Abstract
Background:
The airway instrumentation of direct laryngoscopy and tracheal intubation are powerful noxious stimuli that should be attenuated by appropriate premedication, smooth induction and rapid intubation. The present study evaluated the safe and clinically effective dose of oral pregabalin premedication for attenuation of haemodynamic pressor response of airway instrumentation.
Methods:
A total of 90 normotensive adult consented patients aged 24–56 years, ASA grade I and II, of both gender were randomized into three treatment groups of 30 patients each. Group I received oral placebo, Group II oral pregabalin 75 mg and Group III oral pregabalin 150 mg 1 h prior to induction. Anaesthetic technique was standardized and all groups were assessed for pre-operative sedation, haemodynamic changes after the premedication, before and after induction, after laryngoscopy and intubation, along with intraoperative haemodynamic stability and post-operative side-effects.
Results:
Pre-operative sedation levels were higher with pregabalin premedication. Significant increase in heart rate and mean arterial pressure was observed in Groups I and II after airway instrumentation, while statistically significant attenuation of mean arterial pressure was seen in Group III. No significant decrease in heart rate was observed in any group. None of the patient has suffered from any post-operative side-effects, and no significant differences in the parameters of recovery and awakening time were observed.
Conclusion:
Oral pregabalin premedication has adequately sedated the patients. The haemodynamic pressor response of airway instrumentation was attenuated in a dose-related fashion. The premedicated patients were haemodynamically stable perioperatively without prolongation of recovery time and side-effects.
Keywords: Haemodynamic pressor response, intubation, laryngoscopy, pregabalin, sedation
INTRODUCTION
Haemodynamic pressor response to airway instrumentation (direct laryngoscopy and intubation) is a hazardous complication of general anaesthesia.[1] Many pharmacological techniques were evaluated either in the premedication or during the induction to attenuate these adverse haemodynamic responses to airway instrumentation, such as deepening the anaesthesia, pre-treatment with vasodilators, adrenoceptor blockers, calcium channel blockers and opioids, with variable results.[2,3] Several studies have reported the usefulness of pregabalin as a post-operative analgesic with higher patient satisfaction,[4] but no randomized controlled study has been carried out to evaluate the haemodynamic pressor response of airway instrumentation. The aim of our study was to determine the minimum effective and safe dose of pregabalin premedication for attenuation of pressor response to laryngoscopy.
Pregabalin, a gabapentinoid compound, is described structurally as (S)-3 aminomethyl-5-methylhexanoic acid. Pregabalin is structurally related to the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), but is not functionally related to it. It acts by decreasing the synthesis of neurotransmitter glutamate to act on the central nervous system, and possesses analgesic, anticonvulsant and anxiolytic activity and is effective in preventing neuropathic component of acute nociceptive pain of surgery.[5] It is well absorbed and tolerated after oral administration, with peak plasma concentrations occurring within 1 h. It undergoes negligible hepatic metabolism. It is non-narcotic, with clinically important reduction in pain and adverse haemodynamic response.
The present study was designed as a prospective, blind, randomized controlled study to evaluate and compare the efficacy and safety of two doses of oral pregabalin premedication for attenuation of haemodynamic pressor response of airway instrumentation with pre-operative sedation and perioperative haemodynamic stability.
METHODS
The study, approved by the Institutional Ethical Committee, was carried out from August 2009 to July 2010. This prospective, blind, randomized controlled study consisted of 90 normotensive adult consented patients aged 24–56 years of both genders, scheduled for elective surgery under general anaesthesia with ASA physical status I and II. Patients with anticipated difficult intubation, history of cardiac, pulmonary or renal disease, obesity, allergy to any anaesthetic medication and taking sedatives, hypnotics or antihypertensive medication were excluded from the study. When duration of laryngoscopy exceeded 22 s, or a second attempt for intubation was needed, those patients were also excluded from the study. None of the patients had previous experience with general anaesthesia.
After thorough pre-anaesthetic evaluation, patients were randomly allocated to three groups of 30 patients each by a computer-generated random table. Group I received placebo (P0), Group II received pregabalin 75 mg (P75) and Group III received pregabalin 150 mg (P150), given orally with sips of water about 1 h before induction of general anaesthesia. Group allocations were performed by an anaesthetist who was unaware of the study protocol and was not involved in the study.
