Abstract
This commentary discusses advances in the conceptual understanding of racism and selected research findings in the social neurosciences. The traditional stress and coping model holds that racism constitutes a source of aversive experiences that, when perceived by the individual, eventually lead to poor health outcomes. Current evidence points to additional psychophysiological pathways linking facets of racist environments with physiological reactions that contribute to disease. The alternative pathways emphasize prenatal experiences, subcortical emotional neural circuits, conscious and preconscious emotion regulation, perseverative cognitions, and negative affective states stemming from racist cognitive schemata. Recognition of these pathways challenges change agents to use an array of cognitive and self-controlling interventions in mitigating racism’s impact. Additionally, it charges policy makers to develop strategies that eliminate deep-seated structural aspects of racism in society.
Keywords: Racism, Health Disparities, Behavioral Interventions, Psychosocial Stress
INTRODUCTION
Racism is part of the fabric of life for African Americans and is among the causes of enduring negative health outcomes. There is really nothing new or startling in the assertion that social circumstances encountered as part of day-to-day experience influence physical health. At the turn of the last century, W. E. B. Du Bois (1906) and Kelly Miller (1897) proposed in separate manuscripts that oppressive social conditions encroaching on the lives of African Americans contributed to poor health and premature death. Fifty years later, Frantz Fanon’s classic studies (1967, 1968) examined the effects of oppression and included a recognition of “psychosomatic”—that is physical—consequences. Currently, social epidemiologists, health psychologists, and medical sociologists have extended the insights of these important early scholars by showing how racism generates systems and practices that contribute to persistent disparities in health outcomes (Paradies 2006a; Pascoe and Richman, 2009; Williams 1997). Estimates indicate that the failure to erase these disparities costs tens of thousands of African American lives each year (Levine et al., 2001; Williams and Mohammed, 2009). As long as the rates of the leading causes of death differ along racial lines (Centers For Disease Control and Prevention, 2008), the specter of racism will haunt the United States. The persistence of racial health disparities and of racism in any form calls scholars, therapists, activists, and political leaders to vigorous action.
Racism may impact health directly and indirectly. It can contribute to negative health outcomes indirectly by shaping the health-related behavior of oppressed groups. An important and growing body of research reveals that frustration and social upheaval stemming from racism lead to high rates of smoking, drug use, and overeating, and that these behaviors may mediate the relationship between discrimination and racial health disparities (Jackson and Knight, 2006). This paper focuses on a more direct path, specifically psychophysiological processes that connect racism and disease. First we discuss expanded definitions of racism that have emerged in recent decades. Then these conceptualizations are considered in light of research in social neuroscience, a relatively new discipline which identifies the biological concomitants of complex human actions (Cacioppo et al., 2002). Based on these findings, we chart several chains of psychophysiological events that link racism to health. Finally, we conclude by identifying briefly interventions that may reduce racism’s impact on health.
CONCEPTUALIZING RACISM
Nearly forty years ago, James Jones (1972) in Prejudice and Racism challenged definitions of racism that minimized the important issue of power differentials by focusing primarily on attitudes, distorted ideologies, and unfair treatment. Jones argued that racism involves assertions of power that are expressed on individual, institutional, or cultural levels. Recent conceptual advances have underscored the significant limitations of cognitive and behavioral views of racism and have included critical discussions of its systemic foundations. Two particularly comprehensive conceptualizations of racism were developed by Paradies (2006b) and Harrell (2000). They described racism as a system where power is unevenly distributed along racial lines resulting in the oppression and exclusion of non-White groups. These conceptual advances are critical to a comprehensive understanding of the breadth and persistence of racism (Baker 2008; Bell 2004) and to the success of ameliorative policies and therapeutic interventions.
Just as multidimensional and complex forms of racism can be incorporated into the individual’s cognitive structures, they are woven into the fabric of the society. Indeed, racism emanates from individual, cultural, institutional, and structural domains and has psychological and physiological effects. Thus, according to Paradies (2006b), racism transcends the incorrect or irrational behavior of individuals because “non-human actors such as laws and institutions can perpetuate systemic racism” (p. 146). Through values and practices, social institutions support the efforts of dominant groups to maintain power and privilege (Bonilla-Silva 1997, 2001, 2006). Bonilla-Silva’s (1997) structural approach to racism provided a critical challenge to the assumption that racism is a “free-floating” ideology. He proposed that racism is a central organizing principle that governs the arrangement of the society. Structural racism encompasses social mechanisms that have made the privileges associated with being White and the disadvantages associated with being a person of color relatively permanent characteristics of Western societies. It fostered the “color-blind” policy racism that permeated public policy in the last two decades of the twentieth century (Walters 2003) and constitutes the foundation upon which all other forms of racism are built. Essentially, structural racism energizes and drives the ways in which racism is sustained via interpersonal, cultural, and institutional actions (Bonilla-Silva 2006).
MEDIATORS OF PHYSIOLOGICAL ACTIVATION AND ALTERATIONS
Racism as Stressful
In considering racism’s impact on health, the most straightforward case is that racism makes the lives of the disadvantaged more stressful and thus leads to negative mental and physical health consequences (Clark et al., 1999; Harrell et al., 1998; Krieger 1994). Clark et al. (1999) propose that perceiving an experience as racist initiates a series of processes that results in negative emotional reactions and physiological changes. Physiological arousal includes activation of the hypothalamic pituitary adrenal cortical (HPA) system, which involves the release of the stress hormone cortisol, and also entails changes in immune and cardiovascular functioning. Cardiovascular changes and a myriad of responses including respiratory functions and pupil size come under increased control of the sympathetic branch of the autonomic nervous system during emergencies. These physiological adjustments constitute the sympathetic adrenal medullary axis (SAM) of the stress response. Investigators have marshaled laboratory and survey evidence (Brondolo et al., 2003; Harrell et al., 2003) linking experiences with individual and institutional racism to physiological changes.
