Abstract
Background/Aim:
There is ample evidence in the recent literature that gum chewing after elective colonic anastomosis decreases postoperative ileus (POI). But there are very few studies on small bowel anastomosis done in relaparotomy cases. This study aimed to evaluate the effect of gum chewing on the duration of POI following small bowel anastomosis performed for the closure of intestinal stoma, made as temporary diversion in the selected cases of typhoid perforation peritonitis.
Patients and Methods:
Hundred patients undergoing elective small bowel anastomosis for the closure of stoma were randomly assigned to the study group (n=50) and the control group (n=50). The study group patients chewed gum thrice a day for 1 h each time starting 6 h after the surgery until the passage of first flatus. The control group patients had standard postoperative treatment.
Results:
Study and control group patients were comparable at inclusion. The mean time for the appearance of bowel sounds as well as the passage of first flatus was significantly shorter in the study group (P=0.040, P=0.006). The feeling of hunger was also experienced earlier in study group cases (P=0.004). The postoperative hospital stay was shorter in the study group, but the difference was not significant (P=0.059).
Conclusions:
The cases of relaparotomy requiring additional adhesiolysis and small bowel anastomosis for stoma closure are benefited by postoperative gum chewing.
Keywords: Gum chewing, ileostomy closure, typhoid perforation
Postoperative ileus (POI) is defined as the transient inhibition of normal gastrointestinal motility following abdominal surgery, typically lasting for 3-5 days.[1] It is an inevitable response to surgical trauma leading to uncomplicated ileus where the areas of gastrointestinal tract resume function at different times. The small intestine recovers the normal function first, usually within the first 24 h, followed by the stomach about 12-24 h later; and recovery of the normal large intestine function usually takes between 48 and 72 h.[2] Thus, in uncomplicated ileus, gastrointestinal motility is reestablished within 3 days. If POI lasts longer than 3 days, it is thought to be complicated and may be termed as postoperative paralytic ileus.
Conventionally, POI has been managed by gastric decompression by Ryle's tube, keeping the patient nil per orally, intravenous fluid supplementation till ileus resolves, and patient passes flatus.[2] However, very few improvements in the understanding of POI have occurred in the past 100 years, and therefore therapies have changed little.
To date, no definite treatment for POI has been approved by the US Food and Drug Administration.
In recent years, the use of gum chewing has emerged as a new and simple modality for decreasing POI. It acts by stimulating intestinal motility through cephalic vagal reflex and by increasing the production of gastrointestinal hormones associated with bowel motility.[3] Recently, it has been proposed that hexitols present in sugarless chewing gums might also be playing a role in the amelioration of POI because these are known to cause gastrointestinal symptoms such as gas, bloating, and abdominal cramps in a dose-dependent manner.[4] The published literature reveals that gum chewing in the postoperative period is a safe method to stimulate bowel motility and it has been shown to reduce ileus after elective colonic anastomosis.[5–7] However, there are very few reports on the role of gum chewing in improving POI following small intestinal anastomosis.[8] Cases undergoing relaparotomy are also likely to have prolonged POI due to additional gut handling as a result of adhesiolysis. Our department gets a large number of cases requiring relaparotomy for the closure of ileostomy stoma created as diversion in the selected cases of perforation peritonitis following typhoid fever, and these cases are likely to have prolonged POI.
Hence this study was conducted to evaluate the role of gum chewing in patients undergoing relaparotomy for stoma closure and compare it with a similar control group to measure the return of bowel function and feeling of hunger, length of hospital stay, and postoperative complications.
PATIENTS AND METHODS
This prospective, comparative trial was undertaken at Postgraduate Institute of Medical Sciences, Rohtak, India, from May 2006 to December 2009 after obtaining approval of the Institute Ethics Committee, and an informed written consent was taken from all enrolled patients. All patients underwent relaparotomy for elective small intestinal anastomosis for the closure of stoma that was made earlier as a temporary diversion in selected cases of typhoid perforation peritonitis. During the study period, although ileostomy was also carried out for other indications, for example, tubercular perforation, mesenteric vascular thrombosis, postlaparotomy adhesive intestinal obstruction, and cecal volvulus, but those cases were excluded. The patients were divided into two groups of 50 each by drawing a slip.
In the study group, 50 patients were asked to chew gum thrice a day for 1 h each time starting from 6 h after the surgery until the passage of first flatus. Commercially available sugar-free gum (Orbit) was used for this study. The nasogastric tube was removed after the passage of first flatus and oral intake was allowed thereafter.
