The engineering of multicellular organotypic models of the human intestinal mucosa has wide-ranging potential as a tool for discovery in both health and disease, including interaction with pathogens, antigen trafficking, inflammatory and physiological processes. However, models reported to date remain relatively simple composed of few cell types. Here, we report the development of an organotypic model with close structural and functional resemblance to the human intestinal mucosa; it is comprised of fibroblasts, lymphocytes, epithelial cells, and endothelial cells. Moreover, epithelial cells in our 3-D system can differentiate into multiple lineages (e.g., goblet cells, M cells and differentiated enterocytes). We hypothesized that under both microgravity and proper culture conditions, aggregates of randomly distributed cells will self-organize into a spatial configuration resembling those in native tissues. Our hypothesis was based on recent developments showing that: (1) the culture of epithelial cells as well as endothelial cells under microgravity can be accompanied by a commensurate increase in the cell differentiation1–3 and (2) gelled collagen-I can constitute a flexible extracellular matrix (ECM) to be used under microgravity.4 It is known that collagen-I possesses most of the properties of an ideal scaffold, such as specific gravity similar to the culture medium and the capability to incorporate other relevant ECM proteins.4 In our model, fibroblasts and endothelial cells were embedded in a collagen-I matrix enriched with additional gut basement membrane proteins (i.e., laminin, collagen IV, fibronectin and heparin sulfate proteoglycan) and added to Rotating Wall Vessel (RWV) bioreactors containing epithelial cells (Supplementary Methods). These epithelial cells consisted of a human enterocyte cell line (i.e., HCT-8) that was originally derived from the junction of the small and large bowel.5 The choice of this cell line was based on its ability to successfully differentiate in a low shear microgravity environment1 provided by the RWV bioreactor.6 Activated lymphocytes were added twice to the culture at days 4 (± 1 day) and 9 (± 1 day) (Supplementary Methods).
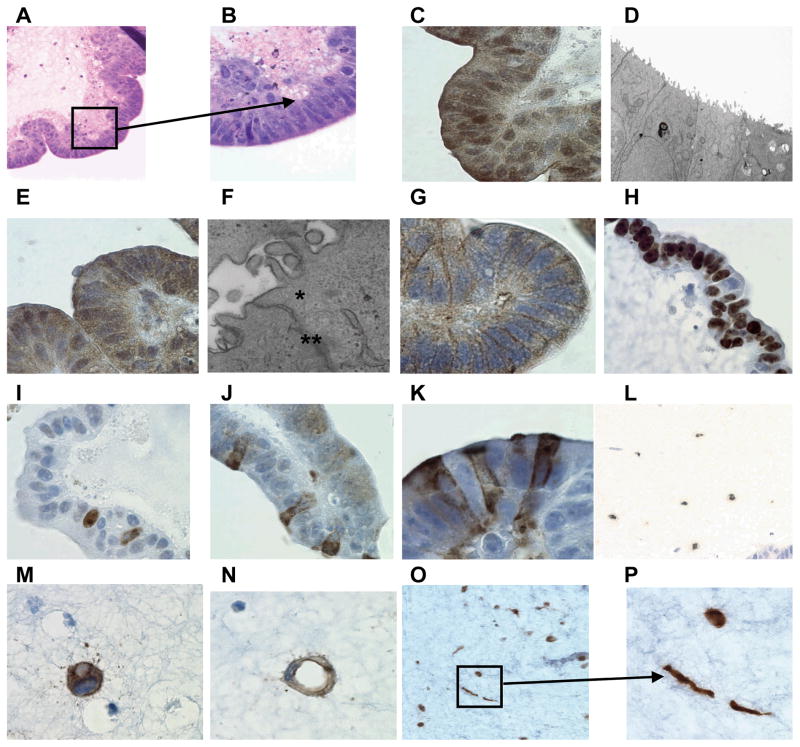
After 10 to 15 days, histological staining and electron microscopy demonstrated the presence of villus-like structures in the constructs. About 60–80% of these epithelial cells were organized as a monolayer of polarized cells with nuclei located in a basal position near the ECM, a major feature of well-differentiated cells (Figure 1A). H&E staining also demonstrated the presence of a brush border, or microvilli, seen collectively as a fuzzy fringe in the apical surface of the epithelium (Figure 1B). The presence of microvilli was further evidenced by immunochemical staining using an anti-villin mouse monoclonal antibody (mAb) or by electron microscopy (Figure 1C and D, respectively). Assessment by immunostaining for zonula occludens (ZO)-1, a protein involved in the formation of tight junctions, and electron microscopy demonstrated that our 3-D organotypic model recapitulates the formation of tight junctions and desmosomes (Figure 1E and F). In addition, because immortalized epithelial cells in 3-D systems may lose the growth pattern found in the normal epithelium, we assessed the expression of E-cadherin and the Ki-67 proliferation marker in our 3-D model. As expected, HCT-8 cell lines expressed E-cadherin but only negligible amount of Ki-67 antigen, a pattern consistent with normal highly-differentiated epithelium (Figures 1G–I). Finally, these HCT-8 cells also expressed numerous markers for multi-lineage differentiation to globet (mucin 2, MUC 2) and M (Sialyl Lewis Antigen) cell lineages (Figures 1J and K). Goblet and M cells were distributed throughout the epithelial layer (Figures 1J and K, respectively). We also investigated the presence of the machinery for the specific digestion and transfer of glucose. We observed apical expression of dissacharidases (i.e., sucrase-isomaltase, SI) and sugar transporters (i.e., energy-dependent sodium-glucose co-transporter 1, SGLT1) which strongly suggests that epithelial cells in our 3-D model are able to absorb and transport glucose (data not shown). Taken together, these results demonstrate a remarkable degree of differentiation of HCT-8 epithelial cells in our 3-D model.
