Abstract
Introduction:
Prevalence of sexually transmitted infection shows regional variations. Though a rising trend of prevalence of viral STI s has been observed, syphilis still continues to remain a commonly diagnosed STI.
Aim:
To study the current status of acquired syphilis in a tertiary care hospital.
Materials and Methods:
Retrospective analysis of all the cases of acquired syphilis registered in our hospital from 2005 to 2009 was done. Complete epidemiological, clinical, and investigational data were recorded and assessed.
Observation:
Total of 570 cases attended the STI clinic from year 2005 to 2009. 42 (7.36%) cases were diagnosed as syphilis. There were 32 (74%) males and 11 (26%) were females. 25 (60%) were married. Only two patients were less than 15 years of age. Primary syphilis was diagnosed in 21 (50%), secondary in 10 (24%), and latent in 11 (26%) cases. Two (9.5%) of primary syphilis showed multiple chancre. Concomitant primary chancre and lesions of secondary syphilis were seen in 2 (20%) patients. Secondary syphilis presented as condyloma lata (50%), maculo-papular rash (40%), and lues maligna in one patient who was HIV positive. Mixed infection was diagnosed in eight patients of which herpes genitalis was the commonest. Two patients were serologically positive for HIV.
Conclusion:
Incidence of syphilis had shown a constant trend over last 5 years. In lieu of change in trends of sexual practices, condyloma was the commonest presentation of secondary syphilis. Pustular syphilis was observed in association with HIV and could be a marker of the immune-deficient state.
Keywords: Acquired, syphilis, sexually transmitted infection
INTRODUCTION
Prevalence of sexually transmitted infections shows regional variations. Various epidemiological studies report a diminishing prevalence of syphilis including other bacterial STIs and a rising incidence of viral STIs.[1] However, a resurgence of syphilis has been observed and reported by some.[2,3]
Acquired immunodeficiency syndrome alters the clinical manifestations, course, and response to treatment of syphilis. Syphilis is characterized by great chronicity and quiet latency, which influence the obstetric outcome and result in several systemic complications. Mixed infections with syphilis are common and partial treatment of syphilis with easily accessible antibiotics may fail to treat the infection completely, thus promoting smoldering infection in the community.
Hence, syphilis continues to be a major STI and its epidemiological trends need surveillance for effecting its control. A retrospective, hospital-based clinico-epidemiological study of syphilis was carried out in order to follow-up changing trends in syphilis.
MATERIALS AND METHODS
Clinical records of all patients who were diagnosed as acquired syphilis and who attended the sexually transmitted disease clinic of the Sucheta Kriplani Hospital, New Delhi, from January 2005 to December 2009 constituted the data base of this retrospective study.
Details of the epidemiological features (including the age, sex, marital status, and sexual behavior), clinical examination (including number of ulcers, lymphadenopathy, morphological type of rash, and stage of syphilis), and concomitant STI were recorded.
Serology for venereal disease research laboratory test (VDRL) and Human immunodeficiency virus (HIV) were done in all the patients irrespective of their disease stage. Treponoma pellidum HEmagglutin (TPHA) was performed in only those patients who could afford it. All the patients of primary syphilis were subjected to dark ground (DG) microscopy.
The patients of latent stage syphilis were diagnosed either due to serological investigation in the spouse of the patient with primary or secondary syphilis or because of the serological positivity in their newborns.
OBSERVATION
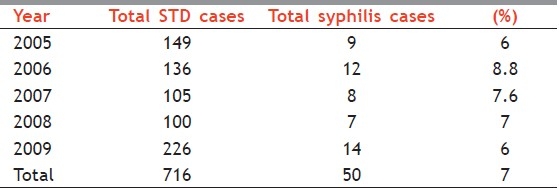
The study was carried out at the sexually transmitted disease (STD) clinic of a tertiary care hospital of Delhi. A total of 716 patients were diagnosed to have a STD. Syphilis was the third most common STD, being present in 7% (50) of the patients. The most common infections were viral, with herpes simplex diagnosed in nearly 28% patients and condyloma acuminata in 20% patients. But the prevalence of syphilis had been consistent in all these years, being as high as 9% in 2006 and as low as 6% in 2005 and 2009 [Table 1].
Table 1.
Annual distribution of syphilis cases
Of the total of 50 diagnosed syphilis cases, 35 (70%) were males 15 (30%) were females; the M:F ratio being 2.3:1. Most of the patients were young adults, with age groups ranging from 17 to 46 years. The mean age was 27 years. Two patients were less than 15 years of age and one patient was more than 60 years old. Interestingly, most of the patients (80%) were literate. Promiscuous behavior was noted in 64% patients. 33 (66%) were married and 42% of these married patients indulged in extramarital contact with commercial sex workers. Homosexuality was noted in 6 (12%) patients, all of them were males in the age group of 18–35 years.
46% (23 patients) had primary syphilis, 32% (16 patients) had latent, and 22 % (11 patients) had secondary syphilis. The clinical presentation of all the patients are tabulated in Table 2
Table 2.
