Abstract
Training in anaesthesia relies on the duration and quality of clinical experience. It involves exposure to a range of interventions. This works well in routine cases, but when an uncommon and life-threatening event occurs, the anaesthetist needs to carry out multiple tasks simultaneously. Aviation has remarkable similarities with the practice of anaesthesia. Over the years, the aviation industry has used simulation to train and assess individuals very effectively. Anaesthetists face rapidly evolving clinical situations. This needs appropriate decision-making and communication with others in the theatre team. Simulation, using current technology, offers innovative and reproducible training experience. It enables standardised scenario building and reflective learning. Various non-technical aspects of an anaesthetist's day-to-day work could also be addressed to during such training. The technology could be used very effectively for the assessment of competence too. Simulation has been used for technology development and appraisal over the years.
Keywords: ACRM, ANTS, fidelity, fixation errors, simulation, simulator, situation awareness
INTRODUCTION
As anaesthetists, we are involved in various tasks of patient care, which include use of rapidly acting drugs, operating complex devices and performing invasive procedures. This demands safety at the same time. That is one of the reasons our specialty is often compared with the aviation industry.
For many outside our specialty, the saying – “Hours of boredom and moments of terror” epitomises an anaesthetist's work. It is the moment of terror that demands exceptional skills and vigilance, akin to aviation. Flight simulation is an essential part of airline training. It offers a safe environment otherwise impossible to imagine in real-life aviation. Anaesthesia as a specialty has remained at the forefront in using simulation for training.
This article is a brief introduction to the use of simulation in acute medical specialties and its potential uses in skills training, learning team work, competency testing and recruitment. Simulation has several potential applications in medical training and professional development in India.
DEFINITION AND SCOPE
The word “Simulate,” as per Merriam-Webster's dictionary, means “to give or create the effect of, to imitate.”[1]
Simulation is a technique to replace or amplify real patient experiences with guided experiences, artificially contrived, which evokes or replicates substantial aspects of real world in a fully interactive manner.[2]
Flight and aerospace simulators available in museums and entertainment theme parks can give a thrilling experience of aviation. With the help of a screen or a monitor, the visual experience is created. It is topped with seats moving on three axes in multiple planes and effective sound. This offers an exciting space travel simulation.
As a simplistic form of clinical simulation, a model of human airway, can be used to teach airway skills. Similarly, a mannequin can be used to demonstrate central venous, intra-osseous access or to perform endotracheal intubation.
Currently, full-size mannequin patients are used in most simulation centres – Sim Man® from Leardal and Human Patient Simulator-HPS II from METI® – to name a few. They are backed by complex software-based physiology. The person operating this software can make the mannequin as realistic as a real patient [Figure 1].
Figure 1.

A mannequin patient simulator
Thus, a mannequin can be made to blink the eyes, pupils can react to light, tongue swelling and vocal cord spasm may make it impossible to ventilate and intubate the mannequin. The mannequin has mechanical internal structures similar to the human body. It has functional airway and lungs. The heart and circulatory systems are imitated by a compressor and a network of tubes, such that there will be heart beat and palpable pulses. Various organ systems can be made even more realistic by using coloured fluids – red fluid circulating as blood and yellowish fluid to fill the urinary bladder. A learner involved in mannequin-based simulation can feel the changes in airway, breathing, circulation etc. An artificially created pneumothorax can be decompressed with a needle, making an audible sound of air, hissing from the chest with improved ventilation, or a successful venepuncture will result in aspiration of blood from the mannequin circulatory system.
The operation theatre environment created with props like anaesthetic machine, monitors, operating table and a team of people playing roles as surgeons and nurses makes the experience realistic.
A typical anaesthetic simulation involves a patient management scenario. A learner is asked to conduct an anaesthetic on a simulated patient. Before the scenario starts, the learner is briefed about the patient condition and he/she can communicate with the patient. A member can answer with a voice-over to give history or complain of pain or difficulty in breathing, etc. During the scenario, using the associated software, the mannequin patient's condition is manipulated. This change will necessitate the learner to take appropriate corrective action, e.g. dramatic drop in the blood pressure makes it necessary to use vasoactive drug administration. Thus, in the “Anaphylaxis” scenario, it is possible to induce extreme bronchospasm with very high airway pressures and hypotension, with no palpable peripheral pulses on the mannequin. When the learner tries to hand ventilate, it may be nearly impossible to do so. If the learner identifies the problem and takes corrective action, i.e. epinephrine injection, then the software operator can quickly resolve the condition, restoring normal physiology.