Figure 1.
Epithelial cell differentiation. Hematoxylin and eosin staining of 14 day-cells cultured in the 3-D microgravity model: tissues were stained purple and scaffold stained pink. Lower (A) and higher magnification (B) shows the presence of polarized epithelial cells with microvilli seen collectively as a fuzzy fringe in the apical surface of the epithelium. The presence of microvilli was further confirmed by immunochemical staining using the anti-villin mouse mAb (C) and by electron microscopy (D). Presence of tight junctions was detected by Immunochemical staining by using an anti-ZO-1 polyclonal rabbit antiserum (E) or electron microscopy (F) (tight junctions (*) and desmosome (**)). Immunochemical staining was also used to detect E-cadherin using the anti-E-cadherin mouse mAb (G). The presence of proliferating cells was detected at day 5 (H) and day 15 (I) by using the anti-Ki67 rabbit mAb. The presence of multi-lineage differentiation was also observed: goblet cells using the anti-MUC-2 monoclonal antibody (J) and M cells using the anti-Sialyl Lewis Antigen mAb at day 15 (K). Cells from a 17-day 3-D organotypic culture were also stained by immunochemistry for lymphocytes using the anti-CD45 mAb (L) (low magnification), for endothelial cells using the anti-CD31 mAb (M) (sprouting) (N) (vessel-like conduit formation)(high magnification), and for fibroblasts using the anti-vimentin mAb at low (O) and (P)(spindle shaped rounded-fat cell-like shaped) at high magnification.
We also examined the presence and persistence of other cell types by monitoring the presence of defined cellular markers for each individual cell type (i.e., CD45 for hematopoietic-derived cells, including lymphocytes; CD31 for endothelial cells and Vimentin for fibroblasts). These studies were performed by immunochemistry. We observed that the lymphocytes migrated through the epithelial cell layer and localized to the ECM. We were able to detect lymphocytes for at least 7 days (last day examined) (Figure 1L). As in the native gut tissue, in our 3-D model fibroblasts and endothelial cells remained dispersed throughout the ECM. Interestingly, we observed that individual endothelial cells exhibited cytoplasmic extensions that form bridges between them, suggesting that these endothelial cells were activated and underwent a remodeling phase (Figures 1M and N). However, the vast majority of these endothelial cells do not appear to differentiate towards the formation of vessel-like conduits. Additional studies are needed to determine the proper conditions that will further enable vessel-like conduits to form. Interestingly, fibroblasts showed different shapes, ranging from classical spindle shaped to rounded-fat cell-like shaped with the nucleus pushed to one side (Figures 1O and P). These results suggest that cells were activated and remain able to both receive and respond to differentiation signals. Finally, several studies have demonstrated that good viability for primary cells lasting more than 10 days in culture systems is difficult to achieve.7 Thus, we assessed cell viability by immunochemical staining using antibodies to cleaved Caspase-3. Up to 20 days after the initiation of the cultures, few cleaved Caspase-3-positive cells were observed in the ECM, the major location of primary cells including lymphocytes, fibroblasts and endothelial cells (data not shown).
Although the combination of the features described above give some insights into the similarities of our 3-D organotypic model to in vivo tissues, we further assessed its functionality by observing its response to exposure to a human enteric bacterial pathogen. Specifically, we examined the changes in the epithelial cell morphology, as well as cytokine production, following exposure to wild-type Salmonella enterica serovar Typhi (S. Typhi) strain ISP1820, to evaluate whether it mimicked the reported stages of the infection. The identification and characterization of S. Typhi-infected cells was accomplished using a polyclonal antibody that specifically detects common Salmonella antigens (CSA-1). A visible feature of the Salmonella entry process in vivo, i.e., membrane rearrangements or ruffles, were observed in our system as early as 1 hour after infection (Supplementary Figure 1B) and increased over time (Supplementary Figures 1C and D). Of note, these ruffles were absent in the control (not-infected cells, Supplementary Figure 1A). One day after infection, the ruffles fade away and bacteria, when present, was mostly observed on the cell surface/brush border of healthy looking epithelial cells or intracellular in epithelial cells sloughed from the monolayer which likely died as a result of the infection (Supplementary Figures 1E and F). We also observed that the exposure to Salmonella resulted in production of cytokines, including IL-1β, IL-6, IL-8, IL-11, IL-12p70, IL-17a, IL-21 and TNF-α (Supplementary Figures 1G, H and I). These results are in agreement, and extend previous studies showing the importance of these cytokines in the control of Salmonella infection8, 9 and further confirming the functional capacity of this 3-D organotypic model to properly react to the presence of an enteric pathogen.