Clinical presentations of the patients
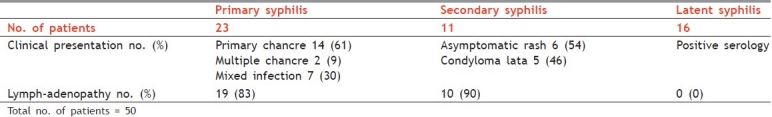
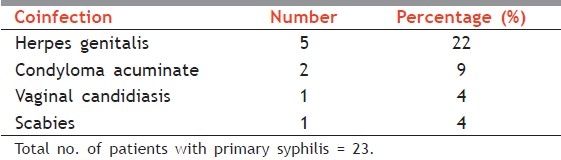
Primary syphilis manifested as single, painless, indurated ulcer in most of the cases, with only two patients showing multiple chancre. Seven (30%) patients of primary syphilis had mixed infection, with herpes genitalis coinfection in five and condyloma acuminate in two patients [Table 3]. Lymphadenopathy was present in 19 (38%) of patients with primary chancre.
Table 3.
Coinfection with primary chancre
Of the 11 patients with secondary syphilis, nonitchy maculopapular rash was observed in 6 (54%), followed by condyloma lata in 5 cases (46%). 90% patients of secondary syphilis had lymphadenopathy. Three patients (27%) of the secondary syphilis showed primary chancre concomitantly.
Six patients reported of homosexual behavior. Two of them presented with classical primary chancre. Four patients presented with secondary syphilis, among whom two presented with condyloma lata alone, and one each with maculopapular rash and condyloma lata with rash.
All the patients with primary stage lesions were positive under DG microscopy. Secondary stage patients were not subjected to DG. All of the patients, irrespective of their stage, were positive for VDRL, the titres ranging from as low as 1:8 to as high as 1:1024, 1:16 being the most common titre. TPHA was carried out in only 18 patients, all of whom tested positively. Of all, two patients were serologically positive for HIV. One had primary syphilis with mixed infection and the other was in secondary stage with both maculopapular lesions and lues maligna.
DISCUSSION
There has been a dramatic change in the epidemiological profile of STDs all around the world. Bacterial STDs which were so common in 1960s and 1970s have now been taken over by viral infections, which have demonstrated an upward trend since 1980s. This could be both due to the spread of HIV as an epidemic all over the world and also because of the changing sexual practices. Viral infections are dominating the STD world today,[1] but syphilis has maintained its constant prevalence rate. Various studies have shown a rise in the prevalence of syphilis in recent years in India[2] as well as in the Western countries.[3]
Year wise incidence of syphilis in our hospital has been around 7%, exhibiting an almost uniform and stable trend over the last 5 years. Most of the studies showing a constant or a rising prevalence of syphilis have shown an actual increase in the secondary stage of presentation.[2,4] Contrary to this, in our study majority of the patients presented in primary stage (46%) followed by latent stage disease (32%). Secondary syphilis was the least common presentation (22%) among the three stages. The secondary stage normally presents as asymptomatic skin rash. The asymptomatic nature of the secondary syphilis could be one of the reasons for the low prevalence in our study. Latent disease was also high and points toward either lack of accurate diagnosis or inadequate treatment. Majority of these patients with latent syphilis were spouses of those with active disease, which indicates a high prevalence of conjugally acquired syphilis due to the lack of use of barrier method of contraception.
30% of patients with primary syphilis had mixed infection, with herpes genitalis being the most common associated infection. This calls for a thorough examination and serological investigations in all the patients presenting as genital ulcers. Syphilitic lesion could be missed among the numerable herpetic erosions.
Among those with secondary stage disease, condyloma lata was as common a presentation as maculopapular rash. This indicates a change in the trends of sexual practices, where in oro-genital and peno-anal contacts are increasingly practiced, besides peno-vaginal contact. Pustular syphilis was present in an HIV positive patient. This presentation could serve as a marker of an immune-deficient state. HIV serology should be carried out in all the patients with a suspicion of a STD. It has also been stated that syphilis is the most common STD responsible for the easy and early spread of HIV.[5]
Therefore, though viral STDs are on the rise, syphilis and herpes genitalis still remain the most common STIs. Mixed infections of the two are also common. Primary stage of the disease is alarming to the patient on account of its site and presents more commonly in the clinics than the secondary rash and the dermatologists should exercise a high suspicion of syphilis in all asymptomatic eruptions.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Jain VK, Dayal S, Aggarwal K, Jain S. Changing trends of sexually transmitted diseases at Rohtak. Indian J Sex Trans Dis. 2008;29:23–5. [Google Scholar]
- 2.Ray K, Bala M, Gupta SM, Khunger N, Puri P, Muralidhar S, et al. Changing trends in sexually transmitted disease in a regional STD centre in north India. Indian J Med Res. 2006;124:559–68. [PubMed] [Google Scholar]
- 3.Schumacher CM, Ellen J, Rompalo AM. Changes in demographics and risk behaviors of person with early syphilis depending on epidemic phase. Sex Transm Dis. 2008;35:190–6. doi: 10.1097/OLQ.0b013e31815a88b0. [DOI] [PubMed] [Google Scholar]
- 4.Kar HH. Incidence of secondary syphilis on a rise and need for a separate flow chart for its syndromic management. Indian J Sex Trans Dis. 2004;25:22–5. [Google Scholar]
- 5.Anand BH, Vijaya D, Ravi R, Reddy RR. Study of genital lesions. Indian J Dermatol Vener Lepr. 2003;69:126–8. [PubMed] [Google Scholar]


