Abstract
Objective:
The anal sex among heterosexual couples is on the rise as reported in many scientific studies. Considering that unprotected anal sex has higher risk of human immunodeficiency virus (HIV) transmission than the vaginal sex, we undertook a study to understand the anal sex practices among Female Sex Workers (FSW).
Materials and Methods:
The study was conducted among FSW attending 11 randomly selected sexually transmitted infection (STI) clinics in Bill and Melinda Gates supported targeted interventions in Andhra Pradesh. A structured questionnaire was administered to the 555 FSW attending these clinics by project clinic counselors. Informed consent was obtained from all the study participants.
Results:
Engaging in anal sex was self reported by 22% of sex workers, though demand from clients was reported to be much higher (40%). The reasons for anal sex practices included more money (61%), clout/influence of the client (45%), risk of losing client (27%), and forced sex (1.2%). Factors associated with anal sex were higher number of clients, higher duration of sex work, higher income, and older age group. Associated risks perceived by FSW were bleeding and injury to anal canal (98%) while only 28% associated it with higher HIV transmission risk. Reported Condom and lubricant use was about 88% and 39% respectively.
Conclusion:
The study shows that there is frequent anal sex, inconsistent condom and infrequent lubricant usage, economic and physical coercion, and low awareness of STI/HIV transmission risk among FSW, which have serious implications for HIV prevention programmes. There is a need to focus on anal sex education and use of lubricants along with condoms during anal sex in FSW-targeted interventions in AP.
Keywords: Anal sex, female sex workers, human immunodeficiency virus, HIV transmission, sexually transmitted infection
INTRODUCTION
Unprotected anal sex is associated with the highest risk of transmission of sexually transmitted infections (STIs) and the human immunodeficiency virus (HIV).[1–4] The higher risk of STI/HIV transmission and acquisition is due to the highly vulnerable nature of the rectal mucosa and anal sphincter as any small tear of rectal mucosa in the receptive partner provides more opportunity for the transmission of HIV/STI. This risk is further increased if the receptive partner is female.[5–7] The estimated increase in risk of HIV transmission may be 20-fold per receptive anal sex act compared to receptive vaginal sex.[2]
Considering the global evidence of heterosexual anal sex,[8–23] it is likely that female sex workers (FSW) may also be engaging in similar practices, implying that HIV prevention programmes must explore and address the issue further. However, there is a paucity of data on anal sex prevalence among FSW, especially in India. Not only the few studies available from India reveal wide-ranging figures,[24–28] they also do not examine the frequency of sex or other associated factors, making it difficult to draw definite conclusions about anal sex practices within the country. The present study was undertaken to determine the prevalence and associated factors of anal sex practices among FSW in Andhra Pradesh (AP).
MATERIALS AND METHODS
A prospective study was designed to better understand the associated factors of anal sex practices among FSW in AP. A questionnaire was developed to collect information on the respondents’ knowledge and their practices pertaining to anal sex; their sexual characteristics; as well as basic demographic and socioeconomic factors. Eleven programme-owned STI clinics (known as Mythri clinics) of targeted interventions, where sex workers are provided regular STI services, were randomly selected from nine Bill and Melinda Gates Foundation supported intervention districts in AP. The sample size was calculated based on 15% rate of anal sex and 40% refusal rate for participation in the study. All the FSW consecutively attending these Mythri clinics for the first time during the month of December 2009 were included in the study. The study objectives were explained to the FSW and their consent for participation was sought. In total, of the 613 FSW attending the clinic during this period, 555 FSW gave their consent and participated in the study. The questionnaire was administered and one-to-one interviews conducted by trained clinic counselors. The study is limited by the fact that respondents were recruited from the STI clinics in Rayalseema and Telengana regions of AP, and so may not be representative of the FSW population of whole state. In addition, some desirability bias may also exist since the interviews were conducted by clinic counselors, and all the participants were exposed to the programme.
The data were entered and analyzed using SPSS (version 17) statistical package. The rate of anal sex among FSW was determined and univariate as well as bivariate analyses were undertaken to understand the relationship between associated factors such as their knowledge on risks associated with anal sex practice. Odd ratios were calculated at 95% confidence interval among key variables such as age, marital status and current living status, number of clients, and number of encounters. Pearson's Chi-square and two-tailed Fisher exact test for dichotomous variables and student t-test for continuous variables were calculated with a 95% significance level (P=0.05).
