Abstract
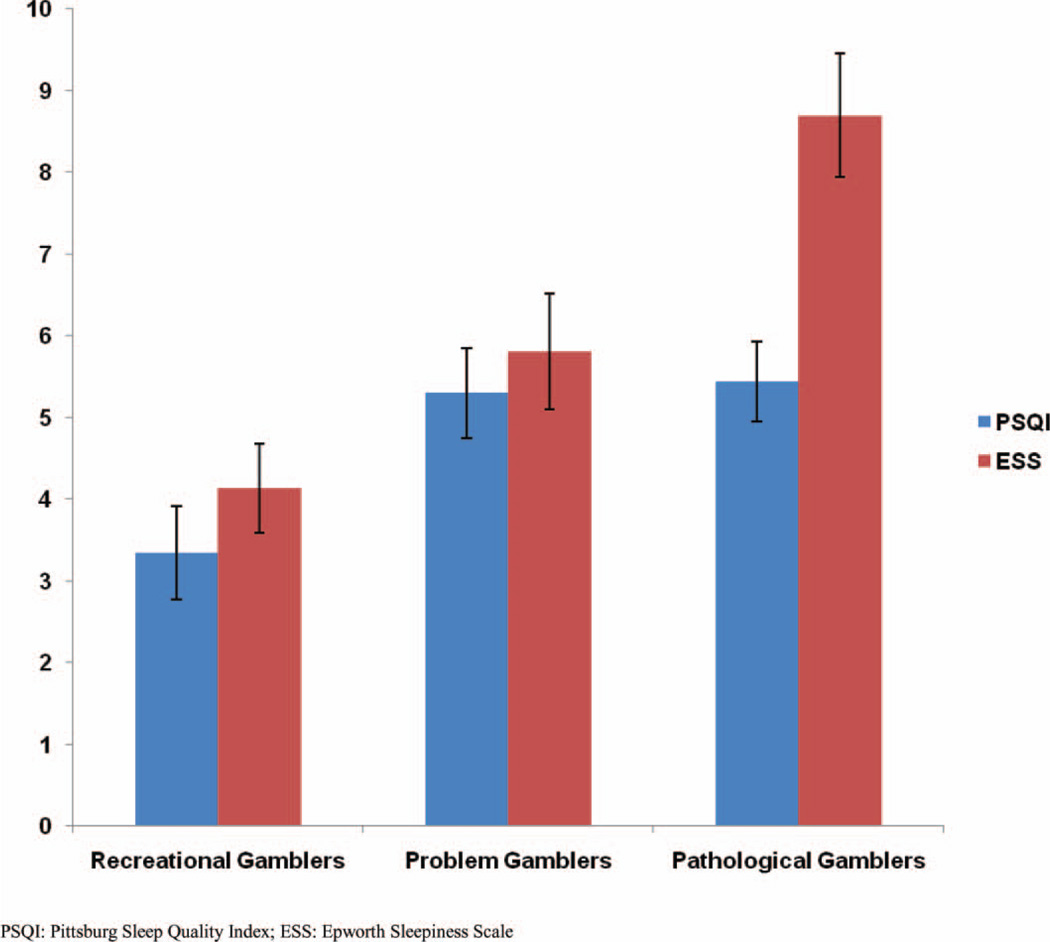
Although sleep has been extensively studied in substance related disorders, it has yet to be examined as thoroughly in gambling-related disorders. The purpose of this study is to examine the relationship between gambling severity and sleep disturbances in a sample of non-treatment seeking gamblers (N = 96) using the Pittsburgh Sleep Quality Index (PSQI) and Epworth Sleepiness Scale (ESS). Mean ESS scores for recreational, problem, and pathological gamblers were 4.13, 5.81, and 8.69, respectively, with a significant difference between pathological gamblers and both problem (P = .007) and recreational gamblers (P < .001). Mean PSQI scores for recreational, problem, and pathological gamblers were 3.35, 5.30, and 5.44, respectively, with a significant difference in sleep quality between recreational and problem gamblers (P = .018), as well as recreational and pathological gamblers (P = .008). As the first study to use objective sleep measures, these findings will not only increase awareness of this relationship, but also provide a foundation on which others can investigate the benefits of screening and adjunct treatment for sleep disorders in the gambling population.
Keywords: Gambling, sleep, insomnia, daytime sleepiness, Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale
INTRODUCTION
Gambling in the United States is a socially acceptable and widespread activity. Although most U.S. adults gamble without incurring problems, approximately 4% of the population has a current gambling disorder, and 6% will experience one at some point in their lives.1 The Diagnostic and Statistical Manual (DSM-IV) defines pathological gamblers as those who gamble despite serious social and personal consequences and who meet 5 of 10 criteria, including withdrawal, tolerance, and preoccupation.2 Problem gamblers, who are at an increased risk for developing pathological gambling, have less severe gambling problems and meet 1 to 4 of the criteria.3 Disordered gambling refers jointly to problem and pathological gambling.
