Abstract
Background:
Fifty percent to 70% of the burden of childhood diarrhea and respiratory infections is attributable to undernutrition. It is compounded by food restriction during illness due to false beliefs, leading to a vicious cycle of malnutrition and infection. In the long run, it decreases the child's productivity, which is an obstacle to sustainable socioeconomic development.
Objectives:
To assess the dietary practices during different illnesses, to study the role of education, culture and religion in feeding an ill child and to create awareness against detrimental practices.
Materials and Methods:
A cross-sectional study was undertaken among 126 caregivers of ill children using an open-ended pretested questionnaire. Statistical package for social sciences software was used for data analysis. Simple proportions, percentages and Chi-square were used.
Results:
Caregivers believed that a child must be fed less during illness. Educational status did not play a role in maintaining beliefs, but elders and religion did. Doctors too were responsible for unwanted dietary restrictions. Media did not have an impact in spreading nutrition messages. Decreased breast feeds, initiating bottle feeds, feeding diluted milk and reducing complementary feeds during illness was widely practiced. Calorie intake during illness was very less and statistically significant. Firmly rooted beliefs about “hot” and “cold” foods lead to restriction of food available at home.
Conclusions:
Healthy feeding practices were few, and inappropriate ones predominant. Dietary education was overlooked. While planning community-based nutrition programs, firmly rooted beliefs should be kept in mind. Involving the elderly caregivers and mothers actively along with the health workers is the need of the hour.
Keywords: Beliefs, caregivers, childhood illness, food restrictions, malnutrition
Introduction
One's belief in food is strongly dictated by his upbringing, superstition and religion. Quantity and quality of feeding should be appropriate for a child's age. Disease consumes calories. Food restriction in illness leads to calorie deprivation and malnutrition, with frequent illnesses. Malnutrition causes mucosal damage and lowers immunity, leading to a vicious cycle of infection and malnutrition. When a child is recovering, an extra meal for 2 weeks is needed. A child's illness is a crucial moment for counselling of child feeding. We aimed at assessing the practices and beliefs regarding the diet of ill children and to offer preventive measures against detrimental practices at the earliest.
Materials and Methods
Sampling
Systematic random sampling was done in the Outpatient Department and wards on weekdays only. A total of 126 children and their caregivers were included. Every second ill child was taken for the study.
Data collection
A cross-sectional survey including open-ended questions was conducted in the department of paediatrics after obtaining informed consent. It was aimed at obtaining details about diet during illness. Data about diet in health was also obtained by the 1-week dietary recall method. A pilot study was conducted prior to this study. Caregivers of children with renal diseases, heart diseases, juvenile diabetes mellitus, thallassemia and surgical cases were excluded. This research adheres to the principles enunciated in the declaration of HELSINKI adopted and amended by the 52nd World Medical Association general assembly Edinburgh 2000 and Indian Council of Medical Research Ethical Guidelines for Biomedical Research on Human Subjects (2000).
Data analysis
Statistical package for social sciences software was used for statistical analysis of raw data. Simple proportions, percentages and Chi-square test (P<0.05) were applied.
Results
Children <6 months will be addressed as group A, 7 months–24 months as group B and 25 months–60 months as group C.
Group A
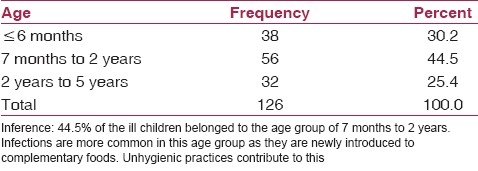
Thirty percent belonged to group A [Table 1].(1) Eighteen percent had Indian Academy of Pediatrics (IAP) Grade I malnutrition, 23.7% Grade II, 13.4% Grade III and 5.3% had Grade IV malnutrition. During health, 89.47% were breast fed (BF). Only 48.5% were BF within 1 h and 14.28% were BF after 3 days. 71.05% did not receive any prelacteals but 13.15% were given sugar water, 13.15% cow's milk and 5% received oral rehydration solution (ORS) as prelacteal feeds. Colustrum was believed to be harmful to child, while some believed that prelacteals clean the bowel. Another reason given was that breast milk is not sufficient.(1) Only 76.47% received significant amount of breast milk and only 19% were exclusively BF. Despite few mothers being aware of exclusive BF, 37% received complementary feeds (CF). Although all the mothers received antenatal care, 55% of them did not receive help with BF. The rest were taught about exclusive breast milk (EBM) till 6 months, which was not followed. Very few said position and attachments of the baby for feeding were discussed.(2)
Table 1.