To summarize, although similar approaches have been attempted by other investigators with moderate success,1, 10 our system provides major innovations and advances such as a matrix enriched with gut basement membrane proteins. Also, to our knowledge, except for our system described above, attempts to integrate multiple cell types in 3-D constructs grown under microgravity have been unsuccessful. Finally, we provided evidence that our 3-D model might be a helpful tool to investigate the early events of the host interaction with gastrointestinal pathogens, including invasion, pathogenesis and immune responses.
Material and Methods
Material and Methods and any associated references are available in the online version of the paper.
Supplementary Material
Acknowledgments
Grant Support: This work was supported in part by contract NO1 AI-30028 and by grants U19 AI-082655 and R01 AI-36525 from the National Institute of Allergy and Infectious Diseases.
Abbreviations
- CD
cluster of differentiation
- CSA-1
common Salmonella antigen
- DAB
3,3-diaminobenzidine
- ECM
extracellular matrix
- HUVEC
human umbilical vein endothelial cells
- mAb
monoclonal antibody
- PBS
phosphate-buffered saline
- RWV
rotating wall vessel
- S. Typhi
Salmonella enterica serovar Typhi
- 3-D
three-dimensional
- ZO
zonula occludens
Footnotes
Disclosures: The authors declare that a provisional patent has been filed in the U.S. Patent and Trademark Office (Number: 61/436,710).
Author Contributions: Rosângela Salerno-Goncalves designed the study, performed the experiments, analyzed the data and wrote the manuscript; Alessio Fasano and Marcelo B. Sztein contributed to the design and analysis of the data and wrote the manuscript.
References
- 1.Carvalho HM, Teel LD, Goping G, O’Brien AD. A three-dimensional tissue culture model for the study of attach and efface lesion formation by enteropathogenic and enterohaemorrhagic Escherichia coli. Cell Microbiol. 2005;7:1771–81. doi: 10.1111/j.1462-5822.2004.00594.x. [DOI] [PubMed] [Google Scholar]
- 2.Khaoustov VI, Darlington GJ, Soriano HE, Krishnan B, Risin D, Pellis NR, Yoffe B. Induction of three-dimensional assembly of human liver cells by simulated microgravity. In Vitro Cell Dev Biol Anim. 1999;35:501–9. doi: 10.1007/s11626-999-0060-2. [DOI] [PubMed] [Google Scholar]
- 3.Sanford GL, Ellerson D, Melhado-Gardner C, Sroufe AE, Harris-Hooker S. Three-dimensional growth of endothelial cells in the microgravity-based rotating wall vessel bioreactor. In Vitro Cell Dev Biol Anim. 2002;38:493–504. doi: 10.1290/1071-2690(2002)038<0493:TGOECI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Su GN, Hidaka M, Kimura Y, Yamamoto G. In situ collagen gelation: a new method for constructing large tissue in rotary culture vessels. In Vitro Cell Dev Biol Anim. 2003;39:368–74. doi: 10.1290/1543-706X(2003)039<0368:ISCGAN>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Tompkins WA, Watrach AM, Schmale JD, Schultz RM, Harris JA. Cultural and antigenic properties of newly established cell strains derived from adenocarcinomas of the human colon and rectum. J Natl Cancer Inst. 1974;52:1101–10. doi: 10.1093/jnci/52.4.1101. [DOI] [PubMed] [Google Scholar]
- 6.Unsworth BR, Lelkes PI. Growing tissues in microgravity. Nat Med. 1998;4:901–7. doi: 10.1038/nm0898-901. [DOI] [PubMed] [Google Scholar]
- 7.Perreault N, Beaulieu JF. Primary cultures of fully differentiated and pure human intestinal epithelial cells. Exp Cell Res. 1998;245:34–42. doi: 10.1006/excr.1998.4221. [DOI] [PubMed] [Google Scholar]
- 8.Kagnoff MF, Eckmann L. Epithelial cells as sensors for microbial infection. J Clin Invest. 1997;100:6–10. doi: 10.1172/JCI119522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raffatellu M, Santos RL, Verhoeven DE, George MD, Wilson RP, Winter SE, Godinez I, Sankaran S, Paixao TA, Gordon MA, Kolls JK, Dandekar S, Baumler AJ. Simian immunodeficiency virus-induced mucosal interleukin-17 deficiency promotes Salmonella dissemination from the gut. Nat Med. 2008;14:421–8. doi: 10.1038/nm1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nickerson CA, Goodwin TJ, Terlonge J, Ott CM, Buchanan KL, Uicker WC, Emami K, LeBlanc CL, Ramamurthy R, Clarke MS, Vanderburg CR, Hammond T, Pierson DL. Three-dimensional tissue assemblies: novel models for the study of Salmonella enterica serovar Typhimurium pathogenesis. Infect Immun. 2001;69:7106–20. doi: 10.1128/IAI.69.11.7106-7120.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.