Abstract
Objectives. To evaluate the impact of student pharmacists delivering medication therapy management (MTM) services during an elective advanced pharmacy practice experience (APPE).
Methods. Student pharmacists provided MTM services at community pharmacy APPE sites, documented their recommendations, and then made follow-up telephone calls to patients to determine the impact of the MTM provided. Students were surveyed about the MTM experience.
Results. Forty-seven students provided MTM services to 509 patients over 2 years and identified 704 drug-related problems (average of 1.4 problems per patient). About 53% of patients relayed the recommendations to their physician and 205 (75%) physicians accepted the recommendations. Eighty-eight percent of patients reported feeling better about their medications after receiving MTM services. A majority of the students perceived their provision of MTM services as valuable to their patients.
Conclusions. Providing MTM services to patients in a pharmacy practice setting allowed student pharmacists to apply skills learned in the doctor of pharmacy (PharmD) curriculum.
Keywords: medication therapy management, experiential education, doctor of pharmacy program, advanced pharmacy practice experience, community pharmacy
Medication therapy management (MTM) was established by the Center for Medicare and Medicaid Services (CMS) under the Medicare Modernization Act of 2003 with the goal of producing optimal therapeutic outcomes and reducing adverse drug events for Medicare Part D beneficiaries.1 Pharmacist involvement in patient care improves health outcomes and medication adherence rates while reducing adverse drug events.2,3 Community pharmacists, in particular, are in an ideal position to provide MTM services, as they have the opportunity to interact with their patients every 1 to 3 months when patients come into the pharmacy to refill their prescriptions.2 Although there are some examples of successful MTM community pharmacy practices, the provision of MTM services in community pharmacies is not widespread nor is it considered standard practice.4 In 2010, the American Pharmacists Association (APhA) found that one of the greatest barriers to pharmacists providing MTM services was not having adequate time.5 Pharmacists not providing MTM reported that lack of time, insufficient staffing levels, and a high level of dispensing activities were major challenges.5
According to the Accreditation Council for Pharmacy Education (ACPE) standards, required advanced pharmacy practice experiences (APPEs) should emphasize the need for continuity of care throughout the health care delivery system.6 One of the characteristics recommended for community APPE sites is that they provide medication therapy management and patient care services for diverse populations.6 Community pharmacists’ inability to implement MTM services means that students do not have opportunities to observe or be involved in the development, implementation, and provision of MTM services during practice experiences.7 Dugan proposed in 2006 that student pharmacists on APPEs could enhance community pharmacy services.8 Incorporating MTM in the curriculum and using active-learning strategies may improve student confidence and their perceived ability to provide these services.9,10 However, to our knowledge, there have been no studies that examined implementation and documentation of MTM services provided by student pharmacists to patients in the community pharmacy setting through the experiential curriculum.
The authors, all faculty members at Western University of Health Sciences College of Pharmacy, proposed incorporating MTM into the college's experiential program as a possible solution to some of the concerns mentioned. The authors are part of a collaborative research team at the institution called the Community Pharmacy Research and Education or CORE group whose mission is “to advance community pharmacy practice to improve patient outcomes and pharmacist professional recognition.”
APPEs at the college take place over 15 months, starting in the second half of the third year of the PharmD program. Students complete seven 6-week APPEs, followed by a final 12-week advanced elective course just prior to graduation. Students can choose 1 of 3 “tracks” for the 12-week APPE: institutional setting, community pharmacy, or independent pharmacy ownership. These tracks are designed to provide students with an advanced, more concentrated experience in a practice setting in which the student is considering working after graduation. The goals of the community pharmacy track are to ensure that the student pharmacist receives adequate exposure to pharmacy practice and is prepared to perform pharmacist-in-charge duties, MTM, and other direct patient care services. The independent pharmacy ownership track is designed to offer specialized training in community pharmacy ownership through onsite experience, self-directed learning, and team work in addition to completing the pharmacist-in-charge and MTM modules.
