Abstract
American Indian and Alaska Native (Native) people experience more traumatic events and are at higher risk for developing posttraumatic stress disorder compared with the general population. We conducted in-depth interviews with six Native healers about their perspectives on traumatic injury and healing. We analyzed the interviews using an inductive approach to identify common themes. We categorized these themes into four categories: causes and consequences of traumatic injury, risk factors, protective factors, and barriers to care. The implications of our study include a need for improving cultural competence among health care and social services personnel working with Native trauma patients. Additional cumulative analyses of Native healers and trauma patients would contribute to a much-needed body of knowledge on improving recovery and promoting healing among Native trauma patients.
Introduction
With more than 560 federally recognized tribes in the US alone, there are more than four million Americans who identify themselves as American Indian or Alaska Native (Native), representing a diversity of languages, locations, traditional practices, indigenous knowledge, and spiritual beliefs.1–3 Despite significant intergroup differences, Native people as a whole are at a greater risk than any other ethnoracial group for experiencing traumatic life events than the general population and are twice as likely to develop posttraumatic stress disorder (PTSD) when compared with the general population.4
Among nearly 3000 injured trauma survivors at 69 hospitals nationwide, Native patients were found to have the highest risk of all racial and ethnic groups for developing symptoms consistent with a diagnosis of PTSD 12 months after injury.5 Similarly, among 269 trauma patients hospitalized at 2 level 1 trauma centers in the Western region of the US, PTSD and related symptoms were significantly more frequent among Native patients than among white patients.6 In the largest epidemiologic survey available regarding Native health, researchers found that two-thirds of the Native populations reported levels of lifetime trauma exposure that were higher than those in the general US population.7 Additionally, trauma from unintentional injury, such as motor vehicle accidents, is experienced at higher rates by North American indigenous populations than by other ethnoracial groups (Dedra Buchwald, MD, personal communication; 2012).a In terms of PTSD, considerable research has been completed with Native populations that confirms the high prevalence of this psychiatric diagnosis among these populations. Although definitive conclusions about PTSD in Native populations are still needed and warrant additional research on trauma-related disorders in Native populations, a focus on the development of culturally appropriate intervention strategies, such as the integration of traditional Indian medicine (TIM) also appears to be warranted.8 TIM is a type of traditional medicine (TM) that is based on indigenous knowledge in the Americas. TM is defined by the World Health Organization (WHO) as “includ[ing] diverse health practices, approaches, knowledge and beliefs incorporating plant, animal and/or mineral based medicines, spiritual therapies, manual techniques and exercises, applied singularly or in combination to maintain well-being, as well as to treat, diagnose or prevent illness.”9
According to WHO, use of TM is common throughout the world in both developed and developing nations. In developed nations, TM is estimated to be used by 30% to 70% of the population, most often involves the use of complementary and alternative medicine therapies such as acupuncture or massage, and is used in conjunction with allopathic medicine (ie, Western medical approaches or biomedicine). In developing nations, TM is estimated to be used by 60% to 80% of the population and often serves as the primary or sole source of health care. Up to 90% of the population in some countries relies on TM for primary health care needs. Although biomedicine is largely replacing TM in many developing nations, a need for a complementary approach is warranted. WHO recognizes the importance of TM around the world in providing health care to vulnerable populations because of its accessibility, affordability, and cultural appropriateness.9 TIM fits within a larger global context of the use of TM in general as sole, primary, or complementary physical, mental, and spiritual health care in both developing and developed nations.
The literature indicates a high prevalence of openness to the use of TIM. In one study of urban Native people, 38% reported that they consulted a Native healer, and 86% of those who did not currently consult a Native healer reported that they were interested in doing so in the future.10 In another study of traditional health practices, 70% of urban Native primary care patients reported that they often participated in traditional health practices, including taking herbal medicine, smudging (a purification practice that involves burning a bundle of dried herbs such as sage), and participating in healing or sweat-lodge ceremonies. Their participation was predicted by strength of cultural affiliation with Native culture.8 In a study of PTSD, depression, and alcohol abuse among 2 tribes, the treatment plan including traditional healers was common in both tribes (Northern Plains and Southwest), particularly the Southwest.11 In a study of Navajo patients, 62% were treated by spiritual interventions from Native healers in the past and 39% reported that their method of treatment included Native healers on a regular basis.12 In a 2000 study, researchers found that urban Native patients participated in TIM simultaneously with biomedical treatments for a variety of physical health problems.8
Integrating traditional Native American healing practices into mainstream treatment interventions is often recommended when working with Native patients13 and could be beneficial to patients.10 For example, aboriginal families receiving clinical care for domestic violence that integrated treatment by traditional healing elders showed significant improvement compared with families who did not participate in the integrated treatment.14
Since the 1990s, indigenous scholars working in mental health among Native communities have called for traditional healing practices to inform (and even transform) conventional psychotherapy.14–17 Mohatt emphasized the need for a practical grounding of indigenous psychotherapy theories in the reality of clinical practice, suggesting that case studies be used as a way to test theory in practice.17 Synthesizing work by Duran15 and Gone,16 Mohatt identified four issues that should be considered when moving from indigenous theory to practice: the need for “critical common elements” to guide the practice, spiritual development among psychotherapists in training, a cross-cultural evaluation model to assess the practice, and recognition that indigenous psychotherapy is not culture-specific but has potential to benefit all patients.
