INTRODUCTION
Hepatic lymphangioma is a rare benign neoplasm characterized by cystic dilatation of the lymphatic vessels in the hepatic parenchyma. In most cases, the hepatic lesion is a part of multi-organ involvement including the liver, spleen, kidneys, skeleton, gastrointestinal tract, mesentery, lungs, and somatic soft tissue.1,2 The typical imaging feature of hepatic lymphangioma is a cystic or multicystic hepatic mass with internal septations.3
In this report, we describe the imaging features of a pathologically proven case of hepatic lymphangioma with microscopic cystic component, and we demonstrate the advantage of using magnetic resonance imaging (MRI) in the diagnosis of lesions composed of multiple aggregated microcysts.
CASE
A 75-year-old woman with no significant medical history presented with abdominal pain for one week. She was tender in the left costovertebral angle and had frequent voiding symptoms without gastrointestinal problems. Routine urinary analysis showed many red blood cells and 20-29 white blood cells per high power field of microscopy indicating renal stone disease. Other laboratory tests were unremarkable. Chest computed tomography (CT) was performed for evaluation of a nodular lesion in the right lower lung field that was detected on routine chest radiography leading to the incidental discovery of a low-density lesion in the left hepatic lobe. While she was admitted to the hospital for treatment of left renal stone disease, further evaluation of the incidental low-density lesion in the left hepatic lobe was performed. Ultrasonography (US) of the upper abdomen demonstrated a 3.1 cm-sized mixed-echoic nodular lesion in segment IV with a hyperechoic rim (Fig. 1A). The right portion of the lesion was anechoic (solid arrow) while the left was hyperechoic. An abdominal CT scan revealed a lobulated mass with a cystic component in the right portion of the mass and delayed enhancement in the left which was thought indicate solid component (Fig. 1B). Magnetic resonance imaging (MRI) of the liver was performed for further evaluation of the mass. The right side of the mass was seen as low signal intensity while the left side was enhanced on gadolinium-enhanced T1-weighted image (Fig. 2A), thus matching to the CT features. However, T2-weighted images showed bright high signal intensity throughout the whole lesion (Fig. 2B, C) suggesting that the lesion was composed of aggregated cysts rather than solid tissue. For confirmative diagnosis, the patient underwent gun biopsy using US-guidance, the results of which demonstrated microscopic findings of a sponge-like lesion composed of microscopic cysts lined by attenuated cells resembling those in normal lymphatic ducts (Fig. 3A). In addition, the lining cells showed staining for the endothelium marker, CD34 (Fig. 3B). The final histopathologic diagnosis for the specimen was hepatic lymphangioma.
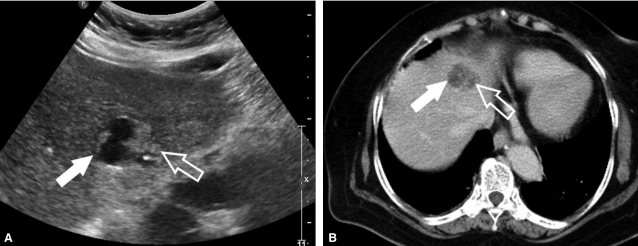
Figure 1.
A mixed echoic hepatic nodule in the segment IV is seen on ultrasonography. The right side of the lesion is anechoic (solid arrow), and the left is hyperechoic (open arrow) (A). On the post enhanced CT scan shows the right side of the lesions is a relatively well-circumscribed low attenuated portion (solid arrow), but the other side is enhanced heterogeneously (open arrow). This feature is matched with ultrasonographic findings (B).
Figure 2.
MR scan shows that its features on the 3D-spoiled gradient echo T1-weighted MR scan after gadolinium contrast injection are very similar to the that of CT scan (A), and fat-suppressed T2-weighted MR scan shows a bright high signal intensity in the whole mass (solid and open arrows), differentiated from the US and CT features. This finding suggests that this hepatic mass may be composed of a fluid-filled structure, cyst (B). Coronal T2-weighted MR scan demonstrates the aggregated cystic component on the left side of the mass well (open arrow) (C).
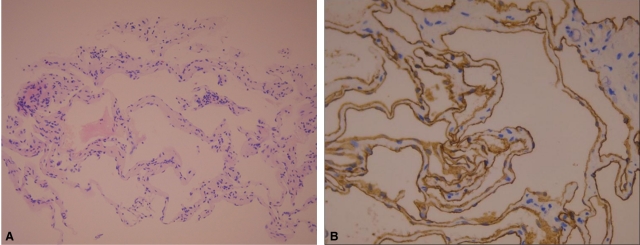
Figure 3.
Pathologically, the sponge-like lesion is composed of microscopic cysts lined by attenuated endothelium, resembling that in normal lymphatics (H-E stain, ×20) (A). Immunohistochemical staining with CD34 antibody, reveals the lining endothelium is well demonstrated on the microscopy (CD34 stain, ×400) (B).