Age distribution of the study population
During illness
The data here represents the beliefs of caregivers irrespective of the appetite changes that occur during illness [Table 2]. While 38.2% caregivers believed that the BF frequency should be decreased,(3) 3% stopped feeding completely and only 3% of the caregivers felt that BF should be increased [Table 3]. Nine percent of the mothers withheld BF when they were ill as they believed that illness would be transmitted to the child. Among those who gave CF, 12.5% diluted the CF during illness and 43% caregivers stopped giving CF.(4) Reasons given for decreased feeds during illness include “child is tired,” “child cannot suck” and “child cannot digest during illness.” One mother had started bottle feeding because she had an episode of diarrhea.
Table 2.
Diagnosis of the child
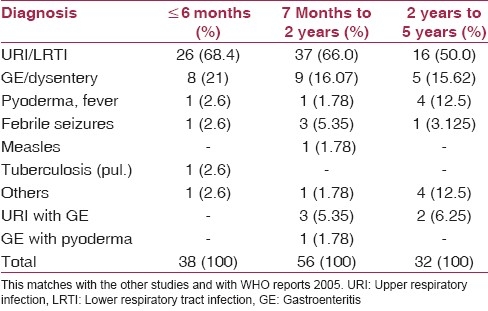
Table 3.
Caregiver's belief about breast feeding frequency in illness

Group B
44.5% of the ill children belonged to group B.(1) 30.3% had IAP Grade I, 12.5% Grade II malnutrition. Seventy-one percent of group B were male children. Female gender could be a risk factor for malnutrition as they are often neglected and their illness managed at home.
During health
Only 64.28% were BF. Fifty percent were fed nonvegetarian food (excluding eggs).
During illness
Nineteen percent caregivers felt BF frequency should be decreased(3) and 5% felt the need to increase feeds. Eleven percent discontinued it when the mother was ill. While 23.63% reduced the frequency of CF, 34.54% stopped CF completely [Table 4].(4) Thirty-three percent preferred thinner [Table 5](5) food during illness and 72% discontinued nonvegetarian food. Calorie intake during illness was very less and statistically significant [Table 6].(6)
Table 4.
Changes in complementary foods during illness

Table 5.
Changes in consistency of food during illness
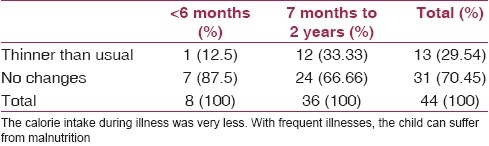
Table 6.
Average intake of calories in health and in illness (groups B and C)

Group C
90.6% of group C were fed nonvegetarian food during health, but 72% discontinued it during illness. Calorie intake during illness was very less and statistically significant.
There were various preferred and avoided foods during different illnesses among group “C” caregivers and are mentioned below (there were multiple responses): In respiratory illness (n=53): Preferred foods were idli (26.41%), rice (18.46%) and bread (16.98%). Seventeen percent did not have any preference. Oily (49%) foods, spicy foods (45.28%) and food considered as “cold” were avoided.
In gastroenteritis (GE) and dysentery (n=14): Rice (28.57%) and idli (21.42%) were favoured solid foods while milk (85.7%) and butter milk (21.42%) were favoured liquids. Forty-three percent of the caregivers avoided all food items. Meat and spicy foods were most avoided. Only 15% caregivers were aware of ORS and used it during GE before arriving at the hospital.
Pyoderma/fever: Idli (40%) and biscuits (40%) were the most favoured. Eighty percent avoided oily foods, 60% cold foods and 40% avoided rice. Milk and coffee were preferred liquids. Sixty percent avoided juices and butter milk. Ten percent perceived coconut water to be special; it was thought to provide energy to the ill child.
