Abstract
Background:
Pregnant women inhabiting urban slums are a “high risk” group with limited access to health facilities. Hazardous maternal health practices are rampant in slum areas. Barriers to utilization of health services are well documented. Slums in the same city may differ from one another in their health indicators and service utilization rates. The study examines whether hazardous maternal care practices exist in and whether there are differences in the utilization rates of health services in two different slums.
Materials and Methods:
A cross-sectional study was carried out in two urban slums of Aligarh city (Uttar Pradesh, India). House-to-house survey was conducted and 200 mothers having live births in the study period were interviewed. The outcome measures were utilization of antenatal care, natal care, postnatal care, and early infant feeding practices. Rates of hazardous health practices and reasons for these practices were elicited.
Results:
Hazardous maternal health practices were common. At least one antenatal visit was accepted by a little more than half the mothers, but delivery was predominantly home based carried out under unsafe conditions. Important barriers to utilization included family tradition, financial constraints, and rude behavior of health personnel in hospitals. Significant differences existed between the two slums.
Conclusion:
The fact that barriers to utilization at a local level may differ significantly between slums must be recognized, identified, and addressed in the district level planning for health. Empowerment of slum communities as one of the stakeholders can lend them a stronger voice and help improve access to services.
Keywords: Barriers to utilization, hazardous delivery practices, maternal health, urban slums
Introduction
The urban population is increasing at a very rapid rate in India. It is projected to inflate to the order of 357 million in 2011 and 432 million by 2021 (Census of India 2001).(1) Rapid urban growth has led to an increase in the number of urban poor, especially those living in slums. India's urban poor have even outnumbered the rural poor, since 1998.(2) Attention to vulnerable communities in the slums is therefore needed from a public health perspective, and pregnant females and children constitute the major “high risk” group. Given the increasing importance of urban health to global prospects, The United Nations Millennium Development Goals look to substantial improvements in maternal and child survival targets, linked exquisitely with their fourth and fifth goals.(3) Although urban India has a relatively strong health and nutrition infrastructure - with public sector investments coming from central, state, and local bodies as well as a vast private sector - there is marked inequitable distribution of service availability and utilization between the rich and poor, between the settled urban population and the marginalized slum dwellers. Vulnerable urban communities continue to be poorly served. This is not only the result of underprovision or “service” barriers. but is a product of interrelated variables such as poverty, inequitable distribution of primary healthcare services, poor referral systems, vertical programming, and attitudinal and management challenges.(2) Understanding how policies and programs can address both service and demand side barriers is a central question, both globally and locally, particularly in view of the poor health status of women and children. Although uniformly disadvantaged, the urban poor cannot be treated as homogenous entities; there exist important sociodemographic variations within the urban poor population in relation to their use of services and the barriers faced in service utilization. Most urban slum areas are built by immigrant families in search of jobs who come from neighboring rural areas, bringing with them their own area-specific social customs, rituals, and taboos. Depending on these factors, the slums may differ from each other in their indicators of health.(4) It is understandable therefore that aggregate urban health statistics would mask inequalities. We described maternity care in two vulnerable slum communities in Aligarh, and examined differences in care and outcomes between the two deprived groups. Keeping in mind the above facts, the present study was carried out with the following specific objectives:
To determine existing maternal health practices during pregnancy and childbirth in two urban slums,
To compare health practices and barriers to services utilization between two different slums.
