Abstract
Objectives:
To determine the prevalence of metabolic syndrome among obese patients using the IDF definition and to identify factors that are associated with it.
Materials and Methods:
A cross-sectional randomized study was conducted at four primary care centers inside Doha, Qatar. One hundred and thirty-six Adults, ≥ 18 Qatari obese patients, were chosen by systematic random sampling. They were interviewed and screened for the presence of metabolic syndrome, which was diagnosed according to the International Diabetes Federation criteria: An abdominal circumference ≥ 94 cm in males or ≥ 80 cm in females, plus any two of the following: HDL cholesterol < 1.03 mmol / mL (< 40 mg / dL) [males] or < 1.3 mmol / mL (< 50 mg / dL) [females], Triglycerides ≥ 1.7 mmol / mL (≥150 mg / dL), Blood pressure ≥ 130 / 85 mmHg or the patient receiving antihypertensive treatment and baseline glycemia > 5.6 mmol / mL (> 100 mg / dL), or previously-diagnosed type 2 diabetes mellitus.
Results:
The overall prevalence of the metabolic syndrome among obese patients was 46.3%. The prevalence was higher in females (50%) than in males (42.4%). It was seen to increase with increasing body mass index class, from class 1 to class 2. The prevalence of metabolic comorbidities of abnormal waist circumference, raised blood pressure, raised fasting blood glucose, high triglycerides, and reduced high density lipoprotein was 88.2, 42.6, 32.4, 31.6, and 27.9%, respectively. Based on the logistic regression multivariable analysis, increasing age and being diabetic were the only significant associated factors that influenced the risk of having the metabolic syndrome.
Conclusion:
The prevalence of the metabolic syndrome was high, and the highest comorbidities were abnormal waist circumference and high blood pressure. Diabetes and increasing age were the only significant risk factors of having this syndrome.
Keywords: Blood glucose, high density lipoprotein, metabolic syndrome, obesity, triglycerides
INTRODUCTION
The metabolic syndrome has been described as a ‘clustering’ of several risk factors for cardiovascular disease, obesity (particularly abdominal obesity), dyslipidemia, insulin resistance, and hypertension. Globally, the incidence of this syndrome is rising at an alarming rate.[1] Obesity is a public health concern because of its association with a number of medical complications that lead to increased morbidity and mortality. The most common obesity-related complications are type-2 diabetes mellitus, hypertension, dyslipidemia, cardiovascular diseases, gallstones and cholecystitis, respiratory dysfunction, non-alcoholic chronic liver disease, and certain cancers.[2] The prevalence of the metabolic syndrome is increasing because of the ‘obesity epidemic.’[3] The increased prevalence of obesity has been accompanied by a parallel increase in the prevalence of the metabolic syndrome. The metabolic syndrome, which is associated with three-fold and two-fold increases in type-2 diabetes mellitus and cardiovascular disease, respectively, has become a major public health challenge around the world.[4] Research is urgently required to elucidate the prevalence and associated risk factors, in countries where it had not been estimated yet. There is very minimal data available on the prevalence of the metabolic syndrome in obese patients.[5] Furthermore, few systematic data are available on the prevalence of the metabolic syndrome in obese persons from the most recent worldwide criteria of the International Diabetes Federation (IDF) metabolic syndrome definition.[6] The objectives of this study are to determine the prevalence of the metabolic syndrome among obese patients using the IDF definition and to identify the factors that are associated with the metabolic syndrome among these patients.
MATERIALS AND METHODS
Study design
The aim of this cross-sectional study was to measure the prevalence of metabolic syndrome among obese Qataris attending the primary health care centers in Doha. The subjects of the study were the attendants of primary health care centers who were selected through a multiple-stage sampling procedure. First, four primary care centers were chosen randomly from the four different regions of Doha city; the northern, southern, central, and western regions.
Inclusion and exclusion criteria
One of every three clients who visit the health center and fulfill the inclusion criteria: age > 18 years and obese (≥ BMI 30 kg/m2) were invited to participate in the study. Exclusion criteria were underlying endocrine diseases such as Cushing's disease, acromegaly, hypothyroidism, hypogonadism, patients on prolonged steroid use, and those who were on active drug treatment for obesity at the time of recruitment.