Unfortunately, there is very little published information available to inform clinical interventions with Native patients at risk for developing PTSD (but see Manson18 for an exception). In their 2007 comprehensive review of the literature in mental health treatment, Gone and Alcántara19 discovered a complete absence of literature providing an empirical assessment of mental health outcomes for interventions with Native patients that were based on Native American traditional healing. However, focused studies on small samples and individual cases studies have been completed assessing interventions that combine Western and Native approaches to healing. The results have been promising, indicating that Native approaches to healing for PTSD and related disorders are therapeutic for Native people.20
Background
From 2009 to 2010, we built on the foundation of the Trauma Survivors Outcomes and Support (TSOS II) study21 to develop Staying Connected: A Feasibility Study Linking American Indian and Alaska Native Trauma Survivors to Their Tribal Communities. This study was designed to provide Native trauma patients treated at the region's level 1 trauma center with compassionate and culturally sensitive care and to link them to their distant tribal communities. The specific parts of that project were: 1) to interview Native healers to gather information on the culture-specific aspects of recovery from traumatic injury and 2) to conduct a randomized, controlled trial to evaluate the implementation and feasibility of the intervention.
In this article, we discuss the results of the first part of that study, to elucidate Native culture-specific aspects of recovery from traumatic injury. Results from the second part are described elsewhere.22 We thus interviewed six Native healers to gain an understanding of the effects of traumatic injury on Native patients, what barriers they may encounter, how to approach patients, and how to provide culturally tailored care.
The aims of this study were to address the following questions:
How do some Native healers conceptualize the causes and consequences of traumatic injury?
How can help-seeking behavior be encouraged among Native patients at risk of developing PTSD?
What can improve outcomes for Native patients?
Methods
Data Collection
We investigated traumatic injury, with particular emphasis on the nature and extent of the thoughts, feelings, and behaviors that often accompany such injury (eg, PTSD). Research study staff were trained to conduct semistructured interviews.
Analytic Methods
The method of data analysis used in our study is based on an approach described by Briggs23 in which each interview is considered on its own terms in order to understand what a participant meant by the answers s/he gave during an interview, rather than decontextualizing answers from their original context. We used a grounded theory approach to code and to compare the interview data.24 We read through each transcript in its entirety a minimum of five times, categorizing the interviewee's responses into similar categories. We reviewed the transcripts independently and then jointly reviewed the categories for consensus. We wrote theoretical memoranda throughout our analysis to make connections within the data and propose explanations for the findings.
We strove to follow the protocol of an indigenous methodology, particularly by being mindful of respect, reciprocity, and responsibility.25 We had regular discussions among ourselves throughout the project to discuss how to relate respectfully to the participants, to give back to the communities that we were studying, and to fulfill our roles and obligations as researchers responsibly. These discussions were an important aspect of our methodology. One way we addressed our indigenous research goals was by giving our participants the opportunity to read and to comment on our findings from their interviews before we completed our study.
Participants
We identified a purposeful, rather than random, sample of Native healers through our personal networks and referrals. Healers were identified as such on the basis of their recognition as healers within their communities as well as across Native communities. We invited the healers to participate in the interviews through e-mail or by telephone. At least one of us met each of the six healers in person on one or more occasions. Ultimately, we interviewed six Native healers using a semistructured interview (see Sidebar: Native Healer Interview Guide: Traumatic Injury, Its Consequences and Treatment) in person or over the telephone. Two study staff members were present during the interviews; one person conducted the interview while the other person took notes. The duration of interviews ranged between 60 and 120 minutes. With permission, the discussion was recorded and later transcribed verbatim. All participants were between the ages of 45 and 75 years. Five men and one woman were interviewed. All participants are affiliated with Native communities in the US; however, to preserve participant confidentiality, we have not identified here the specific communities with which they are affiliated. Each interview participant received $50 as compensation for their time.
Native Healer Interview Guide: Traumatic Injury, Its Consequences and Treatment.
This interview script is intended as a guide for use with Native healers. Its focus is on the experience of traumatic injury, with emphasis on the nature and extent of the thoughts, feelings, and behaviors that accompany such injury. As the interview progresses, follow-up questions may be asked on any of the topics discussed. Participants may decline to answer questions that make them feel uncomfortable.
Thanks again for agreeing to participate in this interview. As we talked about before, I am audiotaping and then will transcribe our conversation so we may have a record of exactly what was said. I won't put your name on the transcript, and we won't use your name in conjunction with any quotes I may use. I am very interested in learning how people react to traumatic injuries; the thoughts, feelings, and behaviors that are experienced as a result of such injuries; and the services needed to treat the problems that arise. Our goal is to develop better, more effective ways of caring for American Indian and Alaska Native people who suffer traumatic injuries. Any questions? Let's begin.
What comes to mind when I say the phrase traumatic injury? What does it mean to you?
What kinds of events can cause traumatic injury?
What are some of the consequences of traumatic injury?
How often do people in your community experience traumatic injury?
Is it a common occurrence?
How concerned are you and members of your community about traumatic injury?
What thoughts, feelings, and behaviors can result from traumatic injury?
Why do people experience these thoughts, feelings, or behaviors?
Some people who suffer traumatic injury don't experience these thoughts, feelings, or behaviors. Why not?
How can such thoughts, feelings, or behaviors affect people's lives?
Have you ever heard someone refer to these thoughts, feelings, or behaviors in a particular way?
Who and what can help people deal with the thoughts, feelings, or behaviors they may experience as the result of traumatic injury?
To what extent are these sources of help available in your community?
How likely are people who experience these thoughts, feelings, or behaviors to seek help for dealing with them?
What can keep people from seeking help? What can encourage people to seek help?
Before we close, do you have any additional comments to share about the topic of traumatic injury?
Thank you for sharing your views with me. Do you have any more questions about the project and its goals?