After the scenario, an observer from the faculty debriefs the learner. It is quite common to record the scenario proceedings audiovisually. The recording can be played back to follow the course of events and the learner reactions. This way, one can observe the actions taken and resulting changes in mannequin physiology. Debriefing questions help reflective learning. Also, feedback from the observers can be used towards effective learning. Hands-on experience in these scenarios is valuable in reinforcing the procedural skills. A simulation centre has a bank of scenarios programmed and successfully tested. Some examples of anaesthetic scenarios are rapid sequence induction, failed intubation and ventricular tachycardia in an anaesthetised patient. An example scenario of “Anaphylaxis during an anaesthetic” is attached here. The content of sequence of events can be modified to suit the learning objectives.
HISTORY AND DEVELOPMENT OF ANAESTHETIC SIMULATION
Our modern day simulators have roots in early aviation trainers, like Sanders Teacher- an aeroplane skeleton with wooden frame and levers. Link trainer, built using various parts of an aircraft, is regarded as a foundation of flight simulators. World War II saw the development of analogue flight simulation trainers. In the 1960s, digital simulators started appearing on the horizon. From 1970 onwards, computer development saw tremendous improvement in fidelity, motion systems and latency.
Various anaesthetic simulators followed this development. Earlier human patient simulators were used only for anaesthetic specialty-related training. In the 1960s, SimOne, a computer-controlled mannequin patient simulator (MPS) was designed. In the 1980s, teams at the Stanford and University of Florida worked independently on MPSs. The Comprehensive anaesthesia simulation environment (CASE) system became the first commercially available MPS. Later, the focus shifted to use MPS beyond the application of anaesthesia.[3] With the advent of inexpensive personal computers and developing software capabilities, MPSs are improving rapidly.
Virtual Reality (VR) simulation offers the possibility of understanding complex and abstract concepts. Through VR, a learner can transport oneself in an imaginary environment. Various props will aid this experience – by head-mounted displays audio-visually and tactile input from wired gloves. Thus, an individual acts as a voyager through a fantastic journey using computer-assisted design. For example, one can experience a journey through the human body transforming oneself to a blood cell in the circulation enabled by an illusory environment. Nowadays, museums use walkthrough 3D reconstructions. They also use projected images and mix them with real objects, creating an illusion for similar experience.
Further information about the technical aspects of VR can be obtained through an article by Burt.[4]
CLASSIFICATION OF HEALTHCARE SIMULATORS
Despite significant developments in simulation products and the sophistication, there is no universal classification of current simulators. Cumin and Merry[5] describe a framework to classify simulators. They have suggested to classify simulators according to user interaction, simuland (a system simulated by the simulator) or physiological base and utility basis.
Interaction
A simulator can be screen based, hardware based or VR based depending on how the user interacts with it. One can react in a hardware-based simulator in the same way as with a patient. VR-based simulation uses special devices like headsets.
Physiology
A simulator can have a script-controlled or model-controlled physiology. Majority of these devices have computer-controlled physiology, with some manual override.
Use
Simulators are used to teach procedural skills and can be used to teach and assess psychomotor skills and cognitive skills [Figures 2 and 3].
Figure 2.

Airway teaching scenario in progress
Figure 3.

The control station
The term “Fidelity” is used to classify and describe the MPS. It represents truthful connection to a source or an accurate reproduction of the original. A high-fidelity MPS is said to recreate the human anatomy and physiology very closely. However, in this context, fidelity may not always explain the characteristics of a simulator precisely – a plastic model airway trainer is a good duplication of anatomy but cannot work as a high-fidelity device.
APPLICATIONS
As outlined above, simulation is an integral part of training, competency testing and research in aviation. Various other “sharp end” industries like nuclear power, fire fighting and military use simulation for similar purposes. In healthcare, simulation is believed to offer similar applications.[2,6] In Australia and New Zealand, it is an integral part of anaesthetic training[7] and is used similarly in other European countries for continuing professional development.
