Abstract
Background:
In 2007, our healthcare system established a clinical fellowship program in pathology informatics. In 2011, the program benchmarked its structure and operations against a 2009 white paper “Program requirements for fellowship education in the subspecialty of clinical informatics”, endorsed by the Board of the American Medical Informatics Association (AMIA) that described a proposal for a general clinical informatics fellowship program.
Methods:
A group of program faculty members and fellows compared each of the proposed requirements in the white paper with the fellowship program's written charter and operations. The majority of white paper proposals aligned closely with the rules and activities in our program and comparison was straightforward. In some proposals, however, differences in terminology, approach, and philosophy made comparison less direct, and in those cases, the thinking of the group was recorded. After the initial evaluation, the remainder of the faculty reviewed the results and any disagreements were resolved.
Results:
The most important finding of the study was how closely the white paper proposals for a general clinical informatics fellowship program aligned with the reality of our existing pathology informatics fellowship. The program charter and operations of the program were judged to be concordant with the great majority of specific white paper proposals. However, there were some areas of discrepancy and the reasons for the discrepancies are discussed in the manuscript.
Conclusions:
After the comparison, we conclude that the existing pathology informatics fellowship could easily meet all substantive proposals put forth in the 2009 clinical informatics program requirements white paper. There was also agreement on a number of philosophical issues, such as the advantages of multiple fellows, the need for core knowledge and skill sets, and the need to maintain clinical skills during informatics training. However, there were other issues, such as a requirement for a 2-year fellowship and for informatics fellowships to be done after primary board certification, that pathology should consider carefully as it moves toward a subspecialty status and board certification.
Keywords: Pathology informatics fellowship, clinical informatics, clinical informatics fellowship, pathology informatics, pathology informatics teaching, clinical informatics teaching
INTRODUCTION
Pathology and Informatics
Pathology is a medical specialty dedicated to the analysis of tissue and fluid specimens. This analysis is done to answer important clinical questions in specific clinical contexts. With a few important exceptions, the main product of a pathology practice – what it provides to patients, physicians, and health systems – is accurate, reliable, and actionable information. Information generated by pathology is used by every clinician in every subspecialty and by virtually every person (as a patient) at multiple times in his or her life. It has been estimated that over a wide range of practice environments, over half of the unique data elements (accessions) in the electronic medical record are from pathology.[1–3]
The relationship between pathology, information, information systems, and processes that create or use information goes back to decades. A detailed history is beyond the scope of this manuscript, but several events are illustrative. Laboratory Information Systems (LISs) were amongst the earliest clinical computer systems in hospitals;[4,5] Systemic Nomenclature of Pathology (SNOP), developed in 1965 by the College of American Pathology, was one of the first medical coding systems, and its progeny Systemic Nomenclature of Medicine (SNOMED) is arguably the most sophisticated.[6] The clinical laboratory is one of the most automated medical facilities;[7] automated cervical–vaginal cytology systems facilitate cancer screening on millions of patients each year and high-resolution digital slides are the largest medical images.[8] By the 1980s, the importance of clinical information management in pathology led to calls, formalized by Dr. Bruce Friedman in a 1990 commentary in the American Journal of Clinical Pathology entitled “Informatics as a Separate Section within a Department of Pathology,”[9] for the creation of pathology informatics as a subspecialty. By the mid 1990s, multiple departments had established independent sections of pathology informatics.
Since 1983, there have been annual national meetings in pathology informatics, starting with the “Automated Information Management for the Clinical Laboratory” (AIMCL). In 1996, a second major pathology informatics conference “Anatomic Pathology Informatics, Imaging and the Internet” (APIII) was created and The Association for Pathology Informatics (API) was formed in 2000. A formal proposal of specific informatics learning objectives and skill sets for pathology residents was published in 2003,[10] and the Journal of Pathology Informatics was started in 2010.
Subspecialty Training in Pathology Informatics
To our knowledge, Dr. Michael Becich established the first formal clinical fellowship program in pathology informatics at the University of Pittsburgh in 1995. As of December 26, 2011, the API lists five programs (Pittsburgh, Partners, Henry Ford, Michigan, and Hopkins) on its web site. To date, these programs, in aggregate, have graduated less than 20 pathologists.
Our Pathology Informatics Clinical Fellowship
Our Pathology Informatics Fellowship Program has two arms: a Pathology Informatics Clinical Fellowship (which is limited to pathologists and will be the focus of this paper) and a Pathology Informatics Research Fellowship (which is a classic mentored research fellowship open to all MDs and PhDs) in which the fellow works under a single mentor in a specific research facility, but also attends the pathology informatics core didactic course.
The Pathology Informatics Fellowship originated in 2007 at one of our hospitals. It is now an integrated (multi-site) training program within our healthcare system and operates in two large academic medical centers and a large community hospital, which has a private practice pathology model and a strong pathology outreach program. Informatics fellows rotate across the individual sites with the core didactic sessions centralized at one of the academic centers.
Since early 2010, the fellowship has been overseen by a central Educational Committee (EC), which oversees all GME activity in our Healthcare System. This oversight includes a charter, known as the “Program Description and Written Curriculum,” that defines the structure and operations of the program and is signed by the program director and the individual pathology departments and approved by the EC. Acceptance of the charter as well as other documentation and application forms by the EC represents the healthcare system's Designated Institutional Official (DIO) approval of the program.
The program graduated its first class of fellows in 2009. In 2010–2011, the program had two clinical fellows (and a single research fellow), and beginning in 2011 the program has five clinical fellows and two research fellows. Approximately half of the fellows have been recruited from pathology residencies within our healthcare system. To date, all graduates have found informatics positions in large academic medical centers.
The program has 11 active faculty members (and several more associate faculty) located across the three sites representing multiple subspecialties of pathology. It is run by an executive committee made up of the pathology informatics directors of the three pathology departments and is chaired by a program director who is ultimately responsible for the operation of the program and the quality of education at all sites. There is also a steering committee that includes the chairs and educational directors of the pathology departments involved with the fellowship program.
American Medical Informatics Association Efforts in Defining the Medical Subspecialty of Clinical Informatics
In March 2007, the American Medical informatics Association (AMIA) was awarded a grant from the Robert Wood Johnson Foundation to begin development of an Accreditation Council for Graduate Medical Education (AGCME) accredited subspecialty in clinical informatics for clinical professionals, beginning with Medicine. Specifically, the grant allowed AMIA to develop two documents (white papers) needed for the American Board of Medical Specialties to begin formal consideration of a medical subspecialty of clinical informatics and associated fellowship programs.[11] Two AMIA working groups developed the documents: “Program Requirements for Fellowship Education in the Subspecialty of Clinical Informatics”[12] and “Core Content for the Subspecialty of Clinical Informatics,”[13] both of which were published in the Journal of the American Medical Informatics Association in the spring of 2009.
Benchmarking our Program Against the AMIA White Papers
In 2011, our program decided to benchmark its structure and operations against one of the 2009 AMIA papers “Program requirements for fellowship education in the subspecialty of clinical informatics” by Safran et al.[12] This paper is referred to extensively below as the “white paper” or the “AMIA white paper.” There were two main reasons for the benchmarking of our program: 1) we expect a routine review of the program by our institution's review board in 2012 and 2) we wanted to understand the strengths and weakness of our program given the likelihood, in the relatively near term, of a general clinical informatics subspecialty of the type envisioned in the AMIA papers above.