DISCUSSION
Hepatic lymphangioma is a rare benign neoplasm that may be solitary2 or associated with multiple liver lesions, and is characterized by cystic dilatation of lymphatic vessels in the hepatic parenchyma. Lymphangioma solely involving the liver is extremely rare,1 and in most cases, the hepatic lesion is a part of multi-organ involvement including the liver, spleen, kidneys, skeleton, gastrointestinal tract, mesentery, lungs, and somatic soft tissue.3,4 The etiology of hepatic lymphangioma is poorly understood. It is generally believed to be a developmental abnormality associated with failure of the developing lymphatic tissues to establish normal communication with regional lymphatic drainage, resulting in the dilatation of abnormal channels.5
On US, CT, and MRI, hepatic lymphangioma may appear as a simple or multiloculated cystic mass with internal septations, but it is difficult to differentiate hepatic lymphangioma from other cystic disease. Because most lymphangiomas are multicystic lobulated lesions, they may be confused with other lesions including septated bile duct cyst, biliary cystadenoma and cystadenocarcinoma, cystic metastasis, or echinococcal cysts.3,6 In particular, biliary cystadenoma and cystadenocarcinoma usually occurs in middle-aged women and demonstrates features such as mural nodules, fibrous capsule, and calcifications. Cystic hepatic metastasis may be seen with mucinous adenocarcinoma of stomach, colorectum or ovary, and CT mostly shows a cystic mass with peripheral solid lesion.7 In the case of an echinococcal cyst, the presence of daughter cysts and a postural dependency of internal vesicles within the mother cyst are the typical imaging features. However, because this disease is extremely rare in Northeast Asia, a positive serologic test and history of travel to an endemic area are necessary for its diagnosis.8,9
MRI of lymphangioma usually shows a multiloculated heterogeneous mass with low signal intensity on T1-weighted images, and high signal intensity on T2-wei ghted images because of its content.10 However, the microcystic component of lymphangioma be mistaken for a solid lesion due to its enhancement after intravenous injection of contrast. MRI is very helpful for determining such characteristic features of the lesion because T2-weighted and heavily T2-weighted imaging are sensitive to the presence of water. Solid serous cystadenoma of the pancreas is another example where MRI can be very useful.11 Microscopically, this solid variant is composed of multiple microcysts containing serous fluid. Thus, MRI, especially MR cholangiopancreatography is useful in differentiating lymphangioma from a true solid neoplasm. Our case also consisted of numerous microcysts, and MRI enabled a correct diagnosis.
In conclusion, we present a case of solitary hepatic lymphangioma that could have been confused with a partially solid neoplasm. MRI facilitated the correct diagnosis of hepatic lymphangioma with multiple aggregated cysts.
SUMMARY
A case of primary hepatic lymphangioma with a microcystic component was incidentally found in a 75-year-old woman. Although ultrasonography (US) and computed tomography (CT) showed a mixed lesion including cystic and solid components, magnetic resonance imaging (MRI) demonstrated the morphologic characteristics of the lesion better than other modalities.
Abbreviations
- CT
computed tomographya
- MRI
magnetic resonance imaging
- US
ultrasonography
References
- 1.Koh CC, Sheu JC. Hepatic lymphangioma--a case report. Pediatr Surg Int. 2000;16:515–516. doi: 10.1007/s003839900327. [DOI] [PubMed] [Google Scholar]
- 2.Stavropoulos M, Vagianos C, Scopa CD, Dragotis C, Androulakis J. Solitary hepatic lymphangioma. A rare benign tumour: a case report. HPB Surg. 1994;8:33–36. doi: 10.1155/1994/63638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan SC, Huang SF, Lee WC, Wan YL. Solitary hepatic lymphangioma--a case report. Int J Clin Pract Suppl. 2005;(147):100–102. doi: 10.1111/j.1742-1241.2004.00276.x. [DOI] [PubMed] [Google Scholar]
- 4.Lugo-Olivieri CH, Taylor GA. CT differentiation of large abdominal lymphangioma from ascites. Pediatr Radiol. 1993;23:129–130. doi: 10.1007/BF02012405. [DOI] [PubMed] [Google Scholar]
- 5.Ko SF, Ng SH, Shieh CS, Lin JW, Huang CC, Lee TY. Mesenteric cystic lymphangioma with myxoid degeneration: unusual CT and MR manifestations. Pediatr Radiol. 1995;25:525–527. doi: 10.1007/BF02015784. [DOI] [PubMed] [Google Scholar]
- 6.Levy AD, Cantisani V, Miettinen M. Abdominal lymphangiomas: imaging features with pathologic correlation. AJR Am J Roentgenol. 2004;182:1485–1491. doi: 10.2214/ajr.182.6.1821485. [DOI] [PubMed] [Google Scholar]
- 7.Mortelé KJ, Ros PR. Cystic focal liver lesions in the adult: differential CT and MR imaging features. Radiographics. 2001;21:895–910. doi: 10.1148/radiographics.21.4.g01jl16895. [DOI] [PubMed] [Google Scholar]
- 8.Haddad MC, Al-Awar G, Huwaijah SH, Al-Kutoubi AO. Echinococcal cysts of the liver: a retrospective analysis of clinico-radiological findings and different therapeutic modalities. Clin Imaging. 2001;25:403–408. doi: 10.1016/s0899-7071(01)00331-x. [DOI] [PubMed] [Google Scholar]
- 9.Hadidi A. Sonography of hepatic echinococcal cysts. Gastrointest Radiol. 1982;7:349–354. doi: 10.1007/BF01887669. [DOI] [PubMed] [Google Scholar]
- 10.Siegel MJ, Glazer HS, St Amour TE, Rosenthal DD. Lymphangiomas in children: MR imaging. Radiology. 1989;170:467–470. doi: 10.1148/radiology.170.2.2911671. [DOI] [PubMed] [Google Scholar]
- 11.Gabata T, Terayama N, Yamashiro M, Takamatsu S, Yoshida K, Matsui O, et al. Solid serous cystadenoma of the pancreas: MR imaging with pathologic correlation. Abdom Imaging. 2005;30:605–609. doi: 10.1007/s00261-004-0286-0. [DOI] [PubMed] [Google Scholar]