Summary
Endovascular treatment of intracranial aneurysms by coiling has become an accepted alternative to surgical clipping1. In cases of wide-necked and sidewall aneurysms, selective embolization is difficult because of the risk of coil protrusion into the parent vessel. The use of three-dimensional coils, stents2, and balloon remodeling have all aided the attempt to adequately manage such lesions. However, compared with sidewall aneurysms, bifurcation aneurysms are more challenging from an endovascular standpoint. Because of their specific anatomy and hemodynamics, the tendency to recur and rerupture is higher. Several authors have reported successful treatment of these complex and wide-necked bifurcation aneurysms by using Y-configured dual stent-assisted coil embolization3,4, the double microcatheter technique5, a more compliant balloon remodeling technique6, the TriSpan neck-bridge device7, or the waffle cone technique8. We describe two cases of wide-necked bifurcation aneurysms in which the waffle cone technique was used for coil embolization. The waffle cone technique was first described in 2006; however, the small number of published cases and the lack of follow-up prevent one from assessing this technique's durability and the probability of recanalization. We report the cases of two patients harboring unruptured wide-necked bifurcation aneurysms that were treated and followed-up for six months.
Key words: aneurysm, bifurcation, embolization, stent
Cases Reports
Patient 1
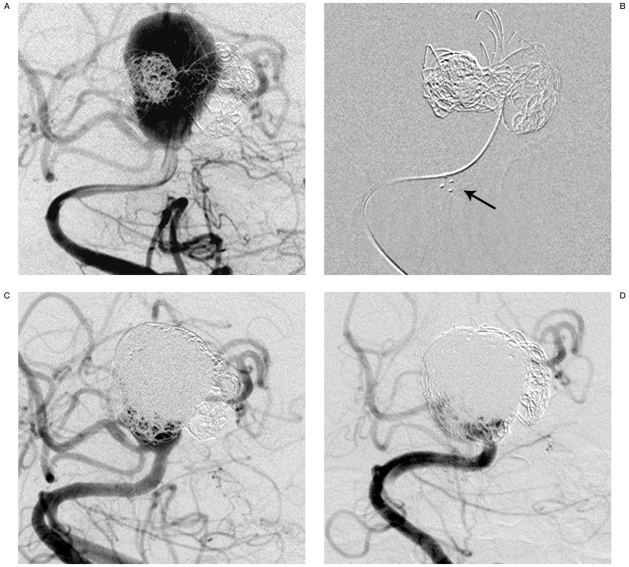
A 65-year-old man presented with progressive left side ptosis, poor vision, and diplopia. Angiography showed a large, basilar bifurcation aneurysm with dolichoectasia of the basilar artery. Endovascular coiling of the aneurysm was performed successfully, and the symptoms subsided. Unfortunately, the symptoms recurred six months later, and angiography showed a recurrent wide-necked basilar bifurcation aneurysm that incorporated both the posterior cerebral arteries and the origins of the right superior cerebellar artery in the aneurysmal neck (Figure 1A).
Figure 1.
A) Anteroposterior view of the right vertebral artery injection demonstrates a recurrent basilar bifurcation aneurysm incorporating both posterior cerebral arteries and the right superior cerebellar artery. B) Anteroposterior angiographic view shows the aneurysm with platinum Neuroform stent marks in the basilar trunk (arrow). Distal marks in the fundus of the aneurysm are obliterated by the coil mass. C) Anteroposterior angiogram shows near-complete coiling of the aneurysm. D) Six-month follow-up anteroposterior angiography shows persistent occlusion of the aneurysm.