Materials and Methods
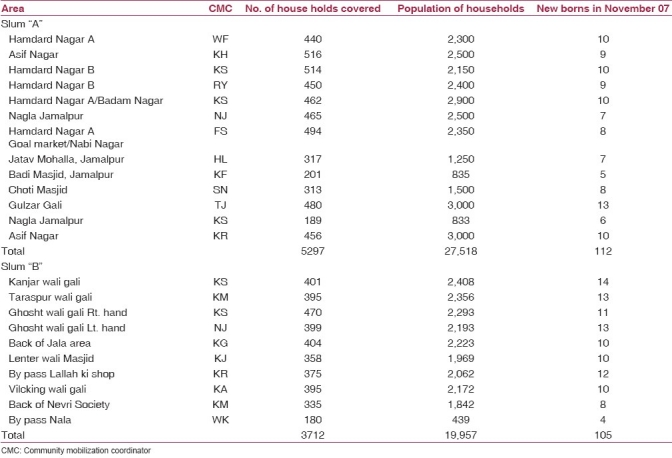
The present cross-sectional descriptive study was carried out in two urban slums selected purposively. Slum A (Nabinagar/Jamalpur) was registered with the municipality and had good civic amenities compared to Slum B (Mehfooznagar), which was unregistered in the municipality, and was thus a “gray area.” Slum A (Nabinagar/Jamalpur) had a population of 27,518 living in 5297 households [Table 1]. Most people were working as daily wagers, laborers, and vendors and belonged to the lower socioeconomic group. Health services available within 2 km of the area included a tertiary care facility (medical college), one private nursing home offering facilities for antenatal care and delivery services, one health subcenter, and one health clinic for children, managed by the “polio partners.” (for the underserved strategy for National Polio Eradication, the “polio partners” include Departments of Community Medicine and Paediatrics, United Nations International Children's Emergency Fund (UNICEF), Rotary International and District Health Administration. A cadre of local community level workers are employed by UNICEF with the primary objective of improving coverage of oral polio vaccine by social mobilization and tracking of newborn children). Slum B (Mehfooz Nagar) was unregistered and had a population of 19,957 living in 3712 households [Table 1]. Most of the residents belonged to lower socioeconomic classes and were engaged in unskilled daily wage works. A large number of inhabitants were unemployed. The health services available within 2 km included Health Clinic for children managed by “polio partners” and two unqualified private providers (Quacks). The nearest Government Health Facility was the District Hospital situated 6 km away.
Table 1.
Distribution of population in slums A and B
Records of all mothers having live birth in the month of November, 2007 were obtained from the community level workers of UNICEF working in the area. There were records of 98 live births in Slum A and 102 live births in Slum B. These households were visited by female researcher. The mothers were interviewed in a nonformal and nonjudgmental manner after obtaining informed consent from the family. Data were recorded in a pretested proforma. Appropriate counseling, treatment and referral services were provided to the mothers, as needed. Data were analyzed using Statistical Package for Social Sciences 12. A Z test for proportions was used where relevant. A value of 0.05 was considered as significant.
Results
Socio-economic profile of study population
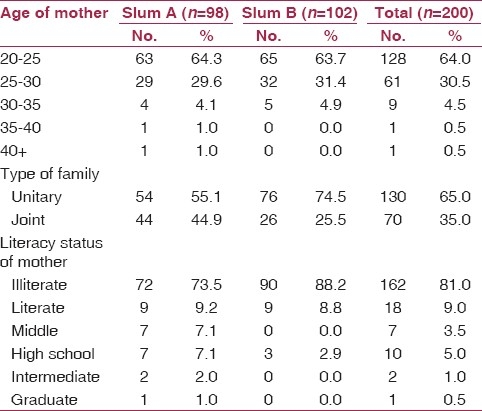
All mothers belonged to low social class. Table 2 shows that most mothers were young, (94.5% being less than 30 years of age), illiterate (81%), and living in unitary type of families (65%).
Table 2.
Socio-cultural profile of study population
Maternal health practices
The maternal health practices [Table 3] studied were antenatal check-up, delivery practices, postnatal check-up and early infant feeding practices.
Table 3.