RESULTS
Profile of study participants
Of 613 respondents recruited, 555 interviews were completed, with a response rate of 90.5%. The results for these 555 questionnaires have been analyzed in the present study. The mean age of the respondents was 30.7 years (SD ± 6.1, range 18–50 years) and the majority were illiterate (54.1%); 70% were married and approximately 60% were still living with their husbands. The average monthly income earned was Rs. 4621 ± 3098. The FSW had been engaging in sex work for an average period of 6.34 years (SD ± 4.29), with an average of 7 clients (SD ± 4.9) and 8 (SD ± 5.9) sexual encounters per week. Money charged by the sex worker from the client varied with the type of sex act performed [Table 1], being lowest for oral sex at Rs 208.12 and the highest for multiple sex at Rs 578.90. The average fee charged for anal sex was Rs 316.09.
Table 1.
Demographic, sexual characteristics, and risk perception among FSW
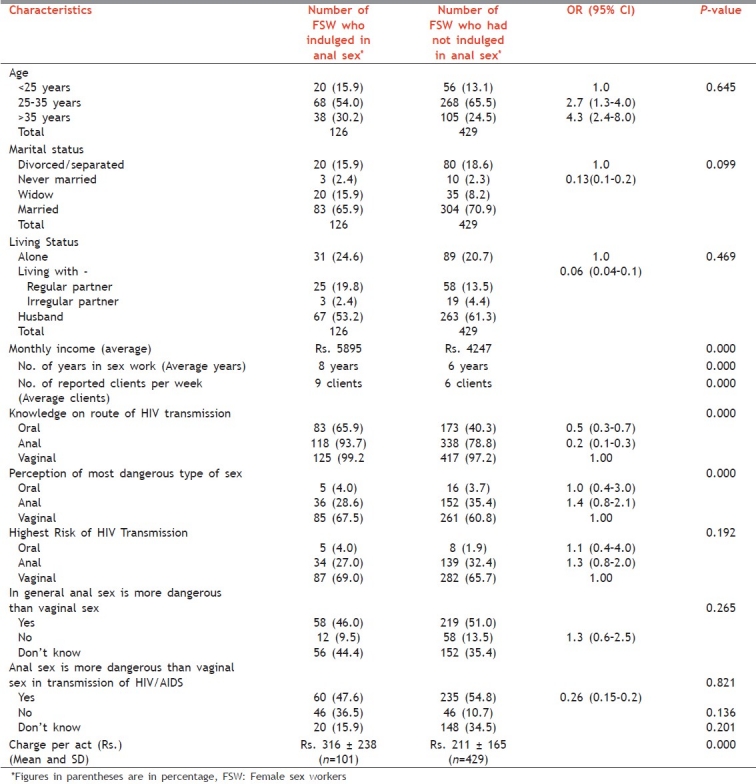
Table 1 shows demographic, sexual characteristics, and the risk perception of FSW who have and have not indulged in anal sex. The sex workers who engaged in anal sex were more likely to have had higher number of clients, higher duration of sex work, and had charged more from clients. The reported rate of anal sex was higher for FSW in the age group 25–35 years (odds ratio [OR] 2.7, 95% confidence interval [CI] 1.3–4.0) and those who were widowed/separated or lived alone. However, both were not statistically significant. The odds ratio for these was higher indicating greater likelihood of a sex worker indulging in anal sex when older or unmarried.
Prevalence of anal sex
Overall, 22.7% (n=126) of the respondents reported having ever engaged in anal sex. Of these, 25 (4.6%) sex workers had been forced into anal sex, while the others (n=101; 18.2%) admitted to regular practice. Even within the group admitting to regular anal sex practice, one-third of sex workers reported forced anal sex at some point or the other.
Risk perception and risk mitigation
Approximately 20% of all respondents were not aware that HIV can be transmitted through anal sex and only 33.9% perceived anal sex to have the highest risk of HIV transmission [Table 1]. Even though 53.2% (n=295) of FSW believed anal sex to be more dangerous than vaginal sex, they associated the dangers mostly with bleeding and physical trauma (98%), while only 27.5% perceived a higher risk of HIV transmission.