Results
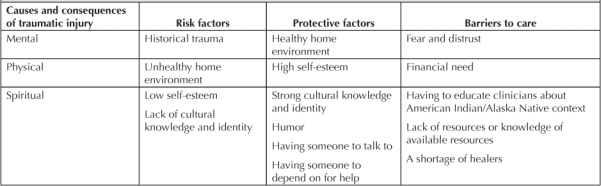
The materials we analyzed included six fully transcribed interviews with Native healers. We ultimately identified four overarching categories of responses: causes and consequences of traumatic injury, risk factors, protective factors, and barriers to care (Table 1). In what follows, we discuss each set of findings that pertain to the four categories and present quotations from the healers to illustrate our findings. To preserve confidentiality for the healers we interviewed, we refer to them simply as Healer 1, Healer 2, and so on.
Table 1.
Themes derived from interviews with American Indian and Alaska Native healers
Causes and Consequences of Trauma
One of the first questions we asked the healers concerned what traumatic injury meant to them. From their answers, we identified three related themes we subsumed under the category of “causes and consequences of trauma.” Healer 5 explained that physical traumatic injury was caused by imbalance of three main domains: mental, physical, and spiritual. The lack of spiritual harmony, he emphasized, contributes to longer recovery from traumatic injury:
Traumatic injury is like three main things that I see people go through—that I've been taught. It's not just the physical, which is what I feel a lot of non-Native cultures see. … and they're just now coming around to mental injuries. … but the main thing that they don't have a clue about—a lot of them—is spiritual harmony. That's the main one. And if you don't have those in balance, if you don't check them, it takes a person longer to recover from a physical injury like a car accident.
Healer 4 gave a few examples of serious injuries that could affect people physically, mentally, and spiritually:
It could be like a car accident. It could even be a snakebite or a spider bite … or maybe an overdose on drugs, or gunshot wound, knife wound, could even be poisonous snakebite or got beat up really bad.
Healer 6 talked about military trauma as a cause of PTSD, describing it as an amplification of preexisting trauma:
Of course military trauma rarely is ever all by itself. There's usually preexisting childhood conditions that happen that have been traumatic, and the military trauma that is experienced tends to amplify the preexisting trauma. And making it more complicated, of course, we have alcohol and drugs and just ongoing violence in our society that continues to amplify military trauma. It's very confusing.
In this response, Healer 1 discussed different types of traumas that can be categorized as physical or mental:
I would have to say probably over half of our population experiences [trauma] regularly, in many different forms. It could be that we're being targeted driving down the street by the police or—I've been stopped, you know. It's also not only domestic violence but also injuries on the work site. And it also can be very clever. The way that someone says something. It's the tone of the voice. If a person has more power than you in the workplace, especially if it's male, we're considered third-class citizens.
When asked “What are some consequences of traumatic injury?” the healers again talked about the interrelated mental, physical, and spiritual consequences. Healer 5 said that Native people are more spiritual than other people and that after experiencing a loss or going through a traumatic event, they may develop PTSD or turn to substance abuse to ease their pain if they do not understand what is happening to them:
And all of a sudden these memories get flooded into your mind and if you don't have that balanced out with your spirituality, then people don't understand why they act out. The expression ‘act out’—they don't know how to act. Some people, you know, they do what they know. They drink. … Native people are very spiritual. That's a gift that the Creator gave us versus other people. There are people who don't know that about themselves and they've never been part of—or they've never grown up with their culture, [and] they've never had guidance from elders. They're the ones who are left behind when someone loved passes on. They're still spiritual but they don't understand what they're going through.
Native people are very spiritual … [some] don't know that about themselves and [have] never been part of … their culture, … never had guidance from elders.
Healer 5, who helps plan ceremonies that address the impact of different types of traumatic events, including combat experience and bereavement, said that the purpose of the ceremonies is to help people understand what they see and feel and learn a healthy response to the traumatic event they've experienced.
Healer 4 talked about the relationship of spiritual trauma to physical trauma:
… Even the doctors and the nurses and the people at a hospital can see the physical impact—the force of the physical impact—let's say if a person got hit real hard by a fist or a pipe or a car or anything else like that. It leaves a physical mark—ie, the bruise, the blood clot, the discoloration, and everything like that. But they don't see the spiritual side, the psychological or the energy impact. They can see the [physical] impact. There's energy behind every trauma. There's energy that's involved in it. So that energy can be seen physically, but it's very difficult to see it spiritually. We use the term spiritually, or even psychologically, on a person's mind and brain, which in turn affects their personality.
In a study of Vietnam veterans, Hopi men who had been initiated into the highest order of Hopi secret religious societies had the lowest scores on any measure of PTSD.26 Healer 6 told of his return from Vietnam, his high level of PTSD, and “hearing things in the sky and hearing sounds and having visions of campfires in the hills and hearing voices at night—people talking to you.” He went to a non-Native counselor, who encouraged him to develop his cultural identity, telling him, “You're struggling with yourself, with your identity, with what you are,” and assured him, “You're not crazy.” This advice and assurance was a turning point for Healer 6, who began to seek out TIM treatment for PTSD, which ultimately proved effective for him. Speaking of Native combat veterans with PTSD, Healer 6 said:
That's a group in a different way: We seem to recognize it as a breaking of our spirit—part of our spirit was missing and that we had to get our spirit back—somehow find its way back to us till we could become whole again. We felt kind of empty inside.
Regarding causes and consequences of all types of trauma, the healers all stressed the importance of maintaining harmony that will restore balance in all areas of the patient's life: the physical, spiritual, and mental. This finding is consistent with findings in similar studies of Native healers.27–29
Risk Factors
With respect to risk factors, historical trauma, not knowing one's culture or language, not having a connection to elders, and growing up in an unhealthy home environment all contribute to Native traumatic injury response. In relation to those contextual factors, Healer 5 said:
When I see a physical injury in people—there are a lot of things that cause that, okay? The doctors don't see that point of view. And what I'm getting at is a lot of our people, because they come from broken homes, because they lost a lot of their culture, because of dysfunctional homes—there's more to it than a broken arm.