Maternal health practices
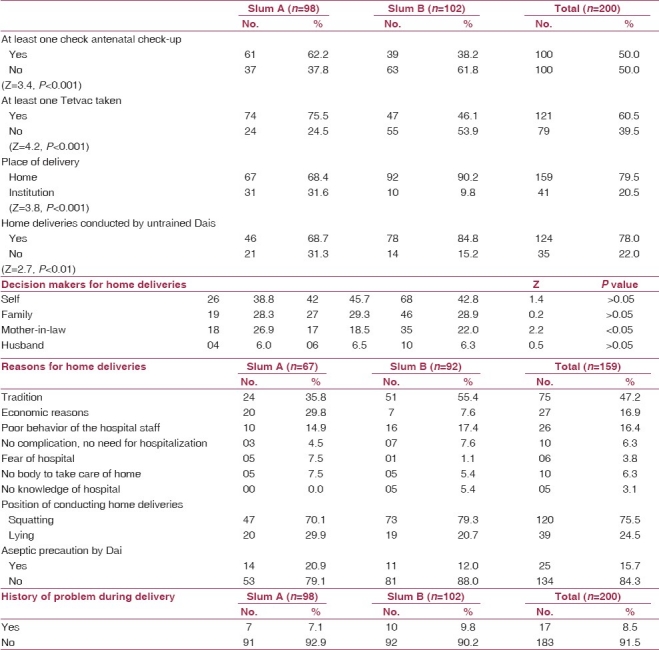
Antenatal check-up
Fifty-two percent of all mothers had at least one antenatal check-up at a government or a private facility. More mothers in slum A had antenatal check-up compared to slum B. This difference was statistically significant (P<0.05). As many as 60.5% mothers received at least one Injection Tetvac during pregnancy. Many women asked for, and received Injection Tetvac from private providers without undergoing antenatal check-up. In slum A, significantly more mothers received Injection Tetvac compared to slum B.
Place of delivery
Home delivery was the norm in both the slum areas, 79.5% of all mothers giving birth at home. The rate of home delivery in slum B (92.2%) was significantly higher than that in slum A (68.4%). Of the 20.5% mothers who delivered in an institution, either a government facility or a private nursing home, a majority were from slum A (31.6%).
Home deliveries
A total of 159 mothers delivered at home. Hazardous practices were found to be common in home deliveries. A majority of home deliveries were assisted by untrained birth attendants (78%). Significantly more deliveries in slum B were assisted by untrained birth Attendants (84.8%) compared to those in slum A (68.7%). Two-thirds of all home deliveries were conducted in squatting position without adequate perineal support. Aseptic precautions such as washing of hands with soap and water, using clean surface for delivery, use of sterile cord tie and sterile blade for cutting the cord were inquired about. Majority of the mothers claimed that the birth attendants did not take aseptic precautions (84.3%). In a number of cases (40.3%), the cord was cut by the edge of a cup broken for this purpose. The difference between these practices between slum A and slum B was marginal. Seventeen mothers (8.5%) gave history of problem during labor. Of these, 15 had prolonged labor, which was managed at home, and 2 had retention placenta for which they were taken to a government facility.
Reason for choosing place of delivery
The most common reasons for home delivery were said to be “family tradition” (47.2%), economic constrains (16.9%), and rude behavior of hospital staff (16.4%). There was a significant difference in the reason most commonly cited for choosing home delivery between the two slums. While “tradition” was a more common reason in slum B, economic constrain was a more common reason in slum A. A government hospital was chosen mainly because of perceived skilled attention available (66.7%) or due to complications in index pregnancy or earlier pregnancy (33.3%). The main reason for choosing a private nursing home was also perceived skilled attention given (53%), because of good behavior of health staff (17.6%) or because it was close to home (17.6%).
Post-natal check-up
There was no history of postnatal check-up in any mother after home delivery. In a number of cases, the traditional birth attendants did visit the mother for giving traditional massage and oil bath to mother and child, but in no case was the mother examined.
Early newborn feeding practices [Table 4]
Table 4.