Condom use in the last anal sex encounter was reported by 88% of the FSW participating in consensual anal sex. Lubricant use in last anal sex encounter was reported by only 39% FSW and high proportion of these used oil-based lubricants (82%).
Demand and supply
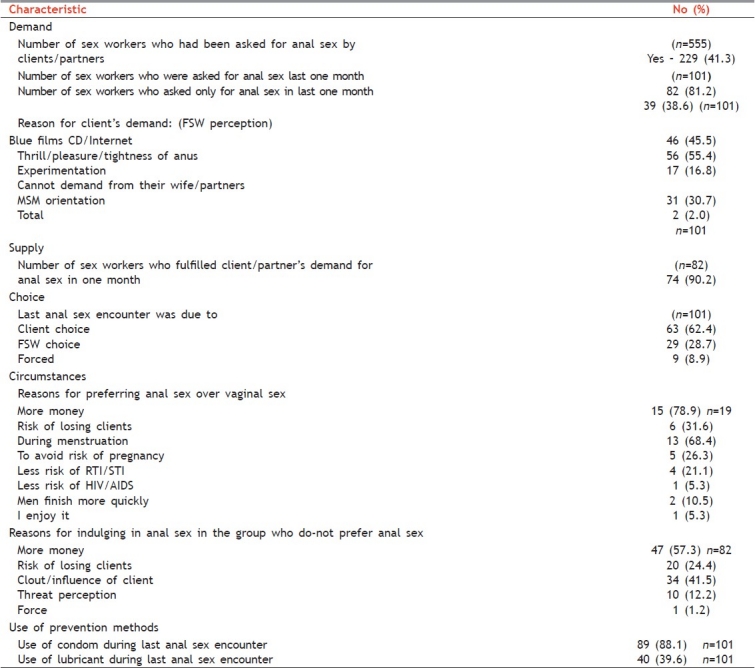
Of 555 respondents, 229 (31%) had reported receiving a demand for anal sex from their clients/partners, while 101 (18.2%) reported having fulfilled that demand. Of the cohort indulging in anal sex practices, 81% (n=82) had had a request for anal sex in the past 1 month, with 40% clients having demanded only anal sex. 90% of these requests had been fulfilled; 75% (n=74) reported having had anal sex in past 1 month, with an average of 1.77 encounters per month. A third of these sex workers (n=33) also reported at least one anal sex encounter in the past week. Not surprisingly, this service comes with a higher fee for the client, varying between Rs. 300 and Rs. 1500 per act. The sex workers engaged in anal sex with paying clients (52%), as well as partners (30%) or husband (18%).
Motivation for engaging in anal sex
The FSW perceived that the clients engage in anal sex for a greater level of thrill or pleasure (55.4%), are influenced by pornographic films or pornographic sites (45.5%), or due to a desire to experiment (16.8%) [Table 2]. The preference for anal sex is generally driven by the client. Of 101 FSW who reported regular anal sex practices, 19 (18.8%) preferred anal sex only. The reasons for preference included higher monetary returns, reduced risk of becoming pregnant, and being able to continue sex work during menstrual periods. The other 82 FSWs agreed for anal sex for monetary reasons (61%), fear of losing clients (26.8%), because of a threat perception from the client (12.2%), or because of actual force (1.2%).
Table 2.
Anal sex practice-demand, supply, choice and prevention techniques
DISCUSSION
The prevalence of anal sex among female sex workers in this study was 22%. Although a baseline study in 2005 among this population by Dandona et al.[24] reported a very low prevalence of anal sex (0.03%), recent studies reveal increasing trends in India.[25,27] The low prevalence reported in 2005 study could be the result of under reporting by the FSW due to stigma attached to anal sex or there may be an actual increase in the practice due to easy access to pornography as seen in the present study. This needs to be explored further. The fact that the FSW by now have been exposed to the programme for a long time and that the study was conducted by clinic counselors, might have helped FSW to be more open about their sexual practices. Our findings are consistent with the reports among high-risk groups from other parts of the world as well. Tian et al.[11] reported a rate of 39% anal intercourse among heterosexual women attending STD clinics in USA; however, the reported prevalence of anal intercourse was lower in African women (3.5–14%).[17–19] There is evidence to show that low reporting could be the result of ambiguous terminology[7,20,29] or of the reluctance of health worker/interviewer to probe the culturally-sensitive issue. Ferguson et al.,[20] after changing the terminology used for anal sex in their study questionnaire, showed an increase in FSW reporting anal sex, with prevalence of 20%. The recent CHARME study in Guntur district of AP[27] reported that two-thirds of the sex workers interviewed (n=60) engaged in anal sex. However, the sample size was very small and all sex workers were recruited from one particular area, making it difficult to draw any conclusions. Preliminary reports from a Behaviour Tracking Survey 2010 (unpublished data),[30] recently conducted by India HIV/AIDS Alliance among 2000 sex workers in AP, confirm high prevalence of anal sex (35.2%), substantiating our study findings.
