38.7% — with a mean of 10.08 (SD ± 2.33) and a maximum of 21 and minimum of 4. The mean of the participants birth order (between the siblings) was 3 (SD ± 1.39), with 17.2% of the students’ fathers having more than one wife (polygamous family). Their school performance was assessed by two questions; the first was about their grade when they passed last year, the second, if they had failed during high school; about 80% were good and very good and only 13.8% failed during high school. Finally about 7% of the participants were cigarette smokers and 92% of those were males.
The overall prevalence of psychiatric disorders was 48% (41% in males and 51% in females).
Regarding the severity of psychiatric disorders (mild score 5 – 8, moderate score 9 – 12, severe score > 12) 52% of cases were mild, 30% moderate, and 18% severe. The highest scoring in both genders was on the psychosocial subsection than on the anxiety subsection, followed by somatic subsection, and finally depression subsections.
Table 3 shows that females have more psychiatric disorders than males (51 and 41%, respectively) however, this difference was marginally statistically significant (P = 0.064). Interestingly there was significant difference between the two genders in the severity of psychiatric disorders (P = 0.017), females psychiatric disorders being more severe than males, but there were no significant differences in the subscale scoring between the two genders, except in the social dysfunction scale (P = 0.026), again females were more than males.
Table 3.
The relation between psychiatric disorder and some variables
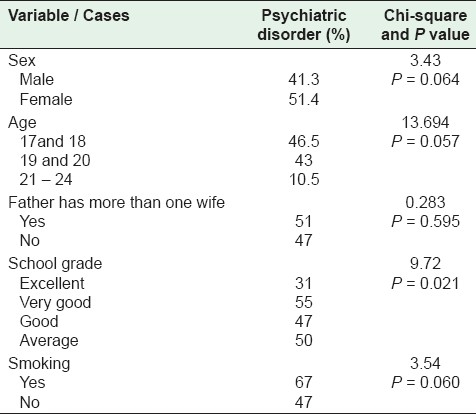
Students aged 21 years and above had the highest prevalence rate of psychiatric disorders, 86%, but with other age groups the overall relation between the age and psychiatric disorders was marginally statistically significant (P value = 0.057).
There was a statistically significant (P = 0.021) relation between school grade and cases, especially in excellent students, where psychiatric disorders were only 31% in this group. However, the relation between school failure (repeating grade12) and the cases were not statistically significant (P = 0.389).
Our result did not find a statistically significant relation between the cases and the family size, birth order, and father having more than one wife.
Finally our study shows a trend of a higher rate of smoking among those with psychiatric disorders, although this relation was again marginally statistically significant (P = 0.060).
DISCUSSION
Numerous studies have been conducted on the prevalence of psychiatric disorders in adolescents worldwide. Findings often revealed a very wide range of prevalence rates among these studies, for example Robert and Attkison, after reviewing 52 studies, reported a prevalence rate ranging from 1 to 51%.[13]
This very wide prevalence rate was due to many factors, mainly the difference in case definition, methodology, and how the information was obtained (self-reported questionnaire, information from parents or teachers, by interview or others). Usually studies based on self-reported questionnaires, which depended mainly on symptoms rather than psychiatric diagnosis, resulted in a higher prevalence rate than others.[2,14,15]
In our study we used a self-reported questionnaire (GHQ-28), which might have contributed to the overall high prevalence rate (48% in this age group).
This result was close to the results of other studies, which used the same tool. Winefield and Goldney reported a case prevalence rate of 40%,[16] Barodman[17] found a prevalence of 43% (both used GHQ-28), and Mc Pherson and Hall found a 48% prevalence rate (used GHQ-12).[18] Okash A, reported 51.7% psychiatric morbidity among Egyptian adolescents.[19] In Sudan Younis described a prevalence of up to 29% in children in the primary care setting.[20]
There are many other methods for diagnosing psychological disorders, for example, the CPS-depression scale, but this scale is used only for depression, Camacho et.al., found that the prevalence of major depression (only major depression) among adolescents was 11.5%.[21]
The other possible reasons for the high prevalence rate in our study were, first; the sociodemographic characteristics of this population. Being settled tribal families, they had gone through tremendous cultural and social changes within a relatively short period of time, and the urbanization was associated with increased psychiatric disorder rates.[22] The large family size and low educational level of the parents were associated with increased psychiatric disorder rates.[8,23] Second, this study was done on a specific group of adolescents (those in the final year of high school), which is a critical period in a student's life – a lot of stress to get a high degree in school added to this. The study was carried out few weeks prior to the midterm examinations, which could have been a factor contributing to added stress and probably resulting in a higher prevalence.
