Abstract
Toxic Epidermal Necrolysis (TEN) and Steven-Johnson Syndrome (SJS) are serious disorders commonly caused as idiosyncratic reactions to drugs, the most common ones being oxicams, anticonvulsants, allopurinol, and sulfonamides. We present a case of TEN in a patient who developed the lesions after ingesting multiple drugs including paracetamol, metoclopramide, antihistamines, and multivitamins. These drugs have rarely been implicated in this disorder. The suspected drugs in this case were paracetamol and metoclopramide. However, the role of other drugs could not be ruled out definitely. The patient was managed with antibiotics, corticosteroids, and parenteral fluids and recovered well.
KEY WORDS: Adverse drug reactions, metoclopromide, paracetamol, Toxic Epidermal Necrolysis
Introduction
Toxic epidermal necrolysis (TEN) is a rare life threatening idiosyncratic mucocutaneous drug reaction characterized by widespread epidermal necrosis followed by epidermal detachment. Drugs, infections and immunizations are the most common causes of TEN. Drug-induced TEN is the commonest cause and antiepileptics, antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDS) and allopurinol are the most commonly implicated agents. Here we report a case of TEN which was induced by multiple drugs some of which have been rarely implicated in the causation of TEN.
Case Report
A 42-year-old woman was referred to medical emergency with extensive epidermal detachment and ocular, genital, and oral lesions of 5 days duration leading to a diagnosis of Toxic Epidermal Necrolysis (TEN). Seven days prior to this admission, she had presented to a general practitioner with symptoms of vertigo, anxiety, and restlessness. Although no provisional or differential diagnosis was found in the documents provided by the patient, she was prescribed antihistamines (cinnarizine and dimenhydrinate), paracetamol/metoclopramide combination and multivitamins. After 8-12 hours, she developed fever, malaise, sore throat, and erythematous maculopapular rash in the perioral region.
She discontinued all medications and was admitted to a general hospital where she was administered piperacillin/tazobactam and dexamethasone. It is unknown whether paracetamol or antihistamines were restarted in the hospital. Her condition deteriorated and she was referred to our hospital. On presentation, she was conscious and afebrile; her heart rate was 110/min and blood pressure was 190/80 mm Hg. Cutaneous examination showed involvement of about 70% total body surface area, with skin necrosis, tenderness, and a positive Nikolsky's sign. There were ulcerations and crusting on oral and genital mucosa. Ocular examination revealed serous discharge along with erosions and crusting of eyelids. She had a history of hypertension and was on some antihypertensive medication (unknown) for a few years. Her hematological and biochemical reports are mentioned in Table 1.
Table 1.
Test reports at three time-points
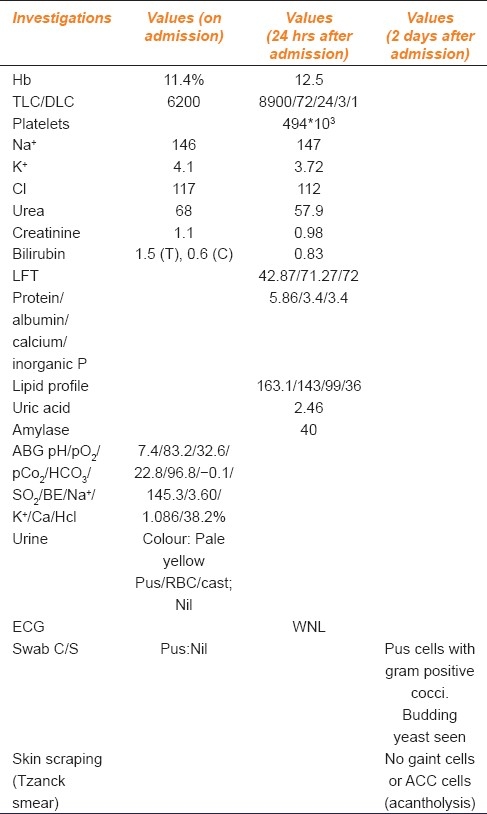
She was administered intravenous fluids, antihypertensive treatment (amlodipine 5 mg/day), injection hydrocortisone (50 mg IV twice daily), and continued on the same antibiotics. Wound care was given by applying topical antiseptics on eroded areas along with nonadherent dressings. Biochemical reports showed a decrease in blood urea (from 68 mg/dl on admission to 57.6 mg/dl on the second day after admission) and a decrease in serum creatinine (from 1.1 mEq/L on admission to 0.78 mEq/L on the second day after admission) [Table 1]. Parenteral therapy was gradually replaced by oral drugs. On the fourth day, she developed herpetic lesions on the oral mucosa and for that tablet acyclovir was advised thrice a day along with chlorhexidine mouthwash, syrup mucaine gel (antacid), and white petroleum jelly for lips. A Tzanck smear, done on fifth day after admission, failed to show any giant cells or Acantholytic Cells (ACC) [Table 1]. This test was done to rule out pemphigus. The patient showed steady improvement with the therapy given and was discharged, after 8 days, without any sequelae.