One irony that early psychophysiological studies revealed is that striving to actively control stressors actually increases activation within the cardiac sympathetic nervous system and disrupts autonomic balance (Obrist 1981). Thus, the findings cautioned that those who recognize racism and attempt to control it may be particularly vulnerable to its negative physiological effects. Similarly, increased physiological activation is a possible mediator of poorer performance on tasks that occurs when individuals believe their efforts could potentially confirm racist stereotypes (Blascovich et al., 2001; Schmader et al., 2008). Though striving to come to grips with racism or to disconfirm its mythology may result in increased physiological activation, passivity and acquiescence are not healthy alternatives. Rather, those who actively confront racism should be armed always with behavioral strategies, discussed below, that will allow them to control levels of physiological arousal.
Though currently much of the research on racism and health is grounded in the stress model, it applies most appropriately where institutional and individual racism generate discrete and perceivable toxic situations and social encounters. However, racism encompasses more than encounters with strident, unenlightened people and oppressive, constraining institutions. Conceptualizing racism within the stress and coping paradigm leads to the conclusion that if one does not perceive circumstances as racist or appraise events as stressful, the physiological reactions to them will not occur. There is evidence that the conscious perception of threatening events is but one of several pathways leading to the disruption of physiological regulation. Limitations of the traditional stress model encourage the search for other mechanisms that mediate racism’s impact.
Prenatal Effects of Racism
In a provocative article, Kuzawa and Sweet (2009) show how racism potentially affects the uterine environment and epigenetic activity, and thus contributes to negative health. The study of epigenetic processes considers an array of factors that influence how genes are expressed (Jaenisch and Bird, 2003). A growing consensus holds that environmental and genetic events constantly interact and are best conceptualized as interdependent (Harrell et al., 2010; Moore 2001). Thus, the mapping of the human genome was simply one step toward understanding the complex interplay between biological and environmental events that govern the unfolding genetic potential. In addition, mounting evidence from animal and human research suggests that during the prenatal period there are epochs where health outcomes are singularly vulnerable to nutritional and psychosocial factors (Barker 1998, 2002). Remarkably, the model Kuzawa and Sweet (2009) developed proposed the prenatal effects of racism are potentially transgenerational. The effects of stressful environments on the fetus can potentially cause lingering metabolic alterations during adulthood, which in females will impact the uterine environment of offspring.
Racism troubles the entire fabric of life in oppressed communities creating encounters with environmental toxins (Greene and Morris, 2006) and poor nutrition, as well as noxious and damaging social and psychological exchanges and circumstances. The uterine environment is adapted to maintain conditions that lead to optimal fetal growth and development. However, chronic psychosocial stressors experienced by the mother during various periods of gestation can threaten the well-being of the fetus. In many respects then, racism is encountered long before the brain of its victim is developed enough to appraise any particular manifestation of it. Low birth weight would be among the more ostensible effects of these insults (Giscombe and Lobel, 2005; Collins et al., 2000, 2004; Hobel and Culhane, 2003; Lauderdale 2006; Mustillo et al., 2004), but the harmful impact may be subtle and less apparent at birth. Programmed effects of racism on health, which may include altered neural development, may not become evident until much later in life.
Racism’s Unconscious Pathway
Two sets of studies highlight another route through which racism influences physiological activity and health outcomes. Experiments using animals have revealed that stress responses can activate a pair of distinct neural circuits in the brain (LeDoux 1996, 2002). Normally, information from the environment moves from the senses to a structure at the base of the brain called the thalamus and from there to the cerebral cortex. In the cortex the sensory input is integrated with previous input, appraised, and evaluated. Ultimately, as the stress and coping model details, the cerebral cortex is where information is represented as the conscious emotional and cognitive events that are experienced when the organism is threatened or placed in danger.
LeDoux (1996) has shown that information about stress in the environment can take an alternate neural path. The thalamus not only receives and transmits sensory input to the cortex, it also connects with a second set of neural circuits that reside within the amygdala, a neighboring structure at the base of the brain. The amygdala initiates a cascade of neural events that activate lower brain centers and cause stress responses in the HPA and SAM systems. For example, the central nucleus of the amygdala (CeA) activates pathways to the lateral hypothalamus and brainstem to stimulate HPA and SAM responses. Connections between the hippocampus and lateral amygdala mediate contextual information that modulates fear responses. Thus, subcortical structures provide a rapid route to physiological activation, but this activation is not dependent on conscious perception of the stimulus. Conscious perception occurs through the separate stream of neural events involving higher cortical activity, but the unconscious subcortical pathways of stress are worthy of further study.
A second line of research, human classical conditioning studies, provides additional evidence that physiological systems can be activated unconsciously. Experimental studies have demonstrated that conditioned autonomic responses take place even when the conditioned stimuli are made unrecognizable by masking techniques (Soares and Ohman, 1993). Additionally, clinical neuropsychological research has shown that conditioned activation occurs in patients whose severe brain damage renders them incapable of generating new episodic memories (Daum et al., 1991). These patients are not able to remember when an unpleasant event—for example, a shock or loud noise—was associated with a particular color. Still, if given a choice, they will subsequently avoid that particular color. Clearly, humans do not have to recognize a conditioned stimulus or consciously process its link to a negative event for the stimulus to elicit physiological arousal.
Thus, conscious awareness of elements of racism is not a necessary condition for physiological activation to take place. The brain initiates early rapid physiological arousal unconsciously that prepares the individual for action, sometimes before the stressor is fully perceived. Accordingly, it is likely that repeated encounters with individual or institutional racism and its context can elicit physiological reactions of which the individual is unaware. The setting or social environs where reactions have occurred may also result in physiological activation. For example, negative interpersonal encounters need not happen on the job or in schools on a daily basis. The work site or the classroom alone might be quite capable of eliciting physiological arousal, unconsciously, because of their connection to aversive events.
Emotion Regulation and Racism
Another avenue by which racism may trigger strong physiological reactions is activated when individuals attempt to manage the anticipatory responses and subsequent reactions to socially racist stressors. This process is called emotion regulation. Emotion regulation refers to the ability to increase, maintain, or inhibit the expression and experience of an emotional response. The alteration in emotional responding occurs in milliseconds and can be voluntary or automatic (Golden et al., 2008; Gross and John, 2003; Ochsner and Gross, 2005). Suppression, the inhibition of one’s emotional response, takes place when the emotion is denied admission into consciousness. Successful suppression of an emotion reduces the reported or observed experience of subjective experience, though the physiological arousal may persist (Jackson et al., 2000). It was noted earlier that active coping can enhance responses to stress. Ironically, several studies report that those who deny or suppress the existence of racism experience higher systolic blood pressure than individuals who confront and actively cope with racially noxious situations (Krieger 1990; Krieger and Sidney, 1996).