On arrival in the operating room, monitors were attached and baseline heart rate and systolic, diastolic and mean arterial blood pressure were recorded. The pre-operative level of sedation was assessed by the Ramsay sedation scale: 1, anxious, agitated or restless; 2, co-operative, oriented and tranquil; 3, responds to command; 4, asleep with brisk response to stimulus; 5, asleep with sluggish response to stimulus; 6, asleep with no response.[6]
A crystalloid intravenous infusion of 6-8 ml/kg was started and all patients were premedicated with metoclopramide (10 mg), glycopyrrolate (0.2 mg), midazolam (1 mg) and butorphanol (1 mg). After pre-oxygenation for 3 min with 100% oxygen, anaesthesia was induced with propofol (2 mg/kg) or in a dose sufficient for loss of verbal commands. The direct laryngoscopy and intubation was facilitated with rocuronium 0.9 mg/kg after 90s, and of minimum possible duration.[7,8] It was being similar to all patients. Anaesthesia was maintained with isoflurane and nitrous oxide 60% in oxygen by gas monitoring on a DatexOhmedaCardiocap 5 monitor. The patients were mechanically ventilated to maintain the normocapnia (CO2 between 35 and 40 mmHg). The supplemental neuromuscular blockade was achieved with rocuronium 0.1 mg/kg. After completion of surgery, residual neuromuscular block was antagonized with appropriate doses of neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg), and the extubation was performed when respiration was adequate.
Intraoperatively, the heart rate, mean arterial blood pressure, electrocardiography, pulse oximeter (SpO2) and EtCO2 levels were continuously monitored and recorded before and after induction, immediately after intubation and 1, 3, 5 and 10 min, thereafter at every 5-min interval till end of surgery. Patients were observed for complications like hypotension, hypertension, arrhythmias, hypoxemia and bronchospasm, and treated as required. Tachycardia was defined as heart rate greater than 100 beats/min and hypertension when systolic blood pressure was more than 180 mmHg. Autonomic or somatic signs of insufficient anaesthesia included lacrimation, sweating and flushing, which were treated by increasing the inhaled concentration of isoflurane and supplemental bolus doses of fentanyl (0.5 μg/kg). Hypotension was defined as fall in mean arterial pressure by more than 20% from baseline, and was treated by increasing the intravenous infusion and, additionally, with vasoactive drugs. Bradycardia was defined as reduction in heart rate less than 60 beats/min, and was treated with intravenous atropine (0.01 mg/kg).
Anaesthetic and surgical techniques were standardized for all patients. All groups were assessed for pre-operative sedation and changes in heart rate and mean arterial blood pressure after induction and airway instrumentation intraoperatively. The patients were transferred to the post-anaesthesia care unit and monitored for at least 3 h, or until there were no signs of any drug-induced effects such as nausea, vomiting, any respiratory inadequacy or haemodynamic instability in form of hypotension/hypertension or tachycardia/bradycardia. If any side-effects were noted, they were treated accordingly.
The sample size was decided in consultation with the statistician, and was based on initial pilot observations, indicating that approximately 20–23 patients should be included in each group in order to ensure a power of 0.80 for detecting clinically meaningful reduction by 10–20% in heart rate and mean arterial blood pressure. Assuming a 5% dropout rate, the final sample size was set at 90 patients, which would permit a type I error of alfa=0.05, with a type II error of beta=0.5 and power of 0.8.
Statistical analysis
The results obtained in the study are presented in a tabulated manner and analyzed using Microsoft Excel and SPSS software. The haemodynamic variables were represented by mean value±SD. The statistical significance in mean difference was performed using analysis of variance (ANOVA) and Chi square test as appropriate. A P value of <0.05 was considered significant and <0.001 as highly significant. The failure rate of drug was defined as >30% increase in haemodynamic parameters from the baseline values.