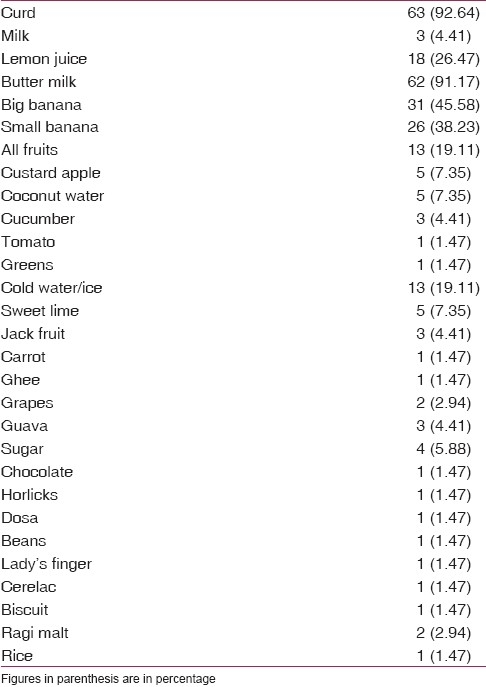
“Hot” and “Cold” food concept
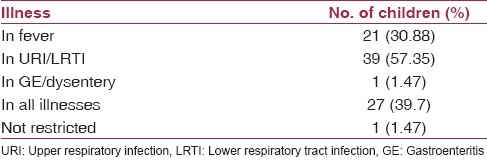
A pilot study was carried out to identify the perception of hot and cold foods. Hot foods mean those that produce heat in the body and cold foods are those that cause colds (running nose, cough, etc.).(3) Based on this a list was developed. Forty-one percent had beliefs about “hot” foods. Chicken (36%), brinjal (20%), mutton and jaggery (14%) were considered(4) “hot” by the majority. Fish, papaya and beet root too were also considered to be “hot”.(7) Seventy-seven percent of the caregivers had beliefs about “cold” foods. Curds (92.65%), butter milk (91%), bananas, lemon juice and other citrus fruits were considered to be “cold [Tables 7 and 8].”(8)
Table 7.
“Hot” foods list
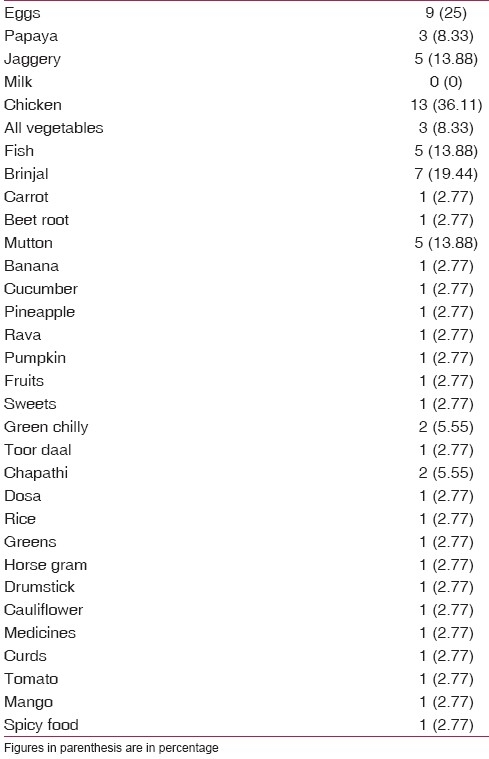
Table 8.
“Cold” foods list
Home remedies
Nineteen percent of the caregivers had given home remedies, 45.83% of them gave Tulsi (Ocimum sanctum) and 41.6% gave ginger. Clove, pepper, honey, turmeric powder and garlic were also administered during cold based on an elder's advice. Those who gave native medicine also followed food restrictions. Turmeric, radish, sugarcane and rice were preferred during jaundice.(5) Oily food, salt and mangoes were avoided. One caregiver was asked to starve the child for a day to clear worms from the bowel.
Other misconceptions
“Eating sprouted seeds leads to cold”; “sugar causes cough in infants”; “milk causes vomiting.”. Some believed that it increases sputum during cold. “Jamoon decreases diarrhea,” “holy water cures measles,” “milk and sugar produce worms in the gut,” “biscuits increase sputum during illness,” “rice causes fever during illnesses (among Muslims),” “undiluted milk forms clots and blocks the gut.”
Role played by doctors
Six doctors had asked to avoid “cold” food, which included curds, butter milk, fruit juices and bananas. Five had asked to avoid rice during fever. Two had advised to restrict diet only to rice and butter milk during diarrhea. Twenty-one doctors had advised not to restrict any kind of food and to follow the usual diet during illness.
The following applies to all groups
In our study, we found that elders at home were the main source of dietary beliefs for the mothers. Of 126 caregivers, 38% had studied up to the high school level and 20% were illiterate; only 0.8% were postgraduates. The Chi-square test was applied to study the association of beliefs about CF frequency and about “hot” and “cold” food concept with educational status. None were statistically significant.(6,7) Sixty-six percent belonged to the very low-income group, but the fact that this hospital is visited mostly by people from the low socioeconomic status should be kept in mind.(8)
Role of religion
Although majority were Hindus, 37% were Muslims. Certain practices were commonly followed among Muslims. Giving prelacteals and Bonniso syrup and the belief that rice causes fever is more prevalent among the Muslims.