Similarly, Healer 1 cited low self-esteem based on a history of racist beliefs by society as a risk factor for developing PTSD:
Well, some of it is, I think, based on low self-esteem because if you believe the system—that the only good Indian is a dead Indianb—then you're going to spend your life trying to please. I think that's part of the reason why we have such a high rate of suicide.
Historical trauma is highly relevant to any discussion of trauma in Native populations and provides an important explanatory model that is commonly used when talking about high rates of present-day traumatic injury and PTSD among Native populations.20 Briefly, historical trauma originated in the aftermath of the Jewish Holocaust and refers to the survivors and their subsequent generations. Applied to the Native American experience, the term refers to the colonization of indigenous communities and subsequent experiences of subjugation and abuse, including coercive assimilation through boarding schools (the experience of which often included physical, sexual, and emotional abuse). Historical trauma also refers to the theft of land; the forced removal and relocation of families and communities; and cultural genocide, including loss of Native language, cultural practices, social structures, and spiritual beliefs and practices.20
Brave Heart and DeBruyn30 suggested that the first generation of survivors of genocide had PTSD symptoms that might have included depression, hypervigilance, anxiety, and substance abuse. As cultural genocide also took place, Native people were not allowed to practice their traditional rituals of mourning and healing, which included phases of grief that would have provided adjustment to their loss, ceremonial and ritual mourning, and family and community support. Brave Heart and DeBruyn stated that “Disenfranchised grief results in an intensification of normative emotional reactions such as anger, guilt, sadness, and helplessness.”30 This unresolved grief is a result of historical trauma that is transmitted down through each Native generation and is cumulative and compounded as more traumatic events occur.
Healer 1 explicitly cited historical trauma as a reason for traumatic injury among Native people:
… Well, actually trauma also—not just trauma injury—also in my mind also means historical trauma, which is 500 years of intergenerational oppression from the dominant culture. And so it looks like—historical, emotional, physical, cultural.
Individual characteristics such as strength of tribal affiliation, knowledge of culture, and family of origin were cited by Healer 4 as determining how someone would react to a traumatic injury:
… People are—they're individuals. They could be full blood. They could be half-breed. They could be another heritage and culture and language. They might not know anything at all. I mean it—all of that's going to affect their thoughts and feelings and their behavior. You know, if they grew up in dysfunctional families—for example, alcohol and drugs, a lot of abuse, physical and verbal abuse—a lot of that's going to affect their—a lot of that will start surfacing and coming up from an accident—a car accident, injury, gunshot wound, or a stab.
Protective Factors
In terms of protective factors, studies of Native patients indicate that cultural identity is an important aspect.20,31 In a case study of a combat veteran with PTSD, themes important to Native experiences of trauma included boarding-school abuse, the interruption of cultural identity formation, and lifelong experiences of racism.31 Key elements of this patient's recovery were active involvement with his Native culture, which instilled in him a sense of Native pride; preparation for and participation in traditional ceremonies; and having the support of his family and tribal community. Our analysis of the interviews with the healers showed cultural identity to be a primary protective factor. Culture is an ever-evolving process for indigenous people that is based on traditional values and helps to establish an identity and a sense of belonging in the world; describes the origin of a people through an oral tradition of legends, songs, and stories; and defines people's understanding of why things happen and what they can do to make changes.32
Healer 5 gave some examples of positive outcomes of physical injury, one for people who know their culture and one for those who do not. Of those who know their culture, Healer 5 said:
… People visit him. … We take him to the longhouse, and he gets to do the songs every Sunday. …He's going to learn more about his culture. … Maybe this person will learn their language a little more because this person is going to listen … learn to respect your elders and listen. … When you're spiritual, you listen to your inside, you listen to who's there. You can understand that it would be good to have the Creator there. That's huge. That's a big difference … you learn how to listen to your body a whole lot more. Your spirituality goes up a notch when you get hurt. It goes up. They get stronger.
Of those who do not know their culture, Healer 5 said that they can still experience positive outcomes related to their physical injury:
… The person—the other guy—has negative thoughts … when a person who doesn't have his culture, who's not hooked up spiritually and is Native, that's the positive thing that can help him is he learns to accept no … and whether he learns to accept no in a healthy way, that depends on who's around him … people that are there even if they're from another tribe … you get closer to God. You get closer to the Creator. … It's called vision. You learn to see past tomorrow. That's the thing that I feel happens to both kinds of people [ie, those who know their culture and those who don't]. You have vision … so now their vision [provided by knowing their culture] helps them see past their emotions, helps them see past their pain or their sadness, and they accept it.
Thus, according to Healer 5, although both types of trauma survivors can potentially experience positive outcomes from their trauma, those who know their culture will benefit more quickly than those who do not. For both types of survivors, however, culture is indeed viewed as medicine for trauma patients, regardless of the strength of their cultural identity.
The theme of culture as medicine that Healer 5 explicitly articulated and that the other five healers we interviewed described is one that appears repeatedly in the literature on Native healers. In a study of four Native women healers, the healers talked about indigenous healing occurring within a cultural context of Native traditions, values, and knowledge.27 In a similar study with four Native men healers, the healers described culture as interwoven with healing.33
Healer 5 described knowing one's language and culture both as a “spiritual support” and as “medicine” for the patient:
In the city, in Western medicine, the best part of their environment is pharmacy. And you're giving that kind of medicine to people who are used to getting their medicine from somewhere else. It's not all there. They need that spiritual support. … You're talking, our culture is medicine. Our Creator doesn't make mistakes. That's sort of the basic thing I teach people who don't know their culture who want to know “Why should I learn it?” I tell them—I ask them first, “Do you believe in God? Do you believe in the Creator?” Yeah, I do. “You think He makes mistakes or She makes mistakes?” No, He doesn't make mistakes. I go, “He gave you your culture, right? Where do you think that culture came from?” It came from God, okay, so when you don't have it, that culture is medicine to you.
