Abstract
We conducted two studies to examine the Cognition Checklist for Mania—Revised (CCL-M-R; Beck, Colis, Steer, Madrak, & Goldberg, 2006). In the first, we gathered data in an undergraduate sample (N = 208) to examine the factor structure of the measure and the correlations of the subscales with the Hypomanic Personality Scale (HPS; Eckblad & Chapman, 1986). Factor analyses refined subscales, and three of the original four subscales developed by Beck and colleagues (2006) were retained. Persons with higher stores on the HPS were likely to endorse manic cognitions associated with overconfidence and excitement-seeking. In a second study, we gathered data from 61 persons diagnosed with bipolar I disorder, 38 with major depressive disorder (MDD), and 33 with no history of mood disorder. Excitement-seeking scores were robustly related to current manic symptoms, as measured by the Internal State Scale (ISS; Bauer et al., 1991). Thus, CCL-M-R excitement-seeking scores appear to be related to risk for mania and to current symptoms of mania within a clinical sample. Other findings, though, suggest that problems with interpersonal relationships (feeling thwarted by others) may emerge among those clinically diagnosed with bipolar I disorder, even though not endorsed among those at risk. Moreover, difficulties with interpersonal relationships and diminished confidence in those with bipolar I disorder paralleled the difficulties observed among those with MDD. Findings suggest that cognitive profiles associated with mania may depend on mood state and course of the disorder.
Although there is no doubt that biological variables contribute to the pathogenesis of bipolar disorder, psychological variables have been repeatedly shown to influence the timing and course of episodes. These findings have prompted researchers to develop psychological interventions to augment medication treatments. Most of this research has been conducted on cognitive interventions for bipolar disorder, with the rationale being that these treatments can help patients modify cognitive biases associated with the disorder (Basco & Rush, 1996; Lam, 2003; Leahy, 2003; Newman, Leahy, Beck, Reilly-Harrington, & Gyulai, 2002; Scott, 1996).
Consistent with Beck’s model (1976), researchers have shown that both bipolar and unipolar depression are associated with a negative cognitive style. That is, people with bipolar disorder who are currently depressed tend to endorse more negative automatic thoughts and dysfunctional attitudes than do those without a history of mood disorder (Hollon, Kendall, & Lumry, 1986; Scott & Pope, 2003; Seligman et al., 1988). They also tend to remember more negative memories when depressed than when they are not depressed (Eich, Macaulay, & Lam, 1997; Weingartner, Miller, & Murphy, 1977). Cognitive biases also appear to be present in people with bipolar disorder during remission. That is, those with bipolar disorder have been found to demonstrate increased attention to negative words compared to normal controls, even when not currently in a negative mood state (Bentall & Thompson, 1990; Lyon, Startup, & Bentall, 1999). Some research suggests that the negative cognitive profiles observed among those with bipolar disorder are highly related to the extent of depressive symptom history (Alloy, Reilly-Harrington, Fresco, Whitehouse, & Zechmeister, 1999).
On the other hand, some researchers have suggested that mania may involve positive biases in cognition (Beck & Weishaar, 1995; Leahy, 1999). For example, people with bipolar disorder exhibit increased attention to positive words (Murphy et al., 1999) and more recall of positive than negative memories (Eich et al., 1997) during periods of mania. During remission, people with bipolar disorder have been found to endorse higher goals in laboratory tasks (Johnson & Carver, 2006) and unrealistic lifetime ambitions (Johnson, Ruggero, & Carver, 2003) than those without bipolar disorder.
Beyond these relatively constant aspects of manic cognition, a series of studies suggest that people with bipolar disorder and those at risk for mania tend to show overly positive cognitive styles as their mood state shifts. That is, researchers have noted that those at risk for mania have a tendency to ruminate on the meaning of positive moods (Feldman, Joormann, & Johnson, 2008), to over-interpret the meaning of small successes (Eisner, Johnson, & Carver, 2008), and to be overly confident when in a positive mood state (Lam, Wright, & Sham, 2005; Mansell & Lam, 2006). Recent factor-analytic evidence suggests that these three facets of state-dependent cognition are independent and that each adds unique variance to hypomanic risk (Johnson & Jones, in press)., Mansell Rigby, Tai, and Lowe (2008) recently found that hypomanic symptoms were correlated with the tendency to endorse a broad range of cognitive statements, including statements regarding consequences of the positive moods (e.g., not being responsible for dealing with the moods, not being understood, not eating), loss of control over moods, diminished tearfulness (when I feel excited, my fears and worries are no longer real), and response styles to positive moods (mood-related increases in idea generation). Indeed, one recent focus has been on understanding the cognitive processes involved in the manic ascent, and to provide interventions tailored toward these issues (Mansell & Pedley, 2008).