There is strong evidence that individual differences in prefrontal activation play an essential role in emotion regulation. In particular, individuals who report persistent negative affect and who show increased physiological reactivity to stressful events are more likely to have a difficult time regulating the intensity and duration of a negative emotion once it has been activated (Davidson 2000; Davidson et al., 2000). Indeed, the emotional response to social rejection or social pain can be very intense, especially in the case of individual or institutional racism. Social pain may activate brain regions that are responsive to physical pain. Eisenberger et al. (2003) provide evidence that the prefrontal cortex, in particular the anterior cingulate cortex and right ventral prefrontal cortex, are active when social pain is experienced. These noxious events are likely to engage and often tax emotion regulatory and restorative processes. Important progress in the study of the effects of racism on health will result from studies of brain mechanisms involved in regulating reactions to intensely distressing social experiences.
Racism, Worry, and Autonomic Balance
Some social neuroscientists who study human adaptation to complex and demanding environments have made the activity of the vagus nerve their central focus (Porges 1995, 2001; Thayer and Friedman, 2004). The vagus nerve is part of the parasympathetic branch of the autonomic nervous system and in many instances reduces activation while assisting in building resources in the body. For example, one division of the vagus nerve reduces the energy demands by slowing heart rate, while other branches increase digestive activities that allow us to store energy that may be needed later (Porges 2001). Neural circuitry coursing from the frontal cortical regions connects with the vagal circuits in the brain stem and facilitates flexible cardiac adaptation to a changing environment (Thayer and Friedman, 2004). While increased vagal activation slows the heart, the vagus can speed heart rate by withdrawing its effects. Thayer and Friedman (2004) note that changes in vagal activity take place on a second-by-second basis, and facilitate rapid behavioral and cognitive adjustments as environmental demands require them. Further, dysregulation of vagal functions signals the presence of chronic diseases and is potentially lethal (Thayer and Lane, 2007).
Research suggests that the frontal lobes, which contain brain centers responsible for some of the most complex human cognitive functions, also house neural pathways that mediate the calming influences of the vagus on the heart. Failures in several higher-order “executive” cognitive processes that reside in the frontal lobes interfere with vagal functioning. For example, when well-ordered and coherent cognitive processing is replaced by perseverative thinking that includes worry and rumination, vagal control of the heart is reduced and a variety of other stress responses occur (Brosschot et al., 2006). Perseverative thinking, which can be conscious as well as unconscious, extends the time course of stress reactions (Brosschot et al., 2010). Normally, the frontal lobes are the source neural input that constantly inhibits the excitatory activity in lower brain centers that are responsible for peripheral stress responses. Thayer and Friedman (2004) argued that chronic threats and aversive events stemming from racism can ultimately interrupt the calming impact of the vagus nerve on cardiac functions by inducing worry and rumination. Therefore, vagal dysregulation resulting from disturbances in executive cognitive functions is an alternate mechanism through which several forms of racism might disrupt physiological activity.
Racism and Cognitive Schema
Cognitive structures that racism generates are the source of the final alternative path along which physiological effects may be mediated. Various forms of racism can be represented in the mind (Harrell 1999; Jones 2000; Taylor et al., 1998) as unpleasant memories as well as cognitive schemata that deprecate non-Western ethos, history, and practices and, by extension, people of color themselves. These mental dispositions threaten psychological well-being and, in the case of cultural racism, block the positive emotional states that normally arise when one embraces one’s cultural heritage and lineage (Daniels et al., 2001; Dressler and Bindon, 2000; Eckersly 2005). Research suggests that interrupting processes that bring about positive emotions may be particularly threatening to physiological regulation. Fredrickson has shown that pleasant emotions undo the cardiovascular activation that accompanies negative emotional states (Fredrickson 2001, 1998).
Research using functional magnetic resonance imaging has started to identify the neural underpinnings of racist schema, though these studies are in their infancy. In both Black and White participants, perceiving Black faces, but not verbal race labels, caused greater amygdala activation than the perceiving White faces (Lieberman et al., 2005). As noted earlier, the amygdala is sensitive to the presence of a threat; African Americans showing activation in this region in the presence of Black faces reveals signs of self-deprecation. It is not unreasonable to posit that for people of color, isolation and alienation resulting from racial schemata that disparage Black people and culture lead to increased levels of negative emotions and contribute to a general sense of defeat. The presence of these unpleasant mental states is likely to be associated with elevated blood pressure in Black populations (Chae et al., 2010; Daniels et al., 2001; Dressler and Bindon, 2000) and HPA activation in general (Kemeny 2009).
Allostasis: From Physiological Changes to Disease
Ultimately, investigators who propose that the social environment influences health must explain how temporary fluctuations in physiological activity lead to more permanent alterations associated with disease. Traditionally, homeostasis has been recognized as the process by which physiological systems regulate their levels of activity around fixed optimal set points (Cannon 1929). More recently, the focus has shifted to allostasis (McEwen 1998), a concept that encompasses the capacity of the body to achieve “other” levels of activity in response to environmental changes and demands. The ability to maintain stability within systems conserves energy and thus has had an evolutionary advantage, as long as the organism did not confront extraordinary circumstances. However, through allostasis, the adaptable organism was able to make physiological adjustments when they were required. Sometimes, by the process of allodynamism (Berntson and Cacioppo, 2000) appropriate alterations were achieved through changes in the underlying mechanisms controlling physiological activity. However, the adjustments in physiological levels may shade toward pathology when they are extreme, sustained, or both. Researchers use measures of allostatic load (See-man et al., 2010) as an index of cumulative demands placed on several physiological systems that may result in enduring unhealthy physiological changes.