… it was a traditional healing. … It reached deep into my soul and just made me feel real. … This is from the old people. They've come back to help, to talk, to be with, to share.
Indigenous therapeutic interventions usually involve an individual's family and community, and healing occurs within the context of the community as a whole. The healed person is able to then help the community. Thus, curing an individual is important to the community because it strengthens all members.34 In his interviews with traditional healing elders in North America, Mehl-Madrona found that the elders identified the importance of the community in the healing of an individual.35
Healer 6 told us that it was only after he turned to his Indian culture that he was able to make peace with his own PTSD, which he developed after his military combat experience. By reaching out to his community for healing, he was able to pass on those traditional values through singing and drumming for Indian men who have lost hope in the prisons he visits:
And sometime in the eyes—or most of the time in the eyes—of the people that I talk to in prison or, say, [in the prison sweat-lodge ceremony], I see that fear of being alone, being trapped. Everything is gone. You know, no family, no friends. They're just in trouble now. They don't know if they'll ever get out. There's no sense of future. Teaching the traditions and songs and the drum seem to help people like that a great deal.
In the following excerpt in which Healer 6 described a healing ceremony for combat veterans, the elements of cultural identity, having someone to talk to, and humor are all present:
You know, it was a traditional healing. … It reached deep into my soul and just made me feel real. And, I mean, this is real. This is from the old people, you know. They've come back to help, to talk, to be with, to share, you know. Even to laugh a little bit. It was just incredible.
Healer 2 told a story from his past when he was down on his luck and had received an injury. He was treated at the hospital, but he did not know how he would pay for his treatment when the time came to release him. He called his boss, and his boss paid for everything. He remarked on the importance of knowing that “someone is there for you” when coping with the aftermath of a traumatic event.
Barriers to Care
We asked the six healers what they thought kept people from seeking help after experiencing PTSD. According to these six healers, patients will not seek help because of the following five barriers: fear and distrust, financial need, having to educate clinicians about Native context, lack of resources or lack of knowledge of available resources, and a shortage of healers. The following responses from the interviewees illustrate the barrier of fear and distrust.
Healer 2 said:
They tend to shy away from any people like yourself, and the reason they do that is that they don't want no one else to know about their problems.
Healer 1 said:
It's all complicated, and so that—so often people are afraid to go for help because they're afraid whatever they share is going to be used against them. … I mean, you don't really know who you can trust. And so if you've been raised with the people who historically don't trust the very agencies that are supposed to be helping you, where do you go?
Indeed, Gone suggested that Native preference for traditional healers might be a result of distrust of European-American institutions, which have a history of participating in the oppression of indigenous people in North America.36
Many patients need help addressing their basic needs, such as food, shelter, and transportation, and these needs must be dealt with before other, more complex psychological issues can be adequately addressed. Healer 2 said:
[A lot of patients] really don't get any help after they leave the hospital because they are on assistance or unable to pay for their help from the hospital. And this causes them a lot of distress.
In their study of Native healers, Struthers et al emphasized the need for Western clinicians to learn about basic cultural beliefs of indigenous patients in order to provide the integrated care that those patients need.33
Healer 1 described a unique barrier to help-seeking that she personally experienced as having “to teach while I'm going through my trauma”:
So I went to a couple of places personally, and they ended up being wonderful, but they were non-Native, and I had to really educate them as I was going through my trauma. So I can't really just express my trauma. I have to teach while I'm going through my trauma, which is really heavy. It's more burdensome.
Healers also noted that a lack of resources knowledge about Native patients posed barriers within more conventional medical models. The interviews indicated that some Native patients are unsure of where to initially go for medical assistance. Healer 2 said:
I'm not too sure what [trauma survivors] do to deal with [mental health needs], because they don't know where to turn and who to ask.
Healer 3 said:
I've been away from [a particular city] for a long time, so I'm not sure what [has] been going on there, but when I was there, there wasn't a lot. I mean, people go to [the city] to the Native hospital there to get some help. But they don't stay at [the city]. And then they have to come back to [the city] after they've been in the hospital, but there's no follow-up.
Although many patients are unaware of available resources, Healer 3 said that there were a lot of resources accessible to people in the complimentary and alternative medicine realm:
I don't know if a lot of people are aware of what's available. There's a lot of resources here, but people may not be aware of it. I mean alternative-medicine-wise, and complementary medicine can assist people with traumatic experiences.
In terms of needing more healers, Healer 4 said:
I've been saying it for years. We need more medicine people. We need more Native healers … male and female.
Discussion
Our analysis of interviews of Native healers provides rich insight into the perspectives of these healers and in turn provides guidance for developing more adequate and appropriate treatment plans for trauma patients from North American indigenous populations. After soliciting their perspectives on the causes and consequences of traumatic injury, we asked the six healers if they had any advice on how to approach Native trauma patients and encourage help-seeking.
Healer 1 had the following simple advice: “Offer, offer, offer. Over and over again,” adding:
You know, when I'm under these circumstances and I don't know where my next meal is coming from, I don't know how you can help. I don't even know what kind of help I'm going to need. You know, sometimes it's just talking. Sometimes it's a need to cry or vent. It depends. I might need a ride, or I might be afraid.
Similarly, Healer 2 said:
Well, just make sure that you're there to help and not ask any questions. And that if they have any questions themselves—just make sure that if they have any questions … that you're willing to answer them.
In terms of encouraging help-seeking among trauma patients, Healer 5 said:
The main thing is, it's a real simple word. It's trust. They gotta have trust. … If they don't have family or they don't have people that look like family walking around, it's hard for them to have trust.