An MTM project was added to the APPE community pharmacy and independent pharmacy ownership tracks in 2009 to determine the feasibility of implementing MTM services at the pharmacies, as well as to examine students’ confidence levels in providing MTM. The rationale was that if students are trained in the classroom in MTM and are capable of providing MTM services in a pharmacy under the direct supervision of preceptors, then it is feasible for community pharmacy preceptors to implement these services at their sites, knowing that the student pharmacists’ assistance will allow the preceptors to focus on their dispensing activities. At the same time, an MTM program would provide students with the opportunity to experience delivering MTM in a patient care setting. The purpose of this study was to evaluate the impact of these MTM services delivered by student pharmacists during their 12-week APPE on student perception of value and preparation for provision of MTM; and on patient response to the recommendations.
METHODS
Student pharmacists who registered for the community pharmacy and independent pharmacy ownership advanced experience tracks were asked to provide these services at their community pharmacy sites from mid-February to the first week of May during 2009 and 2010. Participation in the MTM project was not mandated as a requirement for students to pass the APPE as some practice sites had constraints that prevented them from offering MTM.
The concept of MTM was introduced to students in their first year of pharmacy school. After completing most of their therapeutics courses, students spent a full day of class in their third year learning how to perform MTM services. Prior to starting the APPE, student pharmacists were trained by the CORE faculty members for a day on how to implement MTM services at a practice site and how to document the process on MTM forms. These forms were developed by the CORE faculty members based on APhA suggested standards and are available upon request.
An MTM protocol, created by the CORE faculty members, was incorporated into the course syllabus for added guidance. Patients interested in receiving MTM services completed a medical and medication history form, which was then reviewed by student pharmacists. Within 3 days, the student pharmacists conducted a face-to-face interview with the patient and performed a medication therapy review to address the appropriateness, safety, and cost, and any compliance issues associated with the patient's medications. Students documented the drug-related problems they found, specifically in the following areas: drug use without indication, or duplication of therapy; untreated indication; improper drug selection; subtherapeutic dosage; overdosage; inappropriate administration schedule; adverse drug reaction; drug interaction; and cost-effectiveness. The students provided their patients with a written report addressed to the patient's physician with suggested changes and/or safety concerns, which were approved by the student's preceptor. While the preceptor was not required to interview the patient with the student, the preceptor did need to review and sign off on every recommendation before it was presented to the patient. The patient was also provided with a typed personal medication record that was prepared by the student and approved by the preceptor.
Students followed up with the patient, either by phone or in person, in 1 to 2 weeks after the MTM session. The follow-up questions were designed to track patient-reported outcomes including whether the patient took the student's advice, whether the patient gave the recommendations to their physician, whether the physician accepted the recommendations, and whether the patient felt better about their medication therapy as a result of the service.
After follow-up, students transferred relevant de-identified data per Health Insurance Portability and Accountability Act regulations, into a database that listed interventions and outcomes per patient. A unique identifier code was used to link patient data to the patient's personal medication record. The record was stored securely in the pharmacy and only the Excel file was sent to the study investigators for analysis. Students only sent data for those patients who were reached for follow-up. If a patient could not be reached for follow up, his/her data were not included in the analysis. The study and the tools received investigational review board exempt approval from the university.
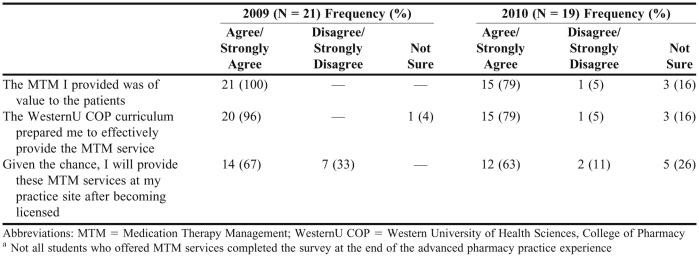
A survey instrument was also administered to students to determine their perceived value of the MTM project, the role of the curriculum in adequately preparing them for providing MTM, and whether they intended to continue these services in practice. Twenty-one student pharmacists who participated in the MTM program in 2009 and 19 who participated in 2010 responded to the survey (Table 2).
Table 2.