The concepts of allostasis and allodynamism constitute a final common pathway for models that link racism to poor health outcomes. These models discuss racism’s health effects in terms of environments that fail to nurture psychological and physical well-being (Jones 2000), weathering effects on organs and physiological systems (Geronimus 1992), and the embodiment of inequitable social systems (Krieger 1999, 2005). Racism threatens health when it produces physiological changes that through any of the paths we have enumerated are extensive, occur repeatedly, or take place during certain critical developmental periods. For example, mounting evidence suggests that the nocturnal blood-pressure levels of African Americans who report encounters with discrimination fail to dip, that is, reach a normal nadir during sleep (Barksdale et al., 2009; Beatty and Matthews, 2009; Brondolo et al., 2008; Lewis et al., 2009). This may constitute an allostatic adjustment that portends the onset of hypertension. Important research on allostasis and allodynamism is specifying the brain centers and peripheral physiological mechanisms that make permanent and pathological the fluctuations in physiological activity that are intended to help one cope with environmental demands (McEwen and Gianaros, 2010). In so doing, these studies contribute important details to maps that chart the physiological paths leading from racism to poor health.
FORMS OF RACISM AND PSYCHOPHYSIOLOGICAL CHANNELS
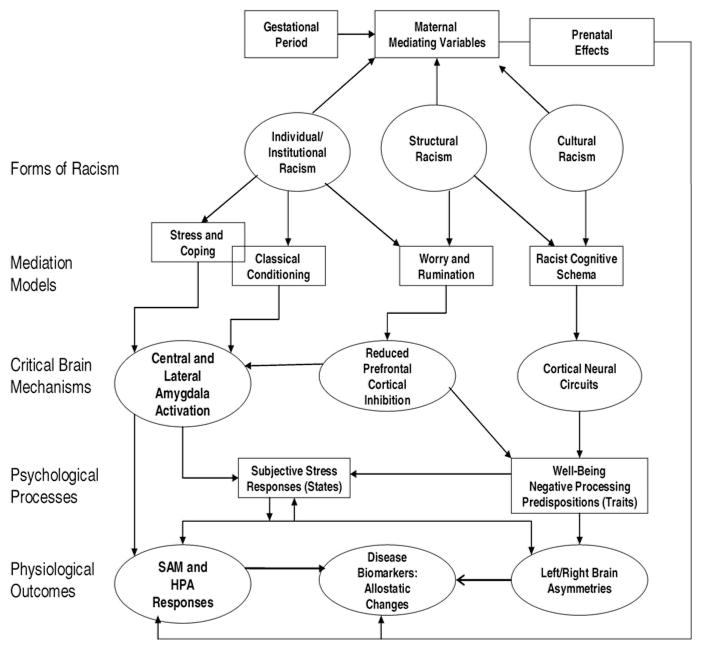
Various manifestations of racism will show distinct affinities for one or more of the pathways through which environmental circumstances influence physiological outcomes. Table 1 posits how four forms of racism are mediated psychologically and translated into physiological outcomes. Each kind of racism generates internal representations, specified in the third column, that give rise to psychological mediators of physiological changes. The psychological mediators are presented in the fourth column.
Table 1.
Mechanisms That Mediate the Psychological and Physiological Effects of Five Forms of Racism
| Forms or Facets of Racism | Examples | Internal Psychological Representation | Mediators of Physiological Impact |
|---|---|---|---|
| Structural | Chronic poverty, unemployment, and failed infrastructure in non-White communities. | Conditioned links between dire context and race; schema reflecting racialized disparities. | Reduced sense of well-being; worry and rumination; racist schema. |
| Cultural | Individual and institutional devaluation and misrepresentation of non-Western and non-White cultural products and values. | Schema and values reflecting negative evaluations of non-White cultural products and values. | Reduced valuing of one’s culture; alienation from cultural roots; negative affect. |
| Institutional | Actions of educational and employment institutions discriminate against African people. | Reactions to and episodic memory of denied access. Negative sense of self (individual and collective) in schema. | Appraisal and coping processes; reduced well-being, increased worry; suppression and unconscious reactions. |
| Individual | Discriminatory acts against people of color. | Reactions to and episodic memory of personal insult or unfair treatment. | Appraisal and coping processes; reduced well-being, increased worry; suppression and unconscious reactions. |
Table 1 argues that the indirect effects of structural racism are experienced primarily in terms of racialized outcomes. Often the disparities it produces are processed outside of awareness, and are represented cognitively in the form of classically conditioned associations between race and negative circumstances or by more complex racist cognitive structures. Structural racism contributes strongly to implicit associations between Black people and crime, poverty, and destitution. In contrast, institutional and individual forms of racism are more likely to be encoded as episodic memory, sometimes consciously. Here racism often takes the form of stressful events that elicit appraisal and coping processes. As the table states, in some instances racism operates through classically conditioned processes which drive many of the emotional components of responses.
Figure 1 conceptualizes an approach to the study of racism and health outcomes. We placed the forms from Table 1 at the first level, with the next row specifying the conceptual model that fits the mechanisms through which each type of racism operates. Brain mechanisms critical to the effects of each manifestation of racism are then described. The next level shows two resulting psychological processes that are critical to the impact of racism, transient changes in emotional and cognitive states and relatively permanent alterations in well-being and cognitive schema. The physiological outcomes on the last level represent the changes racism causes in peripheral physiological and brain activity, as well as the early markers of disease. This illustration is a map of human suffering, with many of the paths representing conduits through which racism impacts social, psychological and biological domains.
Fig. 1.
Proposed models, psychological processes, and physiological pathways that link four forms of racism to health-related physiological changes
Interventions
Evidence suggests that several interventions may reduce the physiological impact of racism. While we will describe a number of these, more extensive reviews of racism-related treatment strategies are available (Paradies et al., 2009). Therapeutic strategies are any corrective actions that interrupt one or more of the paths between the events and processes depicted in Figure 1. We will identify the pathway of focus for each of the interventions under discussion. Cutler (2004) argued that interventions focusing on improving public health emanate from the individual, community, and national levels. His tone was decidedly hopeful, as he noted that several national programs have already achieved remarkable success in changing smoking and drunk-driving behaviors. Thus, there is no reason to shrink from developing a therapeutic agenda for mitigating the effects racism has on biological systems.