Newborn feeding practices
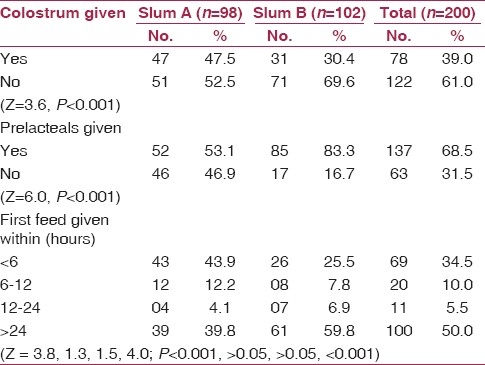
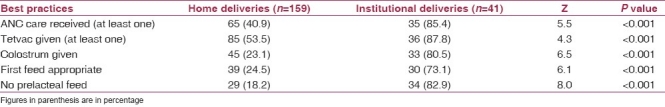
Breastfeeding was universal. However a number of traditional practices detrimental to exclusive breast feeding (EBF) (such as discarding of colostrums (61%), delaying of first feed (65.5%), and giving of prelacteal feeds (68.5%)) were common. Appropriate feeding practices were significantly more common in slum A compared to slum B. Comparing feeding practices in home and in institutional delivery, appropriate practices were found to be significantly more common in institutional deliveries compared to home deliveries [Table 5].
Table 5.
Comparing best practices in home and institutional deliveries
Discussion
The two slums were not found to be uniform entities but differed significantly in their health practices. Differences in health practices were probably due the distance from urban health institutions. Utilization of Ante natal care(ANC) is an important intervention for reducing maternal and perinatal morbidity and mortality.(5) In the present study, at least one antenatal visit was utilized by 52.5% mothers, using either the government or private facility. This is more than the overall antenatal coverage rate in Uttar Pradesh, which is 25%(6) but less than 74.3% reported for slum dwellers in neighboring Delhi(7) and 73.9% reported in an integrated child development services (ICDS) study covering 14 states and 26 districts.(8) A number of mothers visited private facilities for Injection Tetvac only. Thus the rate of utilization of at least one Injection Tetvac was more than the rate of antenatal check-up. Home delivery was the norm in urban slums and most home deliveries were conducted by untrained birth attendants. Our findings were consistent with other studies.(9–12) Home delivery was the preferred choice in both slums for a majority of women (79.5%), mostly by untrained birth attendants (78.0%). Hazardous practices were common and untrained birth attendants conducted most deliveries in squatting position. No aseptic precautions were taken, and cord was cut by the edge of a broken cup. It is interesting to note that once home delivery by untrained birth attendant was chosen, the difference in rates of hazardous practices was marginal between both slums. A majority of the deliveries were conducted in squatting position. Effecting delivery in squatting position is beneficial in that it shortens the duration of first and second stages of labor. However, without proper perineal support provided by birthing chairs or cushions, incidence of maternal injury such as perineal tear is very high.(13) Thus the proportion of the home deliveries conducted in squatting position(56%) may well be considered hazardous for the mothers.(14) Besides, untrained traditional birth attendants do not use aseptic precautions. The traditional methods of cutting of cord with the edge of broken cups were found to be common even today. Such hazardous practices have also been described by other workers in south Asia.(15–17)
It is remarkable to note that there was a significant difference in utilization indices of maternal health services between the two slums; antenatal coverage being lower and home delivery rates being higher in slum B. For understanding the difference in utilization of health facilities, factors such as physical accessibility, household practices, cultural norms, and economic affordability may be considered. As the socio-cultural background was similar in both populations, the difference in the present study was probably because of lack of physical accessibility to health facilities in slum B where the nearest maternal health facility was at a distance of 6 km. “Tradition” as a reason for choosing home for delivery reflects a lack of knowledge of the importance of safe delivery practices. This “lack of knowledge” was significantly more common in slum B where physical access to health facilities also lacked. Other studies have also highlighted lack of knowledge as an important barrier to utilization of care and have pointed out that knowledge improves utilization rates. A study from Uttar Pradesh also concludes the same.(11) Attitude of health workers and their “rude behavior” may also create barriers to access, turning the mothers away from government facilities to private sector or to “traditional” home delivery practices. In the private sector (and also in the public sector where drugs and investigations have to be paid for), poverty may then be the limiting factor. In the present study, in slum A, where health facilities were physically accessible, the main reasons after tradition for home delivery were poor finances and rude behavior of the hospital staff.