A key question, then, is which types of cognitive content are most evident when positive mood states increase for a person with bipolar disorder. Recently, a scale was created to measure the severity of maladaptive beliefs and cognitions during mania: the Cognition Checklist for Mania—Revised (CCL-M-R; Beck et al., 2006). The CCL-M-R was generated by gathering expert opinion about manic statements in a range of domains: the self (Myself), relationships (Relationships), high-risk behaviors (Pleasure/excitement), and goal-driven activities (Activity). In the initial validation study, the CCL-M-R was shown to be internally consistent, and the Myself, Relationships, and Activity subscale scores differentiated between patients admitted to the hospital with the most recent episode classified as manic, mixed, or depressed (Beck et al., 2006). In sum, the newly developed CCL-M-R represents a potentially meaningful clinical tool for identifying the Types of cognitions displayed by persons with bipolar disorder during mania.
Research to date, though, has not assessed several key issues regarding these cognitive patterns. First, in the original validation article, subscales were developed based on face validity, but no study to date has examined the factor structure of the CCL-M-R. Second, it is not known whether items on this scale capture cognitive reactions to having a mood disorder, with all of its consequent effects on a person’s lifestyle; a core goal is to test whether these cognitive patterns can be observed among people at risk for mania. Third, it is not known whether the scale helps to differentiate people with bipolar disorder from those with other mood problems. As such, it is not clear whether this questionnaire could help to identify people with bipolar disorder. Fourth, to the extent that the scale is sensitive to small shifts in mood, it may be more helpful as a tool for clinical prevention of mania. To this aim, we tested whether the scale was correlated with low levels of manic symptoms.
To examine the preceding issues, the present research included two studies. The first study was designed to examine the factor structure of the CCL-M-R using Confirmatory Factor Analysis (CEA) within an undergraduate sample. It was hypothesized that the original subscales would hold, with modifications made to items that did not load well onto the previously theorized factors. We sought to identify the core items of this scale (i.e., those that described significant variance in, and loaded best on, their respective factors). We hypothesized that the confirmed CCL-M-R factors related to manic vulnerability (as measured by the Hypomanic Personality Scale; Eckblad & Chapman, 1986).
In the second study, we applied the factor-analyzed version of the CCL-M-R to a clinical sample of people with bipolar I disorder, those with major depressive disorder (MDD), and those with no history of mood disorder. We examined the relationship between CCL-M-R subscales, diagnosis, and current symptoms. We hypothesized the following: that those with bipolar I disorder would show significantly higher scores on all three factors of the CCL-M-R than those without a history of mood disorder, and that symptoms of current mania (as assessed by the Internal State Scale – Activation subscale) would interact with bipolar disorder status in predicting CCL-M-R scores.
STUDY 1: CFA OF THE CCL-M-R
In Study 1 we examined the factor structure of the CCL-M-R within an undergraduate sample. We sought to identify the core items of this scale and place the confirmed factors within a hybrid structural equation model to examine their relationships to manic vulnerability. It was hypothesized that manic cognitions would relate to mania risk.
Method
Participants
Participants were 208 undergraduate students at the University of Miami (60% female). Although age and ethnicity were not recorded, we have no reason to believe this sample was any different from that of the larger University of Miami student population (approximately 55% non-Hispanic white, 23% Hispanic, 8% Asian, 6% African American, and 7% “Other”). Questionnaires in the current study were administered in large groups in partial fulfillment of a course requirement.
Measures
The CCL-M-R consists of 29 items arranged into four subscales based on face validity: Myself (7 items), Relationships (7 items), Pleasure/excitement (9 items), and Activity (6 items). These subscales measure elevated beliefs about one’s self-worth (Myself) and interpersonal relationships (Relationships), excitement-seeking through engaging in high risk behaviors (Pleasure/excitement), and having high energy levels to engage in goal-driven activities (Activity). See Table 1 for specific items, Total scores and subscale scores may be calculated by summing the items (rated on a 4-point scale) across the relevant items.
TABLE 1.
Retained CCL-M-R Subscale Items and Their Factor Loadings
Myself (Confidence)
|
Relationships (Thwarting)
|
Pleasure/Excitement (Excitement-Seeking)
|
Items not included in the final scale
|
Note. All loadings significant at the p < .05 level.
In addition to the CCL-M-R, participants completed the Hypomanic Personality Scale (HPS; Eckblad & Chapman, 1986). The HPS is a 48-item self-report measure that was designed to assess the risk for bipolar spectrum disorders. Specific domains captured by the scale include a history of mild upward shifts in emotions, behavior, and energy. In the initial validation sample, the HPS demonstrated efficacy in identifying people who both currently met diagnostic criteria for bipolar spectrum disorder and who were at risk for bipolar disorders 10 to 13 years later (Eckblad & Chapman, 1986; Kwapil et al., 2000). The HPS has also demonstrated high internal consistency (α = .87) and test-retest reliability 15 weeks later (r = .81; Eckblad & Chapman, 1986). In the present study, internal consistency was high (α = .87).
