Abstract
Objective. To further develop and evaluate a diabetes disease state management (DSM) program that provided direct patient care responsibilities to advanced pharmacy practice experience (APPE) students as members of healthcare teams.
Design. Nine new clinics and 3 established sites that provide self-care management education to patients with diabetes were established and maintained in rural Colorado pharmacies and supported by students in APPE training for 48 weeks per year.
Evaluation. The 12 clinics provided 120 APPE student placements in 2010-2011. Students’ perceptions of their experiences were positive. Patients who completed the student-supported diabetes self-management education program had improvements in blood glucose, blood pressure, and lipid values.
Conclusions. Twelve diabetes DSM clinics provided direct patient care opportunities to APPE students working as part of healthcare teams while expanding healthcare resources in underserved communities in Colorado.
Keywords: pharmacy education, diabetes, advanced pharmacy practice experience, outcomes
INTRODUCTION
In Standards 2007, the Accreditation Council for Pharmacy Education stated that its interest was “to ensure the development of students who can contribute to the care of patients and to the profession by practicing with competence and confidence in collaboration with other health care providers.”1 The Standards emphasize the importance of experiential education in student development, specifying that “pharmacy practice experiences must permit students, under appropriate supervision and as permitted by practice regulations, to assume direct patient care responsibilities.” Accordingly, it is important and logical for colleges and schools of pharmacy to design pharmacy practice experience programs that give direct patient care responsibilities to students in environments that foster a team-based approach to patient care.
We reported in 2007 the development of a statewide group of clinical pharmacy programs in partnership with hospital, community health center, and community pharmacies, which created 213 APPE training sites in the 2006-2007 academic year for the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences.2 The partnerships were established with pharmacies willing to use APPE students to expand their scope of clinical practice or to support existing programs. Each partner was asked to choose the clinical program they wished implemented or supported. The partners were guaranteed that students would contribute to carrying their program's clinical service workload for 48 weeks per year under the supervision of their pharmacists, and were offered equipment, supplies, and training and mentoring for their pharmacists.
The clinical programs included DSM programs for patients with diabetes in healthcare-professional shortage areas in rural Colorado. We report here the expansion and further development of pharmacy-based diabetes DSM clinics in rural Colorado, the perceptions of students regarding their diabetes DSM clinic experiences, and the health outcomes of patients with diabetes who received care at the clinics.
DESIGN
Expansion of DSM Clinics
Community and community health center pharmacies in rural Colorado at sites distant from existing student-supported diabetes DSM clinics were approached to determine their interest in partnering with the school to establish diabetes DSM programs. Sites that responded positively were asked to identify local providers with good working relationships with the pharmacy and those providers were interviewed by school-based faculty members. The faculty explained the school's interest in enhancing local resources for the care of patients with diabetes and in developing APPE training sites for its students in healthcare environments that support a team-based approach to patient care. Sites where local providers were prepared to partner with pharmacists and pharmacy students in a team-based approach to the care of patients with diabetes, and where local pharmacists were motivated to implement diabetes DSM services and willing to give direct patient care responsibilities to students under appropriate supervision, were targeted for development.
The diabetes DSM programs were implemented by school faculty members with salary offset provided by competitive grant funds. The faculty members provided onsite education for each site's pharmacists based on the American Diabetes Association's evidence-based guidelines for diabetes self-management education and taught the pharmacists the appropriate management of blood sugar, hypertension, and lipid abnormalities in patients with diabetes. Faculty members created clinical training opportunities for the partner's pharmacists by providing onsite care to patients with diabetes and then transitioned the workload of running the clinics to the partner's pharmacists as a way to hone their competency to provide diabetes DSM care. The transition from faculty- to preceptor-directed education varied by site, but in general, preceptors received 8-12 hours of training and observed 2 to 6 patient encounters modeled by faculty members before taking over clinic responsibilities under the ongoing supervision of a faculty member. Faculty members were normally able to assume an off-site consulting role after approximately 2 to 4 weeks. The diabetes DSM clinics usually operated 1 day per week during the preceptor training process, which allowed faculty members to continue their school-based responsibilities during the training process.