Sample size
Sample size determination was conducted by the Epi-info stat-calculator, and was calculated as 148 subjects considering a 10% dropout.
Instruments and data collection
The questionnaire portion of this study was designed to be quick and easy to fill out by the researchers. It was validated through professional review and piloting. It was translated from English to Arabic, and then translated again from Arabic to English, to ensure language consistency. It had two sections, one describing the personal characteristics, and the other questioning the different risk factors of the metabolic syndrome. It was administered via a face-to-face interview. The anthropometric measurements included body weight; height and girth were taken with the subjects in light clothing and without shoes. Height was measured to the nearest 0.1 cm. Weight was measured to the nearest 0.1 kg. Body mass index was computed as the ratio of weight (kg) to the square of height (m) (kg/m2). Waist circumference was defined as the average of two measurements taken after normal expiration to the nearest 0.1 cm at the midpoint between the lowest rib and the iliac crest. Blood pressure was measured on the right arm, with the subject in a sitting position, after a minimum five-minute rest, using a standard mercury sphygmomanometer. Two consecutive measures of systolic and diastolic blood pressure were recorded to the nearest 2 mmHg. The second blood pressure recording was performed at least one minute after the first one. The mean value of the two blood pressure readings was taken into account. Subjects were asked to fast for 12 hours before blood sampling. They were also asked to refrain from smoking for 12 hours before blood draws. A 20-ml blood sample was drawn on disodium Ethylenediaminetetraacetic acid (EDTA) kept at room temperature, and centrifuged within four hours. Samples were analyzed on the same day. Glucose was measured by the glucose oxidase method. Serum triglyceride and HDL levels were measured enzymatically. Metabolic syndrome was diagnosed according to the IDF definition, which was the presence of central obesity: Abdominal circumference ≥ 94 cm in males or ≥ 80 cm in females, plus any two of the following: HDL cholesterol < 1.03 mmol/mL (< 40 mg/dL) [males] or < 1.3 mmol/mL (< 50 mg/dL) [females], Triglycerides ≥ 1.7 mmol/mL (≥ 150 mg/dL), Blood pressure ≥ 130 / 85 mmHg or the patient receiving antihypertensive treatment, and baseline glycemia > 5.6 mmol/mL (> 100 mg/dL), or previously-diagnosed type 2 diabetes mellitus.
Data analysis
The collected data was entered into the SPSS software (version 16). For cross-tabulation and computation, statistical significance using 95% confidence interval (CI) was calculated. A Chi-square test was used for the comparison of different categorical groups with a p-value < 0.05 considered to be significant. Unavailable and multivariable binary logistic regression analyses were used to identify factors that were significantly associated with the metabolic syndrome among obese patients. The findings were presented with the adjusted odds ratio (OR), its 95% confidence interval (CI), and the corresponding P-values.
Ethical considerations
Approval of the research as well as the National Ethical Committee was done. Informed consent was signed by the participants after explanation of the purpose of the study, the direct and indirect benefits and risks as well as confidentiality of the collected data, with their rights to withdraw at any stage of the study.
RESULTS
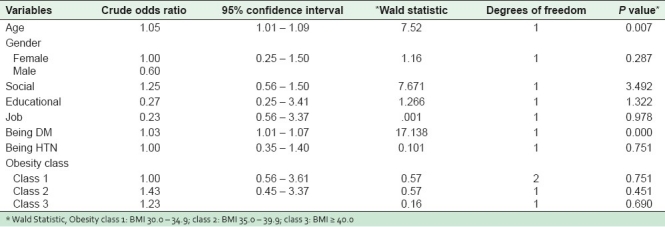
A response rate of 91.9% was achieved in this study as 136 adults had successfully completed the study, from them 48.5% were males and 51.5% females. Near half of them, 48.5%, had passed the primary, secondary school levels, while 22.1% had passed the university level, and 29.4% were illiterate. More than three-quarters of them were married, 77.9%. With regard to the working status, only 34.6% were working, as shown in Table 1. The mean (SD) age of the studied group was 45.2 (12.9), the mean (SD) height of the studied group was 163.2 (10.5), the mean weight (SD) was 101 (23.3), the mean (SD) waist circumference was 111.3 (13.8), and the mean (SD) of their BMI was 37.8 (6.8), as shown in Table 2. The BMI of 44.9% of the studied population was less than 34.9, the BMI of 23.5% was between 35 and 39.9, while 31.6% had morbid obesity [Table 3]. The overall prevalence of the metabolic syndrome was 46.3%. By gender, the prevalence was 42.4% among males and 50% among females. However, there was no significant difference in the prevalence between males and females [Table 4]. The prevalence of metabolic comorbidities of abnormal waist circumflex, raised blood pressure, raised fasting blood sugar, high triglycerides, and reduced high-density lipoprotein was 88.2, 42.6, 32.4, 31.6, and 27.9%, respectively [Table 5]. The results of simple binary logistic regression analysis for potential associated factors of the metabolic syndrome were DM and increasing age, which were the only independent variables that were statistically significant in the multivariate analysis, using multiple binary logistic regressions [Table 6].