Previous studies showed that older adolescents had higher psychiatric disorder rates,[8] and that was the case in our study too, although it was not statistically significant.
Our results supported the previous studies that females had higher psychiatric disorder rates than males[11,14] (female 51% versus males 41%), also the severity of psychiatric disorders was significantly (P = 0.017) higher in females than males, which supported the results of other studies.[8]
Regarding family size, polygamous family, and birth order, they all failed to show a statistically significant relationship between the rates of psychiatric disorders in the adolescent, however, Panyayong demonstrates that one of the factors that is significantly associated with psychiatric disorders is family size with more than four children.[23]
When it came to academic performance, our results showed a significant relationship between the degree of school performance and rate of psychiatric disorders (P = 0.021); students with high degrees (excellent) had the lowest rate of psychiatric disorders, this might be because high degree students were mentally more stable and had more self-confidence than the others. Fleming, Offord, and Boyle and other studies have also described a considerable relationship between mental health and school performance.[24] Surprisingly there was no significant association between the rate of psychiatric disorders and school failure, although students aged 21 – 24 years (likely frequent failures) were found to have a high rate of psychiatric disorders — only 4% of the sample size with 86% rate of psychiatric disorders — which might question the reliability of answering this variable (failure is a sensitive issue and admitting it may be difficult, especially when answering a self-reported questionnaire).
Many studies confirmed the association between psychiatric disorders and smoking;[8,24,25] our study showed a high prevalence rate of psychiatric disorders within smokers, but this association was marginally statistically significant. This was probably due to the fact that the questionnaires were filled inside the school; this might have prevented some students from answering the part on smoking openly.
Although the sample size was appropriate for the school population it was relatively small and might be the reason for the failure of illustrating the relationship between psychiatric disorders and some of the variables studied. Another limitation was that in this study we used GHQ-28, which was a self-reported questionnaire that depended on symptoms rather than specific psychiatric diagnosis for case detection, which might have overestimated the prevalence of psychiatric disorders. Finally, the narrow age range and academic level of the study sample might limit the generalization of the results of the adolescents’ age group.
CONCLUSION
The overall prevalence of psychiatric disorders in high school students using GHQ-28 was 48%, and was more in females (51%) than males (41%). Females showed significantly more severe disorders than males (P = 0.017), and students with a high degree showed a significantly lower rate of mental disorders than others (P = 0.021). However, this study showed no clear association between psychiatric disorders and other social variables (family size, polygamous family, and birth order) or smoking.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Lawrence SN. Adolescent health care a practical guide. 3rd ed. London: Edward Arnold; 1996. pp. 225–7. [Google Scholar]
- 2.Jacobson L, Churchill R, Donovan C, Garrarda E, Fay J. Tackling teenage turmoil: Primary care recognition and management of mental ill health during adolescence. Fam Pract. 2002;19:401–9. doi: 10.1093/fampra/19.4.401. [DOI] [PubMed] [Google Scholar]
- 3.McCann JB, James A, Wilson S, Dunn G. Prevalence of psychiatric disorders in young people in care system. BMJ. 1996;313:1529–30. doi: 10.1136/bmj.313.7071.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferwana MS. Effect of psychiatric training course on GPs ability to detect psychiatric disorders, and their attitudes toward these disorders. (Thesis) 2000;28:52–4. [Google Scholar]
- 5.SAMHSAs National Mental Health Information Center. Mental, Emotional, and Behavioral Disorders in Children and Adolescents. US Department of Health and Human Services. 2001 [Google Scholar]
- 6.Kramer T, Gerald ME. Child and adolescent mental problems in primary care. Adv Psychiatr Treat. 2000;6:287–94. [Google Scholar]