Healer 5 went on to give practical examples of how trust could be developed in a hospital setting, based on his own experience in his tribe, to indicate to patients that the clinicians know something about their specific culture. These examples included physicians covering their stethoscopes with beads, wearing a turquoise ring, or putting Native art on the walls of the hospital and patient rooms. He explained why these visible symbols of inclusion were so important to Native patients and their families:
You know, one little thing when they walk in—and the parents who are coming to see their kids, and these people who are coming from [a remote region] to [a large urban hospital]—they walk in there and they see something about Native people, right in the lobby. All of a sudden … they can think clearly. Because the hardest thing—one of the harder things for people being hurt is that people have to watch it—people who love them. So if you make that easier for them—and sometimes it's as simple as putting a display case as you walk into the hospital—they would see it. The things that I'm explaining to you are the same things that everybody else has and … they take it for granted. … So for us to walk into a place—it's like walking into a foreign country. So if we saw something from us like what they take for granted, all of a sudden we would have a better chance of being more positive.
Healer 5 said it was important for hospitals to have a list of Native healers that Native patients and families could contact if they wanted to do so. In terms of educating hospital staff, Healer 4 said:
[Hospital staff] need staff training. When I was out in Billings, Montana, I came out and I did some staff training for the hospitals with the doctors and the nurses and those that were in the medical profession and the medical role, and I talked to them about traditional Native healing concepts and practices and approaches to healing and the different kinds of medicine people that there were.
Healer 4 also talked about the importance of educating both hospital staff and Native people about the value of Native healing:
You know, it all depends on who's the director. If you've got white people managing Indian health clinics and they have the Western, conventional orthodox view, with no cultural base or understanding or need for a cultural-based approach, they're not going to do it. And the same thing even with Native people. Native people weren't really raised in the Native way. They can be totally assimilated before—totally assimilated and Christianized and all that and don't believe in it or don't see the value of it. They have no knowledge about it, so once again, a lot of our Native people have to be educated themselves.
As discussed earlier, Mohatt17 identified spiritual development as one of the key issues in training a new generation of indigenous psychotherapists who can bring traditional healing to clinical practice in Native communities. Similarly, in his interviews with traditional healing elders, Mehl-Madrona35 reported that “spiritual healing” was one of the most important points elders identified for mental health clinicians to consider when working with Native patients. Because spirituality is such a central part of medicine and healing in Native communities, an indigenous approach to mental health care would require that the clinicians be spiritually developed themselves.
Although spiritual development may seem like a daunting task to clinicians trained in biomedicine, Shore et al offered some guidelines for psychiatrists who want to collaborate with Native healers.37 Their recommendations included that clinicians take the initiative in educating themselves about the Native community they are serving both in terms of general cultural knowledge and in the particular healing practices relevant to the given community; that they actively seek opportunities for collaboration within the community; and that they develop relationships with healers in the community. One way to accomplish these goals would be to study under a traditional healer. For example, one of the healers we interviewed provides mentorship for Native physicians interested in learning about TIM.
According to the healers we interviewed, culture is the primary vehicle for delivering healing. The overarching principle articulated here, that “culture is medicine,” means that connecting with one's culture has both protective and therapeutic value, promoting both resilience to and recovery from traumatic events. The details of treatment will differ depending on the cultural specifics related to one's culture; however, the principle of culture as medicine is the same across Native cultures, according to the healers we interviewed. Thus, indigenous means of treatment through culture may include any or all of the following: language, traditional foods, ceremonies, traditional values, spiritual beliefs, history, stories, songs, traditional plants, and canoe journeys. Connecting Native patients with their Native culture promotes better health outcomes.14,35
Our findings are based on interviews we completed with six Native healers and are not intended to represent or speak for all Native people, who represent a diversity of cultures, languages, and beliefs. Our aim in this project was to inform the development of a care-management intervention with Native trauma patients to be implemented at a level 1 trauma center. Although it is beyond the scope of this article to discuss the outcome of that intervention, the insight we received from the healers we interviewed was crucial to developing a culturally tailored intervention with Native trauma patients.22 Although the cultural particulars of our findings may differ among Native populations (and we expect that they will), the overall emphasis on culture as medicine is one that we suggest is transferable across Native populations.
One important practical suggestion that was made repeatedly was to provide Native cultural training for hospital staff. … that introduces [them] to main concepts of Native health.
Our analysis contributes to a much-needed body of research on indigenous perspectives on health. Our study differs from similar studies that have been done in at least two important ways. First, we conducted interviews with healers from six tribes across North America rather than with healers who all represented the same tribe. Second, the focus of our interviews was traumatic injury, a focus we have not encountered in our reviews of the literature. Given the high prevalence of traumatic injury and PTSD among Native populations, future studies with this focus are warranted.
Practically speaking, the information presented here may prove useful to clinicians seeking culturally informed interventions for treating Native patients, particularly in trauma settings, but also in the settings of substance abuse, counseling, and general medicine. We have presented here many of the practical suggestions that the healers shared with us in the interviews. One important practical suggestion that was made repeatedly was to provide Native cultural training for hospital staff. Our experiences as researchers working at a level 1 trauma center has been that hospital staff are interested in learning more culturally informed ways of treating their Native patients. Periodic workshops could be held as part of an ongoing lecture series that introduces hospital staff to main concepts of Native health. Many of the healers we interviewed generously offered to give presentations to hospital staff on their work.