In the control group, 50 patients were kept nil orally in the postoperative period until the passage of first flatus. The nasogastric tube was removed after the passage of first flatus and oral intake was allowed thereafter.
All the cases were built up preoperatively with enteral nutrition and hematinics wherever indicated. Electrolyte imbalance, if any, was corrected, and any comorbid illness was optimized before surgery. Preoperative bowel preparation was done by using oral polyethylene glycol solution in all the cases. The large gut was cleaned with saline enema since all the patients had a small intestinal stoma. A broad-spectrum antibiotic, cefotaxime 1 g, was administered 1 h before the surgery. All the patients underwent interrupted single-layer extramucosal intestinal anastomosis. In the postoperative period, injections of cefotaxime, amikacin, and metronidazole were given for 3 days.
All the patients were operated under general anesthesia using propafol, diclofenac sodium, and inhalational agents by two surgical consultants of the rank of associate professor or professor. The details of operative procedures were recorded, including adhesiolysis (if any), type of anastomosis, blood loss, and duration of surgery.
Postoperatively, all the cases were monitored for any distention, time of appearance of bowel sounds, time of passage of the first flatus and stool, return of appetite, and complications (if any) were recorded. For postoperative pain relief, an injection of diclofenac sodium was given 8 hourly for the initial 3 days after the surgery and then it was given as per demand. Epidural analgesia, narcotic analgesics, and prokinetic drugs that are known to influence POI were not used. Chest physiotherapy was started on the evening of surgery, and early ambulation was encouraged. Oral feeds were started after the passage of flatus and then diet was advanced as per the discretion of the surgical team.
Patients were discharged when they passed stool, started taking regular meals, and had no complications. The duration of postoperative hospital stay and mortality (if any) were recorded. They were followed up for 3 months. Any patient requiring readmission due to intestinal obstruction was also recorded.
Statistical analysis
The statistical package for social sciences (SPSS) software version 12.0 was used for the statistical analysis. A probability value of less than 5% (P<0.05) was considered significant. Student's t test was used for the comparison of continuous variables between the two groups. The Chi-square test was used to check for differences between proportions.
RESULTS
A total of 100 patients who had previously undergone ileostomy for typhoid perforation peritonitis were prospectively randomized into 50 patients each in the study as well as the control group. The cases were diagnosed on the basis of serology, blood culture, and biopsy report of the resected gut, and all eligible patients that presented during the study were included. A majority of the patients in both the groups were males and in the age group of 21-50 years. The mean age of the patients was 36.90±15.97 years in the study group and 39.94±15.75 years in the control group. Hypoproteinemia and anemia were the most common deficiencies seen in 38 patients of the study group and in 34 patients of the control group. These patients needed preoperative building up and correction of the electrolyte imbalance before they were subjected to stoma closure. The excoriation of the skin demanded early stoma closure in 10 patients of the study group and 13 patients of the control group. Both the groups were statistically comparable with respect to demographic and surgical characteristics [Table 1].
Table 1.
Demographic and surgical characteristics
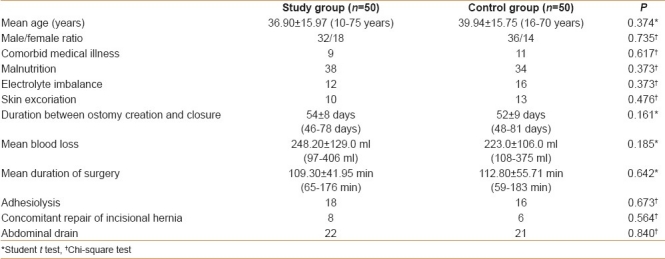
During surgery, intraoperative blood loss was less than 300 ml in the majority of the patients in both the groups and the difference was statistically insignificant (P=0.185).
The mean duration of surgery was 109.30±41.95 min in the study group and 112.80±55.71 min in the control group. The difference was statistically insignificant (P=0.642). Eight cases in the study group and six cases in the control group underwent anatomical repair of incisional hernia as well at the time of stoma closure, and these cases obviously took longer time for surgery.
Adhesions were encountered in the majority of the cases. Eighteen cases of the study group and 17 cases of the control group required adhesiolysis, and their number was comparable among the two groups (P=0.673).