Results
The initial CHA tested the CCL-M-R model with four factors represented by the four subscales and 29 indicators represented by individual items. This model did not fit the data, (χ2[371] = 966.254, p < .001, CFI = .621, RMSEA = .090, SRMR = .105). The modification indices suggested several correlations between errors that would improve model fit. Several items appeared to be closely related to each other and, in these cases, their errors were correlated (e.g., “I am the best” [7] and “Everything I do is great” [9]). With these changes to the model, fit was improved, but was still not good for the data (χ2[362] = 666.848, p < .001, CFI = .806, RMSEA = .065, SRMR = .093). The difference between model fit was significant, however, so the new model was retained (χ2Δ[9] = 299.406, p < .01).
Next, individual items that did not load well onto factors were reviewed and systematically removed from the model one at a time. This process was repeated until all items with standardized factor loadings less than .50 were removed from the model. This cutoff value was used per recommendations by Marsh and Hau (1999) when using CFA models with relatively small sample sizes (i.e., samples with a case to free parameter ratio less than 20:1). Deleted items included Items 13, 36, 11, 22, 49, 43, 52, 19, 9, 10, 57, 30, 20, and 39. After these modifications, model fit was improved (χ2[81] = 149.443, p < .001, CFI = .904, RMSEA = .065, SRMR = .060). The chi-square difference test was significant, and the new model was retained (χ2Δ[281] = 517.405, p < .01). The next item to be deleted was Item 42, but deletion of this item led to a linear dependency between the Activity and Myself subscales. That is, the two remaining items on the Activity subscale did not explain unique variance above and beyond that explained by the Myself subscale. In line with modification indices, the two subscales were combined to form one factor. The two items that had originally loaded onto the Activity factor (44 and 53) did not load well onto the new factor (approximate λs < .30) and explained little variance (approximate R2 < .20). Items 44 and 53 were therefore deleted from the model.
The final 12-item, three-factor model includes only items that have high loadings (λ > .50) onto their respective factors. In addition, latent factors explain at least 28% of the variance in the remaining 12 items. The final model fit the data reasonably well, although the chi-square test was still significant (χ2[50] = 84.313, p = .0017, CFI = .939, RMSEA = .058, SRMR = .053; see Table 1 for CCL-M-R items with their final factor loadings).
As shown in Table 1, the final model, with the fewer items per subscale, suggests a narrower interpretation of the content of the Myself, Relationships, and Pleasure/excitement scales. More specifically, the Myself items that were retained are most relevant to confidence (Confidence). The Relationship items that were retained are specific to a particular issue in bipolar disorder: being thwarted by others in the pursuit of goals (Thwarting). The Pleasure/Excitement items were more specific to excitement-seeking without attention to potential danger (Excitement-seeking). We labeled these factor scales accordingly.
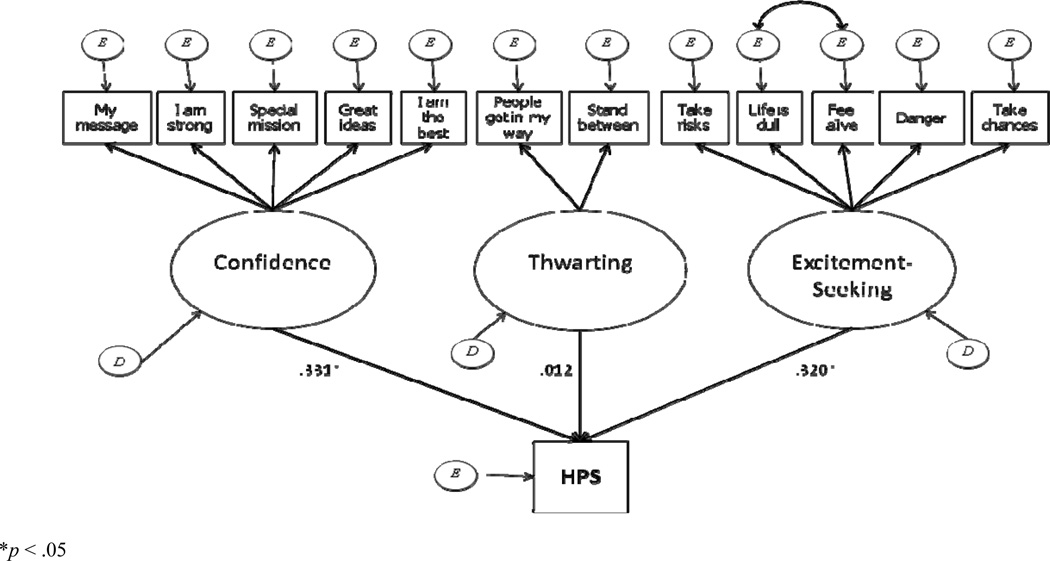
Next, the three modified factors of the CCL-M-R were placed into a hybrid model to examine their relationship with HPS total scores. When the HPS was regressed on the three factors, the model fit the data reasonably well, although the chi-square test was still significant (χ2[59] = 102.227, p = .0004, CFI = .926, RMSEA = .063, SRMR = .058). Modification indices did not suggest any changes to be made to the structural component. Results indicated the HPS total scale related significantly to the Confidence and Excitement-seeking subscales (standardized coefficients = .331 and = .320, respectively, ps < .05). The Thwarting subscale did not relate to the HPS total score (see Figure 1).