Standardised patients (SP) have been used in assessing undergraduate medical students.[8] Given the demand for numbers, it may be logistically challenging to arrange SP in undergraduate medical education in India. Simulation may serve as an alternative in these situations. Software-based manipulation of mannequin can be used to show changes in physiology brought about by various drugs and procedures. This is likely to offer an excellent opportunity to integrate teaching of basic sciences and applied medicine in medical schools in India.
Some of the procedures like chest drain insertion and surgical crico-thyrotomy are very rarely performed in day-to-day anaesthetic practice. These skills may be quite vital in anaesthetic emergencies, but are very hard to acquire and retain. Simulation offers a chance to rehearse these rare procedural skills.
In acute care specialties, we work in multidisciplinary teams to manage patients. But, we rarely practice training exercises as teams. The aviation industry has well-structured teamwork training programmes like Crew Resource Management. D Gaba and his team at Stanford realised the potential of simulation-based team training. They adopted this to develop the Anaesthesia Crisis Resource Management (ACRM) programme. It teaches the principles of team behaviour in crisis situations and assesses decision making, interpersonal communication and team management. The CRM model is applicable in other acute medical specialties like emergency medicine, intensive care and neonatology.
In the ACRM, an individual is exposed to a patient care scenario that escalates in a full-blown crisis (e.g., an anaesthetised patient developing severe arrhythmia over a period of a few minutes). In this situation, the anaesthetist is expected to play a leader's role. He/she should guide the whole theatre team to resolve the crisis. However, successfully resolving the arrhythmia is not the only task. In a scenario, he/she should not get fixed to a certain aspect of physiology, but should look at the rapidly evolving clinical situation, review and refocus appropriately.
The leader is expected to communicate with the surgeon and other team members and stop the surgical intervention. He/she should delegate appropriately, e.g. ask a team member to monitor time, request a surgical colleague to obtain further intravenous access and guide the anaesthetic nurse to get appropriate anti-arrhythmic drugs or a defibrillator, etc. If required, he/she should call for help and ask for additional personnel. Thus, he/she should guide a group of people as a team, to work towards a defined goal.
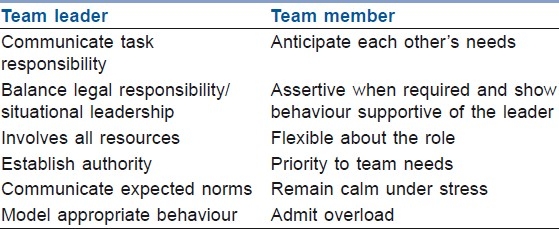
Table 1 enumerates the qualities of an effective team.
Table 1.
Qualities of an effective team
CRM-based training has improved communication in teams, helping a positive change in practice.[9] The Situation Background Assessment Recommendation (SBAR) approach should be used as a standard mode of communication in crisis situations.
Situation: Establish the subject and the reason
Background: Offer additional relevant information
Assessment: State conclusions, concerns
Recommendation: Discuss further action required, expectations
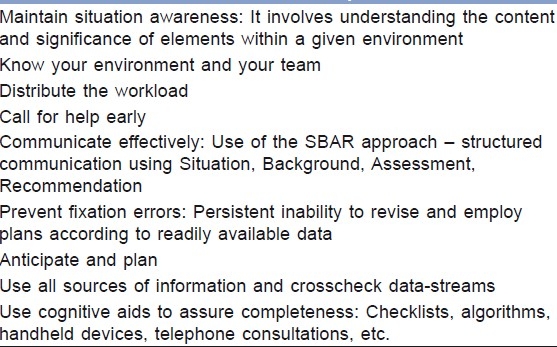
The principle of CRM training stresses on use of all available resources – human, hardware and information. Table 2 outlines a few core concepts of CRM.
Table 2.
Some core concepts of CRM
CRM introduced new ideas in the field of patient care and simulation worked very well to spread these ideas. Interestingly, this created an opportunity to research human behaviour and performance during crises.
There is growing evidence about improved practical skills with the use of simulation-based training.[10] Kuduvalli and colleagues suggest long-term retention of these skills when learned though a simulator-based scenario.[11]
Besides procedural skills, the non-technical skills (NTS) form a significant component of an anaesthetists’ day-to day-work. These are described in terms of cognitive, social and personal resource skills.[12] A team of anaesthetists and psychologists from Scotland has developed the Anaesthesia non-technical skills (ANTS) system. The ANTS framework describes the following four categories of skills:
Situation awareness
Decision making
Task management
Team working
All four categories have component elements, and each has an example of poor and good behaviour. The ANTS framework is used in a number of countries including India, USA and Canada.[13–15] This framework gives an instrument to assess performance during various resource management courses in anaesthetic simulation.