Conclusions
Through an in-depth interview process, our study identified important culture-specific themes that relate to the treatment of Native patients within the setting of trauma medicine. Limitations in this research design exist, and we acknowledge those here. We initially opted to employ an interview guide (included in the Sidebar: Native Healer Interview Guide: Traumatic Injury, Its Consequences and Treatment) that had been used effectively in other studies assessing PTSD in Native populations. However, the interview guide was less effective than we hoped as an interview instrument with the healers we interviewed, all of whom were more comfortable with the genre of storytelling as interview rather than with a question-and-answer format. We noticed this preference after completing three of the interviews and turned to a more open, free-flowing format for the remaining three interviews, in which we used the interview guide at the start of the interview, allowing the healers to talk freely without leading them back to specific questions. We found this approach effective for two reasons: 1) uninterrupted, the healers shared more insight with us than they did when they were trying to directly address our specific questions, and 2) as they told stories of their experiences in healing, they actually answered all of our questions without being directly asked. Thus, we recommend the use of an interview guide as simply an opener when working with Native healers, recognizing the cultural importance (and appropriateness) of the storytelling tradition among indigenous populations, particularly elders.
Another possible limitation of our study is that the six healers we interviewed represented different tribes and nations, rather than one group; similar studies with healers have involved healers from one group.33 However, the six interviews we conducted contained common themes around TIM and recovery from traumatic injury that suggest a unified perspective regarding healing in North American indigenous populations, irrespective of the specific means used (eg, eagle feathers, sweat-lodge ceremonies, prayer, singing). Additionally, because our population of interest is a diverse Native population seen at a level 1 trauma center that serves a five-state region, we were interested in identifying what common healing strategies could be applied across Native populations.
The interview data obtained here are rich in their descriptive and interpretive elements related to improving recovery for Native trauma patients. Additional ethnographic and qualitative work is needed to provide a more complete understanding of the role of TIM in Native wellness. In particular, ethnographic research with Native communities is needed to inform the development of effective diagnostic measures and mental health interventions for clinical practice.18 Future analyses will help generate a fuller understanding of the terms and concepts presented here. Cumulative analyses of indigenous healers' perspectives on health and wellness in indigenous populations are urgently needed to address the health disparities in Native populations. Future research might focus on specific health concerns that are experienced excessively across all Native populations, such as diabetes and cancer, and elicit Native healer perspectives on preventing and treating these diseases.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
We thank the six healers we interviewed; Doug Zatzick, MD, (University of Washington), Dedra Buchwald, MD, (University of Washington), Spero Manson, PhD, (University of Colorado), Georgia Galvin, and Kate Murray for their invaluable contributions to this study.
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
Footnotes
a Dedra Buchwald, MD. Department of Medicine, University of Washington, Seattle, WA 98101. Unpublished paper: Unintentional injury among the indigenous people of the US and Canada: a review of the literature.
b This phrase appears to have originated in a speech given by James Michael Cavanaugh, a Montana congressman, during a debate in 1868. It became a stereotype used as a racial slur against Native people in North America (Mieder W. “The only good Indian is a dead Indian”: History and meaning of a proverbial stereotype. Journal of American Folklore 1993;106[419]:38–60).
References
- Washington, DC: US Census Bureau; 2001. 2000 Census of population and housing, summary file 1 [monograph on the Internet] [cited 2012 Jan 22]. Available from: www.census.gov/prod/cen2000/doc/sf1.pdf. [Google Scholar]
- Washington, DC: US Census Bureau; 2001. 2000 Census of population and housing, summary file 2 [monograph on the Internet] [cited 2012 Jan 22]. Available from: www.census.gov/prod/cen2000/doc/sf2.pdf. [Google Scholar]
- Ogunwole S. Washington, DC: United States Census Bureau; 2006 Feb. We the people: American Indians and Alaska Natives in the United States. Census 2000 Special Reports [monograph on the Internet] [cited 2012 Jan 31]. Available from: www.bia.gov/idc/groups/public/documents/text/idc-001819.pdf. [Google Scholar]
- Washington, DC: Bureau of Justice Statistics; 2000. Sourcebook of criminal justice statistics, 1999. Available from: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1451. [Google Scholar]
- Zatzick DF, Roy-Byrne P, Russo JE, et al. Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial. Gen Hosp Psychiatry. 2001 May–Jun;23(3):114–23. doi: 10.1016/s0163-8343(01)00140-2. [DOI] [PubMed] [Google Scholar]
- Santos MR, Russo J, Aisenberg G, Uehara E, Ghesquiere A, Zatzick DF. Ethnic/racial diversity and posttraumatic distress in the acute care medical setting. Psychiatry. 2008 Fall;71(3):234–45. doi: 10.1521/psyc.2008.71.3.234. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD. Social epidemiology of trauma among 2 American Indian reservation populations. Am J Public Health. 2005 May;95(5):851–9. doi: 10.2105/AJPH.2004.054171. AI-SUPERPFP Team. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchwald D, Beals J, Manson SM. Use of traditional health practices among Native Americans in a primary care setting. Med Care. 2000 Dec;38(12):1191–9. doi: 10.1097/00005650-200012000-00006. [DOI] [PubMed] [Google Scholar]