Discussion
The aim of this study was to determine the beliefs, knowledge and attitude of caregivers toward diet practices during childhood illness. Information about diet during health showed that many caregivers followed faulty dietary practices during health itself, which is the highlight of the study. Antenatal care, a crucial time for dietary education, was not used efficiently. Educational status did not play a role in maintaining beliefs (P>0.05). This shows that beliefs are firmly rooted in the families as traditional practices. By reducing the consistency and frequency during illness, they deprive the child of the required amount of energy and micronutrients.(9) Non-vegetarian food was thought to aggravate fever and produce heat in the body. The “hot” and “cold” food concept was blindly followed without a scientific basis, leading to unnecessary restriction of easily available food at home [Tables 9 and 10].(9,10) Children with Grade I and II malnutrition may appear normal to the caregiver. Added to this, if food is limited during illness, the child can suffer from severe malnutrition with repeated illnesses. Eighty percent of the nutrition-related mortality is associated with a mild form of malnutrition according to the WHO reports.(10) While positive attitudes toward diet during illness were very few, negative attitudes and diet restrictions without scientific basis were widely prevalent. Those who are educated about diet may not follow it as certain practices are deeply rooted and are followed through generations; counselling alone might not make an impact on them. The child is the ultimate innocent victim. We emphasize that the issue has to be tackled at every level in the community and studies be conducted before planning community-based nutrition programs to assess the locally prevalent myths and taboos. A study to establish the scientific basis for “hot” and “cold” food is necessary. Participation of caregivers, particularly elders who influence the mothers, is also indispensable to reduce malnutrition in children.
Table 9.
Illnesses in which “hot” food was restricted by caregivers who had beliefs about “hot” foods (groups B and C)
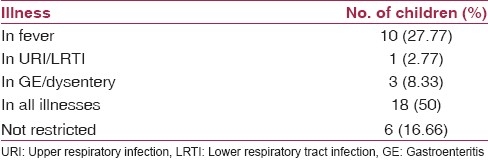
Table 10.
Illnesses in which “cold” food was restricted by caregivers who had beliefs about “cold” food (groups B and C)
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Hasan J, Khan Z, Sinha SN. Socio-cultural factors influencing nutritional status of infants-a longitudinal study. Indian J Matern Child Health. 1991;2:84–6. [PubMed] [Google Scholar]
- 2.Banapurmath CR, Nagaraj MC, Banapurmath S, Kesaree N. Breast feeding practices in villages of central Karnataka. Indian Pediatr. 1996;33:477–9. [PubMed] [Google Scholar]
- 3.Real M, Kumar V, Nanda M, Vanaja K. Beliefs and practices of urban mothers regarding “hot” and “cold” foods in childhood illnesses. Ann Trop Paediatr. 1982;2:93–6. doi: 10.1080/02724936.1982.11748235. [DOI] [PubMed] [Google Scholar]
- 4.Kapil U, Sood AK, Gaur DR. Maternal beliefs regarding diet during common childhood illnesses. Indian Pediatr. 1990;27:595–9. [PubMed] [Google Scholar]
- 5.Ali NS, Azam SI, Noor R. Women's beliefs regarding food restrictions during common childhood illnesses: A hospital based study. J Ayub Med Coll Abbottabad. 2003;15:26–8. [PubMed] [Google Scholar]
- 6.Ali NS, Azam SI, Noor R. Women's perception about food properties in a tertiary care hospital. J Coll Physicians Surg Pak. 2003;13:501–3. [PubMed] [Google Scholar]
- 7.Ganjoo C, Rowlands R. Breast feeding and weaning practices in urban housewives of Srinagar. Indian J Nutr Diet. 1988;25:354–8. [PubMed] [Google Scholar]
- 8.Saito K, Korzenik JR, Jekel JF, Bhattacharji S. A case-control study of maternal knowledge of malnutrition and health-care-seeking attitudes in rural South India. Yale J Biol Med. 1997;70:149–60. [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma KP, Thakur AK. Maternal beliefs regarding diet during childhood illnesses. Indian Pediatr. 1995;32:909–10. [PubMed] [Google Scholar]
- 10.World Health Organization. Infant and young child nutrition. c2002. [Last cited on 2002 Apr 16]. Available from: http://apps.who.int/gb/archive/pdf_files/WHA55/ea5515.pdf .