METHODS
The analysis in this manuscript derives directly from our benchmarking efforts above. This has significant implications for the scope and direction of analysis. Our goal was to look at each proposal in the white paper and determine if it was concordant or discrepant with the charter and existing operations of the fellowship. The analysis is therefore silent on any structures, operations, or areas in the fellowship, which are not related to a proposal in the white paper (there were not many). This decision was made in an attempt to limit the scope and bias in the analysis.
After a short section defining clinical informatics, the white paper makes specific recommendations for clinical informatics fellowship programs in seven major sections:
Institutions
Program personnel and resources
Fellow appointment
Educational program
Evaluation
Learning and working environment
Experimentation and innovation.
A faculty committee (including the director and three fellows) from our program went through the white paper section by section, attempted to list the proposals, determined if each was a proposed requirement (a program must…) or a suggestion (a program should…), and compared them to our fellowship program's current structure and operations. There were two main ways of determining concordance and discrepancy:
If a white paper recommendation was directly comparable to a statement in the fellowship program's charter (the “Program Description and Written Curriculum”) or general healthcare system education council or department requirement, then concordance or discrepancy was determined directly.
If a white paper recommendation was not directly comparable to a statement in the charter (either if the charter was silent on the issue or if the statement in the charter and the recommendation in the white paper were not easily compared), this was noted and the committee determined whether or not the fellowship program's current implementation was consistent with the white paper recommendation. The committee's assessment rationale was incorporated in the manuscript.
After the committee's comparisons with the white paper were recorded, the document was sent to all faculty members and all concerns raised were reviewed and resolved.
The results below parallel the white paper section by section. For each section of the white paper, the results provide the following:
Summarize the main proposals of the white paper
When possible, provide in a tabular form concordance and discordance between the white paper proposals and our fellowship program, and how each decision was made (direct examination of the charter or, if the charter was silent or unclear, consideration of the fellowship program's current structures and operations).
When appropriate, provide some of the background behind those decisions.
It is strongly recommended that the reader download a copy of the AMIA white paper[12] from JAMIA and have it available while reading this paper.
RESULTS
Definitions
The AMIA white paper defines the clinical informatics subspecialty. Summarizing from the white paper:
Clinical informaticians assess information needs of health care professions and patients; characterize, evaluate and refine clinical processes; and develop, implement and refine clinical decision support systems and other clinical information systems.
Our program defines pathology informatics as “the study and management of information, information systems, and processes in pathology.”
While the definitions are not exactly the same, the basic principles are consistent – both pathology informatics and clinical informatics study clinical information, information systems, and processes (including decision support processes) that create, manage, or consume information in clinical practice. Of particular interest is the importance both groups give to processes, not just information and information systems. When we compare pathology informatics and clinical informatics in this analysis, we are comparing apples to apples.
Section I: Institutions
Summary of the AMIA White Paper Proposals
The white paper discusses the proposed clinical informatics fellowship program in the context of a sponsoring institution, a primary site, and optional participating sites. Summarizing the white paper:
Sponsoring Institution (Section I.A.): The sponsoring institution must be ultimately responsible for the fellowship program (including fellow assignments at the primary and participating sites). The institution must make a written commitment of support, establish the fellowship within an administrative unit committed to education and patient care, insure that there is sufficient funding for the program, and the program director has sufficient protected time and financial support for his or her educational and administrative responsibilities to the program, including providing at least 20% of the director's salary and demonstrating the financial capacity to support two fellowship positions at all times.
Primary Training Site (Section I.B.): The primary training site is the health care facility that provides the required training resources. It should be site of the program director's main activity and the place where fellows spend the majority of their informatics training time.
Participating Sites (Section I.C.): Participating sites are not required, but if used the program must ensure a unified educational experience, and the participating sites must offer a significant educational environment that complements the experience at the primary site. There must be a program letter of agreement between the program and each site that states the policies and procedures of the fellowship, identifies the faculty and their responsibilities for teaching, supervision and evaluation of the fellows and the duration and content of the educational experience.
The Pathology Informatics Clinical Fellowship Programs
Table 1 compares the major white paper proposals with the program's implementation. The structure of the fellowship program is discussed in the section “Introduction” and appears to meet all institutional requirements in the white paper.
Table 1.
Relationship between the institution and the program
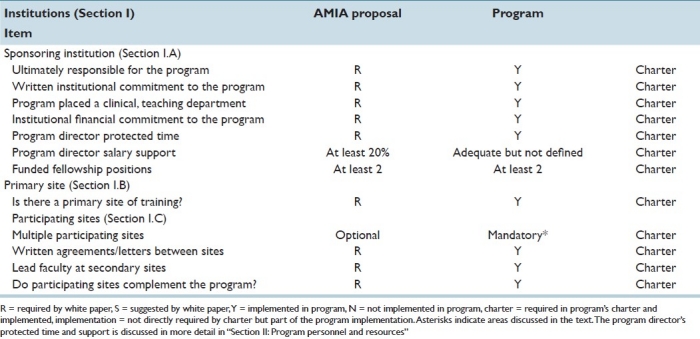
Multiple participating sites are optional in the AMIA proposal, but are required by our charter (we are, by charter, a multi-site program). Our experience is that multiple participating institutions (sites) are fundamentally important to the educational strength of a program. A fellowship program with multiple, diverse sites is able to expose fellows to much wider range of systems, approaches, procedures, and workflows than a program based at a single site. Furthermore, there is a set of informatics operations (such as installing or upgrading a major LIS) that do not happen often at a single site but in which a fellow should be involved with during his or her fellowship, and a program with multiple participating sites is more likely to provide such experiences on a more consistent basis. Finally, informatics is increasingly thought of and architected on multi-facility health system and health network level.
Section II: Program Personnel and Resources
The white paper discusses the program personnel and resources in five sub-sections: Program director, faculty, other program personnel, resources, and medical information access.
Program Director
Summary of the AMIA White Paper Proposals
Program Director (Section II.A): There must be a single program director with the authority and accountability for the operation of the program. The term of the program director should be long enough to maintain continuity of leadership and program continuity. The sponsoring institution's Graduate Medical Education Committee must approve a change in program director and submit the change to the ACGME via the Accreditation Data System (ADS). The director should have specialty expertise and educational and administrative experience acceptable to the review committee, which may include certification in clinical informatics, appropriate medical staff appointments or professional qualifications acceptable to the review committee and five years of experience in clinical informatics education, research and practice.
The program director must oversee and ensure the quality of education in the program, approve local directors at participating sites and faculty as appropriate. The program director is responsible for faculty and fellow evaluation. Finally the program director must ensure compliance with the Review Committee, sponsoring institution and ACGME rules, and obtain Designated Institutional Officer (DIO) review and sign off on all program forms and correspondence submitted to the ACGME involving program citation and/or request for significant changes to the program.
Pathology Informatics Clinical Fellowship Program
Table 2 compares the major white paper proposals with the program's implementation. There is one discrepancy the between the program and a required proposal.
Table 2.
Program Director
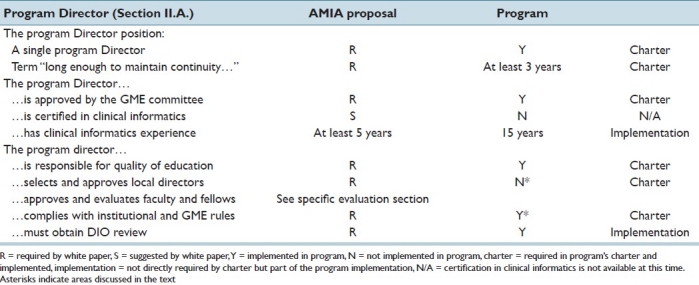
By charter, the fellowship program director has authority and accountability over the operation of the program; however, unlike the white paper proposal, the director operates as chairman of an executive board made up of the pathology informatics directors of the three pathology programs in the fellowship, who are chosen by the chairman of each pathology department.