In cases having persistent ooze at the time of wound closure, an intra-abdominal drain was placed in 22 cases of the study group and 21 cases of the control group. The drain was removed when the amount of drainage fluid was less than 20 ml/day. No statistically significant difference was found regarding the duration of intra-abdominal drainage in both the groups (P=0.840). The postoperative monitoring of cases in both the groups is shown in Table 2.
Table 2.
Postoperative monitoring
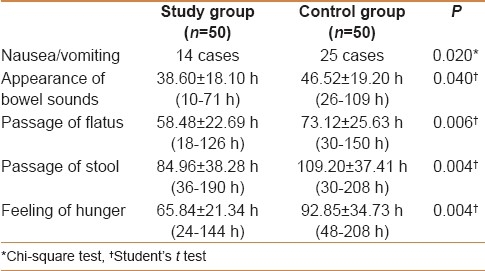
Fourteen patients in the study group and 25 patients in the control group experienced postoperative nausea and vomiting. On statistical analysis, the incidence of nausea and vomiting was significantly more in the control group as compared to the study group (P=0.020). However, postoperative abdominal distention was comparable among the two groups (P=0.362).
The mean time for the appearance of bowel sounds was 38.60±18.10 h in the study group and 46.52±19.20 h in the control group. On statistical analysis, bowel sounds appeared significantly earlier in the study group cases as compared to the control group cases (P=0.040).
The recovery of gastrointestinal motility was determined by the passage of first flatus and bowel movement postoperatively. The mean time for the passage of first flatus was 58.48±22.69 h in the study group (range 18-126 h) and 73.12±25.63 h in the control group (range 30-150 h). On statistical analysis, the patients in the study group passed flatus in a significantly shorter period of time than the patients in the control group (P=0.006). The mean time for the passage of first stool was 84.96±38.288 h in the study group (range 36-190 h) and 109.20±37.41 h in the control group (range 30-208 h), and the difference among the two groups was statistically significant (P=0.004). The patients in both the groups were allowed oral intake after they had passed flatus the first time.
The feeling of hunger was experienced earlier in the study group (mean time 65.84±21.34 h) in comparison to the control group cases (mean time 92.85±34.73 h), and the difference was statistically significant (P=0.004).
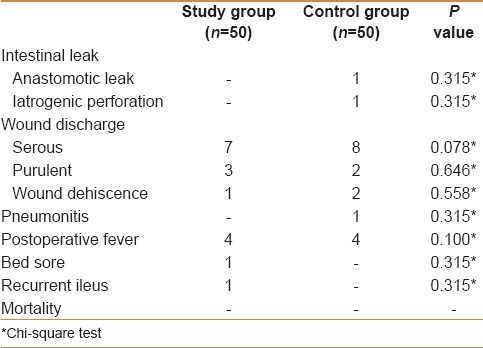
Two patients in the control group had intestinal leak in the postoperative period. One patient had an anastomotic leak, while in another case, the leak occurred from an occult iatrogenic injury of small gut caused by cautery dissection for adhesiolysis and the anastomosis was intact. Both cases were managed by end ileostomy. In them, time to passage of flatus, passage of stool, and feeling of hunger could not be assessed. Other postoperative complications were comparable in two groups as evident from Table 3.
Table 3.
Postoperative complications
All patients in the study group tolerated gum chewing quite well. Twelve patients continued to chew gum even after being asked to stop since they had passed flatus as they found it refreshing and appetizing.
The patients were discharged when they had passed stools, had started taking regular meals, and had no complications. The hospital stay was found to be shorter in the study group cases (mean 8.30±2.91 days) as compared to the control group cases (mean 9.60±4.18 days), but the difference was not statistically significant (P=0.059).
One patient of the study group was readmitted 3 days after the discharge due to adhesive intestinal obstruction. He was managed conservatively and discharged.