Figure 1.
Hybrid Model of the Relationship between the CCL-M-R Factor Structure and the Hypomanic Personality Scale (HPS). (Large ovals represent latent factors; rectangles represent indicators [items] of each latent factor; double-headed arrows among indicators represent correlations among the residual variances of these items. Factor loadings for each indicator are presented in Table 1.)
STUDY 2: THE CCL-M-R IN PEOPLE WITH BIPOLAR I DISORDER, MAJOR DEPRESSIVE DISORDER, AND THOSE WITHOUT A MOOD DISORDER DIAGNOSIS
The goal of Study 2 was to examine the performance of the CCL-M-R in a clinical sample. Persons diagnosed with bipolar I disorder, those diagnosed with MDD, and those with no mood disorder each completed the CCL-M-R. Our goal was to examine whether subscale scores differed by diagnostic group and to examine the role of current symptoms of mania and depression on subscale scores.
Participants and Procedures
Participants in Study 2 included 131 persons recruited from the South Florida community through advertisements in the general media and through referrals from local treatment centers for a study of cognition in bipolar disorder. Of these participants, 61 (37% female) were diagnosed with bipolar I disorder, 38 were diagnosed with MDD (42% female), and 32 (46% female) had no history of mood disorder. The mean ages of the three groups were as follows: bipolar I disorder (42 years), MDD (43 years), and no mood disorder (35 years). Although the mean age of participants in the no mood disorder group was significantly lower than that of the other two groups, analyses indicated no relationship between age and CCL-M-R factor scores. Inclusion criteria included the following: Structured Clinical Interview for DSM-IV (SCID) diagnosis of bipolar I disorder or MDD (or no diagnosis of mood disorder for the healthy control sample), and between ages 18 to 65. Participants were excluded if they were unable to independently and adequately complete self-report measures in English, if there was evidence for neurological conditions that would influence the course of bipolar disorder, or if they were diagnosed with schizoaffective disorder.
Following informed consent procedures, participants were interviewed using the SCID to determine DSM-IV-TR diagnostic status. If eligible for the study, participants then completed the self-report instruments listed in the Measures section that follows. Study procedures were approved by the University of Miami Institutional Review Board. Participants were remunerated for their time in the laboratory.
Measures
Structured Clinical Interview for DSM-IV
(SCID; First, Spitzer, Gibbon, & Williams, 1996). The SCID was used to determine diagnostic status of the participants. This instrument is widely used and demonstrates good inter-rater reliability in samples of bipolar disorder (k = .84; Williams et al., 1992). Before completing SCIDs, interviewers completed extensive didactic and interactive training, including practice interviews, role plays, and co-interviews. All SCID interviews were supervised by Dr. Johnson. Our team has established strong inter-rater reliability and met weekly to review diagnostic concerns.
Internal State Scale
(ISS; Bauer et al., 1991). The ISS is a well-established measure of current symptoms of depression and mania. The scale is composed of four subscales: Activation (ACT), Weil-Being (WB), Perceived Conflict (PC), and Depression Index (DI). ACT scores represent symptoms of mania, with a cutoff score of 200 representing the presence of a current hypomanic/manic episode (Bauer et al., 1991; Bauer, Vojta, Kinosian, Altshulcr, & Glick, 2000; Cooke, Kruger, & Shugar, 1996). In the current study, 31% of those with bipolar I disorder were at or above this score. In addition, WB scores less than 125 validly discriminate those currently experiencing depression from those experiencing mania/hypomania or euthymia (Bauer et al., 1991). In the current study, 47% of those with MDD, and 23% of those with bipolar I disorder, fell below this diagnostic cutoff score. Thus, following suggestion from the scale’s authors, ACT scores were used to identify current symptoms of mania and the WB cutoff score was used to identify depression in the current study.
Cognition Check List for Mania—Revised
Participants were administered the full four-factor, 29-itcm CCL-M-R in the current study. Reliability estimates of the four-factor and three-factor versions of the CCL-M-R were comparable. For the former version, alpha coefficients were as follows: Myself = .84, Relationships = .65, Pleasure/excitement = .88, and Activity = .73. The latter version’s estimates were as follows: Confidence = .83, Thwarting = .83, and Excitement-seeking = .83. Correlations between the three factors were modest (rs = .23 to .33).