The white paper lists a large number of specific responsibilities (see the paper for details); all are consistent with the program charter and are bundled on the “complies with institutional and GME rules” line in Table 2.
Faculty
Summary of the AMIA White Paper Proposals
Faculty (Section II.B): The white paper requires that there be a sufficient number of faculty with documented qualifications to instruct and supervise all fellows at each participating site and recommends at least three faculty (with a total teaching commitment of one full time equivalent) at the primary site. Faculty members should possess appropriate institutional appointments and with informatics qualifications acceptable to the review committee. The faculty should establish and maintain an environment of inquiry and scholarship with an active research component. At least some of the faculty should demonstrate scholarship through peer reviewed funding, publication of original research or review articles in peer-reviewed publications, present at local, regional or national professional and scientific society meetings, and encourage and support fellows in scholarly activities.
Pathology Informatics Clinical Fellowship Program
Table 3 compares the major white paper proposals with the program's implementation.
Table 3.
Program faculty
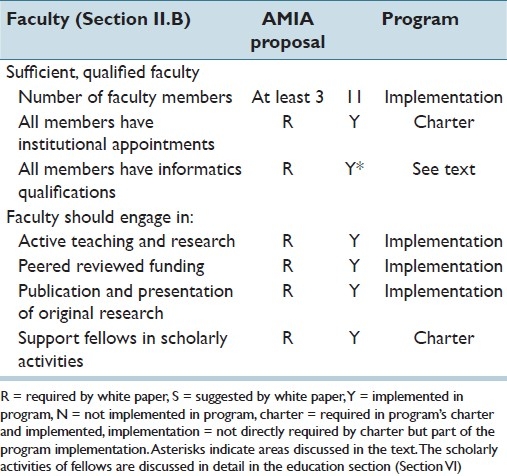
There is no standard certification in pathology informatics, so defining those who are pathology informatics faculty is not straightforward. The program defines an informatics faculty member as a pathology department faculty member who, in the opinion of the fellowship director: 1) runs an independent research laboratory in an area of pathology informatics or 2) oversees a key informatics resource or operation (such as an LIS), and 3) has published (or was an invited speaker at a national meeting) on an area of pathology informatics in the previous year. In addition to the criteria above, the faculty member must self-identify as an informatician and be willing to commit time and resources to the fellowship program and the teaching of fellows. With the exception of the director, all faculty members also have active appointments in another (non-informatics) pathology subspecialty or lead independent research facilities.
Other Program Personnel
Summary of the AMIA White Paper Proposals
Other Program Personnel (Section II.C): The institution and the program must also ensure the availability of all necessary professional, technical, and clerical personnel for the effective administration of the program.
Pathology Informatics Clinical Fellowship Program
The Program is administered by the MGH Department of Pathology through the department's fellowship office. It has the same administrative and recruiting resources as the other pathology fellowships.
Resources
Summary of the AMIA White Paper Proposal
Resources (Section II.D): The white paper proposes that the institution and the program jointly ensure the availability of adequate resources for fellow education, as defined in the specialty requirements. There must be space and equipment for the program, including meeting rooms, classrooms, examination rooms, computers, internet access, visual and educational aids, and work/study space. Furthermore, the primary training site must operate a robust clinical information system that 1) collects, stores, retrieves and manages health and wellness data and information, 2) offers clinical decision support, 3) supports ambulatory, inpatient and remote care settings and, 4) administrative support and technology.
Pathology Informatics Clinical Fellowship Program
Table 4 compares the major white paper proposals with the program's implementation.
Table 4.
Program resources
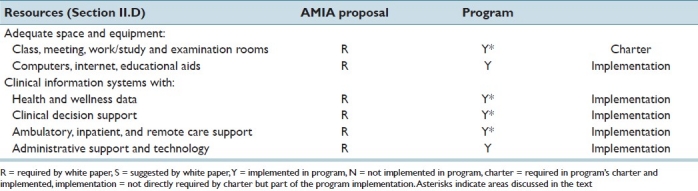
The proposed requirements do not include many of the resources one would expect in a pathology informatics fellowship. There is no mention of clinical laboratories, gross rooms, biorepositories, LISs, etc.; however, there is also no mention of operating rooms, reading rooms, picture archival and communication systems, peri-operative rooms, and other resources that would be expected in informatics programs in other fields such as surgery, radiology, anesthesiology. We consider this a result of the working group focusing on a more generic clinical informatics program.
That said, we find that our fellowship, and probably every pathology informatics program, supports all of the specific requirements in the proposal. Our fellows have access to and work extensively with the LIS and the major upstream and downstream clinical information systems; the laboratory and its systems (independently and in conjunction with the other clinical systems) support patient health and wellness,[14] ambulatory[15] and remote care (e.g. point of care testing, telepathology and outreach pathology, and clinical decision support).[16] There are even patient examination rooms (e.g. in the blood centers).
Medical Information Access
Summary of the AMIA White Paper Proposals
Medical Information Access (Section II.E): Fellows must have ready access to specialty-specific and other appropriate reference material in print or electronic format. Electronic medical literature databases with search capabilities should be available.
Pathology Informatics Clinical Fellowship Program
Fellows in the program have access to all appropriate clinical systems in the healthcare system, including all pathology systems. This includes access to all documentation, specifications, training, and standard operating procedure documents. Electronic medical literature databases with search capabilities are available.
Section III: Fellows and Fellow Appointment
This section discusses the eligibility and number of fellows, the transfer of fellows, and the appointment of fellows and other students.
Summary of the AMIA White Paper Proposals
Fellow Eligibility Criteria and Number of Fellows (Sections III.A &III.B): The program director must comply with the criteria for fellow eligibility as specified in the Institutional Requirements. Fellows must have completed a core-training program accredited by ACGME. The program's educational resources must be adequate to support the number of fellows.
Fellow Transfer (Section III.C): When a fellow transfers to or from the [clinical informatics] program, the program director must obtain or provide written or electronic verification of educational experiences and a summative competency-based performance evaluation of the transferring fellow.
Appointment of Fellows and Other Students (Section III.D): The program director must assure that the presence of other learners (residents, PhD candidates, nursing students, etc.) does not interfere with the appointed fellows’ education.
Partners Pathology Informatics Clinical Fellowship Program
Table 5 compares the major white paper proposals with the program's implementation. The discrepancy about whether candidates must finish their “core training program accredited by ACGME” before joining a clinical informatics fellowship is an important one.
Table 5.
Fellows and fellow appointment
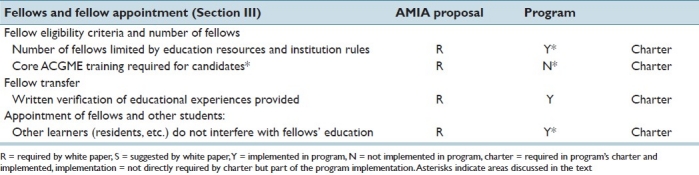
Our experience has convinced us that the concurrent appointment of multiple fellows (and the presence of rotating residents, PhD candidates, etc.) does not interfere with fellow training and in fact is very positive for both the fellows and the program itself. The maximum number of fellows a program can support is a function of the number of participating sites, interested faculty, systems, and ongoing projects. Even within a single site, the large number of information systems used by pathology and the wide diversity of pathology subspecialties and operations (AP, CP, Molecular, Imaging, etc.) means that a program with enough faculty can support a large number of fellows with very little overlap.