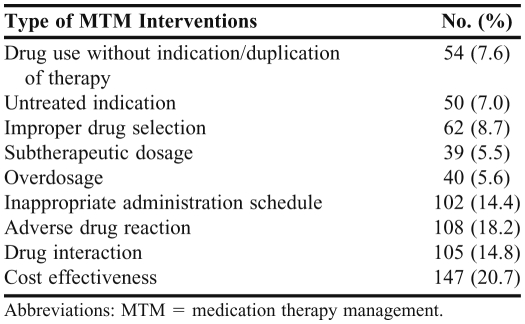
Frequency of Different Types of MTM Interventions Over Two Years (N = 707)
The data received were collated and analyzed using IBM SPSS, version 17.0 for Windows, (SPSS for Windows, Chicago, IL, 2009). Analysis was primarily descriptive in nature, and included summarizing information from student reports and course surveys and comparing data between years using Student t tests at a 95% significance level.
RESULTS
Over the 2-year study period, of 281 student pharmacists completing the APPE, 67 registered for the community pharmacy track and 67 registered for the independent pharmacy ownership track. Not all of the 134 student pharmacists in these 2 tracks were allowed to provide MTM services at their practice site. Of those student pharmacists who did provide MTM, a few failed to report the data collected to the college.
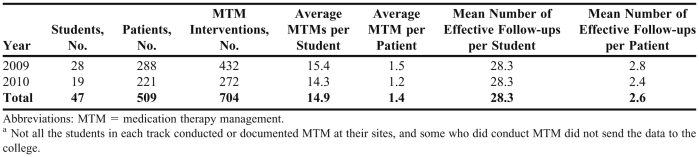
Table 1 presents the data collected from the students who were able to integrate MTM services at their practice experience site. Five hundred nine patients received MTM services, or an average of 10 patients per student. Among the 509 patients, 704 drug-related problems were identified (an average of 1.4 drug-related problems per patient). Each student identified an average of 15 drug-related problems for their MTM patients. There were no significant differences between data for 2009 and 2010 in terms of the average number of MTM services provided (p = 0.09) or follow-up interviews conducted (p = 0.18).
Table 1.
Student Pharmacists’ Provision of Medication Therapy Management at Pharmacy Practice Sites During an Advanced Elective Coursea
Table 2 presents the most common drug-related problems identified by the students: cost effectiveness (n = 146), adverse drug reactions (n = 116), drug interactions (n = 106), and inappropriate administration schedule (n = 102). The least common drug-related problems identified were overdosage (n = 40) and subtherapeutic dosage (n = 39).
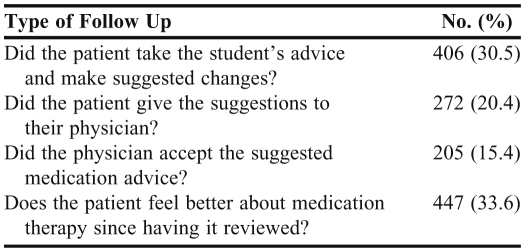
As shown in Table 3, of the 509 patients seen across 2 years, 406 (80%) accepted the student pharmacists’ advice and 272 (53%) presented/relayed the student's recommendations to their physician. Two hundred five (75%) physicians accepted the student pharmacists’ recommendations. In addition, 447 (88%) of the patients responded that they felt better about their medications after receiving MTM services.
Table 3.
No. of Effective Follow-Ups by Students Over Two Years (N = 1330)
As seen in Table 4, 100% of the student pharmacists in 2009 perceived that the MTM services they provided were valuable to their patients compared with 79% of student pharmacists in 2010 (p < 0.05). There was no significant difference between the percentage of students across the 2 years who believed that the pharmacy school curriculum had prepared them to effectively deliver MTM services (96% in 2009 versus 79% in 2010; p = 0.14). Similarly, there was no difference in the response to whether they would provide MTM services as licensed pharmacists in the future (67% in 2009 and 63% in 2010; p = 0.82).
Table 4.