Table 1.
Frequency distribution of the studied population according to demographic characteristics (n = 136)
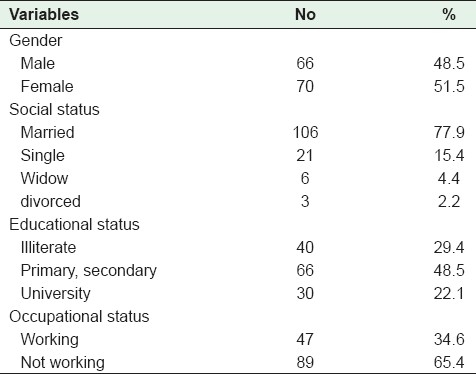
Table 2.
Physical characteristics of the studied group (n = 136)
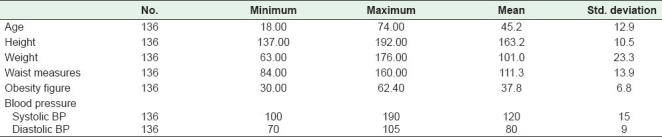
Table 3.
Prevalence of obesity class among the studied population (n = 136)
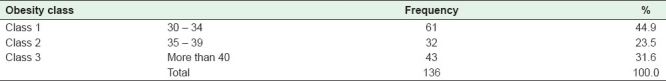
Table 4.
Prevalence of metabolic syndrome among the studied population by gender (n = 136)
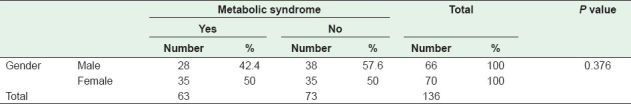
Table 5.
Prevalence of metabolic comorbidities among the studied population (n = 136)
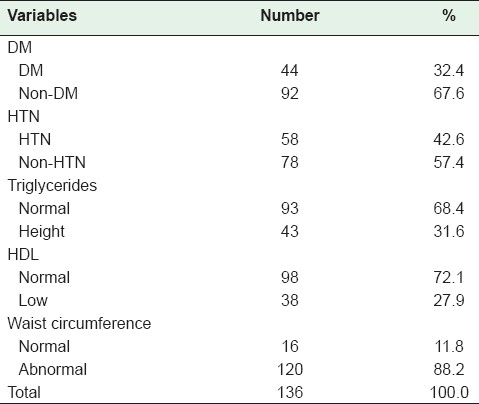
Table 6.