The AMIA white paper proposes that all clinical informatics fellows “must have completed a core training program accredited by ACGME.” While we fully understand and support the value of core clinical training for the practice of clinical informatics, a requirement that candidates complete a core ACGME program prior to matriculation in a clinical informatics program is not consistent with the way that pathology programs have been using existing American Board of Pathology and ACGME rules (especially the specialty year) to train candidates in pathology informatics (and other pathology subspecialties).
Our Pathology Informatics Clinical Fellowship Program will only accept board eligible pathologists or pathology residents taking time away from their pathology residency with the intention of finishing their residency after the fellowship. (Our research fellowship program is open to all MDs and PhDs.) These issues are considered further in the section “Discussion.”
Section IV: Educational Program
The educational program proposal is described under six main headings: Curriculum, fellows’ scholarly activities, didactics, rotations, program outcomes, and program duration. They will be discussed one at a time.
Curriculum
Summary of the AMIA White Paper Proposals
Curriculum (Section IV.A): The curriculum section discusses overall goals and objectives of a proposed clinical informatics fellowship program. Overall educational goals for the program must be written and distributed to fellows and faculty annually; and competency based goals for each assignment [rotation] should be distributed to fellows and faculty annually and should be reviewed by the fellow at the beginning of each rotation or major learning experience. The goals and objectives should include the educational purpose, teaching methods, clinical settings, information systems, educational resources and the methods for evaluation of the fellows’ competence. The goals and objectives should define the level of supervision of the fellows by faculty and should be reviewed and revised at least every three years.
The curriculum should also include regularly scheduled didactic sessions, delineation of fellow responsibilities, progressive responsibilities and supervision of fellows along the continuum of the program. Finally, the curriculum must integrate the ACGME competencies: Patient Care, Medical Knowledge, Interpersonal and Communication Skills, Professionalism and Systems-based Practice.
Pathology Informatics Clinical Fellowship Program
Table 6 compares the major white paper proposals with the program's implementation. There are no significant discrepancies. However, it is worth discussing the educational structure of the fellowship in preparation for the subsequent several sections.
Table 6.
General curriculum
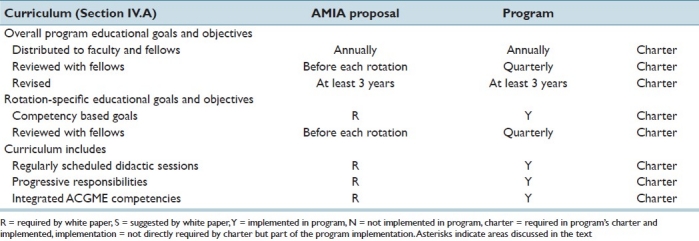
There are four educational components of the Pathology Fellowship Program:
Research rotations in which a fellow does research under the supervision of faculty member, usually in the faculty member's laboratory. This is discussed in the section “Scholarly activities.”
Didactics, which are discussed in the section “Didactic session.”
Operational rotations, in which the fellow works with informatics faculty members and IT/IS teams on clinical information systems, workflows, and real world informatics initiatives. Operational rotations can be short, largely experiential activities, but are usually long-term, multi-disciplinary continuity experiences that include multiple projects. Fellow responsibilities and expectations are commensurate with experience.
Clinical concentrations: Allow fellows to attend diagnostic conferences, tumor boards, rounds, sign-out and other clinical activities in an area of diagnostic pathology or laboratory medicine of interest to the fellow. Operational rotations and clinical concentrations are discussed in the section “Rotations, continuity experiences, major projects, and clinical opportunities.”
Generally (but not always) a fellow is concurrently assigned to all of the educational components, with a typical time distribution of research rotations (30%), didactics (15%), operational rotations (40%), clinical concentration (10%), and meetings and administration (5%). Individual educational activities are elective with two exceptions: The core pathology informatics didactic course (discussed below) and a 3-week rotation at our community hospital site to experience the informatics challenges of a private group running a large outreach practice.
At the beginning of the fellowship (and, increasingly, even before the fellowship begins), the fellow and program director discuss these goals and agree on a unique set of rotations, projects, courses, and clinical concentrations that are both consistent with the fellow's personal objectives and incorporate a common, core set of knowledge and skills expected of all pathology informaticians. This plan is reviewed on a regular basis and in most cases is modified throughout the fellowship as the fellow's understanding and interest change. Each educational activity is evaluated against the plan through the evaluation structure described in the separate evaluation section below.
Scholarly Activities
Summary of the AMIA White Paper Proposals
Fellows’ Scholarly Activities (Section IV.B): The AMIA White Paper proposes that a fellowship curriculum must advance fellows’ knowledge of the basic principles of research, including how such research is conducted, evaluated, explained to patients, and applied to patient care. Fellows should participate in scholarly activity and demonstrate evidence of research productivity through publication in 1) peer-reviewed journals or 2) abstracts, posters or presentations at scientific meetings, and the sponsoring institution and program should allocate adequate educational resources to facilitate fellow involvement in scholarly activities.
Pathology Informatics Clinical Fellowship Program
Table 7 compares the major white paper proposals with the program's implementation.
Table 7.
Fellows’ scholarly activities
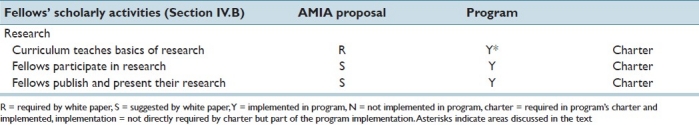
Fellows spend approximately 25–35% of their time in one or more research rotations. During these rotations, they are involved in all aspects of a mentor's laboratory including meetings and journal clubs, present their work at national meetings, and publish their research in peer-reviewed journals.
Depending on their experience, interests, and goals, fellows can attend formal courses in clinical research basics given by the healthcare system or university. These courses include topics such as IRB issues, clinical research management, grant writing, scientific writing, data analysis, statistics, and the use specific research and publication tools.
Didactics
Summary of the AMIA White Paper Proposals
Didactics (Section IV.C): The white paper proposes that formal didactics be a core part of a clinical informatics fellowship. Specifically, the program must have a plan for ensuring that fellows master the major topics of clinical informatics as outlined in the clinical informatics core content document within a two year period. [The clinical core content document is a second white paper produced for the AMIA board. Written by Gardner et al, it was published in Journal of the American Medical Informatics Association in 2009]. Classes and conferences should be scheduled and conducted on a regular basis, attended by faculty and fellows, and may include seminars, literature reviews, research conferences and core curriculum classes, and fellows must participate in planning and conducting conferences.
Pathology Informatics Clinical Fellowship Program
Table 8 compares the major white paper proposals with the program's implementation.
Table 8.
