Abstract
Medicines are cost-effective interventions for the treatment and management of health problems. This research was carried out to determine the common health problems and medicine-use practices in treating health problems in Lamingo, Jos, Nigeria. A total of 109 households covering 676 individuals were recruited and followed up for a period of one month between 6 November 2010 and 11 December 2010. A structured interview was conducted on weekly visits to households to identify illnesses suffered by household members and treatment given. The results showed that 146 common health problems representing 1.3 cases per household per month were found. The cost of treatment per household per month was found to be $14.7. Infectious and parasitic diseases (44.6%), diseases of the digestive (11.0%) and respiratory system (9.6%) were common in the community. Self-medication was common (34.6%) and the patent medicine stores were the most common sources of medicines. Common classes of medicines used by community members were analgesics (23.6%), antimalarials (17.9%) and antibiotics (14.2%). Factors that influenced choice of treatment were previous knowledge and experience of family members with service provider and treatment (44.4%), cost (18.9%) and severity of condition (16.7%). There is, therefore, high occurrence of health problems and self-medication practices in the Lamingo community.
Keywords: Health problems, medicine-use practices, self-medication
INTRODUCTION
In Africa, communicable diseases are major causes of morbidity and mortality. Communicable diseases such as malaria, tuberculosis, HIV/AIDS, respiratory infections and the complications of pregnancy and child birth account for 72% of all deaths.[1] Nigeria is not an exception to this with a high burden of infectious diseases and a maternal mortality ratio of 545 per 100,000 live births.[2]
When people are sick, they either seek medical attention in health facilities or self-medicate. Some individuals take no treatment at all. Many individuals, however, self-medicate due to long waiting times in facilities, inaccessibility of health facilities, cost, and a feeling that the ailment is minor.[3,4] Studies have shown that 23% of the weekly household expenditure in Nigeria is spent on one episode of illness and consumers pay about 64 times the international reference price for medicines to obtain medications from facilities. Payment for healthcare is mainly out-of-pocket in Nigeria, with a few individuals benefiting from the national health insurance scheme.[5]
Medicines are cost-effective interventions for the treatment and management of health problems. Many countries have developed national formularies and treatment guidelines to ensure rational use of medicines. Inappropriate use of medicines in the treatment of common illnesses is a global problem and research has shown that more than 50% of all medicines are used irrationally.[6] This problem is worst in developing countries and has great health and economic consequences. Poor therapeutic outcome, increased adverse drug events, antimicrobial resistance and waste of scarce health resources have resulted from inappropriate use of medicines.[7] The use of medicines at the community level has been shown to be influenced by people's beliefs about their efficacy and safety, perceived need for medicines, cost, literacy level, information channels and confidence about health providers.[6]
An understanding of the occurrence of common health problems and medicine-use practices in the treatment of common health problems in a community is of public health importance. This can form the basis for advocacy, health promotion or policy review. This research was therefore carried out to determine the common health problems and the medicine-use practices in treating them in the Lamingo community, Jos, Nigeria.
MATERIALS AND METHODS
The study was conducted in Lamingo. Lamingo is a semi-urban community in Jos, Nigeria and has within it a Primary Health Centre, a teaching hospital, two community pharmacies and five patent medicine stores.
The study was approved by the ethical committee of the Faculty of Pharmaceutical Sciences, University of Jos, Jos, Nigeria.
A prospective study was carried out between 6 November 2010 and 11 December 2010. A total of 109 households covering 676 individuals were recruited through a systematic random technique and these households were followed up for a period of one month.
Five visits were made in all to each of the participating households. The first visit was to explain the aim and scope of the research to households and to seek their informed consent. Households were informed that information collected would be confidential and that no treatment would be given for any medical condition suffered by family members to avoid bias in reporting. Subsequent visits were made weekly for interviews. A structured interview was conducted guided by a pretested questionnaire containing close and open-ended questions as the data collection tool. The questionnaire was pretested in 15 households for a period of two weeks and adjusted to meet the stated objectives. The questionnaire used for this study was divided into four main domains. The first domain consisted of questions related to the demographic details of households; the second domain consisted of questions related to the illness suffered and illness-related medicine-use; the third domain consisted of questions related to sources of medicines and choice of treatment; and the fourth domain consisted of questions related to cost.
Households were interviewed weekly for information on health problem suffered by any member of the family in the past week, treatment given, sources of medicines, and factors that influenced their choice of treatment and cost of treatment.