Results
Table 2 lists the means and standard deviations of each CCL-M-R factor for the three diagnostic groups as well as total values. To examine the relationship between the three-factor CCI.-M-R scores and diagnostic status, we conducted a multivariate analysis of variance (MANOVA) with the CCL-M-R factors as the outcomes and group status as the predictor. The overall MANOVA indicated group differences in factor scores, F(6) = 4.34, p < .001. Follow-up ANOVA analyses indicated group differences on two of the three factors: Confidence, F(2) = 6.06, p < .01, and Thwarting, F(2) = 3.73, p < .05. No group effect was observed for Excitement-seeking, F(2) = 0.24, p > .05. Contrary to hypotheses, those without a history of mood disorder endorsed significantly higher scores on the Confidence subscale than those with bipolar disorder (t[92] = 2.73, p < .01) and those with MDD (t[69] = 2.92, p < .01). Consistent with hyopotheses, both those with bipolar I disorder and those with MDD endorsed significantly higher scores on the Thwarting subscale than did those with no mood disorder (t[91] = −2.70, p < .01 and t[68] = −2.17, p < .05, respectively). Those with bipolar I disorder did not differ, however, from those with MDD on the Thwarting subscale (t[97] = .73, p > 5).
TABLE 2.
Mean CCL-M-R Subscale Scores and Standard Deviations
| Diagnostic group | Subscale mean | Standard deviation | Sample size |
|---|---|---|---|
| Confidence | |||
| No mood disorder | 7.75 | 3.63 | 32 |
| Bipolar I disorder | 5.41 | 3.55 | 61 |
| MDD | 4.73 | 4.28 | 38 |
| Total | 5.78 | 3.94 | 131 |
| Thwarting | |||
| No mood disorder | 0.50 | 0.88 | 32 |
| Bipolar I disorder | 1.38 | 1.72 | 61 |
| MDD | 1.13 | 1.44 | 38 |
| Total | 1.09 | 1.51 | 131 |
| Excitement-seeking | |||
| No mood disorder | 6.97 | 3.15 | 32 |
| Bipolar I disorder | 6.68 | 3.74 | 61 |
| MDD | 6.36 | 4.01 | 38 |
| Total | 6.66 | 3.66 | 131 |
Note. MDD - major depressive disorder.
We then conducted hierarchical multiple regression analyses to better understand the relationship between current symptoms of mania and depression and CCL-M-R scores. We conducted three separate parallel analyses, one for each CCL-M-R factor, with group (entered as two contrasts, one representing the presence of a mood disorder [1 for mood disorder, 0 for no mood disorder] and the other representing the presence of bipolar disorder [1 for “yes,” 0 for “no”]) entered in the first block, ISS ACT and ISS depression cutoff scores entered in the second block, and the interactions between Group and ISS ACT and Group and ISS depression cutoff entered in the third block as predictors.
Confidence factor scores were predicted by group status. As in the results described earlier, Confidence scores were significantly higher in the no mood disorder group than in the other two groups. Confidence scores did not differ between the MDD and bipolar I disorder groups. There was a trend for group status predicting Thwarting scores, but this relationship did not reach significance (β = .20, p = .07). As above, Excitement-seeking was not related to group status (β = −.06, p > .05). Regarding the role of current symptoms, there was a trend for ISS depression cutoff scores to negatively correlate with Confidence factor scores (β = −.20, p = .05), but this relationship did not reach significance. ISS depression cutoff scores were not related to Thwarting (β = .12, p > .05) or Excitement-seeking (β = −.12, p > .05). There was no relationship of ISS ACT scores predicting Confidence (β = .03, p > .05) or Thwarting (β = .18, p > .05) factor scores. ISS ACT scores did, however, significantly predict Excitement-seeking (β = .32, p < .01) factor scores. That is, those experiencing current symptoms of mania endorsed higher scores on this subscale. Group X ISS ACT interactions were not significantly related to Confidence (β = .02), Thwarting (β = .08), or Excitement-seeking (β = .10), all ps > .05; Group X ISS depression cutoff score interactions were also not related to the factors (Confidence β = −.11, Thwarting β = −.06, and Excitement-seeking β = −.22; all ps > .05).
DISCUSSION
There were several aims of the current research. In the first study, we sought to conduct a confirmatory factor analysis of the CCL-M-R and to identify the relationships between identified factors and manic vulnerability (as measured by the HPS). In the second study, we sought to compare the factor-analyzed CCL-M-R subscales of persons diagnosed with bipolar I disorder with those of persons diagnosed with MDD and those with no history of mood disorder. We also assessed the relationship of the CCL-M-R scales with current symptoms of mania and depression.
In Study 1, factor-analytic procedures suggested several ways to refine the CCL-M-R. The structural model indicated that the Activity subscale of the CCL-M-R was not a psychometric ally stable factor. That is, the items of this subscale did not explain significant variance in factor scores, and item loadings were below acceptable limits. Thus, this subscale was not retained in the final model. Many of the original scale items did not cohere with subscales, and the final scales reflected a more narrow range of content. The final model included three subscales, comprised of items relevant to self (Confidence), to relationships (Thwarting), and to Excitement-seeking. Although the final model resulted in a significant chi-square value, both the RMSEA and SRMR indices of model fit were within acceptable limits.