Individualized approaches to intervening offer promising strategies for reducing physiological activation represented at the bottom of Figure 1. Mindfulness meditation and progressive relaxation are self-controlling techniques that influence autonomic, neuroendocrine, and immune function (Conrad and Roth, 2007; Davidson et al., 2003; Pawlow and Jones, 2002). It would be wise for clinical professionals to make training in these techniques readily available to populations vulnerable to racism’s impact. They should be provided routinely for women during pregnancy. The procedures may mitigate physiological activation traceable to acute and chronic stressors or conditioned to contextual stimuli of which the individual may or may not be aware. Stress management procedures that include cognitive behavioral therapy also influence physiological reactions (Phillips et al., 2008). These therapeutic techniques have the added advantage of restructuring nonproductive and self-deprecating racist cognitive schemata. Cognitive therapies also help individuals confront their emotional and behavioral responses to racism including tendencies to suppress, worry, or ruminate.
Community and national strategies have the potential to launch a proactive attack on cultural racism and the racist cognitive schemata it nurtures. In the United States, African Americans, First Nations People, and Hispanic groups continue to be stereotyped or play restricted roles in film, television, and Internet sources of entertainment. Misrepresentations are a major source of cognitive schemata that associate these groups with crime, vagrancy, and incompetence. Internationally, researchers have expressed concern about the impact of such portrayals on the health of people of color and women (Estacio 2009). Properly funded by local and national agencies, indigenous writers and artists are capable of developing a rich cultural milieu that counters the negative media images plaguing people of color today. Positive emotional states accrue when racially oppressed groups are brought into contact with authentic images, activities, and cultural products rooted in their traditional culture. These positive emotional states improve one’s sense of well-being and usher in healing physiological effects.
Finally, the structural aspects of racism must be eliminated and only an extensive, long-term national commitment will do this. Unemployment, crime, high rates of incarceration, inadequate schools and housing, and rampant poor health outcomes stem from neglected infrastructure in communities of color. Worry and rumination in the face of persistent neglect (Hall et al., 2008)—though predictable responses—pose physiological hazards. Structural and policy-based forms of racism affect the lives of people of color silently and deeply, perhaps because they function subtly in a color blind fashion (Walters 2003). Erasing racial disparities in health outcomes is wedded to providing the racially oppressed with prospects for improved employment, access to quality health care with minimal discrimination, a positive sense of well-being, and knowledge of the world and skills to navigate it successfully. These salutary conditions can be achieved through a national commitment to revitalize the economic, medical, and educational structures in communities of color.
CONCLUSION
The strides the United States has made against interpersonal racism should invigorate efforts to “mitigate, resist, and undo” (Geronimus 2000) the effects of other more insidious manifestations of racism on health. The required interventions will range from multimodal individual psychotherapy to neighborhood and national movements that demand change in cultural institutions and social structures. Ultimately, the marker of progress against the dire forces racism has unleashed will be the reduction of the rates of virulent diseases in historically oppressed communities.
Contributor Information
Camara Jules P. Harrell, Department of Psychology, Howard University
Tanisha I. Burford, Department of Psychiatry, University of Pittsburgh
Brandi N. Cage, Waisman Laboratory for Brain Imaging and Behavior, University of Wisconsin
Travette McNair Nelson, Department of Psychology, Howard University.
Sheronda Shearon, Department of Psychology, Howard University.
Adrian Thompson, Department of Psychology, Howard University.
Steven Green, Department of Psychology, Howard University.
References
- Baker Houston A. Betrayal: How Black Intellectuals Have Abandoned the Ideals of the Civil Rights Era. New York: Columbia University Press; 2008. [Google Scholar]
- Barker David JP. Mothers, Babies, and Health in Later Life. 3. Edinburgh, UK: Churchill Livingstone; 1998. [Google Scholar]
- Barker David JP. Fetal Programming in Coronary Heart Disease. Trends in Endocri-nology and Metabolism. 2002;13(9):364–368. doi: 10.1016/s1043-2760(02)00689-6. [DOI] [PubMed] [Google Scholar]
- Barksdale Debra J, Farrug Eugene R, Harkness Kimberly. Racial Discrimination and Blood Pressure: Perceptions, Emotions, and Behaviors of Black American Adults. Issues in Mental Health Nursing. 2009;30(2):104–111. doi: 10.1080/01612840802597879. [DOI] [PubMed] [Google Scholar]
- Beatty Danielle L, Matthews Karen A. Unfair Treatment and Trait Anger in Relation to Nighttime Ambulatory Blood Pressure in African American and White Adolescents. Psychosomatic Medicine. 2009;71(8):813–820. doi: 10.1097/PSY.0b013e3181b3b6f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell Derrick. Silent Covenants: Brown v. Board of Education and the Unfulfilled Hopes for Racial Reform. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- Berntson Gary Gand, Cacioppo John T. From Homeostasis to Allodynamic Regulation. In: Cacioppo John T, Tassinary Louis G, Berntson Gary G., editors. Handbook of Psychophysiology. 2. New York: Cambridge University Press; 2000. pp. 459–481. [Google Scholar]
- Blascovich Jim, Spencer Steven J, Quinn Dianne, Steele Claude M. African Amerians and High Blood Pressure: The Role of Stereotype Threat. Psychological Sciences. 2001;12(2):225–229. doi: 10.1111/1467-9280.00340. [DOI] [PubMed] [Google Scholar]
- Bonilla-Silva Eduardo. Rethinking Racism: Toward a Structural Interpretation. Amer-ican Sociological Review. 1997;62(3):465–480. [Google Scholar]
- Bonilla-Silva Eduardo. White Supremacy and Racism in the Post–Civil Rights Era. Boulder, CO: Lynne Rienner Publishers; 2001. [Google Scholar]
- Bonilla-Silva Eduardo. Racism without Racists: Color-Blind Racism and the Persistence of Racial Inequality in the United States. Lanham, MD: Rowman and Littlefield Publishers, Inc; 2006. [Google Scholar]
- Brondolo Elizabeth, Libby Daniel J, Denton Ellen-ge, Thompson Shola, Beatty Danielle L, Schwartz Joseph, Sweeney Monica, Tobin Jonathan N, Cassells Andrea, Pickering Thomas G, Gerin William. Racism and Ambulatory Blood Pressure in a Community Sample. Psychosomatic Medicine. 2008;70(1):49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- Brondolo Elizabeth, Rieppi Ricardo, Kelly Kimberly, Gerin William. Perceived Racism and Blood Pressure: A Review of the Literature and Conceptual and Methodological Critique. Annals of Behavioral Medicine. 2003;25(1):55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- Brosschot Jos F, Gerin William, Thayer Julian F. The Perseverative Cognition Hypothesis: A Review of Worry, Prolonged Stress-Related Physiological Activation, and Health. Journal of Psychosomatic Research. 2006;60(2):113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Brosschot Jos F, Verkuil Bart, Thayer Julian F. Conscious and Unconscious Perseverative Cognition: Is a Large Part of Prolonged Physiological Activity Due to Unconscious Stress? Journal of Psychosomatic Research. 2010;69(4):407–416. doi: 10.1016/j.jpsychores.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Cacioppo John T, Berntson Gary G, Adolphs Ralph, Sue Carter C, Davidson Richard J, McClintock Martha K, McEwen Bruce S, Meaney Michael J, Schacter Daniel L, Sternberg Esther M, Soumi Steve S, Taylor Shelley E. Foundations in Social Neuroscience. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- Cannon Walter B. Bodily Changes in Pain, Hunger, Fear, and Rage. New York: Appleton; 1929. [Google Scholar]
- Centers for Disease Control and Prevention. [accessed February 11, 2011];2008 〈 http://www.cdc.gov/omhd/populations/BAA/BAA.htm〉.