The treatment proposed for the patient was to place a 4.5x20 mm Neuroform stent (Boston Scientific/Target, Fremont, CA) directed into the aneurysm with the proximal end anchored in the trunk of the basilar artery before coil embolization of the aneurysm. Our thought was that such positioning would allow the distal end of the stent to open in the fundus of the aneurysm such that the stent's tip would resist coil extravasation into the parent vessel. The patient was administered aspirin (325 mg/d) and clopidogrel (75 mg/d) for three days before the procedure. The procedure was performed under general anesthesia, and a 6-French guiding catheter was placed into the right vertebral artery. Three thousand units of heparin were infused, and the Neuroform stent was advanced over a Transcent 0.014-inch wire (Boston Scientific/Target). The stent was deployed with the distal end of the device in the fundus of the aneurysm (Figure 1B). An Excelsior 1018 microcatheter (Boston Scientific/Target) was then advanced over a Transcent 0.014-inch wire into the aneurysm, with subsequent coiling with Guglielmi detachable coils (Boston Scientific) in combination with Matrix coils (Boston Scientific/Target). The aneurysm appeared nearly completely treated, except for a small remnant neck (Figure 1C). The patient suffered no post-treatment complications or persistent neurological deficit related to this procedure. The 6-month follow-up angiogram (Figure 1D) showed the persistence of the occlusion of the aneurysm.
Patient 2
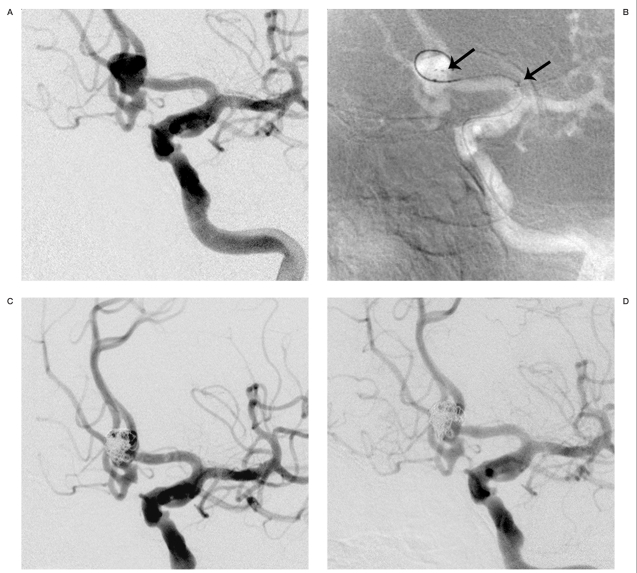
A 53-year-old man presented with intermittent left-side vision loss. Angiography showed a wide-necked anterior communicating artery (AComA) aneurysm with incorporation of the A2 segment of the bilateral anterior cerebral artery (Figure 2A). Hypoplasia of the A1 segment of the right anterior cerebral artery was observed, with the bilateral anterior cerebral territory perfused from the left internal carotid artery via AComA. The procedure was performed under general anesthesia and the usual anticoagulation regimen. A 6-French guiding catheter was placed into the left internal carotid artery. Using a technique similar to that for patient 1, a 4.5x15 mm Neuroform stent was placed partially within the fundus of the aneurysm and anchored in the left A1 segment (Figure 2B). The aneurysm was then coiled with Guglielmi detachable coils. Complete obliteration of the aneurysm cavity was obtained without any compromise of distal flow. The final stent and coiling configuration is illustrated in figure 2C. The 6-month follow-up angiogram (Figure 2D) showed the persistence of the occlusion of the aneurysm.
Figure 2.
A) Anteroposterior view of the left internal carotid artery injection demonstrates a 7-mm wide-necked anterior communicating artery aneurysm incorporating A2 segments of the bilateral anterior cerebral arteries. B) Anteroposterior angiographic view shows the aneurysm with platinum Neuroform stent marks in the fundus and in the A1 segment of the left anterior cerebral artery (arrows). C) Anteroposterior angiogram shows the completely coiled aneurysm. D) Six-month follow-up anteroposterior angiography shows persistent occlusion of the aneurysm.