As hypothesized, we found that mania risk, as measured by the HPS, was significantly related to the Excitement-seeking and Confidence factors. The Thwarting factor was unrelated to HPS scores. In Study 2 we compared CCL-M-R factor scores (derived in Study 1) of persons diagnosed with bipolar I disorder, those with MDD, and those without a history of mood disorder. We also examined the correlations of current symptoms with factor scores. Those with bipolar I disorder and those with MDD endorsed higher scores on the Thwarting factor than those without a history of mood disorder, and also endorsed lower levels of Confidence. Current symptoms of mania correlated significantly with Excitement-seeking scores, but not with the Thwarting or Confidence scores. There was no evidence that current symptoms were more influential for CCL-M-R factor scores in those with bipolar I disorder or MDD as compared to healthy controls, but the absence of symptom variability within the latter group limited the ability to test these interactions.
Taken together, current findings suggest that it is highly important to consider the stage of disorder, both in terms of whether a person is merely at risk for the disorder or struggling with a clinical level of symptoms and in terms of mood state. This is perhaps most salient with items regarding Confidence. Confidence scores were elevated among those at risk for the disorder, but were diminished in the clinical sample (particularly for those experiencing current symptoms of depression). Indeed, people with a history of either mania or major depressive episodes reported low levels of confidence. This may reflect the extreme costs of mood disorders, and suggests the need to study how self-relevant cognitions change with the course of disorder. Surprisingly, Confidence ratings were not tethered to positive mood state among the clinically diagnosed participants, in contrast to previous findings that suggest that confidence may fluctuate with positive moods in a sample of persons diagnosed with bipolar disorder (Mansell & Lam, 2006). Previous studies, though, have examined increases in confidence directly after a success or positive mood induction; volatility in confidence, then, may be more specific to success experiences.
Intriguingly, the clinically diagnosed persons with bipolar I disorder endorsed elevations in the Thwarting scale compared to those without a history of mood disorder, but risk for mania was uncorrelated with Thwarting. Although it is easy to imagine a scenario in which friends and family members try to help a person scale back his or her goals and plans as manic symptoms reach a diagnosable level, findings are somewhat puzzling in that the MDD sample also endorsed feeling thwarted. It may be that mania leads close others to try to rein in excessive goal-driven behavior, but that depressive interactions are also perceived as unsupportive, albeit for different reasons, including negatively biased cognitions. Although both types of syndromes may be associated with relationship costs, the current scale may not elucidate the differential costs.
Finally, results suggest that Excitement-seeking was present among those at risk for the disorder but in the clinical sample it was largely a state-dependent component of mania. This finding is consistent with previous research suggesting that facets of impulsivity (Meyer, Johnson, & Winters, 2001; Swann, Pazzaglia, Nicholls, Dougherty, & Moeller, 2003) increase as manic symptoms intensify among people with bipolar disorder (Meyer et al., 2001).
A limitation of the current studies involves the cross-sectional methodology, which precludes statements of cause and effect. Nonetheless, findings provide further information as to which cognitions are characteristic of those with bipolar I disorder versus which are more state dependent. That is, excitement-seeking appears to be state dependent, whereas diminished confidence and increased sense of being thwarted appear more related to diagnosis. Unfortunately, as diminished confidence and increased perception of thwarting were also related to diagnoses of MDD, the CCL-M-R is likely to be of limited use in differentiating those with bipolar disorder from those with other mood disorder diagnoses. Nonetheless, the scales may capture important aspects of the experience of persons experiencing mood disorders.
Acknowledgments
The authors would like to thank Dr. Aaron T, Beck for his generous work in developing the CCL and guiding this manuscript. They would also like to thank Dr. Camilo Ruggero for his role in assisting in data collection for Study 2, and Dr. Maria M. Llabre for her statistical consultation in preparing this manuscript.
Contributor Information
Daniel Fulford, University of Miami.
Naomi Tuchman, University of Miami.