The National Gambling Impact Study Commission estimated the economic cost of disordered gambling in the United States to be $5 billion per year.4 These values may be underestimated because the prevalence of disordered gambling is trending upward1,5 with the increased accessibility, affordability, anonymity and convenience of online gambling.6
Gambling disorders have an array of adverse physical and mental effects on health.7–9 They are associated with headaches,10 arthritis, angina,8,11 physiological stress,12,13 increased fatigue,14 and comorbid psychiatric or substance related disorders.15,16 Disordered gamblers also tend to use more medical services,8 are at a higher risk for suicidal ideations and attempts,17,18 and have a decreased quality of life.19 Socially, they are involved with domestic violence, child abuse, divorce,20 arrests, and incarceration more frequently than the general public.21–23
Interestingly, sleep disturbances have also been shown to be correlated with many of these adverse outcomes, yet sleep has not been examined thoroughly in gambling-related disorders. DSM-IV defines insomnia as a syndrome of diminished sleep that can be characterized by any of four domains of irregularity: difficulty initiating sleep, difficulty maintaining sleep, early morning awakening, and non-restorative sleep despite sufficient time spent sleeping.2 Epidemiological studies estimate the prevalence of insomnia to be between 10% and 40% depending on the criteria used.24–26 Insomnia is largely recognized as a major public health issue because of its frequency and large multi-faceted cost to society. Not only does poor sleep have harmful effects on several physiological parameters,27,28 but it has also been found to increase the risk for all-cause mortality,29 coronary heart disease, and diabetes mellitus.30 Beyond health related concerns, individuals suffering from sleep disturbances experience an increased risk of motor vehicle accidents, decreased work productivity, increased risk of suicide, excessive use of health care, and decreased quality of life.24–26,31–33
The relationship between sleep and substance related disorders has garnered great attention. Disturbances in sleep have been shown to have a bi-directional association with substance-related disorders.34–37 The neurophysiologic, biochemical, and gross effects of psychoactive substance use on sleep are well documented.35,38–44 In addition, studies suggest that the discontinuation of substance abuse usually does not immediately restore sleep, and in many cases it can further perturb it.45–49 Withdrawal from substance use can have a diverse set of consequences on both the amount and quality of sleep.45–48 These abnormalities in sleep may even increase the likelihood of patient relapse, and withdrawal associated sleep dysfunction can last for several months or years.48,50–54
Surprisingly, the literature on the relationship between sleep and gambling disorders is limited. Authors have described how gamblers will sometimes go days without sleep to gamble,55 and how some gamblers experience extreme stress and loss of sleep during crisis phases of continuous losses.55,56 The literature also discusses gambling withdrawal and the negative outcomes it can have on sleep.57–59 In addition, three cross-sectional studies have assessed sleep in gamblers with one yes-or-no question inquiring about sleep problems.60–62 This research usually involves gamblers who are seeking treatment or in treatment and behave differently than non-treatment seeking gamblers. In an effort to further investigate the relationship between gambling and sleep disturbances, an exploratory study will be conducted with two validated sleep questionnaires in a sample of non-treatment seeking gamblers. Given the similarities between gambling disorders and substance abuse, it is hypothesized that a strong relationship will exist between the severity of gambling and degree of sleep disturbance, similar to what was found between sleep and substance abuse. Hopefully, these findings will shed greater light on this relationship and provide a basis for further exploring the potential for problematic sleep screening and treatments in the disordered gambling population.
METHODS
Study Design
The data used for this cross-sectional study was obtained from the dataset of a larger project which sought to examine associations between gambling and several biopsychosocial domains. Participants were given $80 as incentive to participate, and the total time to complete all assessments was 4 hours. For this particular preliminary study, only responses from sleep and gambling related measures were examined. All participants gave written informed consent and study procedures were approved by the UCLA Institution Review Board for Human Subject Research.
Participants
A total of 120 participants were recruited based on the need to have a large enough sample size to demonstrate significant differences between gambling groups. Participants were recruited from June 2009 to July 2010 in Los Angeles, California, using advertisements online and in local newspapers. Self-selected participants were eligible if they were 18 years or older and able to understand English. Participants were excluded if they demonstrated unstable medical or psychiatric conditions (e.g., suicidal ideations), were currently receiving or seeking treatment for gambling disorders, or tested positive for cannabis, cocaine, opioids, methamphetamine, or alcohol.
Assessments
Gambling severity was assessed using interview style questions corresponding to the 10 DSM-IV criteria for pathological gambling. The questions asked about preoccupation, tolerance, withdrawal, loss of control, escape, chasing, lying, illegal acts, and risked relationships as they pertained to gambling.2 This is a valid and reliable diagnostic screener with high sensitivity and specificity,63,64 and the most common method used in prevalence studies to diagnose gambling disorders.16 Current evidence supports using the DSM-IV criteria to subgroup gambling behavior on a spectrum of severity.65,66 Participants also completed a self-administered questionnaire inquiring about gambling frequency and behavior.
Participants completed both the Pittsburgh Sleep Quality Index (PSQI) and the Epworth Sleepiness Scale (ESS), two valid and reliable self-administered questionnaires that assess sleep quality and daytime sleepiness respectively.67–70 The PSQI is a 19-item questionnaire, with scores ranging from 0–21. Scores greater than 5 indicate poor sleep quality and higher scores correlate well with greater sleep problems and psychological distress.71,72 The ESS consists of 8 individual self-reported items scored from 0–24 cumulatively; it measures a subject’s daytime sleepiness.69 Values greater than 10 indicate significant daytime sleepiness,70 and higher scores are associated with greater mean sleep latency, decreased total sleep time, and lower quality of life.73
Statistical Analysis
To address missing data, incomplete questionnaires were excluded. Participants with an absence of gambling in the past 30 days were also excluded to ensure a population of current gamblers. Lastly, participants who screened positive for a current manic episode were excluded because the DSM-IV definition of pathological gambling partially excludes the diagnosis of bipolar disorder2 and the presence of mania may have skewed the results.
Participants were categorized into three groups as follows based on the number of DSM-IV criteria for pathological gambling met: recreational gamblers (0 criteria), problem gamblers (1–4 criteria), and pathological gamblers (5–10 criteria).3 Chi-square analysis and analysis of variance (ANOVA) were used to determine whether statistically significant demographic differences existed between the gambling groups.
Chi-square analysis was used to compare the presence or absence of either significant daytime sleepiness (based on ESS) or poor sleep quality (based on PSQI). T tests were used to compare mean PSQI and ESS scores between the three gambling groups. SPSS version 19.0 software (SPSS, Inc, Chicago, IL) was used for data entry and analysis.
RESULTS
Sample Characteristics
Of the 120 participants recruited, 20 did not report any gambling in the past month, 3 had incomplete sleep questionnaires, 1 screened positive for bipolar I disorder, and 0 screened positive for current drug or alcohol use or suicidal ideation. Data from the remaining 96 participants were used in this study. In this sample, the majority of participants were male (52%), White (56%), and single (54%); most had some college education (49%), worked full-time (33%), and had an income of $1–25,000 (36%). The mean age was 40.48 years (standard deviation = 13 years).