The transition from preceptor-delivered to student-delivered patient education also was supported by faculty members. The time needed for the transition varied by site and by students, based on the available time each preceptor had to dedicate to the program and on the competencies shown by each student at the start of the APPE experience. Preceptors supervising their first APPE student took approximately 1 month to become comfortable with turning over direct patient-care responsibilities to the students. Each preceptor established confidence in a student at the start of every APPE, but the students supported the majority of the clinic's workload after the second week of the practice experience.
DSM Clinic Procedures
Diabetes DSM clinic procedures have been described in detail previously.3 Patient enrollment came from physician referrals and from patients who sought out pharmacy-based care. Patient appointments were structured to last approximately 60 minutes and the clinics averaged 2 to 5 patient education appointments each week. The students were allowed 60 minutes after each appointment to document their activities and submit preceptor-approved case notes to the patient's providers. When not engaged in diabetes DSM clinic activities, the APPE students were engaged in other pharmacy activities, including dispensing and medication, health-promotion, and disease-prevention counseling.
The model for the diabetes education was for students under preceptor supervision to conduct individual 1-hour appointments with patients diagnosed with type 1 or type 2 diabetes. Six of these one-on-one DSM sessions were held with the patient over a 6-month period. The first visit comprised an initial assessment of the patient that included obtaining a medical and medication history; assessing the patient's understanding of diabetes, hypertension, and lipids; physical assessment including height, weight and abdominal girth measurements; and point-of-care measurements including glycosylated hemoglobin (A1c), blood pressure and fasting total cholesterol, high density lipoprotein-cholesterol (HDL-C), low density lipoprotein-cholesterol (LDL-C), and triglycerides. Visits 2 through 5 focused on patient self-care education and included personalized information on diabetes, hypertension, cholesterol, and triglycerides, and their management by diet, exercise, and medication. The sixth visit provided an opportunity for students to reinforce the patient self-care education and to repeat the point-of-care measurements for A1c, blood pressure, fasting total cholesterol, HDL-C, LDL-C, and triglycerides. Specific information regarding the patient self-care education provided and the checklist protocols followed by students at each patient visit are available from the authors on request.
Further Development of the DSM Clinics
An Internet-based electronic charting software program was developed and implemented at the diabetes DSM clinic sites as a quality improvement measure in 2007. The program permitted the scheduling of patient appointments and alerted students to follow up with patients who missed appointments. It provided a checklist of activities to be completed at each patient visit and generated “red-flag” alerts to remind students when checklist activities were omitted. In addition, it permitted online access for school-based faculty to support students and their onsite preceptors in their patient care activities and permitted educational tools and resources available at the clinics to be standardized. A school-based 1-day training program was implemented for all students at the start of their 6-week APPE. It was established to review and reinforce the classroom training students had received about diabetes, to orient the students to diabetes DSM clinic operations and the electronic charting software program, and to provide training in the use of the clinics’ point-of-care technology. While all students had limited point-of-care skill sets from the school's professional skills courses, those who had participated in health fair activities had developed stronger skill sets. None of the students had any experience prior to the APPE in using the electronic charting software program.
Data Collection and Analysis
Patients’ hemoglobin A1c and lipid values were obtained at visits 1 and 6 from providers’ medical records and onsite in the diabetes DSM clinics from finger-stick blood samples using point-of-care technology (DCA 2000/ DCA Vantage, Siemens, Washington DC and Cholestech LDX, Cholestech, Hayward, CA). Provider-based laboratory data were included as visit 1 and 6 data if the tests had been conducted within 45 days before or 30 days after the pharmacy clinic visit for A1c levels and within 30 days of the clinic visit for lipid values. All blood pressure values were obtained on site at the DSM clinics during visits 1 and 6.