The common disease conditions that occurred in the community during the study were classified according to the sub-categories of the International Statistical Classification of Diseases-10 (ICD-10) and the medicines used by the community members for the treatment of common illnesses were grouped according to their therapeutic class.
Data analysis
Data collected were entered into Statistical Package for Social Sciences (SPSS) Version 16 to generate descriptive statistics which were reported in percentages. The percentage of classes of health problems suffered by the community members was calculated by the number of health problems in a disease class suffered by community members divided by the total number of illness episodes reported during the survey and the resultant proportion was multiplied by 100. The number of illnesses suffered per household per month was calculated by the total number of illness episodes reported in the one month of the survey divided by the total number of households that participated in the study. The cost of treatment (per household per month) was calculated by dividing the sum of the individual cost of treatment reported by the community members in the one month of the survey with the total number of households that participated in the study and the value obtained was converted to US dollars using the official exchange rate at the time of the study.
A one-sample t-test between proportions was performed to determine whether there was a significant difference between the comparison groups. Qualitative data were read repeatedly and emerging themes were identified and coded.
RESULTS
The study population consisted of households of a mean size of 6.2 with the majority of the household heads (52.3%) having a secondary level of education. Only 11% of the households had family members who were benefiting from a health insurance scheme.
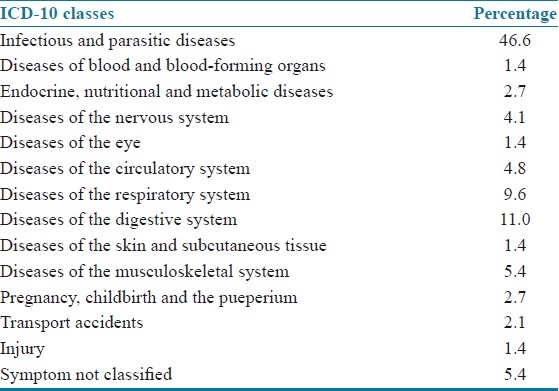
One hundred and forty-six common health problems were found in the 109 households studied within the period of one month. This represents 1.3 cases per household per month; 8.9% of the households did not report any illness during the period of study. Self-medication was common among the studied community. Only about 43% of treatments were sought from skilled health professionals (doctors, pharmacists and nurses) [Table 1]. The cost of treatment (in US dollars) per household per month was found to be $14.7. Infectious and parasitic diseases, diseases of the digestive and respiratory system were found to be the common health problems in the community [Table 2].
Table 1.
Healthcare providers from whom household members sought treatment
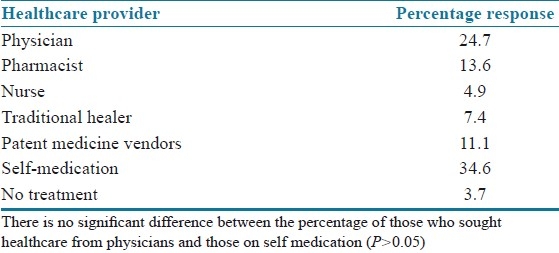
Table 2.
Common health problems present in the community
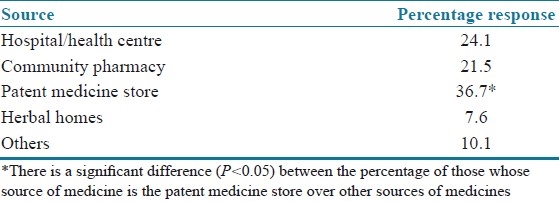
The common classes of medicines used by the community members during the study period were analgesics (23.6%), antimalarials (17.9%) and antibiotics (14.2%) [Table 3]. The patent medicine stores (36.7), hospitals/primary health centers (24.1) and the community pharmacies (21.5) were the common sources of medicines reported by study respondents. Statistical analysis showed that patent medicine store is the preferred sources of medicine among community members [Table 4].
Table 3.
Classes of medication used by community members in the treatment of common illnesses
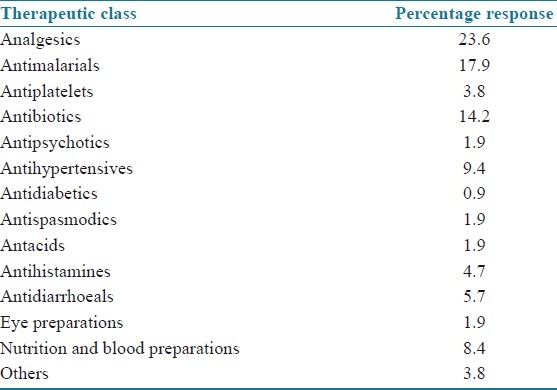
Table 4.