There were 23 recreational gamblers, 37 problem gamblers, and 36 pathological gamblers in this sample. Demographic, gambling, and sleep characteristics are reported for the three groups (Tables 1 and 2). Preliminary analysis did not reveal any significant differences based on demographic characteristics between the three gambling groups (data not shown). As expected, ANOVA found statistical differences between recreational, problem, and pathological gamblers in the number of days gambled, the amount of money spent gambling, and the number of days spent gambling more than the participant could afford (P < .05) (Table 2). However, the time taken to fall asleep and the total sleep time did not differ among the three groups (Table 2). As a whole, the participants gambled an average of approximately 12 days in the past month, and they most frequently gambled on card games (6 days on average), the lottery (5 days on average), and sports (3 days on average) (data not shown). The sample size was not large enough to explore the relationship between the preferred types of gambling and the three gambling severity groups.
TABLE 1.
Demographics
| Variable | Recreational gamblers (n = 23, 24.0%) |
Problem gamblers (n = 37, 38.5%) |
Pathological gamblers (n = 36, 37.5%) |
|---|---|---|---|
| Age | |||
| Mean | 40.43 | 37.32 | 43.28 |
| Standard deviation | 12.61 | 13.38 | 12.84 |
| Sex | |||
| Male | 11 (48%) | 18 (49%) | 21 (58%) |
| Female | 12 (52%) | 19 (51%) | 15 (41%) |
| Level of education | |||
| Less than H.S. degree | 1 (4%) | 1 (3%) | 0 (0%) |
| High School or GED diploma | 1 (4%) | 3 (8%) | 3 (8%) |
| Some college | 8 (35%) | 15 (41%) | 23 (64%) |
| Graduated college | 13 (57%) | 18 (49%) | 10 (28%) |
| Race | |||
| White | 13 (57%) | 26 (70%) | 15 (42%) |
| African American | 4 (17%) | 6 (16%) | 8 (22%) |
| Asian | 2 (9%) | 3 (8%) | 7 (19%) |
| Hispanic | 4 (17%) | 2 (5%) | 2 (6%) |
| Other | 0 (0%) | 0 (0%) | 4 (11%) |
| Marital status | |||
| Legally married or living with partner | 6 (26%) | 5 (14%) | 10 (28%) |
| Separated, divorced, or widowed | 4 (17%) | 9 (24%) | 11 (31%) |
| Single (never married) | 13 (57%) | 23 (62%) | 15 (42%) |
| Employment | |||
| Full-time | 11 (48%) | 12 (32%) | 12 (33%) |
| Part-time | 5 (22%) | 5 (14%) | 8 (22%) |
| Student | 3 (13%) | 6 (16%) | 3 (8%) |
| Retired or disabled | 2 (9%) | 3 (8%) | 4 (11%) |
| Unemployed | 2 (9%) | 11 (30%) | 9 (25%) |
| Annual income | |||
| $0 | 1 (4%) | 7 (19%) | 2 (6%) |
| $1–$24,999 | 8 (35%) | 13 (35%) | 14 (39%) |
| $25,000–$49,999 | 9 (39%) | 12 (32%) | 11 (31%) |
| $50,000–$99,999 | 2 (9%) | 5 (14%) | 5 (14%) |
| $100,000 or greater | 3 (13%) | 0 (0%) | 4 (11%) |
Recreational gamblers were defined as having met 0 DSM-IV criteria for Pathological Gambling, while problem and pathological gamblers met 1–4 and greater than 5 criteria respectively. Preliminary analysis (Chi-square and ANOVA) did not find significant differences between recreational, problem, and pathological gamblers based on the above demographic criteria (α = 0.05). Percentages may not equal 100% due to rounding.
TABLE 2.
Gambling and Sleep Characteristics
| Variable | Recreational gambling (n = 23, 24%) |
Problem gambling (n = 37, 38.5%) |
Pathological gambling (n = 36, 37.5%) |
|---|---|---|---|
| Number of days gambled (in the past 30 days)* | |||
| Mean | 6.43 | 10.35 | 15.25 |
| Standard deviation | 7.12 | 8.54 | 9.78 |
| Number of days gambled more than could afford (in the past 30 days)* | |||
| Mean | 0.26 | 1.11 | 6.42 |
| Standard deviation | 1.25 | 2.81 | 9.87 |
| Average amount spent on gambling (weekly)* | |||
| Mean | $176 | $112 | $990 |
| Standard deviation | $448 | $127 | $2,282 |
| Age when first gambled, y | |||
| Mean | 20.22 | 20.03 | 18.21 |
| Standard deviation | 6.00 | 7.61 | 7.30 |
| Age at first gambling problem, y | |||
| Mean | 25.00 | 29.00 | 28.54 |
| Standard deviation | 1.53 | 12.12 | 8.92 |
| Reported hours of sleep per night | |||
| Mean | 7.30 | 6.98 | 6.88 |
| Standard deviation | 0.738 | 1.40 | 1.27 |
| Reported minutes took to fall asleep | |||
| Mean | 21.30 | 22.19 | 25.01 |
| Standard deviation | 16.26 | 15.11 | 18.71 |
aRecreational gamblers were defined as having met none of the DSM-IV criteria for pathological gambling, whereas problem and pathological gamblers met 1–4 and more than 5 criteria, respectively.
Significant difference between groups as determined using analysis of variance (P < .05).