- Chae David H, Lincoln Karen D, Adler Nancy E, Leonard Dyme S. Do Experiences of Racial Discrimination Predict Cardiovascular Disease Among African Amer-ican Men? The Moderating Role of Internalized Negative Racial Group Attitudes. Social Science and Medicine. 2010;71(6):1182–1188. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark Rodney, Anderson Norman B, Clark Vernessa R, Williams David R. Racism as a Stressor for African Americans: A Biopsychosocial Model. American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Collins James W, David Richard J, Handler Adren, Andes Stephen. Very Low Birth Weight in African American Infants: The Role of Maternal Exposure to Interpersonal Racial Discrimination. American Journal of Public Health. 2004;94(12):2132–2138. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins James W, David Richard J, Symons Rebecca, Handler Adren, Wall Stephen N, Dwyer Lisa. Low-Income African-American Mothers’ Perception of Exposure to Racial Discrimination and Infant Birth Weight. Epidemiology. 2000;11(3):337–339. doi: 10.1097/00001648-200005000-00019. [DOI] [PubMed] [Google Scholar]
- Conrad Ansgar, Roth Walton T. Muscle Relaxation Therapy for Anxiety Disorders: It Works but How? Journal of Anxiety Disorders. 2007;21(3):243–264. doi: 10.1016/j.janxdis.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Cutler David M. Behavioral Health Interventions: What Works and Why? In: Anderson Nor-man B, Bulatao Rodolfo A, Cohen Barney., editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: The National Academies Press; 2004. pp. 643–674. [PubMed] [Google Scholar]
- Daniels Ina, Harrell Camara JP, Floyd Leah, Bell Sonia. Hostility, Cultural Orientation, and Casual Blood Pressure Readings in African Americans. Ethnicity and Disease. 2001;11(4):779–787. [PubMed] [Google Scholar]
- Daum Irene, Channon Shelley, Polkey Charles E, Gray Jeffrey A. Classical Conditioning After Temporal Lobe Lesions in Man: Impairment in Conditional Discriminations. Behavioral Neuroscience. 1991;105(3):396–408. doi: 10.1037//0735-7044.105.3.396. [DOI] [PubMed] [Google Scholar]
- Davidson Richard J. Affective Style, Psychopathology, and Resilience: Brain Mechanism and Plasticity. American Psychologist. 2000;55(11):1196–1214. doi: 10.1037//0003-066x.55.11.1196. [DOI] [PubMed] [Google Scholar]
- Davidson Richard J, Kabat-Zinn Jon, Schumacher Jessica, Rosenkranz Melissa, Muller Daniel, Santorelli Saki F, Urbanowski Ferris, Harrington Ann, Bonus Katherine, Sheridan John F. Alterations in Brain and Immune Function Produced by Mindful Meditation. Psychosomatic Medicine. 2003;65(4):564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Davidson Richard J, Putnam Katherine M, Larson Christine L. Dysfunction in the Neural Circuitry of Emotion Regulation: Perspectives from Affective Neuroscience. Science. 2000;218(7):591–594. doi: 10.1126/science.289.5479.591. [DOI] [PubMed] [Google Scholar]
- Dressler William W, Bindon James. The Health Consequence of Cultural Consonance: Cultural Dimensions of Lifestyle, Social Support, and Arterial Blood Pressure in an African American Community. American Anthropologist. 2000;102(2):244–260. [Google Scholar]
- Du Bois William EB. The Health and Physique of the American Negro: A Sociological Study Made Under the Direction of Atlanta University by the Eleventh Atlanta Conference. Atlanta, GA: Atlanta University Press; 1906. [Google Scholar]
- Eckersly Richard. Is Modern Western Culture a Health Hazard? International Journal of Epidemiology. 2005;35(2):252–258. doi: 10.1093/ije/dyi235. [DOI] [PubMed] [Google Scholar]
- Eisenberger Naomi, Lieberman Matthew D, Williams Kipling D. Does Rejection Hurt? An fMRI Study of Social Exclusion. Science. 2003;302(10):290–292. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- Estacio Emee V. Editorial: Media Exploitation, Racism, and Health. Journal of Health Psychology. 2009;14(2):155–157. doi: 10.1177/1359105308100198. [DOI] [PubMed] [Google Scholar]
- Fanon Frantz. Black Skin, White Masks. New York: Grove Press; 1967. [Google Scholar]
- Fanon Frantz. The Wretched of the Earth. New York: Grove Press; 1968. [Google Scholar]
- Fredrickson Barbara L. What Good are Positive Emotions? Review of General Psychology. 1998;2(3):300–319. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson Barbara L. The Role of Positive Emotions in Positive Psychology: The Broaden-and-Build Theory of Positive Emotions. American Psychologist. 2001;56(3):218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T. The Weathering Hypothesis and the Health of African Ameri-can Women and Infants: Evidence and Speculations. Ethnicity and Disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- Geronimus Arline T. To Mitigate, Resist or Undo: Addressing Structural Influences on the Health of Urban Populations. American Journal of Public Health. 2000;90(6):867–872. doi: 10.2105/ajph.90.6.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giscombe Cheryl L, Lobel Marci. Explaining Disproportionately High Rates of Adverse Birth Outcomes Among African Americans: The Impact of Stress, Racism, and Related Factors in Pregnancy. Psychological Bulletin. 2005;131(5):662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden Philippe R, McRae Kateri, Rand Wiveka, Gross James J. The Neural Bases of Emotion Regulation: Reappraisal and Suppression of Negative Emotions. Biological Psychiatry. 2008;63(6):577–586. doi: 10.1016/j.biopsych.2007.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene Natasha A, Morris Vernon R. Assessment of Public Health Risks Associated with Atmospheric Exposure to PM2.5 in Washington, DC, USA. International Journal of Environmental Research in Public Health. 2006;3(1):86–97. doi: 10.3390/ijerph2006030010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross James J, John Oliver P. Individual Difference in Two Emotion Regulation Processes. Implication for Affective Relationships and Well-being. Journal of Personality and Social Psychology. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hall Diane M, Cassidy Elaine F, Stevenson Howard C. Acting Tough in a Tough World: An Examination of Fear among Urban African American Adolescents. Journal of Black Psychology. 2008;34(3):381–398. [Google Scholar]