Student Pharmacists’ Perceptions About Providing Medication Therapy Management to Actual Patients During an Elective Advanced Pharmacy Practice Experiencea
DISCUSSION
This study shows that student pharmacist provision of MTM services at community pharmacy sites during APPEs is feasible. Even in the limited amount of time that the students in our study were at the community pharmacy sites, they were able to make a significant number of MTM interventions that benefited patients. The majority of patients felt better about their medications after talking with the students. This may have been because they left the pharmacy with a better understanding of the importance of taking the medication, how to take the medications, and what to do if they experienced a side effect of the medication. Because the investigators did not have access to the patients’ medical records or health insurance claims, the extent of this impact on the overall health of the patients and health care costs could not be evaluated.
About half of the patients took the students’ MTM recommendations to their physicians, and in those cases, about three-fourths of the physicians made changes to the patient's medication therapy. This finding points to the importance of pharmacists not only as providers of MTM, but also as members of the interprofessional health care team. It also points to the effectiveness of MTM. There may be some bias in our results related to the follow-up data because the student pharmacist who performed the MTM intervention also conducted the follow-up telephone call with the patient to record the patient's response to the recommendations.
By having this MTM requirement as part of the community pharmacy and independent pharmacy ownership APPE, we were able to see advantages that addressed the aforementioned concerns. First, students were able to gain real-life experience practicing MTM on patients under the supervision of a preceptor. All of the students in 2009 and a majority of students in 2010 who responded to the survey perceived that the MTM services provided were valuable to the patient. Second, most of our students felt that they had been adequately prepared to provide MTM services by what they learned through the pharmacy curriculum. This finding addresses the concerns of those providers who feel that inadequate training and/or experience, or difficulty in documenting services, are barriers to implementing MTM services.5 Even if community pharmacy preceptors are not familiar with the process of conducting MTM, they have the knowledge to approve clinical recommendations that are identified by student pharmacists. This may address both the efficiency of the process in terms of time, as well as improve preceptor confidence in participation in MTM. Finally, most of the students mentioned that they would be willing to continue providing MTM services as licensed pharmacists if they were given the chance. Whether they will provide MTM services is dependent on a number of factors, such as reasonable reimbursement from payers, but at least the students recognize the value of such a service to their patients and express a desire to provide this service as a pharmacist.
A potential concern with this method is the level of supervision that is provided as it is the student and not the pharmacist who handles the majority of the workload. In California, direct supervision of student pharmacists means that a pharmacist is on the premises at all times and is fully aware of all activities performed by the student serving as an intern pharmacist.11 With the preceptor having to review and sign off on all recommendations made by the student, each participating student providing MTM would be considered to be under the direct supervision of the pharmacist. Programs planning to implement MTM services provided by student pharmacists would need to ensure that the student pharmacists’ role was in line with state regulations regarding intern pharmacists.
Some challenges were encountered during this initial implementation phase that will need to be addressed. Some preceptors were hesitant to let student pharmacists provide MTM services at their pharmacies because they were not comfortable with providing these services. We intend to alleviate these concerns by offering preceptor training courses focused on how to work with students to incorporate MTM services at pharmacy practice sites. We also plan to survey preceptors at the end of the APPE about their perceptions of the program and the value of offering these services at their practice site.
Many of the students communicated their recommendations to the physician through the patient. Ideally, MTM should involve direct collaboration among all participating health care providers. We plan to have student pharmacists send their recommendations directly to the physician and then follow up with a phone call to the physician's office. Future research may include surveying physicians about their perceptions of pharmacists providing MTM services.
Student participation has also proved to be a challenge. There were variable levels of motivation and enthusiasm among students about providing MTM services at their APPE sites. We have incorporated an “opt out” process where all students must participate in the program unless there is documentation from the preceptor that the pharmacy declined to participate in the MTM service. To encourage students to be diligent in providing us with MTM data in a timely manner, we require that they submit all collected data in order to pass the APPE. The data sheet has been revised to improve ease of data collection and input. We also plan to evaluate the financial implications for the pharmacy of having students pharmacists provide MTM services.