Sleep Measures
Mean ESS scores for recreational, problem, and pathological gamblers were 4.13 (Standard Error of the Mean [SEM] = 0.546, 95% confidence interval [CI] = 3.06–5.20), 5.81 (SEM = 0.709, 95% CI = 4.42–7.20), and 8.69 (SEM = 0.755, 95% CI = 7.22–10.17), respectively. Analysis of ESS scores demonstrated a significant difference in mean daytime sleepiness between pathological gamblers and problem (P = .007) and recreational gamblers (P < .001) (Table 3, Figure 1). However, the difference in mean ESS scores between problem and recreational gamblers was not found to be significant (P = .065) (Table 3).
TABLE 3.
Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale Scores by Gambling Severity
| Variable | Recreational gamblers | Problem gamblers | Pathological gamblers |
|---|---|---|---|
| Pittsburgh Sleep Quality Index | |||
| N | 23 | 37 | 36 |
| Mean | 3.35 | 5.30 | 5.44 |
| SEM | 0.57 | 0.56 | 0.49 |
| 95% confidence interval | 2.23–4.47 | 4.21–6.39 | 4.49–6.40 |
| Significance (P) | .018 | .008 | .843 |
| Epworth Sleepiness Scale | |||
| N | 23 | 37 | 36 |
| Mean | 4.13 | 5.81 | 8.69 |
| SEM | 0.55 | 0.71 | 0.76 |
| 95% confidence interval | 3.06–5.20 | 4.42–7.20 | 7.22–10.17 |
| Significance (P) | .065 | <.001 | .007 |
aSample size (N), mean, standard error of the mean (SEM), and 95% confidence intervals for sleep quality as indicated by the Pittsburgh Sleep Quality Index and daytime sleepiness as indicated by the Epworth Sleepiness Scale categorized by severity of gambling. Significance (P) was calculated using a two-sided independent sample t test. Recreational gamblers were defined as having met none of the DSM-IV criteria for pathological gambling, whereas problem and pathological gamblers met 1–4 and more than 5 criteria, respectively.
FIGURE 1.
Mean PSQI and ESS scores by gambling severity. (Color figure available online)
Mean PSQI scores for recreational, problem, and pathological gamblers were 3.35 (SEM = 0.571, 95% CI = 2.23–4.47), 5.30 (SEM = 0.556, 95% CI = 4.21–6.39), and 5.44 (SEM = 0.489, 95% CI = 4.49–6.40), respectively (Table 3, Figure 1). There was a significant difference in sleep quality between recreational and problem gamblers (P = .018) and between recreational and pathological gamblers (P = .008), but no significant difference was found between mean PSQI scores for pathological and problem gamblers (P = .843) (Table 3).
Ancillary chi-square analysis also found a significant difference (Chi-Square = 9.865, df = 2, P = .007) in the frequency of significant daytime sleepiness (ESS > 10) based on severity of gambling behavior (data not shown). In our study, 30% (n = 11) of pathological gamblers, 14% (n = 11) of problem gamblers, and 0% (n = 0) of recreational gamblers experienced significant daytime sleepiness (data not shown). Similar analysis of PSQI scores revealed that 42% (n = 15) of pathological gamblers, 32% (n = 12) of problem gamblers, and 17% (n = 4) of recreational gamblers experienced poor sleep quality (PSQI > 5) (data not shown). This association was not found to be statistically significant (Chi-Square = 3.783, df = 2, P = .151) (data not shown).
DISCUSSION
This study examined the relationship between sleep and gambling severity in a sample of non-treatment seeking gamblers. These results indicate that decreased sleep quality is seen in any form of gambling disorder (problem or pathological), but only pathological gamblers experience significantly increased daytime sleepiness relative to recreation gambling controls. Although a few studies have made note of sleep disturbances experienced during crisis or withdrawal,55,56,59 these findings demonstrate that problematic sleep occurs for current non-treatment seeking gamblers as well.
Although an increasing trend in ESS scores based on gambling severity is visually evident (Figure 1), a statistically significant difference was not found between recreational and problem gamblers. However, it should be noted that although no statistically significant difference was found in mean daytime sleepiness between recreational and problem gamblers (P = .065), these results indicate a high likelihood that a difference does exist in mean daytime sleepiness between these groups. A larger sample size may have allowed the achievement of statistical significance. This implies that each categorical increase in gambling severity may correlate with a corresponding increase in mean ESS score, and that a hierarchical relationship between recreational, problem, and pathological gamblers likely does exist in terms of daytime sleepiness. However, in terms of the PSQI, no difference was found in sleep quality between problem and pathological gamblers (P = .843), implying that any form of disordered gambling is sufficient to induce significantly decreased sleep quality. Studies have demonstrated that the PSQI and ESS measure different components of problematic sleep.72 Surprisingly, a statistical difference was not found for the hours of sleep per night and the time it took to fall asleep between the three gambling groups. Because significant differences were found on the ESS and PSQI, this may indicate that gamblers acquire some sleep problems but not others as gambling disorders progress.
Gamblers may have trouble with sleep for a variety of reasons. It is suspected that social, psychological, and biological factors all play a role in promoting disturbed sleep for the gambling population. Socially, gambling is highly accessible due to the continuous availability of casinos and online gambling (24 hours a day, every day of the year). In addition, disordered gamblers may experience dissociation when gambling and lose track of time.74,75 The combination of possible dissociation and accessibility to gambling creates a setting conducive to gambling throughout the night, causing gamblers to lose sleep.