- Harrell Camara JP. Manichean Psychology: Racism and the Minds of People of African Descent. Washington, DC: Howard University Press; 1999. [Google Scholar]
- Harrell Camara JP, Hall Sadiki, Taliaferro James. Physiological Responses to Racism and Discrimination: An Assessment of the Evidence. American Journal of Public Health. 2003;93(2):243–248. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell Camara JP, Neblett Enrique, Onyewuenyi Ikechukwu. Physiological Activity During Adolescence. In: Swanson Dena S, Spencer Margaret B, Edwards Malik C., editors. Adolescent Development in a Global Era. San Diego, CA: Elsevier; 2010. pp. 31–62. [Google Scholar]
- Harrell Jules P, Merritt Marcellus M, Kalu Jamilee. Racism, Stress, and Disease. In: Jones Reginald., editor. African American Mental Health: Theory, Research, and Intervention. Hampton, VA: Cobb and Henry Publishers; 1998. pp. 247–280. [Google Scholar]
- Harrell Shelly. A Multidimensional Conceptualization of Racism-Related Stress: Implications for the Well-Being of People of Color. American Journal of Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Hobel Calvin, Culhane Jennifer. Role of Psychosocial and Nutritional Stress on Poor Pregnancy Outcomes. Journal of Nutrition. 2003;133(5):1709S–1717S. doi: 10.1093/jn/133.5.1709S. [DOI] [PubMed] [Google Scholar]
- Jackson Daren C, Malmstedt Jessica R, Larson Christine L, Davidson Richardson J. Suppression and Enhancement of Emotional Response to Unpleasant Pictures. Psychophysiology. 2000;37(4):515–522. [PubMed] [Google Scholar]
- Jackson James, Knight Katherine M. Race and Self-Regulatory Behaviors: The Role of the Stress Response and HPA Axis in Physical and Mental Health. In: Carstensen Laura L, Warner Schaie K., editors. Social Structure, Aging and Self-Regulation in the Elderly. New York: Springer; 2006. pp. 189–207. [Google Scholar]
- Jaenisch Rudolf, Bird Adrian. Epigenetic Regulation of Gene Expression: How the Genome Integrates Intrinsic and Environmental Signals. Nature Genetic Supplement. 2003;33(3):245–254. doi: 10.1038/ng1089. [DOI] [PubMed] [Google Scholar]
- Jones Camara P. Levels of Racism: A Theoretical Framework and a Gardener’s Tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones James M. Prejudice and Racism. New York: McGraw-Hill; 1972. [Google Scholar]
- Kemeny Margaret E. Psychobiological Responses to Social Threat: Evolution of a Psychological Model of Psychoneuroimmunology. Brain Behavior Immunology. 2009;23(1):1–9. doi: 10.1016/j.bbi.2008.08.008. [DOI] [PubMed] [Google Scholar]
- Krieger Nancy. Racial and Gender Discrimination: Risk Factors for High Blood Pressure. Social Science and Medicine. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- Krieger Nancy. Epidemiology and the Web of Causation: Has Anyone seen the Spider? Social Science and Medicine. 1994;39(7):887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- Krieger Nancy. Embodying Inequality: A Review of Concepts, Measures, and Methods for Studying Health Consequences of Discrimination. International Journal of Health Services. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger Nancy. Embodiment: A Conceptual Glossary for Epidemiology. Journal of Epidemiology and Community Health. 2005;59(5):350–355. doi: 10.1136/jech.2004.024562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger Nancy, Sidney Stephen. Racial Discrimination and Blood Pressure: The CARDIA Study of Young Black and White Adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzawa Christopher W, Sweet Elizabeth. Epigenetics and the Embodiment of Race: Developmental Origins of U.S. Racial Disparities in Cardiovascular Health. American Journal of Human Biology. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- Lauderdale Diane S. Birth Outcomes for Arabic-Named Women Before and After September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- LeDoux Joseph. The Emotional Brain. New York: Simon and Schuster; 1996. [Google Scholar]
- LeDoux Joseph. Synaptic Self: How Our Brains Become Who We Are. New York: Penguin Books; 2002. [Google Scholar]