DISCUSSION
POI occurs commonly after abdominal operations and is one of the limiting factors preventing early hospital discharge.[2] Apart from spinal and local sympathetic neural reflexes, the pathophysiology of POI includes local as well as systemic inflammatory mediators released during surgery as part of the stress response.[1] The other exacerbating factors include type of anesthetic drugs (atropine, enflurane, halothane),[9] use of opioid analgesics, intraperitoneal surgery, degree of bowel manipulation, open vs laparoscopic surgery, and postoperative hypokalemia.[1] Ileus is also related to the anatomic location of gut resection. The time for restoration of motility is the longest after colorectal surgery.[5]
The potential complications of prolonged POI include increased postoperative pain, increased nausea and vomiting, pulmonary complications, poor wound healing, delay in resuming oral intake, delay in postoperative mobilization, prolonged hospitalization, and increased health-care costs. The estimated economic impact of POI in the United States is $7.5 billion per year, excluding the expenses of work loss.[10,11]
In view of the potential complications and high economic impact, a number of pharmacological as well as nonpharmacological approaches have been used to decrease the burden of POI.[12,13] These programs involve transverse or curved surgical incisions, removal of nasogastric tubes at the end of anesthesia, intraoperative and postoperative analgesia, use of peripherally active mu-opioid receptor antagonist (alvimopan), early postoperative feeding, mobilization, and gum chewing/sham feeding. Multimodality therapy including a combination of various approaches may reduce POI by acting through multiple mechanisms. A recently conducted review evaluating pharmacological options to prevent POI concluded that gum chewing and alvimopan are effective in preventing POI, but given safety concerns (risk of myocardial infarction) and higher cost with alvimopan, gum chewing may be preferred.[14]
Sham feeding has been demonstrated to be one of the methods to increase bowel motility.[15,16] It causes both vagal stimulation and hormonal release; either one or both could modulate the bowel motility. Gum chewing, as an alternative to sham feeding, provides the benefits of gastrointestinal stimulation without the complications associated with feeding.[17] In recent years, the use of gum chewing to reduce ileus has been extensively reviewed in various randomized controlled trials on elective intestinal anastomosis and has been found to be beneficial in reducing POI.[5,7,8,18] These reviews have concluded that there is consistent benefit for patients from gum chewing after the intestinal surgery in the form of decreased time to first flatus, bowel movements, and postoperative hospital stay. Although the evidence is based on small trials, such a potentially simple and cheap intervention could have important health and economic benefits. In view of these observations, State University of New York - Upstate Medical University is sponsoring and currently recruiting participants to evaluate the role of gum chewing in reducing POI after elective laparoscopic colectomy.[19] In abdominal surgery, apart from intestinal anastomosis, the gum chewing has also proved to be useful in decreasing POI following caesarian section.[20]
A majority of the studies on gum chewing included cases of colonic anastomosis only and there are very few such trials on elective small gut anastomosis. Some of the studies specifically excluded cases with small gut anastomosis.[21] It is probably because early enteral nutrition is considered to be more difficult to achieve in upper abdominal surgery.[8] It is also possible since most of the published studies are from the West and there are very few indications of elective small gut anastomosis as compared to countries such as India. In one trial, radical cystectomy with urinary diversion with ileal conduit was done in 102 patients and gum chewing has been found to be useful in decreasing POI.[22] However, this kind of surgery is associated with a longer operative time as well as increased complications. Interestingly, in a small trial including 30 children with colon and small bowel resection, gum chewing was not found to be associated with a significant improvement in POI.[23]
Relaparotomy is considered to be another important factor causing prolonged POI. As per literature, numerous studies have been conducted on evaluating the role of gum chewing in intestinal anastomosis, but there are very few cases of relaparotomy and their description is poor. In a recently conducted review of nine such trials including 437 patients, only three trials had included a few cases of relaparotomy.[8]
Our institute is a tertiary care center located in North India catering largely to poor rural population. We get a large number of referrals with ileal perforations due to typhoid fever. The usual operative findings in such cases are gross fecal soiling of peritoneal cavity, inflamed and friable distal ileum having multiple perforations. After the resection of the perforated segment of ileum and peritoneal lavage, end ileostomy with the closure of distal stump is usually performed as a lifesaving measure in such individuals. One such study from Pakistan has also shown that ileostomy proves to be lifesaving procedure in such cases.[24]
In view of these observations, the present study was planned as a prospective randomized controlled trial including 100 such cases of relaparotomy for elective small bowel anastomosis for stoma closure. In all the cases, stoma was created for typhoid perforation of small gut that usually affected the younger age group. None of the previous studies have mentioned about relaparotomy for stoma closure.
The duration of surgery is known to affect POI. In the present study, all the cases required 1-2 h of operating time. The mean duration of surgery was 109.30±41.955 min in the study group and 112.80±55.71 min in the control group, which was comparable. Our results regarding the duration of surgery are comparable with most of the previous studies except Asao et al.,[3] where surgeries took longer time because of these being done laparoscopically.