EVALUATION AND ASSESSMENT
The number of community pharmacy-based diabetes DSM programs established by the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences in partnership with rural and under-served Colorado communities grew from 3 programs in 2007 to 11 programs in 2011, and an additional program was established in an urban setting. The 12 diabetes DSM clinics provided 6-week APPE training opportunities to 120 students during the 2010-2011 academic year.
The clinics provided care to 1,283 patients who had an average 5.7-year history of diabetes prior to attending a pharmacy-based DSM clinic for their first appointment. Four hundred ninety-five patients (∼39%) completed 6 or more visits and 31% of patients (246/788) who did not complete 6 or more visits completed only 1 visit. Of the 495 patients, 417 had 1 or more laboratory measurement values at baseline and 6 months that fit the defined criteria (laboratory values measured within 30 days of the visit, or with A1c 45 days before or 30 days after the visit) to be included in the data set for analysis.
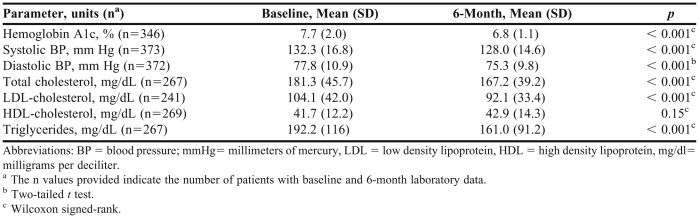
Health outcome data for the 417 patients are reported in Table 1. The patients demonstrated clinically significant improvements in A1c levels, systolic and diastolic blood pressure, total and LDL-cholesterol, and triglycerides at 6 months compared to baseline, but did not demonstrate any difference in HDL-cholesterol values. Mean A1c values were above the national ADA guideline goal (7.7%) at baseline and below that goal (6.8%) at the 6-month assessment. For the 346 patients with both baseline and final A1c measures, baseline A1c measures ranged from 5.1% to 16.9% and 6-month A1c measures ranged from 4.6% to 10.9%. Patients were more likely to have A1c values below 7% at the final visit (n = 227) than at baseline (n = 155; odds ratio = 2.4, 95% CI = 1.7 - 3.2; p < 0.01).
Table 1.
Laboratory Values in Patients With Diabetes Who Participated in Disease State Management Clinics Provided by Pharmacy Students
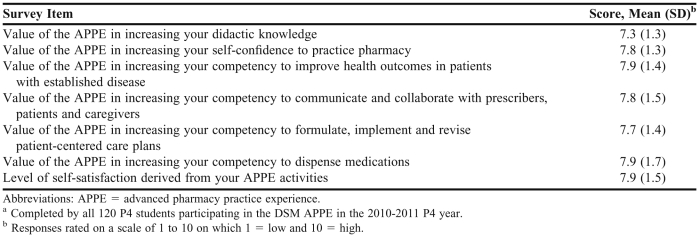
A Blackboard (Blackboard Learn, Washington DC) software-based survey tool was used to assess students’ perceptions of their diabetes DSM clinic experiences. The survey was administered at the end of the 6-week APPE experience to all students who completed a diabetes DSM clinic practice experience during the 2010-2011 academic year.
All 120 students who completed a DSM APPE experience in 2010-2011 completed the perception survey after the experience (Table 2). The students’ responses regarding their APPE experiences at the diabetes DSM clinics were positive. They gave high scores to the self-satisfaction they derived from their activities at the clinics and to the value of the clinics in increasing their competency to improve health outcomes in patients with established disease; in their competency to communicate and collaborate with prescribers, patients, and caregivers; and in their competency to formulate, implement, and revise patient care plans. Based on their responses, they felt the level of performance and the level of responsibility demanded by their experiences were appropriate and that the value of the sites in providing sufficient numbers of patients and opportunities to interact with other healthcare professionals was good. They gave high scores to the value of the sites in increasing their competency to prepare and dispense medications. In comparison to other ratings, the students gave a lower rating to the value of their experiences in increasing their overall classroom knowledge. Approximately half of the students reported that the experience had a favorable impact on their willingness to pursue a rural pharmacy practice career.