RESULTS
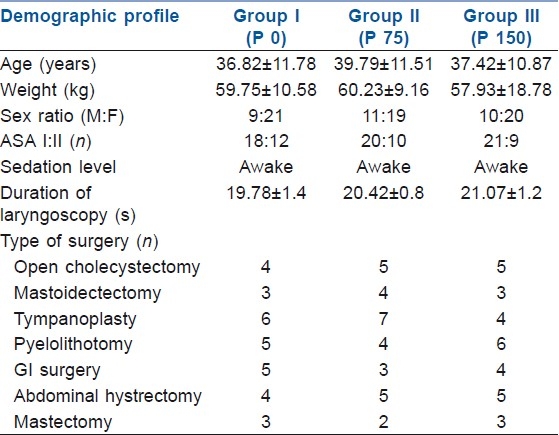
Of the total of 90 patients, 30 patients in each group were evaluated and compared. All the three groups were comparable with respect to the demographic and operational factors. No significant differences were found among them with respect to age, sex, weight, time between oral premedication of pregabalin administration to anaesthetic induction, type of surgical procedures, duration of laryngoscopy and anaesthesia [Table 1].
Table 1.
Demographic profile, duration of laryngoscopy and types of surgery
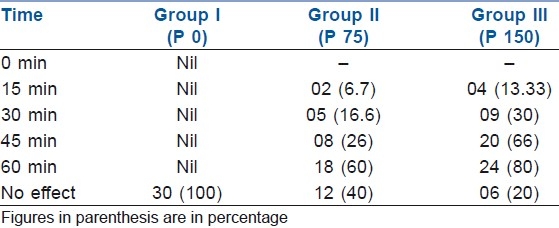
The degree of sedation before pregabalin premedication was comparable between the groups. Sedation was significantly higher in the pregabalin 150 mg group III at the pre-induction stage as compared with groups I and II. Onset of action for level 2 sedation was seen after 15 min in two patients (6.7%) of group II and in four patients (13.33%) of group III, while at 60 min, 24 patients (80%) of group III fell asleep with brisk response (level 4) [Table 2].
Table 2.
Onset of sedation after pregabalin
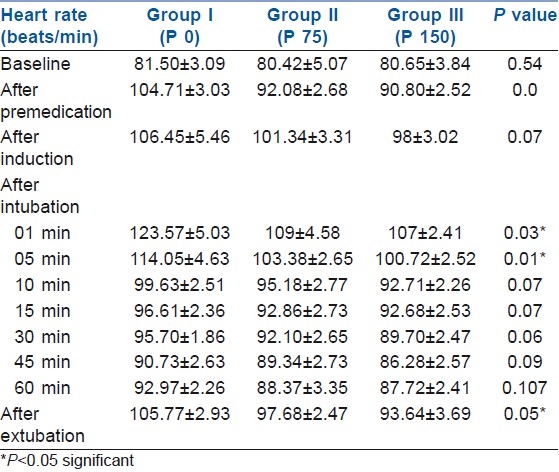
There was no significant difference in the heart rate and mean arterial pressure values among groups before and after premedication. Immediately after laryngoscopy and intubation, the heart rate increased significantly in all groups, but the increase was least in group III (P150). Maximum increase in heart rate from baseline was observed after 1 min of laryngoscopy, but statistically highly significant increase was observed at 5 min, with significant change seen at 10 min. No statistically significant attenuation of heart rate was observed in the premedicated group, although it remained stabilized as compared with the control group (P 0) [Table 3].
Table 3.
Changes in heart rate during anaesthesia
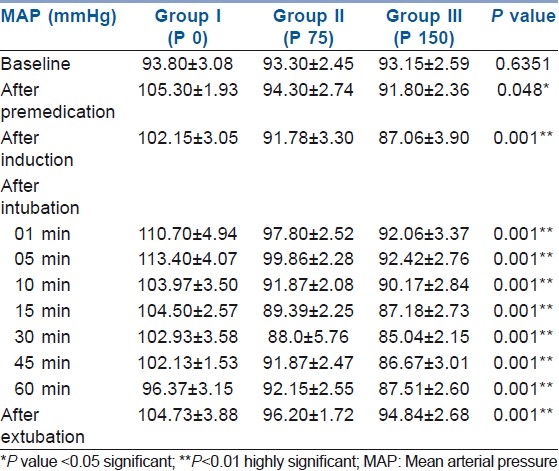
No significant difference was observed in the mean arterial pressure before and after premedication but, after laryngoscopy and intubation, the attenuation of mean arterial blood pressure in the premedicated group was statistically significant as compared with the control group, in a dose-related fashion [Table 4].
Table 4.