More than 30% of those engaging in anal sex reported at least one encounter of anal sex during the last week recall, their average total weekly sexual encounters being eight. This has huge implications for HIV prevention programmes, as unprotected anal sex increases the probability of HIV transmission. Meta-analysis of studies from developed countries showed that probability of HIV transmission is higher (1.7%) per act for receptive anal sex as compared to penovaginal sex (0.8%), a 20-fold increase in the risk of HIV transmission per receptive anal sex act.[2] Moreover, Boily et al.[21] estimated that among heterosexual couples practicing anal sex, the cumulative risk of HIV acquisition within a period of 3 months can increase up to nine times in the woman if 2 out of their total 8 encounters are anal sex. Therefore, the role of anal sex practices among FSW cannot be ignored in the spread of the HIV epidemic.
The significant associated factors for engaging in anal sex included the following: Higher number of clients per week, longer duration into sex work, and potential for gaining higher income [Table 1]. With advancing age, the likelihood of engaging in anal sex becomes higher, with 2.7 times higher odds in age group of 25–35 years and 4.3 times for those older than 35 years. Women who are married or are living with a partner are less likely to practice anal sex than those who are not married, or are separated and widowed, or living alone (OR: 0.13 and 0.06, respectively). It is important to note here that the majority of sex workers were indulging in these practices to fulfill the client's demand, especially due to economic compulsions. A significant proportion of the respondents (48.4%) also reported physical coercion at one point of time or another. Another reason why some FSW feel compelled to offer anal sex to demanding clients is explained by “age-related diminishing demand.” FSW operate in a demand-driven market which makes it all the more difficult for them to refuse anal sex and amplifies economic vulnerability. The demand for anal sex from clients is high and increasing due to easy access to pornography and the desire to experiment. While reasons such as avoiding pregnancy or avoiding contact with menstrual blood, as cited in other studies,[6,9] were also reported, it is clear that the practice of engaging in anal sex is, to a large extent, a demand-driven practice.
The low levels of risk awareness and perception regarding HIV transmission through anal sex among FSW is a cause for serious concern. Twenty percent of respondents were not aware that STI/HIV can be transmitted through the anal route and 80% perceived the anal sex practice to have a lower risk of STI/HIV transmission than vaginal sex. Caetano et al.[23] reported 50%–60% of students interviewed in Brazil knew that HIV can be transmitted through anal sex. In our study, even though the FSW believe anal sex to be more dangerous, 98% associated it with pain and rectal bleeding, probably because these are the immediate problems they experienced.