Discussion
Coil embolization of wide-necked aneurysms remains technically difficult, even with balloon remodeling techniques. Potential herniation of the coil into the parent vessels engenders suboptimal coil packing and may increase the likelihood of compaction of the coil and recanalization of the aneurysm. In treating wide-necked and fusiform aneurysms, the Neuroform stent promises to be an invaluable asset 9,10. The high degree of flexibility renders it a highly navigable tool for the treatment of aneurysms, even those in distal areas such as the case reported above (patient 2). Although the Neuroform stent was designed to cover the aneurysm neck in either a straight or a Y-shaped fashion 3,4 (using two stents), the device also has applicability in bifurcation aneurysms when inserted partially within the fundus of the aneurysm and the lumen of the parent vessel. Horowitz et Al.8 first described the waffle cone technique treating eight wide-necked bifurcation aneurysms in eight patients. In those patients, more than 95% complete occlusion was achieved in six aneurysms, and partial occlusion was achieved in two. These patients suffered no post-treatment complications related to this procedure.
There are several theoretical advantages to this technique. In aneurysms with very large necks, the neck can be effectively reconstructed by the Neuroform stent. In large aneurysms on vessels with sharp curves, the stent can easily be placed into the fundus of the aneurysm and deployed, avoiding the risks of trying to maneuver wires and stents beyond the aneurysm neck. Compared to the Y-shape configuration, the waffle cone technique reduces the amount of metal deposited in the vessels, thus possibly reducing the generation of thrombi. However, the small number of published cases in which the waffle cone technique has been used and the lack of follow-up prevent one from assessing this technique's durability and the probability of recanalization. It is possible for the stent to cause rupture of the aneurysm if it jumps during navigation and deployment. We use the waffle cone technique for those situations in which the use of a traditional stent bridging from the proximal afferent feeding artery across the aneurysm neck to the distal efferent artery is impossible. A 6-month follow-up angiogram in our patients revealed continued obliteration of the aneurysm with patency of the parent vessels.
Our initial results with this technique suggest that it could be an effective alternative in certain cases, but only experience with significant follow-up can determine whether this approach has benefit in the long term.
Conclusions
The "waffle cone" technique allows us to treat the complex and wide-necked bifurcation aneurysms that have an anatomic configuration considered unfavorable for coil placement with the standard technique.
References
- 1.International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 2.Leonardi M, Dall’olio M, et al. Intracranial stenting in the treatment of wide-necked aneurysms. Interventional Neuroradiology. 2007;13:19–30. doi: 10.1177/159101990701300103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thorell WE, Chow MM, et al. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery. 2005;56:1035–1040. [PubMed] [Google Scholar]
- 4.Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms: report of three cases. Neurol Res. 2004;26:276–281. doi: 10.1179/016164104225013969. [DOI] [PubMed] [Google Scholar]
- 5.Baxter BW, Rosso D, et al. Double microcatheter technique for detachable coil treatment of large, widenecked intracranial aneurysms. Am J Neuroradiol. 1998;19:1176–1178. [PMC free article] [PubMed] [Google Scholar]
- 6.Baldi S, Mounayer C, et al. Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. Am J Neuroradiol. 2003;24:1222–1225. [PMC free article] [PubMed] [Google Scholar]
- 7.De Keukeleire K, Vanlangenhove P, et al. Evaluation of a neck-bridge device to assist endovascular treatment of wide-neck aneurysms of the anterior circulation. Am J Neuroradiol. 2008;29:73–78. doi: 10.3174/ajnr.A0767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horowitz M, Levy E, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms: eight cases using the waffle cone technique. Neurosurgery. 2006;58:258–62. doi: 10.1227/01.NEU.0000204713.24945.D2. [DOI] [PubMed] [Google Scholar]
- 9.Fiorella D, Albuquerque FC, et al. Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery. 2004;54:6–16. doi: 10.1227/01.neu.0000097194.35781.ea. [DOI] [PubMed] [Google Scholar]
- 10.Wanke I, Doerfler A, et al. Treatment of wide-necked intracranial aneurysms with a self-expanding stent system: initial clinical experience. Am J Neuroradiol. 2003;24:1192–1199. [PMC free article] [PubMed] [Google Scholar]