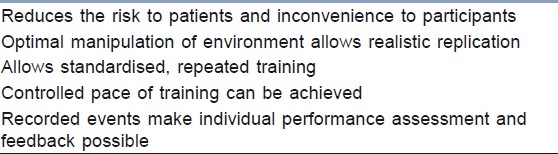
Observation of an individual in a simulated environment enables this assessment. Video replay is an effective way of reflecting on actions and facilitates learning of cognitive processes.[16] The possibility of “pause and discuss” format captures the participants’ understanding of the situation in the moment [Table 3].
Table 3.
Advantages of simulation in healthcare training
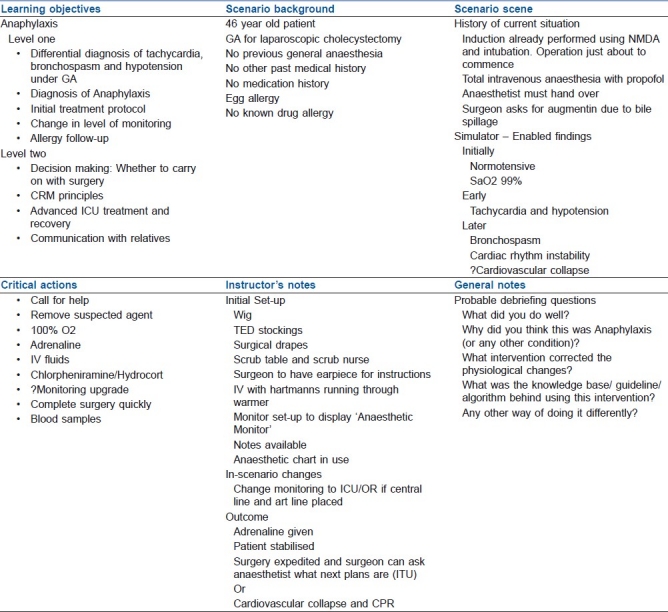
Going beyond training, simulation has been used for the assessment of clinical competencies.[17,18] Assessment of problem-solving skills in acute care [Table 4] yielded very well through simulated scenarios.[19]
Table 4.
Anaphylaxis simulation scenario card
Simulation-based scenarios, when used to assess various skills and competencies, need to be validated as the assessment tools. Boulet describes various issues involved in the process.[20] The Outcome Project of the Accreditation Council for Graduate Medical Education in the US has advocated reliable means of assessing competencies. Objective structured clinical examination (OSCE) has been used to assess the technical skills and theoretical aspects in various clinical specialties.[21] The format of this examination is designed to test all candidates in a uniform manner. The objective nature removes an individual assessor's bias. Simulation yields very well to the demands of OSCE stations in surgical and acute care specialties.
Moving a step further, this technology is used for the medical licensing examination in Italy.[22]
Although simulation is used widely in assessing the procedural skills, how uniformly it could be used in medicine to recruit the “right person for right job” was difficult to establish. There is an effort to validate the simulated scenarios, towards selection of trainees in Anaesthetic specialty training, at some of the deaneries in the UK.[23]
Development and modifications of various airway devices has been performed on mannequins for many years. However, the advantage of manipulating the mannequin anatomy – like converting an easy airway to a difficult one – enabled comparison of devices in real life-like situations.[24–26] Some recent studies underline its potential for technology appraisal – for design of new airway devices, spinal needles.[27,28]
The Society for Simulation in Healthcare[29] is a specialist society, elucidating the research and system integration options in this field.
LIMITATIONS
Notwithstanding the advantages mentioned above, one must realise the limitations of simulation. One of the criticisms is the extent to which a simulator can reproduce the real-life situations. In the healthcare setup, we should be aware of the differences between simulated and real patient anatomy to maximally utilise the benefit of such training.[30] In a recent editorial, Rai and Popat point out a dearth of patient-based studies following mannequin-based ones.[31]
Cumin and colleagues further stress the need for standards in healthcare simulation to achieve full potential of the technology.[32]
SUMMARY
Anaesthesia as a specialty has pioneered patient safety initiatives. The dynamic situation we face when managing an anaesthetic and lack of therapeutic benefit when used alone has led this effort. Adaptation of simulation for training and assessment is leading the way in this field. It has underlined the importance of NTS an anaesthetist uses in everyday work. Sharing information, contingency planning and good communication is essential for safe anaesthetic management of our patients. Simulation offers a way forward to acquire these skills in a controlled manner and will prove as a valuable tool towards our professional development.