The study does report a higher use of condoms (88%) during the last anal sex act. This is much higher than what has been reported in other studies.[17,27] Our study did not explore aspects related to consistent condom use and since interviews were conducted by clinic counselors who have been providing regular risk-reduction counseling to these FSW, the above could be a socially biased response. In the Behaviour Tracking Survey 2010,[30] even though last time condom use for anal and vaginal sex were reported as 90% and 99.4%, respectively, consistent condom use for vaginal sex with paying clients was about 72% and only 14% with regular partners. During focused group discussions on anal sex and condom use, sex workers had reported lower condom use,[28] stating it is difficult for them to confirm the use of condoms during anal sex. Moreover, it was revealed that anal sex took place several times in situations of group sex at the clients’ place, where condom use was not possible. In this study, 60% FSW were either not using a lubricant or reported the use of oil-based lubricants. It is well documented that unless lubricant is used, chances of condom slippage or breakage are much higher with anal sex than with vaginal sex.[31]
CONCLUSION
In conclusion, while the practice of anal sex is quite common among FSW, their perception of HIV transmission/acquisition risks associated with anal sex is alarmingly low. In addition, there is a high demand from clients, including physical coercion, for anal sex, which is further compounded by economic compulsions. It is important for HIV prevention programmes to focus not only on vaginal sex but also on the risks involved with anal sex. Outreach messaging should focus on awareness about its associated risks and should promote the use of condoms and water-based lubricants. Concurrently, the skills of both technical and nontechnical staff involved in STI control and management, as well as HIV prevention programmes, need to be enhanced. More research studies in diverse sociodemographic and geographical settings around the country will help to better understand these dynamics and to thus better inform the design and implementation of HIV prevention programmes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Leyneaert B, Downs AM, de Vincenzi I. Heterosexual transmission of human immunodeficiency virus: Variability of infectivity throughout the course of infection. European Study group on Heterosexual Transmission of HIV. Am J Epidemiol. 1998;148:88–96. doi: 10.1093/oxfordjournals.aje.a009564. [DOI] [PubMed] [Google Scholar]
- 2.Boily MC, Baggley R, Wang L, Masse B, White RG, Hayes RJ, et al. Heterosexual risk of HIV-1 infection per sexual act: Systematic review and meta-analysis of observational studies. Lancet Infect Dis. 2009;9:118–29. doi: 10.1016/S1473-3099(09)70021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jaffe H, Janssen R. Incorporating HIV prevention in the medical care of persons living with HIV. MMWR Recomm Rep. 2003;52:1–24. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, Atlanta Report. Sexually Transmitted Disease Surveillance. 2008. Available from ww.cdc.gov/std/stats .
- 5.Rosenthal SM. The Gynaecological Sourcebook. 4th ed. New York: McGraw-Hill Publications; 2003. p. 153. [Google Scholar]
- 6.Halperin DT. Heterosexual anal intercourse: Prevalence, cultural factors, and HIV infection and other health risks, part I. AIDS Patient Care STDs. 1999;13:717–30. doi: 10.1089/apc.1999.13.717. [DOI] [PubMed] [Google Scholar]
- 7.Voeller B. AIDS and heterosexual anal intercourse. Arch Sex Behav. 1991;20:233–76. doi: 10.1007/BF01541846. [DOI] [PubMed] [Google Scholar]
- 8.Best K. Anal intercourse presents serious HIV/STI Risks. Network. 2001;20:29. [Google Scholar]
- 9.Mosher WD, Chandra A, Jones J. Sexual Behavior and Selected Health Measures: Men and Women 15–44 Years of Age, United States, 2002. Adv Data. 2005;15:1–56. [PubMed] [Google Scholar]
- 10.National Survey of Sexual Health and Behavior (NSSHB) Findings from the National Survey of Sexual Health and Behavior, Centre for Sexual Health Promotion, Indiana University. J Sex Med. 2010;7:362–73. doi: 10.1111/j.1743-6109.2010.02038.x. [DOI] [PubMed] [Google Scholar]
- 11.Tian LH, Peterman T, Tao G, Brooks LC, Metcalf C, Malotte CK, et al. RESPECT-2 Study Group. Heterosexual anal sex activity in the year after an STD clinic visit. Sex Transm Dis. 2008;35:905–9. doi: 10.1097/OLQ.0b013e318181294b. [DOI] [PubMed] [Google Scholar]