Table 2.
Pharmacy Students’ Perceptions of an Advanced Pharmacy Practice Experience in a Community Pharmacy-Based Diabetes Disease-State Management Programa
DISCUSSION
Accreditation standards for US PharmD programs state that graduates must be able to contribute to the care of patients and to the profession by practicing with competence and confidence in collaboration with other health care providers.1 This paper, building on earlier work,2 provides further evidence that a pharmacy school can create advanced pharmacy practice experiences that give large numbers of students experience in providing direct patient care in a disease-state management setting as part of a healthcare team. It also demonstrates that a pharmacy school can form partnerships with rural communities to enhance healthcare resources in healthcare professional shortage areas, and that students can be effective change agents in the development of clinical pharmacy programs.1
The diabetes DSM clinics provided students with the opportunity to work as part of healthcare teams comprised of patients, providers, community pharmacists, and other pharmacy students that delivered meaningful improvements in patients’ health outcomes. The observed improvements in patients’ hemoglobin A1c levels, blood pressure, and lipid values (other than HDL-cholesterol values) were clinically significant and achieved over a 6-month period in a population of patients with an average 5.7-year history of diabetes prior to accessing community pharmacy-based DSM services. Date range limitations were placed on the objective laboratory data analysis to make sure that the patients whose data were analyzed had appropriate values that could be considered drawn at baseline and at 6 months. It was agreed upon that lipid and blood pressure values must have been drawn within 30 days of the first and last visit, and that A1c values must have been drawn within 45 days before or 30 days after those visits. Patients lacking data within these timeframes were excluded from analysis on that laboratory. The students provided face-to-face care to patients referred to the diabetes clinics by their providers as well as patients who sought out pharmacy-based care on their own initiative. The students interacted with patients’ providers through case notes, including in recommendations for ongoing care and changes in patients’ pharmacotherapy. In addition, some students had the opportunity to interact with providers by spending time with them at their practice sites, such as in local hospitals. The students interacted with their preceptors by presenting their cases to them for approval, including their recommendations for changes in pharmacotherapy and other aspects of care. The students interacted with each other as healthcare team members. Each student was onsite at a diabetes clinic for 6 weeks, though the pharmacy-based care of individual patients was conducted over 6 months. Accordingly, new students arriving at the diabetes disease-state management clinics to take over the care of individual patients from previous students were required to read case notes written by the previous students. They in turn were required to write case notes to be read by other students during later practice experiences.
It is important to give patient care responsibilities to students but it is important to recognize that they are inexperienced student practitioners. For example, students need more time than an experienced practitioner to complete tasks and, though they were expected to improve over time, they were given an hour at the start of their diabetes DSM clinic practice experiences to complete their case notes for each patient. Similarly, it was important for preceptors to support students in their activities. The Internet-based electronic charting software program helped the different clinics be more homogenous in the education and care provided and allowed students to receive feedback from faculty members on their charting, as it was available remotely for viewing. This remote access allowed faculty to perform quality assurance checks to verify students were measuring and recording important information, such as baseline and 6-month laboratory values. Likewise, the 1-day school-based pre-APPE training program helped students quickly orient to the clinic operations when they began the APPE. It allowed them to more efficiently take the lead with the DSM programs, assuming the responsibilities of those students who had recently left the site and reducing the time needed for onsite student orientation.