Didactics
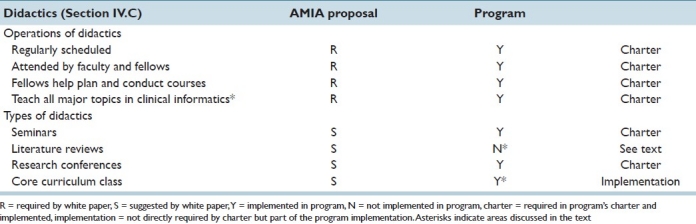
There are five broad types of didactic informatics training in the program:
Elective courses (e.g. university or health system courses such as the research courses discussed in fellows’ scholarly activities, Section IV.B above)
Research conferences and lab meetings (associated with the research rotations)
Seminars
The core pathology informatics didactic (discussed below)
National meetings (discussed below)
There are no fellowship-wide literature review sessions; however, literature review is usually an aspect of most research rotations.
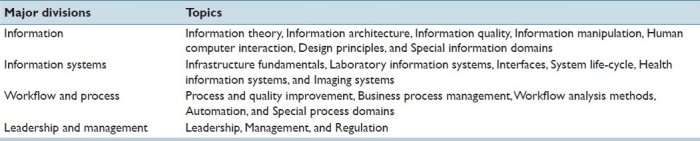
A core didactic course in pathology informatics did not exist when the program began. It was developed in 2009 (and implemented in 2010) in response to the need (identified through fellow evaluations) for a core knowledge base for fellows regardless of informatics specialty interest. The core course is mandatory for all clinical and research fellows in pathology informatics, involves 100 hours of class time (usually taken over 2 years), is taught by the program director, and is based on reading assignments in textbooks and articles. The general areas covered are listed in Table 9 and the detailed content has been submitted for publication. Approximately 70% of the course involves general or medical clinical informatics topics listed in the curriculum proposed by Gardner et al.[13] (e.g. interoperability, system design, process management, financial management, etc.) and the remainder involves more pathology-centric informatics issues (e.g. LISs, microscopic and whole-slide imaging, molecular/genomics, etc.).
Table 9.
Major divisions and topics covered in the core didactic course
The core didactic has become the anchor of the fellowship program. While our fellows have different interests and move between different sites, research labs, and operational projects, the course brings fellows together in a single activity, at the same time and place every week. It also helps to define the scope of pathology informatics in a way that multiple, independent rotations and courses cannot. The need for a core set of knowledge and competencies in clinical informatics is a recurring theme in the white paper and is the one that we have found, independently, to be valuable in our own environment.
National meetings are important to the fellowship program; they bring experts in pathology informatics to a single place, allow fellows to present their work to others and, perhaps most importantly, allow fellows to experience points of views different from those of their own faculty. The fellowship makes the annual Pathology Informatics conference (http://www.pathinformatics.pitt.edu/) a required part of didactic environment. All fellows must attend and present their scholarly and operational work.
The goal of the core is to expose fellows to the major areas of pathology informatics. The core didactic is supplemented by specialty courses and rotations depending on the goals and interests of the individual fellow.
Rotations, Continuity Experiences, Major Projects, and Clinical Opportunities
Summary of the AMIA White Paper Proposals
Rotations, Continuity Experiences, Major Projects and Clinical Opportunities (Section IV.D): The white paper defines rotations as experiential assignments, of finite duration, that are designed to provide fellows with exposure to different types of clinical and health information systems in a range of settings that include inpatient, ambulatory and remote applications. Rotations should constitute a minimum of 15% of a fellow's time over 24 months of training. Fellows must have clearly defined, written descriptions of responsibilities and a reporting structure for all rotations, continuity experiences and major projects (see below). Fellows must write learning objectives prior to each rotation with guidance of faculty and evaluate themselves in terms of those objectives at the conclusion of the rotation.
A “Continuity Experience” is defined as a long-term assignment (at least twelve months) designed to provide an opportunity for fellows to integrate their knowledge and prior experience in a clinical setting that poses real world clinical informatics challenges. The fellow must be embedded in an interdisciplinary team that is addressing a significant clinical informatics challenge. This includes attending regular team meetings, participating in analysis, planning and implementations of recommendations from the team. The interdisciplinary teams must include physicians, nurses, other health care professionals, administrators and information technology/system personnel.
A “Major Project”: Fellows must conceive, develop, implement and evaluate a substantive, applied clinical informatics project and present the results of the evaluation in a peer-reviewed setting.
Clinical Opportunities: The white paper proposal provides that fellow with the opportunity to maintain their primary board skills during the clinical informatics subspecialty training; however the program may not require that the fellows provide more than 12 hours per week of clinical practice outside the requirements of the clinical informatics program.
Pathology Informatics Clinical Fellowship Program
Table 10 compares the major white paper proposals with the program's implementation.
Table 10.
Rotations, continuity experiences, major projects, and clinical opportunities
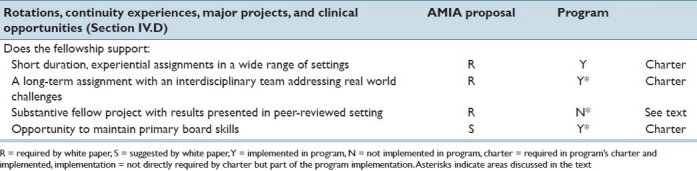
The pathology informatics operational rotation includes the white paper's “experiential rotation” and “continuity experience.” It has been our experience that operational rotations are where fellows learn to evaluate technologies and processes and manage projects and people. It is the core learning experience for clinical fellows (especially in the second year when they have significant leadership responsibilities).
Project continuity also exists in other structures of the program. Fellows normally attend weekly operations meetings of the major IT groups (e.g. the AP LIS group, the CP LIS group, the Transfusion and Blood Banking group). Because these groups are always involved with the major informatics initiatives, the fellow is always aware of these projects. For example, a fellow might be deeply involved in an LIS upgrade during a 4-month rotation, but will follow that project before and after the rotation, through the weekly operational meetings.
The “clinical opportunities” of the white paper seem very similar to our clinical concentration. The concentration has proven a very important component of the informatics fellowship. Our fellows are pathologists (and most have done or will do at least one diagnostic pathology fellowship). They use the clinical concentration to develop and maintain skills in the diagnostic subspecialty in which they will eventually practice.
The pathology fellowship does not currently support a formal “major project” separate from our rotations. Fellows, however, are routinely responsible for multiple real world projects during research and operational rotations, and they present their work in numerous other venues including local meetings, operational meetings, and national conferences.
Program Outcomes
Summary of the AMIA white paper proposals
Program Outcomes (Section IV.E): The program must certify the proficiency of its graduates in eleven activities (the eleven activies are not reproduced here, see the original article). Examples include, “develop, analyze and report effectively (verbally and in writing) on key informatics processes” and “analyze patient care workflow and processes to support improved quality, efficiency, effectiveness and safety of clinical services”.
Pathology Informatics Clinical Fellowship
Table 11 compares the major white paper proposals with the program's implementation. This is the most significant discrepancy between white paper proposal and the program.
Table 11.
Program outcomes
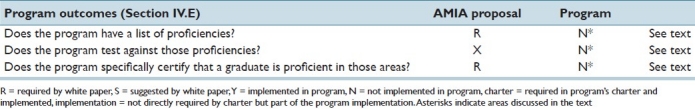
We believe that “program outcomes” is the most important concept in the white paper and the one that will have the greatest impact to our program going forward. As the core pathology informatics course defines a core set of knowledge expected of all graduates, defining a core set of skills expected of a graduate will further help define the field of pathology informatics both internally and to the health system.
We neither have a list of required proficiencies or a program to formally test fellows for proficiencies nor claim that all of our fellows have the same set of skills. We feel that our fellows could accomplish the activities suggested, but some of them are somewhat vague (e.g. one of the proposed outcomes is “Design or develop a clinical or telecommunication application or system.” How does define success?).