Since there is often gross inflammation of the tissues and fecal contamination during initial surgery for typhoid perforation of the ileum, adhesions is a common finding while venturing stoma closure as observed in almost one-third cases in the present study. The number of cases requiring extensive adhesiolysis was comparable in the two groups. This parameter has not been studied earlier because majority of the studies included elective colonic resections for malignancy and have included only a few cases of relaparotomy.[21,25,26]
The incidence of postoperative nausea and vomiting was significantly more in the control group in comparison to the study group (P=0.020). Since demographic profile of the patients was the same in two groups Table 1, gum chewing was possibly responsible for the decreased incidence of nausea and vomiting in the postoperative period. This parameter has not been analyzed in any of the previous studies.[8]
All patients in the study group were asked to chew sugarless gum. Twelve patients in the study group continued to chew gum even after passing flatus since they found it refreshing and appetizing. One of the previous studies has also observed subjective benefit of gum chewing since it kept the mouth moist after surgery.[26] On cost analysis, it was found that gum chewing was very cheap, costing less than $1 for 4 days. The cost of chewing gum is negligible in comparison to the cost of hospital stay, as has been observed in some studies.[25,27]
The mean time for the appearance of bowel sounds was significantly shorter in the study group (P=0.040). None of the earlier authors have studied the appearance of bowel sounds in the two groups.
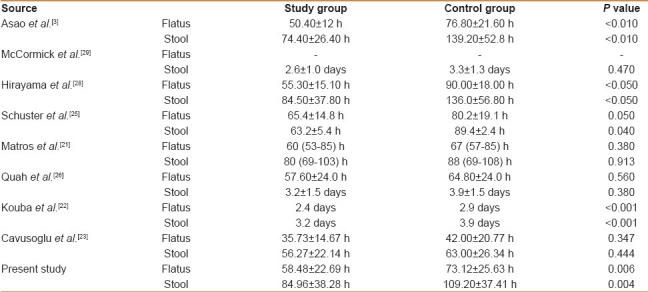
The mean time for the passage of first flatus as well as the first stool was significantly shorter in the study group (P=0.006 and P=0.004, respectively). All the previous studies,[21–23,25,28,29] majority on elective colonic anastomosis, have also observed that patients in the study group were able to pass flatus as well as stools before the control group [Table 4]. McCormick et al.[29] observed that gum chewing resulted in earlier first defecation in laparoscopic colectomy patients but not in the open colectomy patients.
Table 4.
Passage of flatus and stool
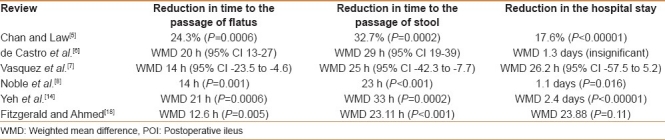
Various systematic reviews and meta-analyses have also found a significant reduction in time to first flatus as well as bowel movement in the gum chewing group [Table 5].[5–8,14,18]
Table 5.
Systematic reviews and meta-analyses on the effect of gum chewing on POI
The mean time taken to experience the feeling of hunger was significantly shorter in the study group in comparison to the control group cases (P=0.004). This parameter has been analyzed previously in only one study with similar findings, but the difference was not statistically significant.[25]
The overall postoperative complication rates did not differ significantly between the gum chewing and control groups in the present as well as previous studies.[3,21,22,25,26,30] However, a systematic review observed that overall infectious complications of any type were reduced in the gum chewing group.[8]
The duration of hospital stay was much less in previous studies in comparison to our study.[21–23,25,29] It is possibly because ours being a government institute providing free services, the patients are usually kept admitted for a longer period. However, the postoperative hospital stay was shorter in study group cases (mean 8.30±2.91 days) as compared to control group cases (mean 9.60±4.18 days). But the difference was not statistically significant (P=0.059). Various systematic reviews and meta-analyses have also found reduction in hospital stay in the gum chewing group, but it was found to be statistically significant by some[5,8] while others observed it to be not significant.[6,7,18]
CONCLUSION
In conclusion, gum chewing after relaparotomy for ileostomy closure, which was done for typhoid perforation peritonitis, has shown to significantly reduce the duration of POI as judged by the appearance of bowel sounds and passage of flatus as well as stool. The cases undergoing relaparotomy for the closure of intestinal stoma belong to a different category than the patients of elective intestinal anastomosis. The duration of POI is likely to be prolonged in such cases due to additional gut handling during adhesiolysis. Poor nutrition, dehydration, and electrolyte imbalance are likely to further aggravate the problem. Gum chewing has played a definite role in reducing POI in such cases, but further studies of bigger dimension are needed to substantiate these findings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Behm B, Stollman N. In: Practical Gastroenterology. Westhampton Beach, NY: Shugar Publishing Inc; 2002. Postoperative ileus; pp. 13–24. [Google Scholar]