Psychological factors also affect the sleep of gamblers. Mood disorders, anxiety disorders, and substance-related disorders are among the most common comorbid conditions of pathological gambling.16 Interestingly, insomnia is an important feature of these disorders,76,77 and the presence of these comorbid disorders may contribute to problems with sleep in gamblers. Shame, guilt, depression, helplessness, and anger are all commonly experienced in pathological gamblers. These feelings become worse as the gambling disorder progresses. Even when criteria are not met for a formal psychiatric diagnosis, the negative or dysphoric affect and state of mind of the gambler can have a significant effect on sleep. The preoccupation with gambling, reliving past gambling experiences, planning next gambling sessions, and thinking about ways to get money to gamble2 can further contribute to the disturbed sleep and stress. Extreme amounts of stress are common in pathological gamblers,13 and evidence is mounting that suggests that this stress also adversely affects sleep.78
Several biological mechanisms may be useful in explaining the sleep problems of gamblers. Of particular interest is the recent work examining the role of clock genes in human biology and disease, particularly mental illness. Clock genes, which code for proteins that regulate the circadian rhythm and the leep/wake cycle, have been implicated not only in sleep disorders, but also in substance abuse disorders and other psychiatric illness, most notably depression and bipolar disorder.79–82 The expression of these clock genes is altered by the use of psychoactive drugs or during the process of psychiatric disease and sleep disorders.79–82 Interestingly, a bi-directional association has been found whereby not only do drugs of abuse have an effect on the expression of these clock genes, but the differential expression of these clock genes in turn influences the consequences of using psychoactive drugs.80,81 Given the substantial role for clock genes in substance abuse, mental illness, and sleep disorders, they may serve a similar function in gambling disorders.
Conversely, problematic sleep may have a significant effect on gambling outcomes. Recent studies have demonstrated that sleep disturbances impair self-control and decision-making,83,84 increase impulsivity, attenuate responses to losses and increase expectations of gains,85 and degrade cognition in executive functioning tasks,86,87 which may suggest that problematic sleep could increase the risk for development of more severe gambling. Substance abusers, who often acquire sleep problems, are known to use drugs to self-medicate and cope with these issues.51,88–90 Similarly, pathological gamblers may gamble as an escape from their sleep problems, as well as anxiety and depression, and this use of gambling as a coping mechanism is even listed in the DSM-IV as one of the 10 diagnostic criteria for the disorder. Along with the recent findings on impulsivity and impaired decision making, this suggests that a bi-directional association may be present, whereby poor sleep promotes detrimental gambling behavior, and disordered gambling in turn adversely affects sleep. Such a positive feedback loop would promote the progression of gambling disorders. Future studies may choose to examine the causal nature of this relationship and investigate which of the two more frequently predicts the other.
The clinical implications of disturbed sleep in gamblers are plentiful. Sleep problems currently receive no mention in the DSM-IV description of pathological gambling,2 and evidence-based treatments for gambling do not include the management of sleep disturbances.91,92 In light of this, treatment providers may be unaware that this population is at risk for poor sleep. Problematic sleep is associated with increased risk of motor vehicle accidents, significantly decreased work productivity, increased risk of suicide, excessive use of health care, and decreased quality of life.24–26,31–33 These associations may intensify the impact inflicted from gambling disorders. In addition, benefits have been shown for the treatment of problematic sleep in other psychiatric conditions, including substance abuse.54,77,93–99 Bootzin and Stevens77 even suggest that the treatment of insomnia associated with substance use withdrawal may be an effective strategy in aiding in the prevention of relapse.
The sample size of this study was the chief limitation. A larger sample size would have allowed greater control for potential confounders, such as comorbid psychiatric disorders. However, because the frequency of psychiatric and substance related disorders is high for disordered gamblers (57.5% for substance use disorders, 37.9% for mood disorders, and 37.4% for anxiety disorders),5,16 examining sleep in disordered gamblers without these comorbidities may be clinically inapplicable. Due to this study’s sample size, it was statistically challenging to explore the specific relationship between sleep disturbances and preferred gambling behavior because several independent gambling factors may play a role in the development of sleep disturbances (e.g., duration, frequency, and amount spent gambling). A larger dataset would allow a multiple logistic regression analysis to account for several independent variables, such as hours played, number of days played, and dollars gambled. Lastly, the nature of questionnaires is that they typically create some recall bias.72 Future studies may attempt to use more objective sleep measures such as polysomniography.
Despite these limitations, this study was able to take a reliable cross-sectional glance at the landscape of sleep disturbances within a severity distribution of gamblers. This was the first study to find an association between problematic sleep and gambling severity using valid and reliable sleep measures in non-treatment seeking gamblers. Hopefully, these findings will not only increase awareness of this relationship, but also provide a foundation on which others can investigate the benefits of screening and adjunct treatment for sleep disorders in the gambling population.
Acknowledgments
This project was funded by the National Institute on Drug Abuse (Grant #: K23DA 19522-2) and the Annenberg Foundation.
Footnotes
Full terms and conditions of use: http://www.tandfonline.com/page/terms-and-conditions
This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden.