Sheri L. Johnson, University of California, Berkeley
REFERENCES
- Alloy LB, Reilly-Harrington NA, Fresco DM, Whitehouse WG, Zechmeister JS. Cognitive styles and life events in subsyndromal unipolar and bipolar disorders: Stability and prospective prediction of depressive and hypomanic swings. Journal of Cognitive Psychotherapy: An International Quarterly. 1999;13:21–40. [Google Scholar]
- Ashworth CM, Blackburn IM, McPherson EM. The performance of depressed and manic patients on some repertory grid measures: A longitudinal study. British Journal of Medical Psychology. 1985;58:337–342. doi: 10.1111/j.2044-8341.1985.tb02650.x. [DOI] [PubMed] [Google Scholar]
- Ball J, Mitchell P, Malhi G, Skillecorn A, Smith M. Schema-focused cognitive therapy for bipolar disorder: Reducing vulnerability to relapse through attitudinal change. Australian and New Zealand Journal of Psychiatry. 2003;37:41–48. doi: 10.1046/j.1440-1614.2003.01098.x. [DOI] [PubMed] [Google Scholar]
- Basco MR, Rush AJ. Cognitive-behavioral therapy for bipolar disorder. New York: Guilford Press; 1996. [Google Scholar]
- Bauer MS, Crits-Christoph P, Ball WA, Dewees E, McAllister EA, Cacciola J, et al. Independent assessment of manic and depressive symptoms by self-rating: Scale characteristics and implications for the study of mania. Archives of General Psychiatry. 1991;48:807–812. doi: 10.1001/archpsyc.1991.01810330031005. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Vojta C, Kinosian B, Altshuler L, Glick H. The Internal State Scale: Replication of its discriminating abilities in a multisite, public sector sample. Bipolar Disorders. 2000;2:340–346. doi: 10.1034/j.1399-5618.2000.020409.x. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. Oxford: International Universities Press; 1976. [Google Scholar]
- Beck AT, Colis MJ, Steer RA, Madrak L, Goldberg JF. Cognition Checklist for Mania—Revised. Psychiatry Research. 2006;145:233–240. doi: 10.1016/j.psychres.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weishaar ME. Cognitive therapy. In: Corsini RJ, Wedding D, editors. Current psychotherapies. 5th Ed. Itasca, IL: Peacock; 1995. pp. 229–261. [Google Scholar]
- Bentall RP, Thompson M. Emotional Stroop performance and die manic defence. British Journal of Clinical Psychology. 1990;29:235–237. doi: 10.1111/j.2044-8260.1990.tb00877.x. [DOI] [PubMed] [Google Scholar]
- Cooke R, Kruger S, Shugar G. Comparative evaluation of two self report mania rating scales. Biological Psychiatry. 1996;40:279–283. doi: 10.1016/0006-3223(95)00392-4. [DOI] [PubMed] [Google Scholar]
- Eckblad M, Chapman LJ. Development and validation of a scale for hypomanic personality. Journal of Abnormal Psychology. 1986;95:214–222. doi: 10.1037//0021-843x.95.3.214. [DOI] [PubMed] [Google Scholar]
- Eich E, Macaulay D, Lam RW. Mania, depression, and mood dependent memory. Cognition and Emotion. 1997;11:607–618. [Google Scholar]
- Eisner L, Johnson SL, Carver CS. Cognitive responses to failure and success relate uniquely to bipolar depression versus mania. Journal of Abnormal Psychology. 2008;117:154–163. doi: 10.1037/0021-843X.117.1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman GC, Joormann J, Johnson SL. Responses to positive affect: A self-report measure of rumination and dampening. Cognitive Therapy and Research. 2008;32:507–525. doi: 10.1007/s10608-006-9083-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spirzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient edition (SCID-I-I/P Version 2.0) 722 West 168th Street, New York, NY 10032: Biometrics Research Department, New York State Psychiatric Institute; 1996. (Available from the. [Google Scholar]
- Hollon SD, Kendall PC, Lumry A. Specificity of depressotypic cognitions in clinical depression. Journal of Abnormal Psychology. 1986;95:52–59. doi: 10.1037//0021-843x.95.1.52. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Carver CS. Extreme goal setting and vulnerability to mania among undiagnosed young adults. Cognitive Therapy and Research. 2006;30:377–395. doi: 10.1007/s10608-006-9044-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Eisner L, Carver CS. Ambitious goal-setting and diagnoses of mania. British Journal of Clinical Psychology. (in press). [Google Scholar]
- Johnson SL, Jones S. Separable facets of manic cognition. Journal of Clinical Psychology. (in press). [Google Scholar]
- Johnson SL, Ruggero CJ, Carver C. Cognitive, behavioral and affective responses to reward: Links with hypomanic symptoms. Journal of Social and Clinical Psychology. 2003;24:894–906. [Google Scholar]
- Jones S, Mansell W, Waller L. Appraisal of hypomania-relevant experiences: Development of a questionnaire to assess positive self-dispositional appraisals in bipolar and behavioural high risk samples. Journal of Affective Disorders. 2006;93:19–28. doi: 10.1016/j.jad.2006.01.017. [DOI] [PubMed] [Google Scholar]
- Kwapil TR, Miller MB, Zinser MC, Chapman LJ, Chapman J, Eckblad M. A longitudinal study of high scorers on the hypomanic personality scale. Journal of Abnormal Psychology. 2000;109:222–226. [PubMed] [Google Scholar]