Associated factors of the metabolic syndrome using simple binary logistic regression (n = 136)
DISCUSSION
In the current study, the overall prevalence of the metabolic syndrome among obese Qatari adults, attending primary health care centers was 46.3%, which was constant, with a previous finding from a study among obese Kuwaiti adults, which was 46.8% using NECP ATP III.[7] The prevalence in the current study was higher than the prevalence among obese adults attending the obesity clinic in Malaysia, which was 40.2% using the IDF definition of the metabolic syndrome,[8] but was considerably lower than that in other comparable studies in obese patients conducted in Italy (53%) and Taiwan (50.7%).[9,10] The differences in prevalence might be due to the different definition used for the criteria of the metabolic syndrome in the different study populations. The studies in Italy and Taiwan used the National Cholesterol Education Program Adult Treatment Panel (NCEP ATP) III definition,[9,10] while the NCEP ATP III criteria were similar to the IDF criteria, except that central obesity was not a mandatory criteria, unlike that proposed by the IDF. This might give rise to a higher prevalence of the overall metabolic syndrome in the studies using the NCEP ATP III definition.[11,12] The current study showed that prevalence of the metabolic syndrome among females (50%) was higher than males that in males (42.4%), which was consistent with Marchesini et al., who reported a prevalence of 56.7% in females, compared to 51.9% in males.[9] Similarly, Lee et al. found a higher prevalence among females at 31.9%, and 20.5% among males, but found that males were significantly associated with an increased risk of having the metabolic syndrome.[10] However, the present study and the study conducted by Marchesini et al.[9] did not find a similar association. Population-based studies have also shown that the prevalence of the metabolic syndrome using the IDF criteria tended to be higher in females.[13,14] The current study showed that the prevalence of the metabolic syndrome was noted to increase from obesity class 1 to 2, although the prevalence in obesity class 3 was slightly lower. Similarly in NHANES III, the metabolic syndrome was present in 5% of those with normal weight, 22% in those who were overweight, and 60% in those who were obese.[15] A large waist circumference alone identified up to 46% of the individuals who would develop the metabolic syndrome within five years.[16] A similar finding was seen by Marchesini et al., who showed that the prevalence of the metabolic syndrome in their obese subjects increased with a rising obesity class and the metabolic syndrome was significantly associated with BMI.[5] However, the metabolic syndrome was not significantly associated with the BMI class in the current study. The prevalence of individual metabolic comorbidities of the metabolic syndrome in the current study, according to the IDF definition, was abnormal waist circumflex, raised blood pressure, raised fasting blood sugar, high triglycerides, and the reduced high density lipoprotein was 88.2, 42.6, 32.4, 31.6, and 27.9%, respectively. Similar findings were observed in US NHANES III 2003–2006 survey indicating a high prevalence of components of the metabolic syndrome, as defined by ATP III. Among the 3423 adults, abdominal obesity was present in 53%, elevated blood pressure in 40%, and hyperglycemia in 39%. These were the most frequently occurring risk factors for the metabolic syndrome, regardless of whether one examined the crude or age-adjusted estimates. A smaller percentage of adults had elevated TG (31%) and low HDL (25.1%).[17] Insulin resistance was the common proposed mechanism linking obesity and hypertension.[18] An analysis of the 1998 Singapore National Health Survey found that the hypertension factor was positively loaded for obesity. This finding was in-keeping with the existing knowledge that obesity was clearly linked to essential hypertension.[19] Age and being diabetic were the only significant associated factors found to influence the odds of having the metabolic syndrome in this study. This finding was consistent with other comparable studies.[9,10] Marchesini et al. reported that the odds of having the metabolic syndrome increased by 1.43 (95% CI 1.32–1.56) for every ten-year age increment.[9] This was also inconsistent with the results of (NHANES III,1988–1994), which showed that at the baseline, the prevalence of the metabolic syndrome was 26.8% in men and 16.6% in women. After eight years of follow-up, there was an age-adjusted 56% increase in prevalence among men and a 47% increase among women.[20] Also many studies reported that most of diabetic patients with type 2 diabetes had features of the metabolic syndrome.[21]
Limitations of the study
The relatively small sample that was chosen from patients who attended the primary care centers made it difficult to generalize the results from this study, so a population-based study with a large sample was needed.
CONCLUSION
The prevalence of the metabolic syndrome among obese patients using the IDF definition was high; it was higher among females and significantly increased with the presence of diabetes and increase in age. The abnormal waist circumference, raised blood pressure, and raised fasting blood sugar were the most common metabolic comorbidities found in obese patients followed by high triglycerides and reduced HDL. In the future such findings should be taken into account when planning for new or expansion of existing health services and when implementing future non-communicable disease prevention and control programs.