The student perception data are important because they provide evidence that the students had the self-confidence specified by ACPE in Standards 2007 to accept direct patient care responsibilities as part of a functioning health care team.1 The students accepted that the levels of performance and responsibility demanded by the diabetes DSM APPE were appropriate and it is unlikely they would have done so and derived self-satisfaction from their activities unless they had developed the self-confidence to accept their direct patient care responsibilities. One assessment that provides evidence that students met the competency to accept direct patient care responsibilities is that every student participating in these APPE sites in the 2010-2011 academic year received a grade of “pass” for their experience. While this global assessment considered students’ performance across all aspects of the APPE, of which the DSM component was only one part, there was a strong emphasis on the importance for students to effectively manage the DSM program, and that performance was weighted heavily within the overall APPE assessment. The fact that providers in each of these communities continued to refer patients into the diabetes DSM program and continued to respond to requests for patients’ health information and to therapy recommendations provides further support that students accepted the responsibilities given to them and performed at the level required of them. This is consistent with earlier evidence evaluating physician responses to student recommendations for changes in patients'care.3 The high scores given by students regarding their increased competency to improve patient health outcomes, communicate and collaborate with other professionals and patients, and increased competency in working with patient care plans are all useful quality assurance measures that the diabetes DSM clinics provided appropriate student learning outcomes. The high ratings regarding the value of the sites in increasing their competency to prepare and dispense medications demonstrates that the students’ learning opportunities were not restricted to disease-state management activities. The students gave a lower rating to the value of their experiences in increasing their knowledge in comparison to other ratings, but the primary purpose of the diabetes DSM clinics was to give students the opportunity to gain experience and self-confidence in the application of knowledge acquired in the classroom rather than the acquisition of that knowledge. Further confirming the impact of the program, 6 students who completed an APPE at a diabetes DSM clinic went on to accept pharmacist positions in the same clinics after graduation, including 1 graduate who opened his own rural community pharmacy and requested help from the pharmacy school with establishing a diabetes DSM clinic.
Based on the knowledge that pharmacy-based diabetes DSM programs have been shown in controlled trials to improve patients’ health outcomes,4-8 this study was designed to expand healthcare resources in underserved communities in Colorado and provide student learning opportunities rather than to demonstrate the effectiveness of pharmacy-based DSM clinics in improving patient health outcomes. Accordingly, the improved patient health outcomes observed in the study are attributable to the healthcare team (patients and their caregivers, providers and pharmacists, and pharmacy students) and further work is required to determine the improved health outcomes attributable to the pharmacy students and their preceptors. Nonetheless, the patients at the time of their first visit to a pharmacy-based diabetes DSM clinic had been diagnosed with diabetes for approximately 6 years, yet within the next 6 months they achieved significant improvements in glycemic, blood pressure, and lipid control. There would be little value in operating the diabetes DSM clinics if patient health outcomes did not improve.
A full discussion of patients’ adherence to treatment is beyond the scope of this paper but non-adherence to various forms of treatment including patients with cardiovascular disease or at high risk for cardiovascular disease is common and the 61% non-adherence rate (failure to complete the self-care education program) observed in this study is well within the range of non-adherence to treatment reported by other investigators.9-12 The percentage of patients who did not complete the program varied from clinic to clinic but was highest in the clinics that served indigent populations, including homeless people and migrant farm workers. The program was free, but many patients lived some distance from the nearest clinic site and 6 visits may have posed financial and logistical challenges. The nature of the interaction between patients and students might have influenced some patients to withdraw from the program. Due to the 6-week practice experiences, patients who completed 6 visits over 6 months interacted with as many as 4 different students. This was explained to the patients at their first visit, but lack of continuity (ie, not seeing the same student at each visit) may have influenced program adherence. In addition, the self-management education program did not take patients’ preferences into account. Some patients may have preferred the program to be conducted over a shorter time span and some may have preferred and benefitted from peer support in groups rather than one-on-one education.
The study was limited in that it did not track the effectiveness of patients’ management of their diabetes beyond the end of the self-care education program. It is important to maintain as well as achieve targets for the care of diabetes. For the overall effectiveness of the self-care education program to be determined, it will be important to track patients’ laboratory measures of care beyond the end of the delivery of the program. Integration of follow-up visits on an annual or semi-annual basis may help with this tracking and would be consistent with national guidelines that recommend that diabetes education should reoccur yearly.