Publisher's Disclaimer: The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae, and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand, or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
REFERENCES
- 1.Shaffer H, Hall M. Updating and refining prevalence estimates of disordered gambling behaviour in the United States and Canada. Can J Public Health. 2002;92:168–172. doi: 10.1007/BF03404298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV-TR (text revision) Washington, DC: APA; 2000. [Google Scholar]
- 3.Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: a research synthesis. Am J Public Health. 1999;89:1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerstein D, Hoffmann J, Larison C, et al. Gambling impact and behavior study: report to the National Gambling Impact Study Commission. Chicago, IL: National Opinion Research Center Chicago; 1999. [Google Scholar]
- 5.Kessler R, Hwang I, LaBrie R, et al. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychol Med. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffiths M. Internet gambling: issues, concerns, and recommendations. Cyberpsychology Behav. 2003;6:557–568. doi: 10.1089/109493103322725333. [DOI] [PubMed] [Google Scholar]
- 7.Potenza MN, Fiellin DA, Heninger GR, Rounsaville BJ, Mazure CM. Gambling: an addictive behavior with health and primary care implications. J Gen Intern Med. 2002;17:721–732. doi: 10.1046/j.1525-1497.2002.10812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morasco BJ, Pietrzak RH, Blanco C, Grant BF, Hasin D, Petry NM. Health problems and medical utilization associated with gambling disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2006;68:976–984. doi: 10.1097/01.psy.0000238466.76172.cd. [DOI] [PubMed] [Google Scholar]
- 9.Morasco BJ, Vom Eigen KA, Petry NM. Severity of gambling is associated with physical and emotional health in urban primary care patients. Gen Hosp Psychiatry. 2006;28:94–100. doi: 10.1016/j.genhosppsych.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Pasternak AV, IV, Fleming M. Prevalence of gambling disorders in a primary care setting. Arch Fam Med. 1999;8:515–520. doi: 10.1001/archfami.8.6.515. [DOI] [PubMed] [Google Scholar]
- 11.Pietrzak R, Morasco B, Blanco C, Grant B, Petry N. Gambling level and psychiatric and medical disorders in older adults: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Geriatr Psychiatry. 2007;15:301–313. doi: 10.1097/01.JGP.0000239353.40880.cc. [DOI] [PubMed] [Google Scholar]
- 12.Meyer G, Hauffa BP, Schedlowski M, Pawlak C, Stadler MA, Exton MS. Casino gambling increases heart rate and salivary cortisol in regular gamblers. Biol Psychiatry. 2000;48:948–953. doi: 10.1016/s0006-3223(00)00888-x. [DOI] [PubMed] [Google Scholar]
- 13.Goudriaan AE, Oosterlaan J, de Beurs E, Van den Brink W. Pathological gambling: a comprehensive review of biobehavioral findings. Neurosci Biobehav Rev. 2004;28:123–141. doi: 10.1016/j.neubiorev.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Bergh C, Kühlhorn E. Social, psychological and physical consequences of pathological gambling in Sweden. J Gambl Stud. 1994;10:275–285. doi: 10.1007/BF02104968. [DOI] [PubMed] [Google Scholar]
- 15.Petry N, Stinson F, Grant B. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 16.Lorains FK, Cowlishaw S, Thomas SA. Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta analysis of population surveys. Addiction. 2011;106:490–498. doi: 10.1111/j.1360-0443.2010.03300.x. [DOI] [PubMed] [Google Scholar]
- 17.Ledgerwood D, Petry N. Gambling and suicidality in treatment-seeking pathological gamblers. J Nerv Ment Dis. 2004;192:711–714. doi: 10.1097/01.nmd.0000142021.71880.ce. [DOI] [PubMed] [Google Scholar]
- 18.Petry N, Kiluk B. Suicidal ideation and suicide attempts in treatment-seeking pathological gamblers. J Nerv Ment Dis. 2002;190:462–469. doi: 10.1097/01.NMD.0000022447.27689.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin E-YJ, Casswell S, Easton B, Huckle T, Asiasiga L, You RQ. Time and money spent gambling and the relationship with quality-of-life measures: a national study of New Zealanders. Journal of Gambling Issues. 2010;24:33–53. [Google Scholar]
- 20.Shaw M, Forbush K, Schlinder J, Rosenman E, Black D. The effect of pathological gambling on families, marriages, and children. CNS Spectr. 2007;12:615–622. doi: 10.1017/s1092852900021416. [DOI] [PubMed] [Google Scholar]
- 21.Blaszczynski A, McConaghy N, Frankova A. Crime, antisocial personality and pathological gambling. Journal of Gambling Behavior. 1989;5:137–152. [Google Scholar]
- 22.Brown RIF. Pathological gambling and associated patterns of crime: comparisons with alcohol and other drug addictions. Journal of Gambling Studies. 1987;3:98–114. [Google Scholar]
- 23.Ledgerwood DM, Weinstock J, Morasco BJ, Petry NM. Clinical Features and treatment prognosis of pathological gamblers with and without recent-gambling-related illegal behavior. J Am Acad Psychiatry Law. 2007;35:294–301. [PubMed] [Google Scholar]
- 24.Hossain JL, Shapiro CM. The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath. 2002;6:85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 25.Leger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010;14:379–389. doi: 10.1016/j.smrv.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 26.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3:S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 27.Tochikubo O, Ikeda A, Miyajima E, Ishii M. Effects of insufficient sleep on blood pressure monitored by a new multi-biomedical recorder. Hypertension. 1996;27:1318–1324. doi: 10.1161/01.hyp.27.6.1318. [DOI] [PubMed] [Google Scholar]
- 28.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 29.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–107. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 30.Ayas NT, White DP, Manson JAE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 31.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, Lerner D. The cost of poor sleep: workplace productivity loss and associated costs. J Occup Environ Med. 2010;52:91–98. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- 33.Wade AG. The societal costs of insomnia. Neuropsychiatr Dis Treat. 2010;7:1–18. doi: 10.2147/NDT.S15123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug Alcohol Depend. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 35.Tynjala J, Kannas L, Levalahti E. Perceived tiredness among adolescents and its association with sleep habits and use of psychoactive substances. J Sleep Res. 1997;6:189–198. doi: 10.1046/j.1365-2869.1997.00048.x. [DOI] [PubMed] [Google Scholar]