Changes in mean arterial pressure during anaesthesia
Intraoperative heart rate and mean arterial blood pressure values were attenuated and remained stabilized to base values in the premedicated group. Even in the post-anaesthesia care unit, cardiovascular parameters remained at a lower level in the pregabalin group in a dose-related manner than in the control group.
Clinically significant respiratory depression was not seen in any group of the study. The fall in oxygen saturation was not seen. The pre-operative lowest recorded SpO2 values were between 97% and 98% in all three groups, and it further decreased only to 95% in group III (P 150).
A decreased amount of propofol was required for induction of anaesthesia in the pregabalin groups (1.71±0.14 mg/kg) as compared with the control group (1.93±0.12 mg/kg) for loss of verbal command. Intraoperatively, the control group was supplemented by bolus doses of fentanyl (0.5 μg/kg) when there was more than a 20% increase in the haemodynamic parameters or signs of inadequate depth of anaesthesia, while no analgesic supplement was needed for the pregabalin groups. Rapid intravenous infusion was required in seven patients of group III (P 150) and two patients of group II (P 75) to treat hypotension. Vasoactive medication was not required in any patient.
There were no differences among the three groups with respect to awakening and recovery time. All patients were well oriented and were able to obey commands in the post-operative care unit. No post-operative respiratory depression, nausea and vomiting have occurred and no other post-operative complication was recorded in any group during our study.
DISCUSSION
The present study evaluated the safe and clinically effective dose of oral pregabalin premedication for its sedative effect and for attenuation of haemodynamic pressor response of airway instrumentation of direct laryngoscopy and intubation. The significant attenuation of haemodynamic pressor response was observed by oral pregabalin premedication in a dose-related manner, with minimum effect on heart rate. The increase in haemodynamic values in the control group may be due to inadequate sedation and analgesia. The analgesic effect of gabapentin has been investigated during the past few years and, because of its good analgesic and opioid-sparing effect, it is now effectively used in post-operative pain management.[9,10] Fassoulaki et al. and Memis et al. have studied the effective attenuation of pressor response of laryngoscopy and intubation after oral premedication of gabapentin.[11,12] The haemodynamic results of our study were in agreement with recent results with gabapentin. Compared with gabapentin, pregabalin has a predictable and linear pharmacokinetic profile.[5]
The haemodynamic pressor response during laryngoscopy and intubation, in the form of tachycardia and hypertension, occurs frequently.[1] Shribman et al. reported that laryngoscopy alone or with tracheal intubation increases the arterial blood pressure and catecholamine levels, while intubation significantly increases heart rate.[13] Reid et al. and Hassan et al. reported high incidences of cardiac arrhythmias, myocardial ischemia, acute left ventricular failure and cerebrovascular accidents following intubation in hypertensive patients.[14,15] These physiological changes are due to variation in the balance of sympathetic and parasympathetic outflow or receptor hypersensitivity. Specific measures should be taken to prevent these changes as hypertension may affect perioperative morbidity through the extent of end organ damage, like myocardial ischemia or cerebral haemorrhage.[16] Aronson and Fontes stated that rise in pulse pressure as little as 10 mmHg in both normotensive and hypertensive persons is associated with a 20% or more increased risk of renal failure, coronary events and cerebral stroke.[17]
Many pharmacological techniques were introduced and evaluated either in the premedication or during induction to attenuate the haemodynamic pressor response to airway instrumentation, but results were controversial. More attention is given to the use of selective beta-adrenergic blockers to prevent the reflex sympatho-adrenal discharge-mediated tachycardia and hypertension during laryngoscopy and intubation. Hypotensive agents, including sodium nitroprusside, nitroglycerine, adrenoreceptor blockers, calcium channel blockers and opioids, have been used effectively to attenuate these haemodynamic responses. Intranasal nitroglycerine tends to block the hypertensive response to airway instrumentation.[18] The intravenous lidocaine (1.5 mg/kg) prevented the increase in mean arterial pressure with no effect on heart rate. Among opioids, remifentanil(1 μg/kg), alfentanil (10–20 μg/kg) or fentanyl (0.5–1 μg/kg) have been used successfully to attenuate haemodynamic pressor response to laryngoscopy and tracheal intubation, but these are associated with bradycardia, hypotension and post-operative respiratory depression.[2,19,20] Glossopharyngeal and superior laryngeal nerve blocks along with topical analgesia may also be effective methods. Helfman et al. reported that a 150 mg esmolol bolus was superior to intravenous high-dose lidocaine or low-dose fentanyl in preventing the tachycardia associated with intubation.[3]
In our study, the 150 mg oral pregabalin has sedated the patients pre-operatively and effectively attenuated the laryngoscopy and intubation-induced haemodynamic pressor response intraoperatively. There was perioperative haemodynamic stability with no post-operative side-effects and respiratory inadequacy.