- 2.Livingstone EH, Passaro EP., Jr Postoperative ileus. Dig Dis Sci. 1990;35:121–32. doi: 10.1007/BF01537233. [DOI] [PubMed] [Google Scholar]
- 3.Asao T, Kuwano H, Nakamura J, Morinaga N, Hirayama I, Ide M. Gum chewing enhances early recovery from postoperative ileus after laparoscopic colectomy. J Am Coll Surg. 2002;195:30–2. doi: 10.1016/s1072-7515(02)01179-1. [DOI] [PubMed] [Google Scholar]
- 4.Tandeter H. Hypothesis: Hexitols in chewing gum may play a role in reducing postoperative ileus. Med Hypotheses. 2009;72:39–40. doi: 10.1016/j.mehy.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 5.Chan MK, Law WL. Use of chewing gum in reducing postoperative ileus after elective colorectal resection: A systematic review. Dis Colon Rectum. 2007;50:2149–57. doi: 10.1007/s10350-007-9039-9. [DOI] [PubMed] [Google Scholar]
- 6.de Castro SM, van den Esschert JW, van Heek NT, Dalhuisen S, Koelemay MJ, Busch OR, et al. A systematic review of the efficacy of gum chewing for the amelioration of postoperative ileus. Dig Surg. 2008;25:39–45. doi: 10.1159/000117822. [DOI] [PubMed] [Google Scholar]
- 7.Vásquez W, Hernández AV, Garcia-Sabrido JL. Is gum chewing useful for ileus after elective colorectal surgery? A systematic review and meta-analysis of randomized clinical trials. J Gastrointest Surg. 2009;13:649–56. doi: 10.1007/s11605-008-0756-8. [DOI] [PubMed] [Google Scholar]
- 8.Noble EJ, Harris R, Hosie KB, Thomas S, Lewis SJ. Gum chewing reduces postoperative ileus. A systematic review and meta-analysis? Int J Surg. 2009;7:100–5. doi: 10.1016/j.ijsu.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Ogilvy AJ, Smith G. The gastrointestinal tract after anaesthesia. Eur J Anaesthesiol Suppl. 1995;10:35–42. [PubMed] [Google Scholar]
- 10.Delaney CP. Clinical perspective on postoperative ileus and the effects of opiates. Neurogastroenterol Motil. 2004;16(Suppl):61–6. doi: 10.1111/j.1743-3150.2004.00559.x. [DOI] [PubMed] [Google Scholar]
- 11.Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182(5A Suppl):3S–10S. doi: 10.1016/s0002-9610(01)00781-4. [DOI] [PubMed] [Google Scholar]
- 12.Miedema BW, Johnson JO. Methods for decreasing postoperative gut dysmotility. Lancet Oncol. 2003;4:365–72. doi: 10.1016/s1470-2045(03)01118-5. [DOI] [PubMed] [Google Scholar]
- 13.Kurz A, Sessler DI. Opioid-induced bowel dysfunction: Pathophysiology and potential new therapies. Drugs. 2003;63:649–71. doi: 10.2165/00003495-200363070-00003. [DOI] [PubMed] [Google Scholar]
- 14.Yeh YC, Klinger EV, Reddy P. Pharmacologic options to prevent postoperative ileus. Ann Pharmacother. 2009;43:1474–85. doi: 10.1345/aph.1M121. [DOI] [PubMed] [Google Scholar]
- 15.Yuan CS, Foss JF, O’Connor M, Toledano A, Roizen MF, Moss J. Methylnaltrexone prevents morphine-induced delay in oral-cecal transit time without affecting analgesia: A double-blind randomized placebo-controlled trial. Clin Pharmacol Ther. 1996;59:469–75. doi: 10.1016/S0009-9236(96)90117-4. [DOI] [PubMed] [Google Scholar]
- 16.Kalff JC, Schraut WH, Simmons RL, Bauer AJ. Surgical manipulation of the gut elicits an intestinal muscularis inflammatory response resulting in postsurgical ileus. Ann Surg. 1998;228:652–63. doi: 10.1097/00000658-199811000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basse L, Thorbol JE, Lossl K, Kehlet H. Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum. 2004;47:271–7. doi: 10.1007/s10350-003-0055-0. discussion 277-8. [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald JE, Ahmed I. Systematic review and meta-analysis of chewing-gum therapy in the reduction of postoperative paralytic ileus following gastrointestinal surgery. World J Surg. 2009;33:2557–66. doi: 10.1007/s00268-009-0104-5. [DOI] [PubMed] [Google Scholar]
- 19. Does chewing gum after elective laparoscopic colectomy surgery decrease ileus? Verified by State University of New York - Upstate Medical University, Jun 2009. First Received: March 3, 2008 Last Updated: Jun 16, 2009. Clinical Trials. Gov Identifier: NCT00632801.