In developing countries like India, it calls for a herculean effort to change the practice of home delivery by traditional untrained attendants to delivery by trained birth attendant or to institutional delivery. Although the emphasis of the National Reproductive and Child Health Programme is to promote institutional deliveries, the poor infrastructure, and limited government health facilities in states like Uttar Pradesh make home deliveries, and thus the role of Trained Traditional Birth Attendants (TBA) inevitable. Moreover, there is evidence that skilled attendant at birth (TBA, Auxiliary Nurse-Midwife or Doctor) is a significant determinant of maternal and child health.(9) It is possible to mitigate maternal mortality and morbidity even in resource scarce settings, using a variety of models of care.(18,19) There is an ongoing debate about re-enforcing home-based birthing strategies with skilled birth attendants in developing counties.
In spite of universal breast feeding being the norm, certain early newborn practices such as prelacteal feeding, discarding of colostrums, and delaying the first feed beyond 6 hours of birth are common.(20,21) Such practices were observed in the present study as well. The slums differed in their breast feeding practices significantly suggesting that barriers to access to health facilities, either physical or traditional play an important role in establishment of exclusive breast feeding. The higher rate of antenatal visits and institutional deliveries in slum A may be responsible for better breast feeding practices. Mothers undergoing institutional delivery are known to have higher rates of breast feeding.(22)
Conclusion
One of the important barriers to realization of maternal health goals was the low utilization of services provided by the public health system through its supply side mechanisms. The important demand side barriers to utilization included “tradition,” financial constraints, and rude behavior of the health staff. Utilization of health services is poor in urban slums even when physical accessibility is present. Social and cultural barriers are more common in slums where health services are not reachable. Skilled birth attendants are not reaching those who need them most. Evidence from the study suggests that demand side barriers may be as important as supply factors in deterring patients from obtaining treatment. Yet relatively little attention has been given, either by policy makers or researchers, to ways of minimizing their effect. Accessibility to health services of slum population must therefore be taken into account in District Health Planning. Since it may not be possible to establish a health facility staffed with a doctor or a nurse in every slum area, there is a need to increase awareness of the community about benefits of using modern maternity care at nearby health centers for better pregnancy outcome. Urban local bodies should establish a network of community health workers/volunteers to facilitate this process through health promotion activity. Also, the health education component of care can bring about changes in attitude and practice and this component should be strengthened in the health delivery system.
Acknowledgments
The research team acknowledges the help provided by community health mobilizers (CMCs) (UNICEF) in the field.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.National Urban Health Mission (2008-2012) Draft document: Meeting the health challenge. [Last accessed on 2011 Aug 9]. Available from: http://www.uhrc.in/downloads/Reports/NUHM-Draft .