When assessing techniques to lessen the haemodynamic pressor responses of airway instrumentation, the induction agents may influence the results. We have used propofol as an induction agent, which produces hypotension more than thiopental and bradycardia, which has helped to compensate in part the haemodynamic changes induced due to laryngoscopy and intubation in all patients. The salivary and tracheobronchial mucus secretions necessitate prophylactic administration of an antisialagogue agent. Glycopyrrolate, which does not penetrate the blood–brain barrier, was the rational choice.
The incidence of nausea and vomiting after general anaesthesia has been reported to be as high as 24%. Many studies were carried out to prevent post-operative nausea and vomiting, and reported that none of the available antiemetics is entirely effective, perhaps because most of them act through the blockage on one type of receptor. The combined antiemetic with different sites of activity may be more effective.[21] The intravenous antiemetic, such as ondansetron, often with dexamethasone, has been used. Metoclopramide has been shown to be an effective and safe antiemetic for both prevention and treatment of post-operative nausea and vomiting.[22] In the present study, metoclopramide was used as it acts both centrally and peripherally, enhances gastric emptying time and increases the tone of the lower oesophageal sphincter.[23] Post-operative nausea and vomiting were not recorded in any patient during study.
We studied patients up to 59 years as elderly patients more often take drugs such as antidepressants, hypnotics and antihypertensives with increased sensitivity to anaesthetic medications, and the safety and effectiveness of pregabalin in children and adolescents has not been established.
The attenuation of pressor response of airway instrumentation of direct laryngoscopy and intubation with near-stable haemodynamic variables and no post-operative complication during the present study was an indication of clinically effective and safe analgesia and sedation with oral pregabalin (150 mg) premedication. Several mechanisms may contribute to the beneficial effects, which includes the modulation of visceral pain and central sensitization.[5,6] It will be appropriate at this juncture to put forward that the favourable pharmacokinetics of pregabalin make it a valuable premedicant for attenuation of haemodynamic pressor response of airway instrumentation during general anaesthesia.[22,23]
The intraoperative haemodynamic stability may be beneficial in obese, hypertensive and cardiac compromised patients. The pregabalin may be used in asthmatic and airway-compromised patients as it does not cause post-operative respiratory depression.
CONCLUSION
Pregabalin is emerging as an effective and safe drug as it leads to sedation, analgesia and haemodynamic stability. A single, oral dose of 150 mg of pregabalin premedication seems to be effective in attenuating the haemodynamic response to orotracheal intubation after the first attempt, an effect which may be useful in patients suffering from coronary insufficiency.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Prys Roberts C, Green LT, Meloche R, Foex P. Studies of Anaesthesia in relation to hypertension II, Hemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971;43:531–47. doi: 10.1093/bja/43.6.531. [DOI] [PubMed] [Google Scholar]
- 2.Korpien R, Sarnivaara L, Siren K, Sarna S. Modification of the haemodyamic responses to induction of anaesthesia and tracheal intubation with alfentanil, esmolol and their combination. Can J Anaesth. 1995;42:298–304. doi: 10.1007/BF03010706. [DOI] [PubMed] [Google Scholar]