- Levine Robert S, Foster James E, Fullilove Robert E, Fullilove MT, Briggs Nathanial C, Hull Pamela C, Husaini Baqar A, Hennekens Charles H. Black-White Inequalities in Mortality and Life Expectancy, 1933–1999: Implications for Healthy People 2010. Public Health Reports. 2001;116(5):474–483. doi: 10.1093/phr/116.5.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis Tene T, Barnes Lisa L, Bienias Julia L, Lackland Daniel T, Evans Dennis A, Mendes De Leon Carlos F. Perceived Discrimination and Blood Pressure in Older African American and White Adults. Journal of Gerontology and Biomedical Science Medicine. 2009;64(9):1002–1008. doi: 10.1093/gerona/glp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman Matthew D, Hariri Ahmad, Jarcho Johanna M, Eisenberger Naomi I, Bookheimer Susan Y. An fMRI Investigation of Race-Related Amygdala Activity in African-American and Caucasian-American Individuals. Nature Neuroscience. 2005;8(4):720–722. doi: 10.1038/nn1465. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S. Protective and Damaging Effects of Stress Mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S, Gianaros Peter J. Central Role of the Brain in Stress and Adaptation: Links to Socioeconomic Status, Health, and Disease. Annals of the New York Academy of Science. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Kelly. A Review of Hoffman’s Race Traits and Tendencies of the American Negro. Washington, DC: The American Negro Academy; 1897. [Google Scholar]
- Moore David S. The Dependent Gene: The Fallacy of “Nature vs Nurture”. New York: Henry Holt and Company; 2001. [Google Scholar]
- Mustillo Susan, Krieger Nancy, Gunderson Erica P, Sidney Steven, McCreath Heather, Kiefe Catarina I. Self-Reported Experiences of Racial Discrimination and Black-White Differences in Preterm and Low-Birthweight Deliveries. American Journal of Public Health. 2004;94(12):2125–2131. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obrist Paul. Cardiovascular Psychophysiology: A Perspective. New York: Plenum; 1981. [Google Scholar]
- Ochsner Kevin, Gross James J. The Cognitive Control of Emotion. Trends in Cognitive Neuroscience. 2005;9(5):242–249. doi: 10.1016/j.tics.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Paradies Yin. A Systematic Review of Empirical Research on Self-Reported Racism and Health. International Journal of Epidemiology. 2006a;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Paradies Yin. Defining, Conceptualizing and Characterizing Racism in Health Research. Critical Public Health. 2006b;16(2):143–157. [Google Scholar]
- Paradies Yin, Chandrakumar Loga, Klocker Natascha, Frere Marion, Webster Kim, Burrell Michelle, McLean Philippa. Building on our Strengths: A Framework to Reduce Race-Based Discrimination and Support Diversity in Victoria. Melbourne, Australia: Victorian Health Promotion Foundation; 2009. [Google Scholar]
- Pascoe Elizabeth A, Richman Laura S. Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlow Laura, Jones Gary. The Impact of Abbreviated Progressive Muscle Relaxation on Salivary Cortisol. Biological Psychology. 2002;60(1):1–16. doi: 10.1016/s0301-0511(02)00010-8. [DOI] [PubMed] [Google Scholar]
- Phillips Kristin M, Antoni Michael H, Lechner Suzanne C, Blomberg Bonnie B, Llabre Maria M, Avisar Eli, Glück Stefan, DerHagopian Robert, Carver Charles S. Stress Management Intervention Reduces Serum Cortisol and Increases Relaxation During Treatment for Nonmetastatic Breast Cancer. Psychosomatic Medicine. 2008;70(9):1044–1049. doi: 10.1097/PSY.0b013e318186fb27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges Stephen W. Orienting in a Defensive World: Mammalian Modifications of our Evolutionary Heritage: A Polyvagal Theory. Psychophysiology. 1995;32(4):301–318. doi: 10.1111/j.1469-8986.1995.tb01213.x. [DOI] [PubMed] [Google Scholar]
- Porges Stephen W. Polyvagal Theory: Phylogenetic Substrates of a Social Nervous System. International Journal of Psychophysiology. 2001;42(2):123–146. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- Schmader Toni, Johns Michael, Forbes Chad. An Integrated Process Model of Stereotype Threat Effects on Performance. Psychological Review. 2008;115(2):336–356. doi: 10.1037/0033-295X.115.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman Teresa, Epel Elissa, Gruenewald Tara, Karlamangla Arun, McEwen Bruce S. Socioeconomic Differentials in Peripheral Biology: Cumulative Allostatic Load. Annals of the New York Academy of Sciences. 2010;1186(1):223–239. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- Soares Joaquim J, Ohman Arne. Backward Masking and Skin Conductance Responses After Conditioning to Nonfeared but Fear-Relevant Stimuli in Fearful Subjects. Psychophys-iology. 1993;30(5):460–466. doi: 10.1111/j.1469-8986.1993.tb02069.x. [DOI] [PubMed] [Google Scholar]
- Taylor Jerome, Obiechina Chioma O, Harrison Sherlyn. Toward a Psychology of Liberation and Restoration: Answering the Challenge of Cultural Alienation. In: Jones Reginald., editor. African American Mental Health: Theory, Research, and Intervention. Hampton, VA: Cobb and Henry Press; 1998. pp. 283–301. [Google Scholar]
- Thayer Julian F, Friedman Bruce H. A Neurovisceral Integration Model of Health Disparities in Aging. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: The National Academies Press; 2004. pp. 567–603. [PubMed] [Google Scholar]
- Thayer Julian F, Lane Richard D. The Role of Vagal Function in the Risk of Cardiovascular Disease and Mortality. Biological Psychology. 2007;74(2):224–242. doi: 10.1016/j.biopsycho.2005.11.013. [DOI] [PubMed] [Google Scholar]
- Walters Ronald W. African American Life Series. Detroit, MI: Wayne State University Press; 2003. White Nationalism, Black Interests: Conservative Public Policy and the Black Community. [Google Scholar]
- Williams David R. Race and Health: Basic Questions, Emerging Directions. Annals of Epidemiology. 1997;7(5):322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams David R, Mohammed Selina A. Discrimination and Racial Disparities in Health: Evidence and Needed Research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]