- Geneva: World Health Organization: WHO Policy Perspectives on Medicines; 2002 May. Traditional medicine: growing needs and potential, No. 2 [monograph on the Internet] pp. 1–6. [cited 2012 Jan 22]. p. Available from: http://whqlibdoc.who.int/hq/2002/WHO_EDM_2002.4.pdf. [Google Scholar]
- Marbella A, Harris MC, Diehr S, Ignace G, Ignace G. Use of Native American healers among Native American patients in an urban Native American health center. Arch Fam Med. 1998 Mar–Apr;7(2):182–5. doi: 10.1001/archfami.7.2.182. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, et al. Prevalence of major depressive episode in two American Indian reservation populations: unexpected findings with a structured interview. Am J Psychiatry. 2005 Sep;162(9):1713–22. doi: 10.1176/appi.ajp.162.9.1713. [DOI] [PubMed] [Google Scholar]
- Kim C, Kwok YS. Navajo use of native healers. Arch Intern Med. 1998 Nov 9;158(20):2245–9. doi: 10.1001/archinte.158.20.2245. [DOI] [PubMed] [Google Scholar]
- Scurfield RM. Healing the warrior: admission of two American Indian war-veteran cohort groups to a specialized inpatient PTSD unit. Am Indian Alsk Native Ment Health Res. 1995;6(3):1–22. doi: 10.5820/aian.0603.1995.1. [DOI] [PubMed] [Google Scholar]
- Puchala C, Paul S, Kennedy C, Mehl-Madrona L. Using traditional spirituality to reduce domestic violence within aboriginal communities. J Altern Complement Med. 2010 Jan;16(1):89–96. doi: 10.1089/acm.2009.0213. [DOI] [PubMed] [Google Scholar]
- Duran E. New York: Teachers College Press; 2006. Healing the soul wound: counseling with American Indians and other native peoples. [Google Scholar]
- Gone JP. Psychotherapy and traditional healing for American Indians: exploring the prospects for therapeutic integration. Counseling Psychologist. 2010;38(2):166–235. [Google Scholar]
- Mohatt GV. Moving toward an indigenous psychotherapy. Counseling Psychologist. 2010;38(2):236–42. [Google Scholar]
- Manson SM. Ethnographic methods, cultural context, and mental illness: bridging different ways of knowing and experience. Ethos. 1997;25(2):249–58. [Google Scholar]
- Gone JP, Alcántara C. Identifying effective mental health interventions for American Indians and Alaska Natives: a review of the literature. Cultur Divers Ethnic Minor Psychol. 2007 Oct;13(4):356–63. doi: 10.1037/1099-9809.13.4.356. [DOI] [PubMed] [Google Scholar]
- Gone JP. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol. 2009 Aug;77(4):751–62. doi: 10.1037/a0015390. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Roy-Byrne P, Russo JE, et al. Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial. Gen Hosp Psychiatry. 2001 May–Jun;23(3):114–23. doi: 10.1016/s0163-8343(01)00140-2. [DOI] [PubMed] [Google Scholar]
- Tsosie U, Nannauck S, Buchwald D, et al. Staying connected: a feasibility study linking American Indian and Alaska Native trauma survivors to their tribal communities. Psychiatry. 2011 Winter;74(4):349–61. doi: 10.1521/psyc.2011.74.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs C. New York: Cambridge University Press; 1986. Learning how to ask: a sociolinguistic appraisal of the role of the interview in social science research. [Google Scholar]
- Glaser B, Strauss A. Chicago: Aldine Transaction; 1967. The discovery of grounded theory: strategies for qualitative research. [Google Scholar]
- Wilson S. Blackpoint, Nova Scotia: Fernwood Publishing Ltd; 2008. Research is ceremony: indigenous research methods. [Google Scholar]
- Villanueva M. Posttraumatic stress disorder, alcohol, and tribes: obstacles to research. Alcohol Clin Exp Res. 2003 Aug;27(8):1374–80. doi: 10.1097/01.ALC.0000080163.54436.3F. [DOI] [PubMed] [Google Scholar]
- Struthers R. The lived experience of Ojibwa and Cree women healers. J Holist Nurs. 2000 Sep;18(3):261–79. doi: 10.1177/089801010001800307. [DOI] [PubMed] [Google Scholar]
- Struthers R. The artistry and ability of traditional women healers. Health Care Women Int. 2003 Apr;24(4):340–54. doi: 10.1080/07399330390191706. [DOI] [PubMed] [Google Scholar]
- Struthers R, Eschiti V. Being healed by an indigenous traditional healer: sacred healing stories of Native Americans. Part II. Complement Ther Clin Pract. 2005 May;11(2):78–86. doi: 10.1016/j.ctnm.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Brave Heart MY, DeBruyn LM. The American Indian Holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res. 1998;8(2):56–78. [PubMed] [Google Scholar]
- Manson SM. The wounded spirit: a cultural formulation of post-traumatic stress disorder. Cult Med Psychiatry. 1996 Dec;20(4):489–98. doi: 10.1007/BF00117089. [DOI] [PubMed] [Google Scholar]
- Green BL. Culture is treatment: considering pedagogy in the care of Aboriginal people. J Psychosoc Nurs Ment Health Serv. 2010 Jul;48(7):27–34. doi: 10.3928/02793695-20100504-04. [DOI] [PubMed] [Google Scholar]
- Struthers R, Eschiti V, Patchell B. The experience of being an Anishinabe man healer: ancient healing in a modern world. J Cult Divers. 2008 Summer;15(2):70–5. [PubMed] [Google Scholar]
- LaFromboise TD, Trimble JE, Mohatt GV. The counseling intervention and American Indian tradition: an integrative approach. Counseling Psychologist. 1990;18(4):628–54. [Google Scholar]
- Mehl-Madrona L. What traditional indigenous elders say about cross-cultural mental health training. Explore (NY) 2009 Jan–Feb;5(1):20–9. doi: 10.1016/j.explore.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Gone JP. “We never was happy living like a Whiteman” : mental health disparities and the postcolonial predicament in American Indian communities. Am J Community Psychol. 2007 Dec;40(3–4):290–300. doi: 10.1007/s10464-007-9136-x. [DOI] [PubMed] [Google Scholar]
- Shore JH, Orton H, Manson SM. Trauma-related nightmares among American Indian veterans: views from the dream catcher. Am Indian Alsk Native Ment Health Res. 2009;16(1):25–38. doi: 10.5820/aian.1601.2009.25. [DOI] [PubMed] [Google Scholar]