- 36.Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcohol Clin Exp Res. 2004;28:578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- 37.Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009;10:787–796. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jaehne A, Loessl B, Barkai Z, Riemann D, Hornyak M. Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev. 2009;13:363–377. doi: 10.1016/j.smrv.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Lumley M, Roehrs T, Asker D, Zorick F, Roth T. Ethanol and caffeine effects on daytime sleepiness/alertness. Sleep. 1987;10:306–312. [PubMed] [Google Scholar]
- 40.McCann UD, Ricaurte GA. Effects of (+/−) 3,4-methylenedioxymetham phetamine (MDMA) on sleep and circadian rhythms. ScientificWorldJournal. 2007;7:231–238. doi: 10.1100/tsw.2007.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schierenbeck T, Riemann D, Berger M, Hornyak M. Effect of illicit recreational drugs upon sleep: cocaine, ecstasy and marijuana. Sleep Med Rev. 2008;12:381–389. doi: 10.1016/j.smrv.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 42.Sharma R, Engemann S, Sahota P, Thakkar MM. Role of adenosine and wake-promoting basal forebrain in insomnia and associated sleep disruptions caused by ethanol dependence. J Neurochem. 2010;115:782–794. doi: 10.1111/j.1471-4159.2010.06980.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stein MD, Friedmann PD. Disturbed sleep and its relationship to alcohol use. Subst Abus. 2005;26:1–13. doi: 10.1300/j465v26n01_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wasielewski JA, Holloway FA. Alcohol’s interactions with circadian rhythms. A focus on body temperature. Alcohol Res Health. 2001;25:94–100. [PMC free article] [PubMed] [Google Scholar]
- 45.Jones EM, Knutson D, Haines D. Common problems in patients recovering from chemical dependency. Am Fam Physician. 2003;68:1971–1978. [PubMed] [Google Scholar]
- 46.Morgan PT, Malison RT. Cocaine and sleep: early abstinence. Scientific World-Journal. 2007;7:223–230. doi: 10.1100/tsw.2007.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Budney AJ, Hughes JR, Moore BA, Novy PL. Marijuana abstinence effects in marijuana smokers maintained in their home environment. Arch Gen Psychiatry. 2001;58:917–924. doi: 10.1001/archpsyc.58.10.917. [DOI] [PubMed] [Google Scholar]
- 48.Landolt HP, Gillin JC. Sleep abnormalities during abstinence in alcohol-dependent patients. Aetiology and management. CNS Drugs. 2001;15:413–425. doi: 10.2165/00023210-200115050-00006. [DOI] [PubMed] [Google Scholar]
- 49.Kowatch RA, Schnoll SS, Knisely JS, Green D, Elswick RK. Electroencephalographic sleep and mood during cocaine withdrawal. J Addict Dis. 1992;11:21–45. doi: 10.1300/J069v11n04_03. [DOI] [PubMed] [Google Scholar]
- 50.Brower KJ, Aldrich MS, Hall JM. Polysomnographic and subjective sleep predictors of alcoholic relapse. Alcohol Clin Exp Res. 1998;22:1864–1871. [PubMed] [Google Scholar]
- 51.Brower KJ, Aldrich MS, Robinson EA, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. Am J Psychiatry. 2001;158:399–404. doi: 10.1176/appi.ajp.158.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Drummond SP, Gillin JC, Smith TL, De-Modena A. The sleep of abstinent pure primary alcoholic patients: natural course and relationship to relapse. Alcohol Clin Exp Res. 1998;22:1796–1802. [PubMed] [Google Scholar]
- 53.Foster JH, Peters TJ. Impaired sleep in alcohol misusers and dependent alcoholics and the impact upon outcome. Alcohol Clin Exp Res. 1999;23:1044–1051. [PubMed] [Google Scholar]
- 54.Arnedt JT, Conroy DA, Brower KJ. Treatment options for sleep disturbances during alcohol recovery. J Addict Dis. 2007;26:41–54. doi: 10.1300/J069v26n04_06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lesieur HR, Rosenthal RJ. Pathological gambling: a review of the literature (prepared for the American Psychiatric Association task force on DSM-IV committee on disorders of impulse control not elsewhere classified) Journal of Gambling Studies. 1991;7:5–39. doi: 10.1007/BF01019763. [DOI] [PubMed] [Google Scholar]
- 56.Lesieur HR, Custer RL. Pathological gambling: roots, phases, and treatment. Ann Am Acad Pol Soc Sci. 1984:146–156. [Google Scholar]
- 57.Wray I, Dickerson MG. Cessation of high frequency gambling and ‘withdrawal’ symptoms. Br J Addict. 1981;76:401–405. doi: 10.1111/j.1360-0443.1981.tb03238.x. [DOI] [PubMed] [Google Scholar]
- 58.Lorenz V, Yaffee R. Pathological gambling: psychosomatic, emotional and marital difficulties as reported by the gambler. Gambling Studies. 1986;2:40–49. [Google Scholar]
- 59.Rosenthal RJ, Lesieur HR. Self reported withdrawal symptoms and pathological gambling. Am J Addict. 1992;1:150–154. [Google Scholar]
- 60.Griffiths M. Gambling: an emerging area of concern for health psychologists. J Health Psychol. 2001;6:477–479. doi: 10.1177/135910530100600501. [DOI] [PubMed] [Google Scholar]
- 61.Hodgins DC, El Guebaly N. Natural and treatment assisted recovery from gambling problems: a comparison of resolved and active gamblers. Addiction. 2000;95:777–789. doi: 10.1046/j.1360-0443.2000.95577713.x. [DOI] [PubMed] [Google Scholar]
- 62.Bakken IJ, Gotestam KG, Grawe RW, Wenzel HG, Øren A. Gambling behavior and gambling problems in Norway 2007. Scand J Psychol. 2009;50:333–339. doi: 10.1111/j.1467-9450.2009.00713.x. [DOI] [PubMed] [Google Scholar]
- 63.Zimmerman M, Chelminski I, Young D. A psychometric evaluation of the DSM-IV pathological gambling diagnostic criteria. Journal of Gambling Studies. 2006;22:329–337. doi: 10.1007/s10899-006-9020-x. [DOI] [PubMed] [Google Scholar]
- 64.Stinchfield R. Reliability, validity, and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. Am J Psychiatry. 2003;160:180–182. doi: 10.1176/appi.ajp.160.1.180. [DOI] [PubMed] [Google Scholar]