- Lam D. Bipolar disorder: A cognitive therapy approach. Behaviour Research and Therapy. 2003;41:629. [Google Scholar]
- Lam D, Wright K, Sham P. Sense of hyper-positive self and response to cognitive therapy in bipolar disorder. Psychological Medicine. 2005;35:69–77. doi: 10.1017/s0033291704002910. [DOI] [PubMed] [Google Scholar]
- Leahy RL. Decision making and mania. Journal of Cognitive Psychotherapy. 1999;13:83–105. [Google Scholar]
- Leahy RL. Cognitive Therapy. In: Johnson SL, Leahy RL, editors. Psychological treatments of bipolar disorder. New York: Guilford Press; 2003. pp. 139–161. [Google Scholar]
- Lembke A, Ketter TA. Impaired recognition of facial emotion in mania. American Journal of Psychiatry. 2002;159:302–304. doi: 10.1176/appi.ajp.159.2.302. [DOI] [PubMed] [Google Scholar]
- Lyon HM, Startup M, Bentall RP. Social cognition and the manic defense: Attributions, selective attention, and self:schema in bipolar affective disorder. Journal of Abnormal Psychology. 1999;108:273–282. doi: 10.1037//0021-843x.108.2.273. [DOI] [PubMed] [Google Scholar]
- Mansell W, Jones SH. The Brief-HAPPI: A questionnaire to assess cognitions that distinguish between individuals with a diagnosis of bipolar disorder and non-clinical controls. Journal of Affective Disorder. 2006;93(1–3):29–34. doi: 10.1016/j.jad.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Mansell W, Lam D. “I won’t do what you tell me!”: Elevated mood and the assessment of advice-taking in euthymic bipolar I disorder. Behaviour Research and Therapy. 2006;44(12):1787–1801. doi: 10.1016/j.brat.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Mansell W, Pedley R. The ascent into mania: A review of psychological processes associated with the development of manic symptoms. Clinical Psychology Review. 2008;28(3):494–520. doi: 10.1016/j.cpr.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Mansell W, Rigby Z, Tai S, Lowe C. Do current beliefs predict hypomanic symptoms beyond personality style? Factor analysis of the hypomanic attitudes and positive predictions inventory (HAPPI) and its association with hypomanic symptoms in a student population. Journal of Clinical Psychology. 2008;64(4):450–465. doi: 10.1002/jclp.20455. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Hau K-T. Confirmatory factor analysis: Strategies for small sample sizes. In: Hoyle RH, editor. Statistical strategies for small sample research. Thousand Oaks, CA: Sage; 1999. pp. 252–284. [Google Scholar]
- Meyer B, Johnson SL, Winters R. Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS scales with symptoms. Journal of Psycho-pathology and Behavioral Assessment. 2001;23(3):133–143. doi: 10.1023/A:1010929402770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy FC, Sahakian BJ, Rubinsztein JS, Rodgers RD, Robbins AM, Paykel ES. Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine. 1999;29:1307–1321. doi: 10.1017/s0033291799001233. [DOI] [PubMed] [Google Scholar]
- Newman C, Leahy RL, Beck AT, Reilly-Harrington N, Cyulai L. Bipolar disorder: A cognitive therapy approach. Washington, DC: American Psychological Assocation; 2002. [Google Scholar]
- Reilly-Harrington NA, Alloy LB, Fresco DM, Whitehouse WG. Cognitive styles and life events interact to predict bipolar and unipolar symptomatology. Journal of Abnormal Psychology. 1999;108:567–578. doi: 10.1037//0021-843x.108.4.567. [DOI] [PubMed] [Google Scholar]
- Scott J. The role of cognitive behaviour therapy in bipolar disorders. Behavioural and Cognitive Psychotherapy. 1996;24:195–208. [Google Scholar]
- Scott J. Treatment outcome studies. In: Johnson SL, Leahy RL, editors. Psychological treatments of bipolar disorder. New York: Guilford Press; 2003. pp. 226–241. [Google Scholar]
- Scott J, Pope M. Cognitive styles in individuals with bipolar disorder. Psychological Medicine. 2003;33:1081–1088. doi: 10.1017/s0033291703007876. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Castellon C, Cacciola J, Schulman P, Luborsky L, Ollove M, Downing R. Explanatory style change during cognitive therapy for unipolar depression. Journal of Abnormal Psychology. 1988;97:13–18. doi: 10.1037//0021-843x.97.1.13. [DOI] [PubMed] [Google Scholar]
- Stern GS, Berrenberg JL. Skill-set, success outcome, and mania as determinants of the illusion of control. Journal of Research in Personality. 1979;13:206–220. [Google Scholar]
- Swann AC, Pazzaglia P, Nicholls A, Dougherty DM, Moeller FG. Impulsivity and phase of illness in bipolar disorder. Journal of Affective Disorders. 2003;73(1–2):105–111. doi: 10.1016/s0165-0327(02)00328-2. [DOI] [PubMed] [Google Scholar]
- Weingartner H, Miller H, Murphy DL. Mood-state-dependent retrieval of verbal associations. Journal of Abnormal Psychology. 1977;86:276–284. doi: 10.1037//0021-843x.86.3.276. [DOI] [PubMed] [Google Scholar]
- Williams JBW, Gibbon M, First MB, Spirzer RL, Davies M, Borus J, et al. The Structured Clinical Interview for DSM-III-R (SCID): II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]