ACKNOWLEDGMENT
The author is grateful for the help of the staff of the Anaesthetics department and Dr. M. Mackenzie, Consultant Anaesthetist, East Surrey Hospital, Redhill.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Springfield, Massachusetts: Merriam-Webster, Inc; 1995. Merriam-Webster dictionary; Home and office edition. [Google Scholar]
- 2.Gaba DM. The future vision of simulation in healthcare. Qual Saf Health Care. 2004;13:i2–10. doi: 10.1136/qshc.2004.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lampotang S. Medium and high integration patient simulators. In: Riley RH, editor. Manual of Simulation in Healthcare. Oxford University Press; 2008. [Google Scholar]
- 4.Burt DE. Virtual reality in anaesthesia. Br J Anaesth. 1995;75:472–80. doi: 10.1093/bja/75.4.472. [DOI] [PubMed] [Google Scholar]
- 5.Cumin D, Merry AF. Simulators for use in anaesthesia. Anaesthesia. 2007;62:151–62. doi: 10.1111/j.1365-2044.2006.04902.x. [DOI] [PubMed] [Google Scholar]
- 6.Helmreich RL, Davies JM. Anaesthetic simulation and lessons to be learned from aviation. Can J Anaesth. 1997;44:907–12. doi: 10.1007/BF03011959. [DOI] [PubMed] [Google Scholar]
- 7.Weller J. Effective management of anaesthetic crises-design, development and evaluation of simulation based course. In: Riley RH, editor. Manual of Simulation in Healthcare. Oxford University Press; 2008. [DOI] [PubMed] [Google Scholar]
- 8.Colliver JA, Swartz MH. Assessing clinical performance with standardized patients. JAMA. 1997;278:79–91. doi: 10.1001/jama.278.9.790. [DOI] [PubMed] [Google Scholar]
- 9.Weller J, Wilson L, Robinson B. Survey of change in practice following simulation based training in crisis management. Anaesthesia. 2003;58:471–9. doi: 10.1046/j.1365-2044.2003.03078_1.x. [DOI] [PubMed] [Google Scholar]
- 10.Bruppacher HR, Alam SK, LeBlanc VR. Simulation based training improves physicians’ performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010;112:775–6. doi: 10.1097/ALN.0b013e3181d3e31c. [DOI] [PubMed] [Google Scholar]
- 11.Kuduvalli PM, Parker CJ, Leuwer MC, Guha AC. Retention and transferability of team-resource-management skills in anaesthetic emergencies: The longer term impact of high fidelity simulation based course. Euro J Anaesth. 2009;26:17–22. doi: 10.1097/EJA.0b013e32831bc665. [DOI] [PubMed] [Google Scholar]
- 12.Flin R, O’Connor P, Crichton M. Safety at the sharp end: A guide to non-technical skills. Aldershot: Ashgate Publishing Limited; 2008. [Google Scholar]
- 13.Yee B, Naik V, Joo H, Savoldelli G, Chung D, Houston P, et al. Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education. Anesthesiology. 2005;103:241–8. doi: 10.1097/00000542-200508000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Divekar D. Nontechnical skills in anaesthesiology. Pravara Med Rev. 2009;4:4–10. [Google Scholar]
- 15.Steadman R. Improving on reality.Can simulation facilitate practice change? Anaesthesiology. 2010;112:775–6. doi: 10.1097/ALN.0b013e3181d3e337. [DOI] [PubMed] [Google Scholar]
- 16.Flin R, Patey R, Glavin R, Maran N. Anaesthetists’ non-technical skills. Br J Anaesth. 2010;105:38–44. doi: 10.1093/bja/aeq134. [DOI] [PubMed] [Google Scholar]