Discussion
This is most likely a case of drug-induced TEN as other causes like upper respiratory tract infection, viral infection, or malignancy were not present. As this was an acute presentation, which occurred right after the drugs were administered, Systemic Lupus Erythematosus (SLE) and rheumatological disorders were ruled out. Pemphigus was ruled out, as the results of the Tzanck smear were negative. TEN was diagnosed from the history and typical clinical features and biopsy was not needed. The prodrome was shorter (8-12 hrs) than the usual 1-3 days. This might have been due to the use of multiple drugs causing an unknown interaction or more likely due to a previous exposure to any or all of these drugs. Causality assessment was done for each of the drugs separately by the method of Kramer et al.[1] Paracetamol and metoclopramide were categorized as probable (score 5) and antihistamines and multivitamins as possible (score 3) causal drugs for this adverse drug reaction. The patient was also on some unknown antihypertensive drug for some years. Since this drug intake was uneventful for a long time, the chances of this medication causing this episode of TEN are minimal.
There have been two case reports[2,3] of TEN caused by paracetamol and a case control study[4] showing increased risk of SJS or TEN with paracetamol use. Metoclopramide can also cause TEN according to a case report.[5] There have been no case reports of TEN due to a combination of both the drugs, nor have there been any reports regarding TEN being caused by antihistamines or multivitamins. The most likely cause of TEN in this case was paracetamol/metoclopramide. However, the probability of other drugs being responsible could not be ruled out completely. Rechallange was not done as it would be clinically unjustifiable.
Conclusion
TEN in this patient was probably caused by paracetamol and metoclopramide, but a possibility of an interaction as well as the role of other drugs cannot be ruled out.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Kramer MS, Leventhal JM, Hutchinson TA, Feinstein AR. An algorithm of Operational assessment of adverse drug reactions. JAMA. 1979;242:623–32. [PubMed] [Google Scholar]
- 2.Bygum A, Gregersen JW, Buus SK. Acetaminophen-induced toxic epidermal necrolysis in a child. Pediatr Dermatol. 2004;21:236–8. doi: 10.1111/j.0736-8046.2004.21309.x. [DOI] [PubMed] [Google Scholar]
- 3.Aalevi A, Ben-Amitai D, Garty BZ. Toxic epidermal necrolysis associated with acetaminophen ingestion. Ann Pharmacother. 2000;34:32–4. doi: 10.1345/aph.19064. [DOI] [PubMed] [Google Scholar]
- 4.Roujeau JC, Kelly JP, Naldi L, Rzany B, Stern RS, Anderson T, et al. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995;333:1600–7. doi: 10.1056/NEJM199512143332404. [DOI] [PubMed] [Google Scholar]
- 5.Metoclopromide: First report of toxic epidermal necrolysis: Case report. React Wkly. 2008;1189:25. [Google Scholar]