- 3.Helfman SM, Gold MI, Delisser EA, Herrington CA. Which drug prevents tachycardia and hypertension associated with tracheal intubation: Lidocaine, Fentanyl, or Esmolol? AnesthAnalg. 1991;72:82–6. doi: 10.1213/00000539-199104000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K. Premedication with pregabalin 75 or 150 mg with ibuprofen to control pain after day-case gynaecological laparoscopic surgery. Br J Anaesth. 2008;100:834–40. doi: 10.1093/bja/aen098. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice. Epilepsia. 2004;45:13–8. doi: 10.1111/j.0013-9580.2004.455003.x. [DOI] [PubMed] [Google Scholar]
- 6.Stawicki SP. Sedation scales: Very useful, very underused. OPUS12 Scientist. 2007;1:10–2. [Google Scholar]
- 7.Miller RD. Miller's Anaesthesia. 7th ed. Vol. 27. Philadelphia: Churchill Livingstone Elsevier; 2009. [Google Scholar]
- 8.Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology. 1993;79:913–8. doi: 10.1097/00000542-199311000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Seib RK, Paul JE. Preoperative gabapentin for postoperative analgesia: A meta-analysis. Can J Anaesth. 2006;53:461–9. doi: 10.1007/BF03022618. [DOI] [PubMed] [Google Scholar]
- 10.Pandey CK, Priye S, Singh S, Singh U, Singh RB, Singh PK. Pre-emptive use of gabapentin significantly decreases postoperative pain and rescues analgesic requirements in laparoscopic cholecystectomy. Can J Anaesth. 2004;51:358–3. doi: 10.1007/BF03018240. [DOI] [PubMed] [Google Scholar]
- 11.Fassoulaki A, Melemeni A, Paraskeva A, Petropoulos G. Gabapentin attenuates the pressor response to direct laryngoscopy and tracheal intubation. Br J Anaesth. 2006;96:769–73. doi: 10.1093/bja/ael076. [DOI] [PubMed] [Google Scholar]
- 12.Memis D, Turan A, Karamanlioglu B, Seker S, Ture M. Gabapentin reduces cardiovascular responses to laryngoscopy and tracheal intubation. Eur J Anaesth. 2006;23:686–90. doi: 10.1017/S0265021506000500. [DOI] [PubMed] [Google Scholar]
- 13.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine response to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 14.Reid LC, Brace DE. Irritation of the respiratory tract and its reflex effect upon heart. SurgGynaeObstet. 1940;70:157–62. [Google Scholar]
- 15.Hassan HG, EL-Sharkawy TY, Renk H, Mansour G, Fouda A. Hemodynamic and catecholamine stress responses to laryngoscopy with vs without endotracheal intubation. ActaAnesthesiolScand. 1991;35:442–7. doi: 10.1111/j.1399-6576.1991.tb03325.x. [DOI] [PubMed] [Google Scholar]
- 16.Fox EJ, Sklar GS, Hill CH, Villanueva R, King BD. Complication related to the pressure responses to endotracheal intubation. Anaesthesiology. 1977;47:524–5. doi: 10.1097/00000542-197712000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Aronson S, fonts ML. Hypertension: A new look at an old problem. CurrOpinAnesth. 2006;19:59–64. doi: 10.1097/01.aco.0000192784.47645.7b. [DOI] [PubMed] [Google Scholar]
- 18.Fassoulaki A, Kaniaris P. Intranasal administration of nitroglycerine attenuates the presser response to laryngoscopy and intubation of the trachea. Br J Anaesth. 1983;55:49–52. doi: 10.1093/bja/55.1.49. [DOI] [PubMed] [Google Scholar]
- 19.Habib AS, Parker JL, Maguire AM, Rowbotham DJ, Thomson JP. Effects of remifentanil and alfentanil on the cardiovascular responses to induction of anesthesia and tracheal intubation in the elderly. Br J Anaesth. 1998;80:467–9. doi: 10.1093/bja/88.3.430. [DOI] [PubMed] [Google Scholar]
- 20.Martin DE, Rosenberg H, Aukberg SJ, Bartkowski RR, Edwards MW, Greenhow DE, et al. Low dose fentanyl blunts circulatory responses to tracheal intubation. AnesthAnalg. 1982;61:680–4. [PubMed] [Google Scholar]
- 21.Wilson EB, Bass CS, Abrameit W. Metoclopramide versus ondasertron in prophylaxis of nausea and vomiting for laparoscopic cholecystectomy. Am J Surg. 2001;181:138–41. doi: 10.1016/s0002-9610(00)00574-2. [DOI] [PubMed] [Google Scholar]
- 22.Bovill JG, Howie MB. Clinical pharmacology for Anesthetists. Philadelphia: WB Saunders; 1999. [Google Scholar]
- 23.Davies NJ, Chashman JN. Lee's synopsis of anaesthesia. 13th Ed. Vol. 3. Oxford: Butterworth-Heineman Elsevier; 2006. pp. 3–352. [Google Scholar]