- 20.Abd-El-Maeboud KH, Ibrahim MI, Shalaby DA, Fikry MF. Gum chewing stimulates early return of bowel motility after caesarean section. 2009;116:1334-9. BJOG. 2009;116:1334–9. doi: 10.1111/j.1471-0528.2009.02225.x. Epub 2009 Jun 12. [DOI] [PubMed] [Google Scholar]
- 21.Matros E, Rocha F, Zinner M, Wang J, Ashley S, Breen E, et al. Does gum chewing ameliorate postoperative ileus? Results of a prospective, randomized, placebo-controlled trial. J Am Coll Surg. 2006;202:773–8. doi: 10.1016/j.jamcollsurg.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 22.Kouba EJ, Wallen EM, Pruthi RS. Gum chewing stimulates bowel motility in patients undergoing radical cystectomy with urinary diversion. Urology. 2007;70:1053–6. doi: 10.1016/j.urology.2007.07.048. [DOI] [PubMed] [Google Scholar]
- 23.Cavuşoğlu YH, Azili MN, Karaman A, Aslan MK, Karaman I, Erdoğan D, et al. Does gum chewing reduce postoperative ileus after intestinal resection in children? A prospective randomized controlled trial. Eur J Pediatr Surg. 2009;19:171–3. doi: 10.1055/s-0029-1202776. [DOI] [PubMed] [Google Scholar]
- 24.Ahmed HN, Niaz MP, Amin MA, Khan MH, Parhar AB. Typhoid perforation still a common problem: Situation in Pakistan in comparison to other countries of low human development. J Pak Med Assoc. 2006;56:230–2. [PubMed] [Google Scholar]
- 25.Schuster R, Grewal N, Greaney GC, Waxman K. Gum chewing reduces ileus after elective open sigmoid colectomy. Arch Surg. 2006;141:174–6. doi: 10.1001/archsurg.141.2.174. [DOI] [PubMed] [Google Scholar]
- 26.Quah HM, Samad A, Neathey AJ, Hay DJ, Maw A. Does gum chewing reduce postoperative ileus following open colectomy for left-sided colon and rectal cancer? A prospective randomized controlled trial. Colorectal Dis. 2006;8:64–70. doi: 10.1111/j.1463-1318.2005.00884.x. [DOI] [PubMed] [Google Scholar]
- 27.Papaconstantinou H. Chewing gum accelerates discharge of patients from the hospital after colon resection. News from Annual Clinical Congress, American College of Surgeons 17th Oct. 2005. [Last accessed on 2011 June 28]. Available from: URL: http://www.facs.org/clincon2005/press/ prpapaconstantinou.html .
- 28.Hirayama I, Suzuki M, Ide M, Asao T, Kuwano H. Gum chewing stimulates bowel motility after surgery for colorectal cancer. Hepatogastroenterology. 2006;53:206–8. [PubMed] [Google Scholar]
- 29.McCormick JT, Garvin R, Caushai P, Simmang C, Gregorck S, Huber P, et al. The effects of gum chewing on bowel function and hospital stay after laparoscopic vs open colectomy: A multiinstitution prospective randomised trial. Am J Coll Surg. 2005;3(Suppl):66–7. [Google Scholar]
- 30.Watson H, Griffiths P, Lamparelli M, Watson M. Does chewing (gum) aid recovery after bowel resection? A randomized controlled trial (RCT) Colorectal Dis. 2008;10:6. [Google Scholar]