As we move into this area, several questions will arise:
Should there be a single core set of skills (for all graduates) or should there be a core set and a second tier of skills depending on the subspecialty interest and career goals of the candidate?
How does one define each skill?
How does one prove (and certify) proficiency?
Finally, a larger issue exists (which may be simply terminology): Does a list of skills rise to the level of program outcomes or is the goal of program something more? This will be considered further in the section “Discussion.”
Program Duration
Summary of the 2009 AMIA White Paper Proposals
Program Duration (Section IV.F): The proposed length of the educational program is 24 months and fellows must complete the program within 48 months of matriculation.
Pathology Informatics Clinical Fellowship
The Pathology Informatics Clinical Fellowship currently recommends a 2-year fellowship, but does support a 1-year program, especially if the candidate is planning to do a second pathology fellowship at our healthcare system and can complete the 2-year core didactic course. However, we have made exceptions if a candidate can only attend 1 year. This is a complex issue and will be considered further in the section “Discussion.”
Section V: Evaluations
Section V of the white paper deals with evaluation of fellows and faculty (Sections V.A, V.B and V.C).
Fellow Evaluations
Summary of the 2009 AMIA White Paper Proposals
Fellow Evaluations (Section V.A): The faculty must evaluate fellows during each educational assignment and document this evaluation at the end of the assignment. The evaluations must include the six ACGME competencies, use multiple evaluators, document progressive improvement appropriate to educational level and provide each fellow with a documented semiannual evaluation of performance with feedback. Evaluation of performance must be accessible for review by the fellow according to institutional policy. Permanent records of evaluations and significant counseling must be maintained in the fellows file and must be available to the fellow and other authorized personnel.
At the conclusion of the training program, each fellow must produce a well-documented portfolio of the knowledge, experiences and skills they have acquired during their training program. The portfolio should follow the general outline of the clinical informatics program requirements document and the final copy should be approved in writing by the Program Director.
At the conclusion of the training program, the program director must provide a summary evaluation of each fellow. The document must document the fellow's performance during the final period of the fellowship and verify that the fellow has demonstrated sufficient competence to enter the practice of clinical informatics without direct supervision.
Pathology Informatics Clinical Fellowship Program
Table 12 compares the major white paper proposals with the program's implementation. There are no significant discrepancies.
Table 12.
Fellow evaluation
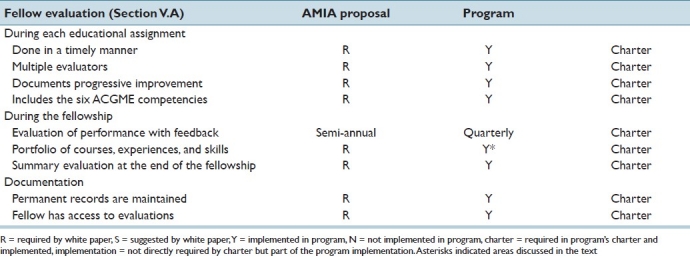
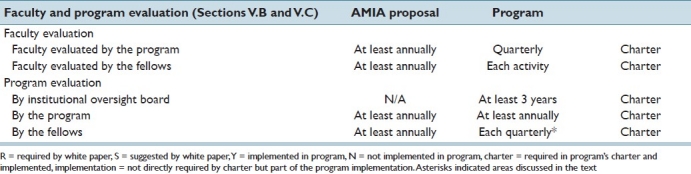
Fellow, faculty, and program evaluation is mandated by the EC as well as the academic departments involved as shown in Tables 12 and 13. Evaluation forms are approved by our institution's EC and records are maintained by the institution's fellowship office.
Table 13.
Faculty and program evaluation
Fellows are required to maintain a log of the educational activities (rotations, conferences, projects, papers, etc.) that they have participated in and the log is reviewed on a regular basis by the fellow and director and forms the basis of an annual report by each fellow. These activity logs are similar to the white paper proposal of a “well documented portfolio of [acquired] knowledge, experiences and skills” maintained by each fellow in a clinical informatics fellowship. In our experience, it is an important tool (for both the fellow and director) for managing a fellows’ training in pathology informatics.
Faculty and Program Evaluations
Summary of the 2009 AMIA White Paper Proposals
Faculty Evaluations (Section V,B): The program must evaluate faculty performance as it relates to the educational program. The evaluations should include teaching ability, commitment, knowledge, professionalism and scholarly activities. The evaluation must include at least annual written confidential evaluations of by fellows.
Program Evaluation and Improvement (Section V.C): The program must document formal, systematic evaluation of the curriculum at least annually. The evaluation should include a) fellow performance, b) faculty development and c) program quality. Faculty and fellows must have the opportunity to evaluate the program and the program must use the results of these evaluations to improve the program. If deficiencies are found the program should prepare a written plan of action that should be reviewed and approved by the faculty.
Pathology Informatics Clinical Fellowship Program
Table 13 compares the major white paper proposals with the program's implementation. There are no significant discrepancies.
In addition to the program evaluations in Table 13, the director meets with the fellows weekly as a group and discusses the program. This routine, informal evaluation of the program has proven to be the most effective mechanism for identifying problems and limitations in the program and has resulted in significant improvements, such as the core didactic course.
Section VI: Fellow Duty Hours in the Learning and Working Environment
Summary of the 2009 AMIA White Paper Proposal
Section VI of the white paper discusses fellow duty hours in the learning and working environment. It deals with a number of issues including supervision of fellows, fatigue, duty hours, on-call activities, moonlighting and duty hours exceptions. The basic principles include: program commitment to the safety of fellows and patients, the priority of protected educational time and resources and adherence to current legal and ACGME rules and recommendations.
Pathology Informatics Clinical Fellowship Program
There do not appear to be discrepancies between the proposal and program. The pathology informatics fellowship is a formal non-GME clinical fellowship overseen by the Partners EC. The EC has given the program DIO review and co-signature, and the program operates under the standard rules for GME training. Pathology informatics fellows sign standard healthcare system non-ACGME clinical fellowship contracts. Fellows do not have patient coverage responsibilities and institutional duty hours are followed. Fellows may carry an information systems operations beeper, but this is only for educational purposes (the fellow is never the first responder for an IT system emergency). Moonlighting is currently not allowed.
Section VII: Experimentation and Innovation
Summary of the 2009 AMIA White Paper Proposal
Section VII of the white paper discusses “experimentation and innovation”. In summary, “Requests for experimentation or innovative projects that may deviate from the institutional, common and specialty specific program requirements must be approved in advance by the Review Committee… Once a Review Committee approves a project, the sponsoring institutions and program are jointly responsible for the quality of education offered to fellows for the duration of such project.”
Pathology Informatics Clinical Fellowship
While we have made significant changes and innovations since the beginning of fellowship program (e.g. the core didactic course) and are continuously adding other processes in response to fellow and faculty feedback, we do not believe these “deviate from the institutional, common, and specialty specific program requirements.” That said, pathology informatics is a dynamic field and careful consideration of the needs of fellows, practices, and of the field of pathology in general will almost certainly drive program innovation on an almost continuous basis.
Summary of Discrepant Findings
Table 14 summarizes the seven areas of discrepancy between the white paper and the pathology fellowship program identified in our evaluation. Five of these involve elements required by the white paper; of which “core ACGME certification for candidates” would only be relevant if clinical informatics is ACGME certified, and “program director selects local directors” is a relatively minor, local issue (see results “Section II: Program personnel and resources”).