Sources of medicines used by community members
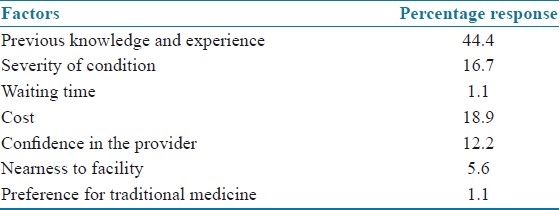
The common factors that influenced community members’ choice of treatment were previous knowledge and experience of patient about service provider and treatment (44.4%), cost (18.9%) and perceived severity of condition (16.7%) [Table 5].
Table 5.
Factors that influence choice of treatment
DISCUSSION
An understanding of the common illnesses and medicine-use practices in a community is important in designing public health interventions.
The average of 1.3 cases per household per month (about 91% of households reporting at least one health condition during the study period), with the majority of health problems being infectious and parasitic diseases is of public health concern. Although this is a reflection of the major burden of disease in Africa, most infectious and parasitic diseases are preventable and cost-effective measures exist for the prevention of these diseases. Such measures among others include the use of insecticide-treated bednets to prevent malaria, safe blood transfusion to prevent HIV/AIDS and other blood-borne infections, mass screening and chemotherapy.[1,8–10] Hence there is need for promoting these measures at the community level. This will help prevent ill health, save healthcare cost and reduce pressure due to these infections on scarce health resources.
The common classes of drugs procured by community members were analgesics, antimalarials and antibiotics. The procurement of antimalarials and antibiotics is a reflection of the high burden of infectious and parasitic diseases in the community. In addition, malaria is a major cause of morbidity in Nigeria. About 50% of the population has at least one episode of malaria annually, with children under five having an average of two to four attacks.[11]
About 70% of Nigerians live below $1 per day and payment for healthcare is made out-of-pocket.[5] The average monthly expenditure of $14.7 on medicines per household is high. Ill health depletes household resources and this will continue to put household members below the poverty line. Other direct and indirect non-medical costs such as transport, special food requirements, loss of working hours, were not covered by this research. Indirect cost due to an illness in Africa is high. For example, a sick adult would spend about one to five days out of work per malaria episode; and the value of lost working days due to malaria per episode has been estimated in Ghana, Sri Lanka, and Malawi to be $7.63, $4.78, and $1.54 respectively.[12] This shows that illness cost burdens on households are high.
People are increasingly taking responsibility of their health. Self-medication is common in developing countries and is a major cause of inappropriate use of medicines. The prevalence of Self-medication (34.6%) in the studied community is comparable to other community-based studies in Ethiopia (27.6%) and India (31.3%). In developing countries, individuals self–medicate with prescription medicines because individuals can purchase these medicines over-the-counter.[6] Our studies confirm this practice. Community members who self-medicated with prescription drugs got their medicines over-the-counter from community pharmacies and patent medicine stores. Research has shown that patent medicine stores are major sources of prescription medicines in Nigeria; however, they are not licensed to sell prescription medicines. Prescription medicines are those medicines that by regulation or policy are only issued to a patient with a prescription. This shows that the sales of pharmaceutical products in the country are under-regulated. The under-regulation of pharmaceutical products has led to high prevalence of fake medicines; high incidence of self-medication; adverse drug events; treatment failures; antimicrobial resistance; lack of public confidence in the drug market; protracted ill health and untimely death of victims in Nigeria.[13]
Patent medicine vendors play an important role in healthcare provision at the community level. Community members sought medical attention and procured medicines from patent medicine vendors [Tables 1 and 4]. This study confirms similar findings in other parts of Nigeria.[3] However, studies have shown that this sector has not been well-regulated in Nigeria.[3,14] Due to the weak regulation of this sector, inappropriate use of medicines is common with this sector. According to a respondent, “In the chemist (patent medicine store), they can cut and give you the drug according to your money while in the pharmacy or hospital, they don’t cut and you have to pay for the complete dose of the drug”. This implies that patients are unlikely to take the full course of medicine when they procure medicines from patent medicine vendors. In Nigeria, patent medicine vendors do not undergo any formal course before they are given the license to practice and this can affect the quality of services they provide to members of the community. One way of improving the quality of services provided by them to members of the community is by organizing regular trainings for them and attending these trainings can be a prerequisite for their annual licensing. Research has shown that the training of patent medicine vendors can improve the quality of healthcare they provide within the community.[15]
Traditional medicine plays a vital role in African communities. The study revealed that 7.4% of those ill sought medical attention from traditional medicine healers. However, in most countries in Sub-Saharan Africa, traditional medicines have not been fully integrated into the primary healthcare system, and traditional medicine practice is not regulated and standardized. Lack of adequate regulation and standardization of traditional medicine practices have great health consequences. Hence there is need for this aspect of medicine practice to be regulated and integrated into the primary healthcare system.