- 17.Murray DJ, Boulet JR, Kras JF, Woodhouse JA, Cox T, McAllister JD. Acute care skills in anesthesia practice: A simulation-based resident performance assessment. Anesthesiology. 2004;101:1084–95. doi: 10.1097/00000542-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Schwid HA, Rooke GA, Carline J, Steadman RH, Murray WB, Olympio M, et al. Anesthesia simulator research consortium: Evaluation of anesthesia residents using mannequin-based simulation: A multi-institutional study. Anesthesiology. 2002;97:1434–44. doi: 10.1097/00000542-200212000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Gaba D, Howard S, Flanagan B, Smith B, Fish K, Botney R. Assessment of clinical performance during simulated crises using both technical and behavioral ratings. Anesthesiology. 1998;89:8–18. doi: 10.1097/00000542-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Tetzlaff JE, Warltier DC. Assessment of competency in Anesthesiology. Anesthesiology. 2007;106:812–25. doi: 10.1097/01.anes.0000264778.02286.4d. [DOI] [PubMed] [Google Scholar]
- 21.Boulet JR, Murray DJ. Simulation-based assessment in anesthesiology: Requirements for practical implementation. Anesthesiology. 2010;112:1041–52. doi: 10.1097/ALN.0b013e3181cea265. [DOI] [PubMed] [Google Scholar]
- 22.Guagnano MT, Merlitti D, Manigrasso MR, Pace-Palitti V, Sensi S. New medical licensing examination using computer-based case simulations and standardized patients. Acad Med. 2002;77:87–90. doi: 10.1097/00001888-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Adams D, Sice P, Anderson I, Gale T, Lam H, Langton J, et al. Validation of simulation for recruitment to training posts in anaesthesia. Anaesthesia. 2009;64:805–6. [Google Scholar]
- 24.Koyama Y, Inagawa G, Miyashita T, Kikuchi T, Miura N, Miki T, et al. Comparison of the Airway Scope®, gum elastic bougie and fibreoptic bronchoscope in simulated difficult tracheal intubation: A manikin study. Anaesthesia. 2007;62:936–9. doi: 10.1111/j.1365-2044.2007.05152.x. [DOI] [PubMed] [Google Scholar]
- 25.Komatsu R, Kamata K, Sessler D, Ozaki M. A comparison of the Airway Scope® and McCoy laryngoscope in patients with simulated restricted neck mobility. Anaesthesia. 2010;65:564–8. doi: 10.1111/j.1365-2044.2010.06334.x. [DOI] [PubMed] [Google Scholar]
- 26.Tan BH, Liu EH, Lim RT, Liow LM, Goy RW. Ease of intubation with the GlideScope or Airway Scope by novice operators in simulated easy and difficult airways – A manikin study. Anaesthesia. 2009;64:186–90. doi: 10.1111/j.1365-2044.2008.05753.x. [DOI] [PubMed] [Google Scholar]
- 27.Harrison S, Robinson NP, Shaikh A, Yentis SM. Manikin evaluation of the Tulip®, a new supraglottic airway. Anaesthesia. 2009;64:807. [Google Scholar]
- 28.Cook TM, Payne S, Skryabina E, Hurford D, Clow E, Georgiou A. A simulation-based evaluation of two proposed alternatives to Luer devices for use in neuraxial anaesthesia. Anaesthesia. 2010;65:1069–79. doi: 10.1111/j.1365-2044.2010.06537.x. [DOI] [PubMed] [Google Scholar]
- 29. [Last cited on 2011 Feb 03]. Available from: http://www.ssih.org/SSIH/ssih/Home/
- 30.Hesselfeldt R, Kristensen MS, Rasmussen LS. Evaluation of the airway of SimMan full-scale patient simulator. Acta Anaesthesiol Scand. 2005;49:1339–45. doi: 10.1111/j.1399-6576.2005.00856.x. [DOI] [PubMed] [Google Scholar]
- 31.Rai MR, Popat MT. Evaluation of airway equipment: Man or mannequin? Anaesthesia. 2011;66:1–3. doi: 10.1111/j.1365-2044.2010.06567.x. [DOI] [PubMed] [Google Scholar]
- 32.Cumin D, Weller J, Henderson K, Merry AF. Standards for simulation in anaesthesia: Creating confidence in tools. Br J Anaesth. 2010;105:45–51. doi: 10.1093/bja/aeq095. [DOI] [PubMed] [Google Scholar]