- 12.Johnson AM, Mercer CH, Erens B, Copas AJ, McManus S, Wellings K, et al. Sexual behavior in Britain: Partnerships, practices, and HIV risk behaviours. Lancet. 2001;358:1835–42. doi: 10.1016/S0140-6736(01)06883-0. [DOI] [PubMed] [Google Scholar]
- 13.McDonald NE, Wells GA, Fisher WA, Warren WK, King MA, Doherty JA, et al. High-risk STD/HIV behaviour among college students. JAMA. 1990;263:3155–9. [PubMed] [Google Scholar]
- 14.Leichliter JS. Heterosexual Anal Sex: Part of an Expanding Sexual Repertoire? Sex Transm Dis. 2008;35:910–1. doi: 10.1097/OLQ.0b013e31818af12f. [DOI] [PubMed] [Google Scholar]
- 15.Avasthi A, Kaur R, Prakash O. Sexual Behaviour of Married Young Women: A Preliminary Study from North India. Indian J Community Med. 2008;33:163–7. doi: 10.4103/0970-0218.39677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verma RK. Homosexual Activity among Rural Indian Men: Implications for HIV Interventions. AIDS. 2004;18:1845–7. doi: 10.1097/00002030-200409030-00014. [DOI] [PubMed] [Google Scholar]
- 17.Kalichman SC, Simbayi LC, Cain D, Jooste S. Heterosexual anal intercourse among community and clinical settings in Cape Town, South Africa. Sex Transm Infect. 2009;85:411–5. doi: 10.1136/sti.2008.035287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skoler Karpoff S, Ramjee G, Ahmed K, Altini L, Plagianos MG, Friedland B, et al. Efficacy of Carraguard for prevention of HIV infection in women in South Africa: A randomized, double-blind, placebo controlled trial. Lancet. 2008;372:1977–87. doi: 10.1016/S0140-6736(08)61842-5. [DOI] [PubMed] [Google Scholar]
- 19.Lane T, Pettifor A, Pascoe S, Fiamma A, Rees H. Heterosexual anal intercourse increases risk of HIV infection among young South African men. AIDS. 2006;20:123–5. doi: 10.1097/01.aids.0000198083.55078.02. [DOI] [PubMed] [Google Scholar]
- 20.Ferguson A, Morris C. Assessing the role of anal intercourse in the epidemiology of AIDS in South Africa (letter) Int J STD AIDS. 2003;14:856. doi: 10.1258/095646203322556228. [DOI] [PubMed] [Google Scholar]
- 21.Boily MC, Baggaley R, Masse B. The role of heterosexual anal intercourse for HIV transmission in developing countries: Are we ready to draw conclusions? Sex Transm Infect. 2009;85:408–10. doi: 10.1136/sti.2009.037499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen B, Cruz-Valdez A, Rivera-Rivera L, Castro R, Arana-García ME. Affection, kisses and condoms: The basics of sexual practices of female sex workers in Mexico City] Afecto, besos y condones: El ABC de las prácticas sexuales de las trabajadoras sexuales de la Ciudad de México. Salud Púlica de México. 2003;45:S594–607. [PubMed] [Google Scholar]
- 23.Caetano ME, Linhares IM, Pinotti JA, Maggio da Fonseca A, Wojitani MD, Giraldo PC. Sexual behavior and knowledge of sexually transmitted infections among university students in Sao Paulo, Brazil. Int J Gynaecol Obstet. 2010;110:43–6. doi: 10.1016/j.ijgo.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Dandona R, Dandona L, Gutierrez JP, Kumar AG, McPherson S, Samuels F, et al. High risk of HIV in non-brothel based female sex workers in India. BMC Public Health. 2005;5:87. doi: 10.1186/1471-2458-5-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mondal S, Ramesh B, Blanchard JF, Moses S. Condom-Use and Experience of Violence: Evidence from Polling Booth Survey among Female Sex-Workers in Karnataka, India. International Conference AIDS. 2006 Aug 13-18; 16 Abstract No. MoPE0605. [Google Scholar]
- 26.Bradley J, Shetty A, James A. HIV Risk and Vulnerability in Female Sex Workers in Mumbai: Reflection From The Field. CHARME Working Paper No 8. 2010 Apr [Google Scholar]
- 27.Beattie T, Bradley J, Shetty A, Vanta UD, Lowndes CM, Alary M. The evolution of female sex workers in Guntur, Andhra Pradesh: A qualitative study of HIV related issues. CHARME Working Group Paper No 5. 2009 Oct [Google Scholar]
- 28.Matheou A. A blind spot in HIV prevention - Female anal sex. Issue Brief. Available from: http://www.aidsallianceindia.net/?q=node/40andpid=173 .
- 29.Ndinda C, Chimbwete C, McGrath N, Pool R. Perceptions of anal sex in rural South Africa. Cult Health Sex. 2008;10:205–12. doi: 10.1080/13691050600988416. [DOI] [PubMed] [Google Scholar]
- 30.Behaviour Tracking Survey. India HIV/AIDS Alliance. 2010 [Google Scholar]
- 31.Smith A, Jolley D, Hocking J, Benton K, Gerofi J. Does additional lubrication affect condom slippage and breakage? Int J STD AIDS. 1998;9:330–5. doi: 10.1258/0956462981922359. [DOI] [PubMed] [Google Scholar]