Table 14.
Summary of discrepant findings
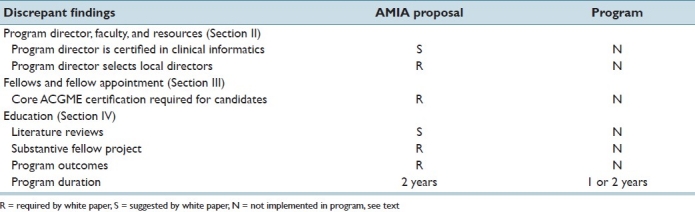
The pathology fellowship does not require a formal, substantive fellow project, but our fellows work on, complete, and present substantive projects routinely as part of research and operational rotations. Formalizing this process would not be difficult, but we are not entirely convinced that such formalization would provide additional value to trainees.
Program outcomes (a defined set of skills the all graduates have certified proficiency in) and a mandatory 2-year fellowship are by far the most important discrepancy identified by the analysis. They are considered further in the section “Discussion.”
DISCUSSION
The AMIA proposal for program requirements in clinical informatics fellowships was developed by an interdisciplinary team during a series of meetings; the rules, structure, and operations of our Pathology Informatics Clinical Fellowship were founded on the many years of experience gathered by pathology informatics programs across the country and evolved at our healthcare system in response to the educational needs of our departments and trainees. The two were developed independently. What is perhaps the most interesting finding in this manuscript is how close the white paper proposal is to the reality of the pathology informatics fellowship. From our reading of the proposal, outlined in this manuscript, it is our opinion that the pathology informatics fellowship would fit all of the requirements for a fellowship program in clinical informatics as put forth in the white paper.
This is perhaps not very surprising: at a high level, clinical informatics and pathology informatics have very similar goals and approaches, and both the proposal and the program were heavily influenced by the traditions (and existing rules) of the ACGME. That said, the very close alignment found by the authors is comforting.
This finding does not imply that the ideal structure of a pathology and/or clinical informatics fellowship program has been found. There is much to be done, especially in improving the common knowledge set, defining basic competencies, and measuring proficiency in those competencies. It also does not necessarily suggest that clinical fellowships in pathology should be identical to clinical informatics fellowships in other medical specialties. Medical specialties are fundamentally different enough that at some level of granularity, the necessary informatics knowledge and skills sets will inevitably differ. Reading the white paper, we believe that it never attempts to define what is sufficient for each subspecialty; it does attempt, however, to define a foundation from which specialties can build. Remember also the scope and direction of our evaluation: We were attempting to determine if the suggestions in the white paper existed in fellowship program but we did do not do the opposite – the evaluation is silent on issues that might be important to the pathology program but are not included in the clinical informatics white paper. However, the results do indicate that there are substantial similarities in clinical informatics across multiple medical domains.
There are several ideas in the clinical informatics white paper and the pathology informatics fellowship that are worth discussing:
Multiple Sites, Faculty, Resources, and Fellows
The white paper proposal supports the use of multiple sites, requires the use of multiple faculty members (Section II.B.1 of the white paper), and mandates that the program “demonstrate financial capacity to support two fellowship positions at all times” (Section I.A.6 of the white paper). We agree with this recommendation. In our experience, multiple sites, faculty, systems, and resources significantly improve the quality and dynamics of the training program and allow the program to support more fellows (and fellows with more diverse interests). Multiple fellows, again in our experience, both improve the educational experience and aggressively drive the innovation in the program.
Clinical Opportunities within Pathology Informatics Fellowships
The proposed clinical informatics fellowship is designed for physicians and its structure includes “clinical opportunities” (Section IV.D.5 of the white paper) through which clinical informatics fellows can “maintain their primary board skills.” The Pathology Informatics Clinical Fellowship is also designed for physicians (pathologists) and allows fellows to maintain their primary diagnostic skills during the fellowship through a “clinical concentration.” Both view practicing medicine and informatics (concurrently) as very positive. There is a very strong, positive relationship between the (proper) design of a system and the (proper) use of a system – a relationship we call the “system-practice co-dependency.” Active physician-informaticians can see and describe both sides of this co-dependency and in doing so provide great value to the system developer, implementer, strategic planner, health system, and user.
The clinical concentration goes to the heart of the relationship between informatics and medicine. One of our fellows and an author of this manuscript was a physician in the Air Force. He was not trained as a line officer or pilot, but starting from day 1 of flight surgeon training it was made clear that flight surgeons had to actively engage the entire squadron and its pilots and become an integral part of it. They had to log a minimum number of flight hours per month and were encouraged to take time off from clinic to participate in 1–2 weeklong missions in which they did almost nothing medical. The purpose of all this was to understand the people in the squadron and their needs, and therefore become better able to identify potential problems early and actively prevent them. It also enabled camaraderie, which led to trust in the flight surgeon. A flight surgeon without a good relationship with or who has a poor understanding of his squadron can cause the entire squadron to avoid seeing them for fear of becoming medically disqualified from flying.
Every experienced informatician has seen similar dynamics in pathology departments. If the informatician is not trusted and not actively involved on a daily basis, systems are not implemented correctly, “work-a-rounds” that ignore informatics principles are developed, and systems are not maintained in alignment with needs and thus become increasingly ineffective. An informatician who is also a diagnostic pathologist is better prepared to help mitigate these issues. Even if the informatician does not actually sign out, he or she should not sit in a distant room unknown and unrecognized by his or her own peers in the department.
Core Knowledge, Competencies, and Outcomes
This is perhaps the most overlooked issue in pathology informatics training today. Traditionally, pathology informatics fellowships have been relatively informal: A fellow would work under a mentor doing research and working on operational projects. Mentorship remains central to fellowship training; however, over the past several years, our fellows have been coming to us with prior, extensive experience in clinical and bioinformatics (including extensive experience in clinical informatics and Masters Degrees in biomedical informatics) specifically for formal and comprehensive training in running informatics divisions. At the same time, pathology departments, reference laboratories, and chief information officers want to know the specific knowledge, skill sets, and competencies a pathology informatics fellowship confers.
The white paper identifies this problem and proposes a number of approaches that, in total, could help address it. Some, such as well-defined educational goals of the program (and of each rotation and course), fellow-written and peer-reviewed publications, a well thought out portfolio of rotations, projects, and immersions, as well as a comprehensive system of evaluation, have been included in the pathology informatics fellowship from its inception. Others, such as the core didactic course, were formally included in 2010 in response to the perceived need for a common, core knowledge base for all fellows. The core course increasingly defines the breadth of knowledge expected of a graduate of our program and has the potential to help define the scope of the field. Today, in general, we use research and operational rotations to provide specialty expertise and didactics to provide discipline-wide breadth.
The next logical step would be defining an acceptable set of competencies that all fellows must master and every program can certify that their graduates have mastered. The white paper proposes 11 such competencies (Program Outcomes, Section VI.E). The list is fairly straightforward and flexible enough so that it could be applied to fellows of multiple interests; and while it is a good start, we feel that it will take time and experience to develop a mature list of competencies. It is something we will be looking to implement in our program in the next several years.
More importantly, however, we are not convinced that the proposed list of skills (and perhaps any list of skills) rises to the level of fellowship outcomes, which we would define as those attributes that make a graduate of a clinical informatics program different from a technology savvy pathologist, an experienced healthcare information technology executive, or an IT consultant. We feel (but cannot prove) that our graduated fellows have those skills, but so do thousands of others who will never enter a fellowship program.