Several factors influence medicine-use by community members. This study demonstrates that previous knowledge and experience of patient and cost play an important role in deciding where to seek treatment in Nigerian communities. Cost of treatment may have a negative effect on health. People may not seek the desired treatment because they are limited by lack of funds. According to a respondent, “drugs are cheaper in the chemist (patent medicine store) than the hospital or pharmacy”. Hence, the federal government should establish a comprehensive national health insurance scheme and community financing of healthcare should be encouraged.
Study limitation
The study was based on self-reported diagnosis of disease conditions by respondents. Therefore, there is a probability of reporting incorrect diagnosis of disease conditions.
CONCLUSION
The study therefore demonstrated that the occurrence of health problems in the studied community is high. These health problems are commonly caused by infectious and parasitic agents and cost-effective preventable measures exist for the prevention of diseases caused by these agents. The study also demonstrated that self-medication was common among the studied community and the patent medicine store was the most popular source of medicine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fact Sheet N°. 314. Geneva: WHO; 2011. World Health Organization (WHO). Facts about health in the African region of WHO. [Google Scholar]
- 2.Nigeria Demographic and health survey 2008. Abuja: National Population Commission; 2009. National Population Commission and ICF Macro. [Google Scholar]
- 3.Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7:120–7. doi: 10.4103/1596-3519.55666. [DOI] [PubMed] [Google Scholar]
- 4.Lal V, Goswani A, Anand K. Self-medication among residents of urban resettlement colony, New Delhi. Indian J Public Health. 2007;51:249–51. [PubMed] [Google Scholar]
- 5.Olugbenga-Bello AI, Adebimpe WO. Knowledge and attitude of civil servants in Osun state, southwest Nigeria towards the national health insurance. Niger J Clin Pract. 2010;13:421–6. [PubMed] [Google Scholar]
- 6.Hardon A, Hodgkin C, Fresle D. Geneva: World Health Organization and University of Amsterdam; 2004. How to investigate the use of medicines by consumers. [Google Scholar]
- 7.Geneva: WHO; 2009. World Health Organization (WHO). Medicine use in primary care in developing and transitional countries. [Google Scholar]
- 8.Hay SI, Guerra CA, Tatem AJ, Atkinson PM, Snow RW. Opinion: Tropical infectious diseases: Urbanization, malaria transmission and disease burden in Africa. Nat Rev Microbiol. 2005;3:81–90. doi: 10.1038/nrmicro1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 10.Corbett EL, Steketee RW, Kulie FO, Latif AS, Kamall A, Hayes RJ. HIV-1/AIDS and the control of other infectious disease in Africa. Lancet. 2002;359:2177–87. doi: 10.1016/S0140-6736(02)09095-5. [DOI] [PubMed] [Google Scholar]
- 11.Abuja: Federal Ministry of Health; 2005. Federal Ministry of Health. National strategies and guidelines for home and community management of malaria. [Google Scholar]
- 12.Russell S. The economic burden of illness for households in developing countries: A review of studies focusing on malaria, tuberculosis and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J Trop Med Hyg. 2004;71(suppl 2):147–55. [PubMed] [Google Scholar]
- 13.Okwonkwo AD, Okwonkwo UP. Patent medicine vendors, community pharmacist and STI management in Abuja, Nigeria. Afr Health Sci. 2010;10:253–65. [PMC free article] [PubMed] [Google Scholar]
- 14.Brieger WR, Osamor PE, Kabiru KS, Oladepo O, Otusanya SA. Interactions between patent medicine vendors and customers in urban and rural Nigeria. Health Policy Plan. 2004;19:177–82. doi: 10.1093/heapol/czh021. [DOI] [PubMed] [Google Scholar]
- 15.Oshiname F. Primary care training for patent medicine vendors in rural Nigeria. Soc Sci Med. 2009;35:1477–84. doi: 10.1016/0277-9536(92)90050-z. [DOI] [PubMed] [Google Scholar]