- 2.Bangalore: Environmental Health Project; 2003. EHP Report on national consultation on improving the health of the urban poor. Bangalore, 30th June – 1st July 2003. [Google Scholar]
- 3.New York: United Nations; 2001. Report of the Secretary-General. Road map towards the implementation of the United Nations millennium declaration. (UN document no. A/56/326) [Google Scholar]
- 4.de Bernis L, Sherratt DR, AbouZahr C, Lerberghe W. Skilled attendants for pregnancy, childbirth and postnatal care. Br Med Bull. 2003;67:39–57. doi: 10.1093/bmb/ldg017. [DOI] [PubMed] [Google Scholar]
- 5.Lassi ZS, Haider BA, Bhutta ZA. Cochrane Database Syst Rev. Vol. 11. Hoboken, New Jersey: John Wiley and Sons, Ltd. Publications; 2010. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes (Review) p. CD007754. 2010. [DOI] [PubMed] [Google Scholar]
- 6.India: Chhatrapati Shahuji Maharaj Medical University; 2005-07. Basic Facts: Uttar Pradesh Unpublished report of the project Concurrent Assessment and Technical Assistance to Districts of Uttar Pradesh, Sponsered by Department of Family Welfare, Govt. of Uttar Pradesh, through Department of Community Medicine. [Google Scholar]
- 7.Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 8.Chandhiok N, Dhillon BS, Kambo I, Saxena NC. Determinants of antenatal care utilization in rural areas of India: A criss-sectinal study from 28 districts (An ICMR task force study) J Obstet Gynecol India. 2006;56:47–52. [Google Scholar]
- 9.de Bernis L, Sherratt DR, AbouZahr C, van Lerberghe W. Skilled attendants for pregnancy, childbirth and postnatal care. Br Med Bull. 2003;67:39–57. doi: 10.1093/bmb/ldg017. [DOI] [PubMed] [Google Scholar]
- 10.Islam M. The safe motherhood initiative and beyond. Bull World Health Organ. 2007;85:735. doi: 10.2471/BLT.07.045963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baqui AH, Williams EK, Darmstadt GL, Kumar V, Kiran TU, Panwar D, et al. Newborn care in rural Uttar Pradesh. Indian J Paediatr. 2007;74:241–7. doi: 10.1007/s12098-007-0038-6. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal P, Singh MM, Garg S. Maternal health-care utilization among women in an urban slum in Delhi. Indian J Community Med. 2007;32:203–5. [Google Scholar]
- 13.Lawrence A, Lewis L, Hofmeyr GJ, Dowswell T, Styles C. Maternal positions and mobility during first stage labour. Cochrane Database Syst Rev. 2009;2:CD003934. doi: 10.1002/14651858.CD003934.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allahbadia GN, Vaidya PR. Squatting position for delivery. J Indian Med Assoc. 1993;91:13–6. [PubMed] [Google Scholar]
- 15.Chaudhry UK. Traditional practices of women from India: pregnancy, childbirth, and newborn care. J Obstet Gynecol Neonatal Nurs. 1997;26:533–9. doi: 10.1111/j.1552-6909.1997.tb02156.x. [DOI] [PubMed] [Google Scholar]
- 16.Osrin D, Tumbahangphe KM, Shrestha D, Mesko N, Shrestha BP, Manandhar MK, et al. Cross sectional, community based study of newborn infants in Nepal. BMJ. 2002;325:1063. doi: 10.1136/bmj.325.7372.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geneva: WHO; 2001. WHO:RHT/MSM/:98.4 Reproductive Health (Technical Support) Maternal and Newborn Health: Safe Motherhood. Care of the Umbilical cord: A review of the evidence. (unpublished report) p. 8. [Google Scholar]
- 18.Ronsmns C, Vanneste AM, Chakraborty J, van Ginneken J. Decline in maternal mortality in Matlab, Bangladesh: a cautionary tale. Lancet. 1997;350:1810–4. doi: 10.1016/S0140-6736(97)08012-4. [DOI] [PubMed] [Google Scholar]
- 19.Pathmanathan I, Liljestrand J, Martins JM, Rajapaksa LC, Lissner C, de Silva A, et al. Washington, DC: World Bank; 2003. Investing in maternal health: learning from Malaysia and Sri Lanka; p. 204. [Google Scholar]
- 20.Sethi V, Kashyap S, Sethi V. Infant feeding practices in a relocation slum- a pilot study. Indian Pediatr. 2003;40:579–80. [PubMed] [Google Scholar]
- 21.Banapurmath CR, Selvamuthukumarasamy A. Breastfeeding and the first breastfeeds-correlation of initiation pattern to mode of delivery in 1279 hospital delivered babies. Indian Pediatr. 1995;32:1299–301. [PubMed] [Google Scholar]
- 22.Rahi M, Taneja DK, Misra A, Mathur NB, Badhan S. Newborn care practices in an urban slum of Delhi. Indian J Med Sci. 2006;60:506–13. [PubMed] [Google Scholar]