CONCLUSIONS
A statewide group of pharmacy-based diabetes DSM clinics were established to serve rural and underserved Colorado communities and provide direct patient care responsibilities for 120 students per year in APPE training. The clinics allowed students to function as part of healthcare teams comprised of patients and their caregivers, providers, community pharmacists, and other pharmacy students. The students accepted responsibility for and received satisfaction from their DSM responsibilities and reported positive learning outcomes. Patients with diabetes who were cared for by the student-supported healthcare teams demonstrated clinically significant improvements in A1c, blood pressure, total cholesterol, LDL-cholesterol, and triglyceride values.
ACKNOWLEDGEMENTS
The work described in this paper was supported by financial contributions from the Caring for Colorado Foundation, the Colorado Department of Public Health and Environment, the Colorado Health Foundation, the Colorado Trust Foundation, Herman and Ethel Horwich Charitable and the Kaiser Permanente Foundation.
REFERENCES
- 1.Accreditation Counsel for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Effective July 1, 2007. https://www.acpe-accredit.org/standards/default.asp. Accessed February 10th, 2012.
- 2.Turner CJ, Ellis S, Giles J, et al. A strategy to develop advanced pharmacy practice experiences. Am J Pharm Educ. 2007;71(3):Article 46. doi: 10.5688/aj710346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCollum M, Nuffer W, Ellis SL, Turner CJ. Physician acceptance of pharmacotherapy recommendations made by pharmacy students in a rural pharmacy-based diabetes care and education clinic. Am J Pharm Educ. 2009;73(2):Article 24. doi: 10.5688/aj730224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knapp K, Ray M, Law A, Okamoto M, Chang P. The role of community pharmacies in diabetes care: eight case studies. California HealthCare Foundation. 2005 [Google Scholar]
- 5.Ragucci K, Fermo J, Wessel A, Chumney E. Effectiveness of pharmacist-administered diabetes mellitus education and management services. Pharmacotherapy. 2005;25(12):1809–1816. doi: 10.1592/phco.2005.25.12.1809. [DOI] [PubMed] [Google Scholar]
- 6.McCord A. Clinical impact of a pharmacist-managed diabetes mellitus drug therapy management service. Pharmacotherapy. 2006;26(2):248–253. doi: 10.1592/phco.26.2.248. [DOI] [PubMed] [Google Scholar]
- 7.Fera T, Bluml B, Ellis W. Diabetes Ten City Challenge: Final economic and clinical results. J Am Pharm Assoc. 2009;49(3):383–391. doi: 10.1331/JAPhA.2009.09015. [DOI] [PubMed] [Google Scholar]
- 8.Chisholm-Burns MA, Lee JK, Spivey CA, et al. US Pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48(10):923–933. doi: 10.1097/MLR.0b013e3181e57962. [DOI] [PubMed] [Google Scholar]
- 9.Simon N, Bennett K, Feely J. A review of studies of adherence with antihypertensive drugs using prescription databases. Ther Clin Risk Manag. 2005;1(2):93–106. doi: 10.2147/tcrm.1.2.93.62915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grassi G, Seravalle G, Mancia G. Cardiovascular consequences of poor compliance to antihypertensive therapy. Blood Pressure. 2011;20(4):196–203. doi: 10.3109/08037051.2011.557902. [DOI] [PubMed] [Google Scholar]
- 11.Mauskop A, Borden WB. Predictors of statin adherence. Curr Cardiol Rep. 2011;13(6):553–558. doi: 10.1007/s11886-011-0221-2. [DOI] [PubMed] [Google Scholar]
- 12.Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011;65(3):314–322. doi: 10.1111/j.1742-1241.2010.02544.x. [DOI] [PubMed] [Google Scholar]