Maybe this is simply a disagreement on terminology (we would probably have little issue if the term was changed from program outcomes to “core informatics skills”). However, the fundamental objective of a clinical informatics fellowship, in pathology and in other fields, has in our opinion not been fully defined. We consider this a very important work in progress.
The discussion of skills and outcomes is further complicated in pathology by the wide range of very diverse subspecialties in pathology itself. A fellow with a background in clinical pathology who plans a career as a medical director of a large, automated laboratory and wants informatics training to understand the systems and processes important in running such a lab requires (potentially) a different set of skills and outcomes than one who wants to apply image analysis to surgical pathology or a fellow who wants to eventually lead a pathology IT/IS group or be a chief medical (or pathology) information officer. It is not that common outcomes or skills are not needed or are definable; the issue instead is whether we would be better served by a two-tiered menu of common (general) and specific skills or whether outcomes should be tied to specific pathology subspecialties. The use of fellow-specific portfolios, listed in the white paper (Section V.A.1.e) and implemented in the pathology program, is a part a response to this concern. This is an area of active discussion within the fellowship today.
Fellowships, ACGME Certification, and Why Do Pathologists go into Pathology Informatics
The white paper was part of an effort to create an ACGME certified subspecialty in clinical informatics, and some of its recommendations, such as a requiring a physician to have finished primary board training before matriculating in a clinical informatics fellowship or a fellowship of 2-year duration, make sense in this context. As pathology considers joining this initiative, it is worth considering the implications for pathology informatics of a 2-year fellowship and board certification.
In our experience, there are three general groups of pathologists that get involved with informatics and join pathology informatics training programs. The first group of pathologists want to become informatics researchers and their needs can be handled separately. The second group has a desire to become primarily (clinical) pathology informaticians with a career path that leads to an informatics director's position in a pathology department, a Chief Medical Information Officer, or a Chief Pathology Information Officer at a health system. For such a career path, one can easily see how a 2-year fellowship and subsequent board certification could make sense.
However, there is a third major group of pathologists that are drawn to informatics for a different reason. These candidates want to use informatics to enhance a career in diagnostic pathology or laboratory medicine. These include the candidate who wants to run a core laboratory and needs informatics knowledge to improve the operations of the laboratory or the anatomic pathologist who wants to learn about image analysis or data quality to improve their specific practice. Such a candidate will almost certainly do at least one diagnostic fellowship after residency; requiring an additional 2-year informatics fellowship would be a relatively high burden.
The issue, as we see it, is that this third group of pathologists is large and very important to pathology, especially given the highly technical, information heavy nature of our field. Many of our fellows, and many of our faculty, are part of this group. Many had extensive informatics skills before they became pathologists (as undergraduates, in graduate school or industry) and now seek to use these skills for very specific purposes in their careers. They neither need nor desire a 2-year fellowship, but will often do 1-year fellowship (or do an ACGME approved “specialty year” as part of their residency). We can imagine a scenario in which the required 2-year fellowships and boards could possibly decrease the number of fellowship-trained pathology informaticians.
Potential subspecialty boards aside, the considerations above are beginning to create two tracks in our clinical fellowship program. One involves 2 years of informatics training and is directed toward the trainee seeking a full-time career in clinical pathology informatics. The second has a single year of informatics and a second year of fellowship in a traditional subspecialty (with the trainee completing the entire 2-year informatics core didactic course). In our opinion, having two approaches provides value to both the individual trainee and the field of pathology as a whole. We plan to continue this two-track approach regardless of the outcome of the subspecialty / board certification discussion and recommend that pathology formalize such an approach in the future.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2012/3/1/11/93893
REFERENCES
- 1.Forsman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem. 1996;42:813–6. [PubMed] [Google Scholar]
- 2.Becich MJ. Information management: moving from test results to clinical information. Clin Leadersh Manag Rev. 2000;14:296–300. [PubMed] [Google Scholar]
- 3.Forsman R. The electronic medical record: implications for the laboratory. Clin Leadersh Manag Rev. 2000;14:292–5. [PubMed] [Google Scholar]
- 4.Myers J. Computer-retrievable surgical pathology files.A low-cost, shareable system. Arch Pathol. 1975;99:516–21. [PubMed] [Google Scholar]
- 5.Shortliffe EH, Blois MS. The computer meets medicine and biology: emergence of a discipline. In: Shortliffe EH, Cimino JJ, editors. Biomedical Informatics: Computer applications in health care and biomedicine. 3rd ed. New York: Springer; 2006. pp. 123–42. [Google Scholar]
- 6.Cornet R, de Keizer N. Forty years of SNOMED: a literature review. BMC Med Inform Decis Mak. 2008;8(Suppl 1):S2. doi: 10.1186/1472-6947-8-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaninotto M, Plebani M. The hospital central laboratory: automation, integration and clinical usefulness. Clin Chem Lab Med. 2010;48:911–7. doi: 10.1515/CCLM.2010.192. [DOI] [PubMed] [Google Scholar]
- 8.Weinstein RS, Graham AR, Richter LC, Barker GP, Krupinski EA, Lopez AM, et al. Overview of telepathology, virtual microscopy and whole slide imaging: prospects for the future. Hum Pathol. 2009;40:1057–69. doi: 10.1016/j.humpath.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Friedman BA. Informatics as a Separate Section within a Department of Pathology. AJCP. 1990;94(4 Suppl 1):S2–6. [PubMed] [Google Scholar]
- 10.Henricks WH, Boyer PJ, Harrison JH, Tuthill JM, Healy JC. Informatics training in pathology residency programs: proposed learning objectives and skill sets for the new millennium. Arch Pathol Lab Med. 2003;127:1009–18. doi: 10.5858/2003-127-1009-ITIPRP. [DOI] [PubMed] [Google Scholar]
- 11.Detmer DE, Lumpkin JR, Williamson JJ. Defining the medical subspecialty of clinical informatics. J Am Med Inform Assoc. 2009;16:167–8. doi: 10.1197/jamia.M3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Safran C, Shabot MM, Munger BS, Holmes JH, Steen EB, Lumpkin JR, et al. Program requirements for fellowship education in the subspecialty of clinical informatics. J Am Med Inform Assoc. 2009;16:158–66. doi: 10.1197/jamia.M3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardner RM, Overhage JM, Steen EB, Munger BS, Holmes JH, Williamson JJ, et al. Core content for the subspecialty of clinical informatics. J Am Med Inform Assoc. 2009;16:153–7. doi: 10.1197/jamia.M3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Jesús VR, Mei JV, Bell CJ, Hannon WH. Improving and assuring newborn screening laboratory quality worldwide: 30-year experience at the Centers for Disease Control and Prevention. Semin Perinatol. 2010;34:125–33. doi: 10.1053/j.semperi.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Kim JY, Lewandrowski KB. Point-of-care testing informatics. Clin Lab Med. 2009;29:449–61. doi: 10.1016/j.cll.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Kim JY, van Cott EM, Lewandrowski KB. The Use of Decision Analysis Tools for the Selection of Clinical Laboratory Tests: Developing Diagnostic and Forecasting Models Using Laboratory “Evidence.”. In: Marchevsky AM, Wick MR, editors. Evidence Based Pathology and Laboratory Medicine. 1st ed. New York: Springer; 2011. pp. 305–22. [Google Scholar]