- 65.Toce Gerstein M, Gerstein DR, Volberg RA. A hierarchy of gambling disorders in the community. Addiction. 2003;98:1661–1672. doi: 10.1111/j.1360-0443.2003.00545.x. [DOI] [PubMed] [Google Scholar]
- 66.Strong DR, Kahler CW. Evaluation of the continuum of gambling problems using the DSM IV. Addiction. 2007;102:713–721. doi: 10.1111/j.1360-0443.2007.01789.x. [DOI] [PubMed] [Google Scholar]
- 67.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 68.Buysse D, Reynolds C, III, Monk TH, Berman S, Kupfer DJ. Pittsburgh sleep quality index (PSQI) Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 69.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 70.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 71.Buysse DJ, Reynolds C, III, Monk TH, Hoch CC, Yeager A, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14:331–338. [PubMed] [Google Scholar]
- 72.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/ polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–571. [PMC free article] [PubMed] [Google Scholar]
- 73.Olson L, Cole M, Ambrogetti A. Correlations among Epworth Sleepiness Scale scores, multiple sleep latency tests and psychological symptoms. J Sleep Res. 1998;7:248–253. doi: 10.1046/j.1365-2869.1998.00123.x. [DOI] [PubMed] [Google Scholar]
- 74.Diskin KM, Hodgins DC. Narrowing of attention and dissociation in pathological video lottery gamblers. Journal of Gambling Studies. 1999;15:17–28. doi: 10.1023/a:1023062912062. [DOI] [PubMed] [Google Scholar]
- 75.Noseworthy TJ, Finlay K. A comparison of ambient casino sound and music: effects on dissociation and on perceptions of elapsed time while playing slot machines. Journal of Gambling Studies. 2009;25:331–342. doi: 10.1007/s10899-009-9136-x. [DOI] [PubMed] [Google Scholar]
- 76.Riemann D. Insomnia and comorbid psychiatric disorders. Sleep Med. 2007;8(Suppl 4):S15–S20. doi: 10.1016/S1389-9457(08)70004-2. [DOI] [PubMed] [Google Scholar]
- 77.Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. 2005;25:629–644. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 78.Van Reeth O, Weibel L, Spiegel K, Leproult R, Dugovic C, Maccari S. Physiology of sleep (review)-interactions between stress and sleep: from basic research to clinical situations. Sleep Med Rev. 2000;4:201–219. [Google Scholar]
- 79.Falcon E, McClung CA. A role for the circadian genes in drug addiction. Neuropharmacology. 2009;56(Suppl 1):91–96. doi: 10.1016/j.neuropharm.2008.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Manev H, Uz T. Clock genes: influencing and being influenced by psychoactive drugs. Trends Pharmacol Sci. 2006;27:186–189. doi: 10.1016/j.tips.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 81.Perreau-Lenz S, Spanagel R. The effects of drugs of abuse on clock genes. Drug News Perspect. 2008;21:211–217. doi: 10.1358/dnp.2008.21.4.1213350. [DOI] [PubMed] [Google Scholar]
- 82.Rosenwasser AM. Circadian clock genes: non-circadian roles in sleep, addiction, and psychiatric disorders? Neurosci Biobehav Rev. 2010;34:1249–1255. doi: 10.1016/j.neubiorev.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 83.Hagger MS. Sleep, self regulation, self control and health. Stress Health. 2010;26:181–185. [Google Scholar]
- 84.Killgore WD, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008;9:517–526. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 85.Venkatraman V, Chuah Y, Huettel SA, Chee M. Sleep deprivation elevates expectation of gains and attenuates response to losses following risky decisions. Sleep. 2007;30:603–609. doi: 10.1093/sleep/30.5.603. [DOI] [PubMed] [Google Scholar]
- 86.Harrison Y, Horne JA. The impact of sleep deprivation of decision making: a review. J Exp Psychol Appl. 2000;6:236249. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- 87.Tucker AM, Whitney P, Belenky G, Hinson JM, Van Dongen HPA. Effects of sleep deprivation on dissociated components of executive functioning. Sleep. 2010;33:47–57. doi: 10.1093/sleep/33.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bonn-Miller MO, Babson KA, Vujanovic AA, Feldner MT. Sleep problems and PTSD symptoms interact to predict marijuana use coping motives: a preliminary investigation. J Dual Diagn. 2010;6:111–122. [Google Scholar]
- 89.Crum RM, Storr CL, Chan YF, Ford DE. Sleep disturbance and risk for alcohol-related problems. Am J Psychiatry. 2004;161:1197–1203. doi: 10.1176/appi.ajp.161.7.1197. [DOI] [PubMed] [Google Scholar]
- 90.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31:1351–1356. [PMC free article] [PubMed] [Google Scholar]
- 91.Brewer JA, Grant JE, Potenza MN. The treatment of pathologic gambling. Addict Disord Their Treat. 2008;7:1–13. [Google Scholar]
- 92.Leung KS, Cottler LB. Treatment of pathological gambling. Curr Opin Psychiatry. 2009;22:69–74. doi: 10.1097/YCO.0b013e32831575d9. [DOI] [PubMed] [Google Scholar]
- 93.Neubauer DN. Current and new thinking in the management of comorbid insomnia. Am J Manag Care. 2009;15:S24–S32. [PubMed] [Google Scholar]
- 94.Rybarczyk B, LundHG, Mack L, Stepanski E. Comorbid insomnia. Sleep Med Clin. 2009;4:571–582. [Google Scholar]
- 95.Stepanski EJ, Rybarczyk B. Emerging research on the treatment and etiology of secondary or comorbid insomnia. Sleep Med Rev. 2006;10:7–18. doi: 10.1016/j.smrv.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 96.Arnedt JT, Conroy DA, Armitage R, Brower KJ. Cognitive-behavioral therapy for insomnia in alcohol dependent patients: A randomized controlled pilot trial. Behav Res Ther. 2011;49:227–233. doi: 10.1016/j.brat.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brower KJ, Perron BE. Sleep disturbance as a universal risk factor for relapse in addictions to psychoactive substances. Med Hypotheses. 2010;74:928–933. doi: 10.1016/j.mehy.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bolla KI, Lesage SR, Gamaldo CE, et al. Sleep disturbance in heavy marijuana users. Sleep. 2008;31:901–908. doi: 10.1093/sleep/31.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Friedmann PD, Herman DS, Freedman S, Lemon SC, Ramsey S, Stein MD. Treatment of sleep disturbance in alcohol recovery. J Addict Dis. 2003;22:91–103. doi: 10.1300/J069v22n02_08. [DOI] [PMC free article] [PubMed] [Google Scholar]