- 7.Xianchen L. Behavioral and emotional problems in Chinese Adolescent. J Am Acad Child Adolesc Psychiatry. 2001;40:64–78. doi: 10.1097/00004583-200107000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Helen RW, Robert DG, Anthony HW. The General Health Questionnaire: Reliability and validity for Australian youth. Aus N Z J Psychiatry. 1989;23:53–8. doi: 10.3109/00048678909062592. [DOI] [PubMed] [Google Scholar]
- 9.Fichter MM, Elton M, Diallina M, Koptagel-Ilal G, Fthenakis WE, Weyerer S. Mental illness in Greek and Turkish adolescent's. Eur Arch Psychiatry Neurol Sci. 1988;237:125–34. doi: 10.1007/BF00451279. [DOI] [PubMed] [Google Scholar]
- 10.Al-Gazali M. Emotional and behavioral problems among school children in United Arab Emirates. J Am Acad Child Adolesc Psychiatry. 1998;37:880–6. doi: 10.1097/00004583-199808000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Walker Z, Townsend J. Promoting adolescent mental health in primary care a review of literature. J Adolesc. 1998;21:621–34. doi: 10.1006/jado.1998.0183. [DOI] [PubMed] [Google Scholar]
- 12.Al-Fares EA, Al-Shammari SA, Al-Hamad IS. Prevalence of psychiatric disorders in an academic primary care center in Riyadh. Saudi Med J. 1992;13:49–53. [Google Scholar]
- 13.Feijo RB, Saueressing M, Salazar C, Chaves ML. Mental health screening by self reported questionnaire among community adolescents in southern Brazil. J Adolesc Health. 1997;20:232–7. doi: 10.1016/S1054-139X(96)00085-7. [DOI] [PubMed] [Google Scholar]
- 14.Romano E, Trembly RE, Vetaro F, Zoccolillo M, Pajani L. Prevalence of psychiatric diagnosis and role of perceived impairment finding from adolescent community sample. J Child Psychol Psychiatry. 2001;42:451–61. [PubMed] [Google Scholar]
- 15.Tomori M, Zalar B, Plesnicar BK. Gender differences in psychosocial risk factors among Slovenian adolescents. Adolescence. 2000;35:431–43. [PubMed] [Google Scholar]
- 16.Winefield HR, Goldney RD, Winefield AH, Tiggemann M. The General Health Questionnaire: reliability and validity for Australian youth. Australian and New Zealand Journal of Psychiatry. 1989;23:53–8. doi: 10.3109/00048678909062592. [DOI] [PubMed] [Google Scholar]
- 17.Baordman AP. The General Health Questionnaire and the detection emotional disorders by the GP. Br J Psychiatry. 1987;151:373–81. doi: 10.1192/bjp.151.3.373. [DOI] [PubMed] [Google Scholar]
- 18.NIMH study measures prevalence of mental illness in US. Am Fam Physician. 1985;31:261–2. [PubMed] [Google Scholar]
- 19.Okasha A, Ragheb K, Attia AH, Seif el Dawla A, Okasha T, Ismail R. Prevalence of obsessive compulsive symptoms (OCS) in a sample of Egyptian adolescents. Encephale. 2001;27:8–14. [PubMed] [Google Scholar]
- 20.Giel R, de Arango MV, Climent CE, Harding TW, Ibrahim HH, Younis YO. Childhood mental disorders in primary health care: Results of observations in four developing countries. Pediatrics. 1981;68:677–83. [PubMed] [Google Scholar]
- 21.Camacho PA, Rueda-Jaimes GE, Latorre JF, Navarro-Mancilla AA, Escobar M, Franco JA. Validity and reliability of the Center for Epidemiologic Studies-Depression scale in Colombian adolescent students. Biomedica. 2009;29:260–9. [PubMed] [Google Scholar]
- 22.Panyayong B, Wachrasindhu A. Psychiatric disorders in Thai school aged children: Associated factor. J Med Assoc Thailand. 2002;85(Suppl 1):S137–47. [PubMed] [Google Scholar]
- 23.Fleming JE. Prevalence of childhood and adolescent depression in the community. Br J Psychiatry. 1989;155:647–54. doi: 10.1192/s0007125000018146. [DOI] [PubMed] [Google Scholar]
- 24.Lisa CD. The association between psychiatric disorders and the progression of tobacco use behaviors. J Am Acad Child Adolesc Psychiatry. 2001;40:1159–69. doi: 10.1097/00004583-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Upadhayaya HP, Deas D, Brady KT. Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41:1294–305. doi: 10.1097/00004583-200211000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–7. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 27.Consultation-liaison psychiatry in Germany, Austria and SwitzerlandScreening instruments for general hospitals and primary care. Albert Diefenbacher. Karger. 2004:77. [Google Scholar]
- 28.Burvill PW, Knuiman MW. Which version of the general health questionnaire should be used in community studies? Aust N Z J Psychiatr. 1983;17:237–42. doi: 10.3109/00048678309161279. [DOI] [PubMed] [Google Scholar]