Footnotes
Source of Support: Nil
Conflict of Interest: The author declares that there are no competing interests
REFERENCES
- 1.Anne PN. The metabolic syndrome. British Nutrition Foundation Nutrition Bulletin. London, UK: British Nutrition Foundation; 2004. pp. 36–43. [Google Scholar]
- 2.Liberopoulos EN, Mikhailidis DP, Elisaf MS. Diagnosis and management of the metabolic syndrome in obesity. Obes Rev. 2005;6:283–96. doi: 10.1111/j.1467-789X.2005.00221.x. [DOI] [PubMed] [Google Scholar]
- 3.Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome: A global public health problem and a new definition. J Atheroscler Thromb. 2005;12:295–300. doi: 10.5551/jat.12.295. [DOI] [PubMed] [Google Scholar]
- 4.The World Health Report 2004: Obesity: Preventing and managing the global epidemic. Geneva: World Health Organization; 2004. World Health Organization (WHO) [PubMed] [Google Scholar]
- 5.Malaysian Association for the Study of Obesity (MASO) Strategy for the prevention of obesity - Malaysia. MASO. 2005 [Google Scholar]
- 6.International Diabetes Federation. Rationale for new IDF worldwide definition of metabolic syndrome. International Diabetes Federation. 2005 [Google Scholar]
- 7.Al-shiji S, Fakhar Osama A, Gamal M. Metabolic syndrome among adult attending obesity clinics in kuwit. Alexandria Bulln. 2007;43:3. [Google Scholar]
- 8.Termizy HM, Mafauzy M. Metabolic syndrome and its characteristics among obese patients attending an obesity clinic. Singapore Med J. 2009;50:390–4. [PubMed] [Google Scholar]
- 9.Marchesini G, Melchionda N, Apolone G, Cuzzolaro M, Mannucci E, Grossi E. The metabolic syndrome in treatment-seeking obese persons. Metabolism. 2004;53:435–40. doi: 10.1016/j.metabol.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Lee WJ, Chen HH, Wang W, Wei PL, Lin CM, Huang MT. Metabolic syndrome in obese patients referred for weight reduction surgery in Taiwan. J Formos Med Assoc. 2003;102:459–64. [PubMed] [Google Scholar]
- 11.Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the U.S. Diabetes Care. 2005;28:2745. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 12.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 13.Kim HM, Kim DJ, Jung IH, Park C, Park J. Prevalence of the metabolic syndrome among Korean adults using the new International Diabetes Federation definition and the new abdominal obesity criteria for the Korean people. Diabetes Res Clin Pract. 2007;77:99–106. doi: 10.1016/j.diabres.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Ko GT, Cockram CS, Chow CC, Yeung VT, Chan WB, So WY, et al. Metabolic syndrome by the international diabetes federation definition in Hong Kong Chinese. Diabetes Res Clin Pract. 2006;73:58–64. doi: 10.1016/j.diabres.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2003;163:427–36. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palaniappan L, Carnethon MR, Wang Y, Hanley AJ, Fortmann SP, Haffner SM, et al. Insulin Resistance Atherosclerosis Study Predictors of the incident metabolic syndrome in adults: The Insulin Resistance Atherosclerosis Study. Diabetes Care. 2004;27:788–93. doi: 10.2337/diacare.27.3.788. [DOI] [PubMed] [Google Scholar]
- 17.Ervin RB. Division of Health and Nutrition Examination Surveys. Prevalence of Metabolic Syndrome Among Adults 20 Years of Age and Over, by Sex, Age, Race and Ethnicity, and Body Mass Index: United States, National Health Statistics. [Last accessed on 2009 May 13]. Available from: http://www.cdc.gov/nchs/data/nhsr/nhsr013 . [PubMed]
- 18.Eckel R, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 19.Ang LW, Ma S, Cutter J, Chew SK, Tan CE, Tai ES. The metabolic syndrome in Chinese, Malays and Asian Indians. Factor analysis of data from the 1998 Singapore National Health Survey. Diabetes Res Clin Pract. 2005;67:53–62. doi: 10.1016/j.diabres.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159:1104–9. doi: 10.1001/archinte.159.10.1104. [DOI] [PubMed] [Google Scholar]
- 21.Cull CA, Jensen CC, Retnakaran R, Holman RR. Impact of the metabolic syndrome on macrovascular and microvascular outcomes in type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study 78. Circulation. 2007;116:2119–26. doi: 10.1161/CIRCULATIONAHA.107.733428. [DOI] [PubMed] [Google Scholar]