Some key data collection concerns also need to be examined. For example, information on patient characteristics (number of prescription medications, demographics, etc) was not collected because of time constraints. Also, the lack of student access to laboratory values made it difficult to determine the efficacy of medication therapies. We may try to address this in the future by having the students provide point-of-care testing of blood pressure, fasting blood glucose, A1C level, and cholesterol levels. We plan to have the students request the most recent laboratory tests from the patient or the patient's physician. Also, we have expanded the elective APPE from 12 weeks to 16 weeks. This should provide sufficient time to monitor patients and measure the impact of the student pharmacists’ interventions.
We plan to continue to collect data on the MTM services that students provide during the APPE. We did not report 2011 findings from the MTM program here because of gaps in the data resulting from logistical changes that took place within the college. However, based on the data that were collected, the results for 2011 were similar to those for 2009 and 2010. A longitudinal MTM program such as the addition of a 6-week APPE has been considered by the college to allow more effective continuity of care for patients and collection of long-term data. However, such a program would be difficult to coordinate given the variability in APPE offerings at different practice sites and the possibility that a student may not be assigned to every site to provide MTM services during some months. Therefore, our current plan is to continue to make the MTM program an activity only for students in the APPE.
CONCLUSIONS
An MTM module, as part of an advanced pharmacy practice experience elective course, provided student pharmacists with the opportunity to practice skills learned during the pharmacy curriculum. Provision of MTM services by students allowed community pharmacy sites to implement MTM services for 12 weeks. These services identified drug-related problems that may not have been previously identified by the pharmacy or the patients’ physicians, and many of the patients left feeling better about their medications as a result of the MTM services provided. Student pharmacists felt adequately prepared to provide MTM services at the practice sites and recognized the value of providing these services to their patients.
REFERENCES
- 1.Centers for Medicare and Medicaid Services (CMS) HHS. Medicare program; medicare prescription drug benefit, Final Rule. Federal Register. 2005;70:4193–4585. [PubMed] [Google Scholar]
- 2.Pindolia VK, Stebelsky L, Romain TM, et al. Mitigation of Medication Mishaps via Medication Therapy Management. Ann Pharmacother. 2009;43(4):611–20. doi: 10.1345/aph.1L591. [DOI] [PubMed] [Google Scholar]
- 3.Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Arch Intern Med. 2003;163:2014–8. doi: 10.1001/archinte.163.17.2014. [DOI] [PubMed] [Google Scholar]
- 4.Thomas J, Zingone MM, Smith J, et al. Feasibility of contracting for medication therapy management services in a physician's office. Am J Health-Syst Pharm. 2009;66(15):1390–3. doi: 10.2146/ajhp080464. [DOI] [PubMed] [Google Scholar]
- 5.American Pharmacists Association. Medication Therapy Management Digest Tracking the Expansion of MTM in 2010: Exploring the Consumer Perspective. http://www.pharmacist.com/AM/Template.cfm?Section=MTM&CONTENTID=25712&TEMPLATE=/CM/ContentDisplay.cfm. Accessed January 13, 2012.
- 6.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree: Version 2.0. January 23, 2011. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed January 13, 2012.
- 7.Rodis JL, Legg JE, Casper KA. Partner for Promotion: an Innovative Advanced Community Pharmacy Practice Experience. Am J Pharm Educ. 2008;72(6):Article 134. doi: 10.5688/aj7206134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dugan BD. Enhancing community pharmacy through advanced pharmacy practice experiences. Am J Pharm Educ. 2006;70(1):Article 21. doi: 10.5688/aj700121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuhn C, Powell PH, Sterrett JJ. Elective course on medication therapy management services. Am J Pharm Educ. 2010;74(3):Article 40. doi: 10.5688/aj740340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eukel HN, Skoy ET, Frenzel JE. Provision of medication therapy management to university faculty and staff members by third-year pharmacy students. Am J Pharm Educ. 2010;74(10):Article 182. doi: 10.5688/aj7410182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.California State Board of Pharmacy. 2012 Lawbook for Pharmacy. http://www.pharmacy.ca.gov/laws_regs/lawbook.pdf. Accessed January 13, 2012.